Beyond Aortic Stenosis: Addressing the Challenges of Multivalvular Disease Assessment
Abstract
:1. Introduction
2. Pathophysiology of Concomitant Aortic Stenosis and Other Valve Lesions
2.1. Functional Valve Disease
2.2. Rheumatic Heart Disease
2.3. Degenerative Etiology
2.4. Infiltrative Cardiomyopathies
2.5. Congenital Heart Disease
2.6. Infective Endocarditis
2.7. Other Causes
3. Diagnostic Challenges
3.1. Role of Echocardiography
3.2. The Role of Stress Echocardiography
3.3. Role of CT
3.4. Role of CMR
4. Therapeutic Approach
4.1. Therapeutic Approach to the Patient with Aortic Stenosis
4.2. Therapeutic Approach to the Patient with Aortic Stenosis and Concomitant Valvular Disease
5. Future Aspects and Gaps in Evidence
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AS | aortic stenosis |
| VHD | valvular heart disease |
| CT | computed tomography |
| CMR | cardiac magnetic resonance |
| MR | mitral regurgitation |
| RHD | rheumatic heart disease |
| CHD | congenital heart disease |
| IE | infective endocarditis |
| TR | tricuspid regurgitation |
| LV | left ventricular |
| PH | pulmonary hypertension |
| RV | right ventricular |
| RA | right atrial |
| ARF | acute rheumatic fever |
| MV | mitral valve |
| AV | aortic valve |
| AR | aortic regurgitation |
| CA | cardiac amyloidosis |
| BAV | bicuspid AV |
| EROA | effective regurgitant orifice area |
| PISA | proximal isovelocity surface area |
| LF-LG | low-flow low-gradient |
| AVA | AV area |
| MDCT | multidetector computer tomography |
| MS | mitral stenosis |
| PHT | pressure half-time |
| DSE | dobutamine stress echocardiography |
| TAVR | transcatheter AV replacement |
| SSFP | steady-state free precession |
| LGE | late gadolinium enhancement |
| ECV | extracellular volume |
| AVR | AV replacement |
| SAVR | Surgical AVR |
| INR | international normalized ratio |
References
- Unger, P.; Pibarot, P.; Tribouilloy, C.; Lancellotti, P.; Maisano, F.; Iung, B.; Piérard, L. Multiple and Mixed Valvular Heart Diseases. Circ. Cardiovasc. Imaging 2018, 11, 862. [Google Scholar] [CrossRef] [Green Version]
- Ong, G.; Pibarot, P. Combined Aortic Stenosis and Regurgitation: Double the Trouble. Heart 2019, 105, 1515–1522. [Google Scholar] [CrossRef]
- Iung, B.; Baron, G.; Butchart, E.G.; Delahaye, F.; Gohlke-Bärwolf, C.; Levang, O.W.; Tornos, P.; Vanoverschelde, J.L.; Vermeer, F.; Boersma, E.; et al. A Prospective Survey of Patients with Valvular Heart Disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur. Heart J. 2003, 24, 1231–1243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossi, A.; Dandale, R.; Nistri, S.; Faggiano, P.; Cicoira, M.; Benfari, G.; Onorati, F.; Santini, F.; Messika-Zeitoun, D.; Enriquez-Sarano, M.; et al. Functional Mitral Regurgitation in Patients with Aortic Stenosis: Prevalence, Clinical Correlates and Pathophysiological Determinants: A Quantitative Prospective Study. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 631–636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, K.; Yu, G.; Jue, J. Prevalence and Spectrum of Conditions Associated with Severe Tricuspid Regurgitation. Echocardiography 2014, 31, 558–562. [Google Scholar] [CrossRef]
- Beach, J.M.; Mihaljevic, T.; Svensson, L.G.; Rajeswaran, J.; Marwick, T.; Griffin, B.; Johnston, D.R.; Sabik, J.F.; Blackstone, E.H. Coronary Artery Disease and Outcomes of Aortic Valve Replacement for Severe Aortic Stenosis. J. Am. Coll. Cardiol. 2013, 61, 837–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Unger, P.; Dedobbeleer, C.; Van Camp, G.; Plein, D.; Cosyns, B.; Lancellotti, P. Mitral Regurgitation in Patients with Aortic Stenosis Undergoing Valve Replacement. Heart 2010, 96, 9–14. [Google Scholar] [CrossRef]
- Rossi, A.; Dini, F.L.; Agricola, E.; Faggiano, P.; Benfari, G.; Temporelli, P.L.; Cucco, C.; Scelsi, L.; Vassanelli, C.; Ghio, S. Left Atrial Dilatation in Systolic Heart Failure: A Marker of Poor Prognosis, Not Just a Buffer between the Left Ventricle and Pulmonary Circulation. J. Echocardiogr. 2018, 16, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Dreyfus, G.D.; Corbi, P.J.; Chan, K.M.J.; Bahrami, T. Secondary Tricuspid Regurgitation or Dilatation: Which Should Be the Criteria for Surgical Repair? Ann. Thorac. Surg. 2005, 79, 127–132. [Google Scholar] [CrossRef]
- Remenyi, B.; Carapetis, J.; Wyber, R.; Taubert, K.; Mayosi, B.M. Position Statement of the World Heart Federation on the Prevention and Control of Rheumatic Heart Disease. Nat. Rev. Cardiol. 2013, 10, 284–292. [Google Scholar] [CrossRef]
- Watkins, D.A.; Johnson, C.O.; Colquhoun, S.M.; Karthikeyan, G.; Beaton, A.; Bukhman, G.; Forouzanfar, M.H.; Longenecker, C.T.; Mayosi, B.M.; Mensah, G.A.; et al. Global, Regional, and National Burden of Rheumatic Heart Disease, 1990–2015. N. Engl. J. Med. 2017, 377, 713–722. [Google Scholar] [CrossRef]
- Krisher, K.; Cunningham, M.W. Myosin: A Link Between Streptococci and Heart. Science 1985, 227, 413–415. [Google Scholar] [CrossRef] [PubMed]
- Bryant, P.A.; Robins-Browne, R.; Carapetis, J.R.; Curtis, N. Some of the People, Some of the Time. Circulation 2009, 119, 742–753. [Google Scholar] [CrossRef] [Green Version]
- He, V.Y.F.; Condon, J.R.; Ralph, A.P.; Zhao, Y.; Roberts, K.; De Dassel, J.L.; Currie, B.J.; Fittock, M.; Edwards, K.N.; Carapetis, J.R. Long-Term Outcomes From Acute Rheumatic Fever and Rheumatic Heart Disease: A Data-Linkage and Survival Analysis Approach. Circulation 2016, 134, 222. [Google Scholar] [CrossRef] [PubMed]
- Vasan, R.S.; Shrivastava, S.; Vijayakumar, M.; Narang, R.; Lister, B.C.; Narula, J. Echocardiographic Evaluation of Patients with Acute Rheumatic Fever and Rheumatic Carditis. Circulation 1996, 94, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Pandian, N.G.; Kim, J.K.; Arias-Godinez, J.A.; Marx, G.R.; Michelena, H.I.; Chander Mohan, J.; Ogunyankin, K.O.; Ronderos, R.E.; Sade, L.E.; Sadeghpour, A.; et al. Recommendations for the Use of Echocardiography in the Evaluation of Rheumatic Heart Disease: A Report from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2023, 36, 3–28. [Google Scholar] [CrossRef]
- Negi, P.C.; Mahajan, K.; Rana, V.; Sondhi, S.; Mahajan, N.; Rathour, S.; Verma, R.; Dhiman, A.; Dev, M.; Rao, S.; et al. Clinical Characteristics, Complications, and Treatment Practices in Patients with RHD: 6-Year Results From HP-RHD Registry. Glob. Heart 2018, 13, 267–274.e2. [Google Scholar] [CrossRef]
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of Valvular Heart Diseases: A Population-Based Study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Coffey, S.; Roberts-Thomson, R.; Brown, A.; Carapetis, J.; Chen, M.; Enriquez-Sarano, M.; Zühlke, L.; Prendergast, B.D. Global Epidemiology of Valvular Heart Disease. Nat. Rev. Cardiol. 2021, 18, 853–864. [Google Scholar] [CrossRef]
- Manduteanu, I.; Simionescu, D.; Simionescu, A.; Simionescu, M. Aortic Valve Disease in Diabetes: Molecular Mechanisms and Novel Therapies. J. Cell. Mol. Med. 2021, 25, 9483–9495. [Google Scholar] [CrossRef] [PubMed]
- Shroff, G.R.; Bangalore, S.; Bhave, N.M.; Chang, T.I.; Garcia, S.; Mathew, R.O.; Rangaswami, J.; Ternacle, J.; Thourani, V.H.; Pibarot, P. Evaluation and Management of Aortic Stenosis in Chronic Kidney Disease: A Scientific Statement From the American Heart Association. Circulation 2021, 143, E1088–E1114. [Google Scholar] [CrossRef] [PubMed]
- Ternacle, J.; Krapf, L.; Mothy, D.; Magne, J.; Nguyen, A.; Galat, A.; Gallet, R.; Teiger, E.; Côté, N.; Clavel, M.A.; et al. Aortic Stenosis and Cardiac Amyloidosis: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 74, 2638–2651. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, O.; Cordeiro, F.; Gago, M.F.; Miltenberger-miltenyi, G.; Ferreira, C.; Sousa, N.; Cunha, D. Fabry Disease and the Heart: A Comprehensive Review. Int. J. Mol. Sci. 2021, 22, 4434. [Google Scholar] [CrossRef] [PubMed]
- Thakker, R.A.; Abdelmaseih, R.; Hasan, S.M. Sarcoidosis and Aortic Stenosis: A Role for Transcatheter Aortic Valve Replacement? Curr. Probl. Cardiol. 2021, 46, 100858. [Google Scholar] [CrossRef]
- Galat, A.; Guellich, A.; Bodez, D.; Slama, M.; Dijos, M.; Zeitoun, D.M.; Milleron, O.; Attias, D.; Dubois-Randé, J.L.; Mohty, D.; et al. Aortic Stenosis and Transthyretin Cardiac Amyloidosis: The Chicken or the Egg? Eur. Heart J. 2016, 37, 3525–3531. [Google Scholar] [CrossRef] [Green Version]
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.-P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the Management of Adult Congenital Heart Disease The Task Force for the Management of Adult Congenital Heart Disease of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Adult Congenital Heart Disease (ISACHD). Eur. Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef]
- Michelena, H.I.; Della Corte, A.; Evangelista, A.; Maleszewski, J.J.; Edwards, W.D.; Roman, M.J.; Devereux, R.B.; Fernández, B.; Asch, F.M.; Barker, A.J.; et al. International Consensus Statement on Nomenclature and Classification of the Congenital Bicuspid Aortic Valve and Its Aortopathy, for Clinical, Surgical, Interventional and Research Purposes. Eur. J. Cardio-Thorac. Surg. 2021, 60, 448–476. [Google Scholar] [CrossRef]
- Bravo-Jaimes, K.; Prakash, S.K. Genetics in Bicuspid Aortic Valve Disease: Where Are We? Prog. Cardiovasc. Dis. 2020, 63, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Ciotti, G.R.; Vlahos, A.P.; Silverman, N.H. Morphology and Function of the Bicuspid Aortic Valve with and without Coarctation of the Aorta in the Young. Am. J. Cardiol. 2006, 98, 1096–1102. [Google Scholar] [CrossRef]
- Castonguay, M.C.; Burner, K.D.; Edwards, W.D.; Baddour, L.M.; Maleszewski, J.J. Surgical Pathology of Native Valve Endocarditis in 310 Specimens from 287 Patients (1985–2004). Cardiovasc. Pathol. 2013, 22, 19–27. [Google Scholar] [CrossRef]
- Michelena, H.I.; Katan, O.; Suri, R.M.; Baddour, L.M.; Enriquez-Sarano, M. Incidence of Infective Endocarditis in Patients with Bicuspid Aortic Valves in the Community. Mayo Clin. Proc. 2016, 91, 122–123. [Google Scholar] [CrossRef] [Green Version]
- Fishbein, G.A.; Fishbein, M.C. Pathology of the Aortic Valve: Aortic Valve Stenosis/Aortic Regurgitation. Curr. Cardiol. Rep. 2019, 21, 81. [Google Scholar] [CrossRef] [PubMed]
- Gujral, D.M.; Lloyd, G.; Bhattacharyya, S. Radiation-Induced Valvular Heart Disease. Heart 2016, 102, 269–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benfari, G.; Nistri, S.; Faggiano, P.; Clavel, M.-A.; Maffeis, C.; Enriquez-Sarano, M.; Vassanelli, C.; Rossi, A. Mitral Effective Regurgitant Orifice Area Predicts Pulmonary Artery Pressure Level in Patients with Aortic Valve Stenosis. J. Am. Soc. Echocardiogr. 2018, 31, 570–577.e1. [Google Scholar] [CrossRef] [PubMed]
- Unger, P.; Plein, D.; Van Camp, G.; Cosyns, B.; Pasquet, A.; Henrard, V.; de Cannière, D.; Melot, C.; Piérard, L.A.; Lancellotti, P. Effects of Valve Replacement for Aortic Stenosis on Mitral Regurgitation. Am. J. Cardiol. 2008, 102, 1378–1382. [Google Scholar] [CrossRef] [PubMed]
- HONEY, M. Clinical and Haemodynamic Observations on Combined Mitral and Aortic Stenosis. Br. Heart J. 1961, 23, 545–555. [Google Scholar] [CrossRef] [Green Version]
- Karp, K.; Teien, D.; Bjerle, P.; Eriksson, P. Reassessment of Valve Area Determinations in Mitral Stenosis by the Pressure Half-Time Method: Impact of Left Ventricular Stiffness and Peak Diastolic Pressure Difference. J. Am. Coll. Cardiol. 1989, 13, 594–599. [Google Scholar] [CrossRef] [Green Version]
- Wunderlich, N.C.; Beigel, R.; Siegel, R.J. Management of Mitral Stenosis Using 2D and 3D Echo-Doppler Imaging. JACC Cardiovasc. Imaging 2013, 6, 1191–1205. [Google Scholar] [CrossRef] [Green Version]
- de Marchi, S.F.; Windecker, S.; Aeschbacher, B.C.; Seiler, C. Influence of Left Ventricular Relaxation on the Pressure Half Time of Aortic Regurgitation. Heart 1999, 82, 607–613. [Google Scholar] [CrossRef] [Green Version]
- Lancellotti, P.; Pibarot, P.; Chambers, J.; La Canna, G.; Pepi, M.; Dulgheru, R.; Dweck, M.; Delgado, V.; Garbi, M.; Vannan, M.A.; et al. Multi-Modality Imaging Assessment of Native Valvular Regurgitation: An EACVI and ESC Council of Valvular Heart Disease Position Paper. Eur. Heart J. Cardiovasc. Imaging 2022, 23, e171–e232. [Google Scholar] [CrossRef]
- Siani, A.; Perone, F.; Costantini, P.; Rodolfi, S.; Muscogiuri, G.; Sironi, S.; Carriero, S.; Pavon, A.G.; van der Bilt, I.; van Rosendael, P.; et al. Aortic Regurgitation: A Multimodality Approach. J. Clin. Ultrasound 2022, 50, 1041–1050. [Google Scholar] [CrossRef] [PubMed]
- Marwick, T.H.; Chandrashekhar, Y. Quantification and Selective Use of Multimodality Imaging in the Assessment of Valvular Regurgitation. JACC Cardiovasc. Imaging 2022, 15, 957–959. [Google Scholar] [CrossRef] [PubMed]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef]
- Vieitez, J.M.; Monteagudo, J.M.; Mahia, P.; Perez, L.; Lopez, T.; Marco, I.; Perone, F.; González, T.; Sitges, M.; Bouzas, A.; et al. New Insights of Tricuspid Regurgitation: A Large-Scale Prospective Cohort Study. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 196–202. [Google Scholar] [CrossRef]
- Cigarroa, R.G.; Lange, R.A.; Williams, R.H.; Bedotto, J.B.; Hillis, L.D. Underestimation of Cardiac Output by Thermodilution in Patients with Tricuspid Regurgitation. Am. J. Med. 1989, 86, 417–420. [Google Scholar] [CrossRef]
- Lancellotti, P.; Pellikka, P.A.; Budts, W.; Chaudhry, F.A.; Donal, E.; Dulgheru, R.; Edvardsen, T.; Garbi, M.; Ha, J.-W.; Kane, G.C.; et al. The Clinical Use of Stress Echocardiography in Non-Ischaemic Heart Disease: Recommendations from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 1191–1229. [Google Scholar] [CrossRef] [Green Version]
- Piérard, L.A.; Lancellotti, P. Stress Testing in Valve Disease. Heart 2007, 93, 766–772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gentry Iii, J.L.; Phelan, D.; Desai, M.Y.; Griffin, B.P. The Role of Stress Echocardiography in Valvular Heart Disease: A Current Appraisal. Cardiology 2017, 137, 137–150. [Google Scholar] [CrossRef]
- Pawade, T.; Sheth, T.; Guzzetti, E.; Dweck, M.R.; Clavel, M.-A. Why and How to Measure Aortic Valve Calcification in Patients with Aortic Stenosis. JACC Cardiovasc. Imaging 2019, 12, 1835–1848. [Google Scholar] [CrossRef]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]
- Clavel, M.-A.; Messika-Zeitoun, D.; Pibarot, P.; Aggarwal, S.R.; Malouf, J.; Araoz, P.A.; Michelena, H.I.; Cueff, C.; Larose, E.; Capoulade, R.; et al. The Complex Nature of Discordant Severe Calcified Aortic Valve Disease Grading: New Insights from Combined Doppler Echocardiographic and Computed Tomographic Study. J. Am. Coll. Cardiol. 2013, 62, 2329–2338. [Google Scholar] [CrossRef] [Green Version]
- Pawade, T.; Clavel, M.-A.; Tribouilloy, C.; Dreyfus, J.; Mathieu, T.; Tastet, L.; Renard, C.; Gun, M.; Jenkins, W.S.A.; Macron, L.; et al. Computed Tomography Aortic Valve Calcium Scoring in Patients with Aortic Stenosis. Circ. Cardiovasc. Imaging 2018, 11, e007146. [Google Scholar] [CrossRef] [Green Version]
- Clavel, M.-A.; Pibarot, P.; Messika-Zeitoun, D.; Capoulade, R.; Malouf, J.; Aggarval, S.; Araoz, P.A.; Michelena, H.I.; Cueff, C.; Larose, E.; et al. Impact of Aortic Valve Calcification, as Measured by MDCT, on Survival in Patients with Aortic Stenosis: Results of an International Registry Study. J. Am. Coll. Cardiol. 2014, 64, 1202–1213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tastet, L.; Enriquez-Sarano, M.; Capoulade, R.; Malouf, J.; Araoz, P.A.; Shen, M.; Michelena, H.I.; Larose, É.; Arsenault, M.; Bédard, É.; et al. Impact of Aortic Valve Calcification and Sex on Hemodynamic Progression and Clinical Outcomes in AS. J. Am. Coll. Cardiol. 2017, 69, 2096–2098. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.G.; Novaro, G.M.; Blandon, R.J.; Whiteman, M.S.; Asher, C.R.; Kirsch, J. Aortic Valve Area: Meta-Analysis of Diagnostic Performance of Multi-Detector Computed Tomography for Aortic Valve Area Measurements as Compared to Transthoracic Echocardiography. Int. J. Cardiovasc. Imaging 2009, 25, 601–609. [Google Scholar] [CrossRef]
- Cawley, P.J.; Maki, J.H.; Otto, C.M. Cardiovascular Magnetic Resonance Imaging for Valvular Heart Disease: Technique and Validation. Circulation 2009, 119, 468–478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woldendorp, K.; Bannon, P.G.; Grieve, S.M. Evaluation of Aortic Stenosis Using Cardiovascular Magnetic Resonance: A Systematic Review & Meta-Analysis. J. Cardiovasc. Magn. Reson. 2020, 22, 45. [Google Scholar] [CrossRef]
- Garcia, J.; Kadem, L.; Larose, E.; Clavel, M.-A.; Pibarot, P. Comparison between Cardiovascular Magnetic Resonance and Transthoracic Doppler Echocardiography for the Estimation of Effective Orifice Area in Aortic Stenosis. J. Cardiovasc. Magn. Reson. 2011, 13, 25. [Google Scholar] [CrossRef] [Green Version]
- Troger, F.; Lechner, I.; Reindl, M.; Tiller, C.; Holzknecht, M.; Pamminger, M.; Kremser, C.; Reinstadler, S.J.; Bauer, A.; Metzler, B.; et al. Aortic Stenosis Reexpanded—A Novel Approach to Determine Aortic Valve Area with Phase Contrast Cardiovascular Magnetic Resonance Imaging. Eur. Heart J. 2021, 42, 1600. [Google Scholar] [CrossRef]
- Ajmone Marsan, N.; Delgado, V.; Shah, D.J.; Pellikka, P.; Bax, J.J.; Treibel, T.; Cavalcante, J.L. Valvular Heart Disease: Shifting the Focus to the Myocardium. Eur. Heart J. 2023, 44, 28–40. [Google Scholar] [CrossRef]
- Debl, K.; Djavidani, B.; Buchner, S.; Lipke, C.; Nitz, W.; Feuerbach, S.; Riegger, G.; Luchner, A. Delayed Hyperenhancement in Magnetic Resonance Imaging of Left Ventricular Hypertrophy Caused by Aortic Stenosis and Hypertrophic Cardiomyopathy: Visualisation of Focal Fibrosis. Heart 2006, 92, 1447–1451. [Google Scholar] [CrossRef] [PubMed]
- Everett, R.J.; Tastet, L.; Clavel, M.-A.; Chin, C.W.L.; Capoulade, R.; Vassiliou, V.S.; Kwiecinski, J.; Gomez, M.; van Beek, E.J.R.; White, A.C.; et al. Progression of Hypertrophy and Myocardial Fibrosis in Aortic Stenosis: A Multicenter Cardiac Magnetic Resonance Study. Circ. Cardiovasc. Imaging 2018, 11, e007451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Treibel, T.A.; Kozor, R.; Schofield, R.; Benedetti, G.; Fontana, M.; Bhuva, A.N.; Sheikh, A.; López, B.; González, A.; Manisty, C.; et al. Reverse Myocardial Remodeling Following Valve Replacement in Patients with Aortic Stenosis. J. Am. Coll. Cardiol. 2018, 71, 860–871. [Google Scholar] [CrossRef]
- Everett, R.J.; Treibel, T.A.; Fukui, M.; Lee, H.; Rigolli, M.; Singh, A.; Bijsterveld, P.; Tastet, L.; Musa, T.A.; Dobson, L.; et al. Extracellular Myocardial Volume in Patients with Aortic Stenosis. J. Am. Coll. Cardiol. 2020, 75, 304–316. [Google Scholar] [CrossRef] [PubMed]
- Boskovski, M.T.; Gleason, T.G. Current Therapeutic Options in Aortic Stenosis. Circ. Res. 2021, 128, 1398–1417. [Google Scholar] [CrossRef]
- Writing Committee Members; Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2021, 77, e25–e197. [Google Scholar] [CrossRef]
- Lieberman, E.B.; Bashore, T.M.; Hermiller, J.B.; Wilson, J.S.; Pieper, K.S.; Keeler, G.P.; Pierce, C.H.; Kisslo, K.B.; Harrison, J.K.; Davidson, C.J. Balloon Aortic Valvuloplasty in Adults: Failure of Procedure to Improve Long-Term Survival. J. Am. Coll. Cardiol. 1995, 26, 1522–1528. [Google Scholar] [CrossRef] [Green Version]
- Ad, N.; Holmes, S.D.; Patel, J.; Pritchard, G.; Shuman, D.J.; Halpin, L. Comparison of EuroSCORE II, Original EuroSCORE, and The Society of Thoracic Surgeons Risk Score in Cardiac Surgery Patients. Ann. Thorac. Surg. 2016, 102, 573–579. [Google Scholar] [CrossRef] [Green Version]
- Nashef, S.A.M.; Roques, F.; Sharples, L.D.; Nilsson, J.; Smith, C.; Goldstone, A.R.; Lockowandt, U. EuroSCORE II. Eur. J. Cardiothorac. Surg. 2012, 41, 734–744. [Google Scholar] [CrossRef] [Green Version]
- Chang, C.; Raza, S.; Altarabsheh, S.E.; Delozier, S.; Sharma, U.M.; Zia, A.; Khan, M.S.; Neudecker, M.; Markowitz, A.H.; Sabik, J.F.; et al. Minimally Invasive Approaches to Surgical Aortic Valve Replacement: A Meta-Analysis. Ann. Thorac. Surg. 2018, 106, 1881–1889. [Google Scholar] [CrossRef]
- Furukawa, N.; Kuss, O.; Aboud, A.; Schönbrodt, M.; Renner, A.; Hakim Meibodi, K.; Becker, T.; Zittermann, A.; Gummert, J.F.; Börgermann, J. Ministernotomy versus Conventional Sternotomy for Aortic Valve Replacement: Matched Propensity Score Analysis of 808 Patients. Eur. J. Cardiothorac. Surg. 2014, 46, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Hammermeister, K.; Sethi, G.K.; Henderson, W.G.; Grover, F.L.; Oprian, C.; Rahimtoola, S.H. Outcomes 15 Years after Valve Replacement with a Mechanical versus a Bioprosthetic Valve: Final Report of the Veterans Affairs Randomized Trial. J. Am. Coll. Cardiol. 2000, 36, 1152–1158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puskas, J.; Gerdisch, M.; Nichols, D.; Quinn, R.; Anderson, C.; Rhenman, B.; Fermin, L.; McGrath, M.; Kong, B.; Hughes, C.; et al. Reduced Anticoagulation after Mechanical Aortic Valve Replacement: Interim Results from the Prospective Randomized on-X Valve Anticoagulation Clinical Trial Randomized Food and Drug Administration Investigational Device Exemption Trial. J. Thorac. Cardiovasc. Surg. 2014, 147, 1202–1210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jawitz, O.K.; Wang, T.Y.; Lopes, R.D.; Chavez, A.; Boyer, B.; Kim, H.; Anstrom, K.J.; Becker, R.C.; Blackstone, E.; Ruel, M.; et al. Rationale and Design of PROACT Xa: A Randomized, Multicenter, Open-Label, Clinical Trial to Evaluate the Efficacy and Safety of Apixaban versus Warfarin in Patients with a Mechanical On-X Aortic Heart Valve. Am. Heart J. 2020, 227, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Gabella, T.; Voisine, P.; Puri, R.; Pibarot, P.; Rodés-Cabau, J. Aortic Bioprosthetic Valve Durability: Incidence, Mechanisms, Predictors, and Management of Surgical and Transcatheter Valve Degeneration. J. Am. Coll. Cardiol. 2017, 70, 1013–1028. [Google Scholar] [CrossRef]
- Unger, P.; Tribouilloy, C. Aortic Stenosis with Other Concomitant Valvular Disease: Aortic Regurgitation, Mitral Regurgitation, Mitral Stenosis, or Tricuspid Regurgitation. Cardiol. Clin. 2020, 38, 33–46. [Google Scholar] [CrossRef]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1695–1705. [Google Scholar] [CrossRef]
- Popma, J.J.; Deeb, G.M.; Yakubov, S.J.; Mumtaz, M.; Gada, H.; O’Hair, D.; Bajwa, T.; Heiser, J.C.; Merhi, W.; Kleiman, N.S.; et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1706–1715. [Google Scholar] [CrossRef]
- Ferlini, M.; Fortuni, F.; Di Giacomo, C.; Cornara, S.; Somaschini, A.; Oltrona Visconti, L.; Ferrario, M. Transcatheter Aortic Valve Replacement versus Surgery in Low-Risk Patients: A Meta-Analysis of Randomized Studies. J. Cardiovasc. Med. 2020, 21, 168–170. [Google Scholar] [CrossRef]
- Leon, M.B.; Smith, C.R.; Mack, M.J.; Makkar, R.R.; Svensson, L.G.; Kodali, S.K.; Thourani, V.H.; Tuzcu, E.M.; Miller, D.C.; Herrmann, H.C.; et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2016, 374, 1609–1620. [Google Scholar] [CrossRef]
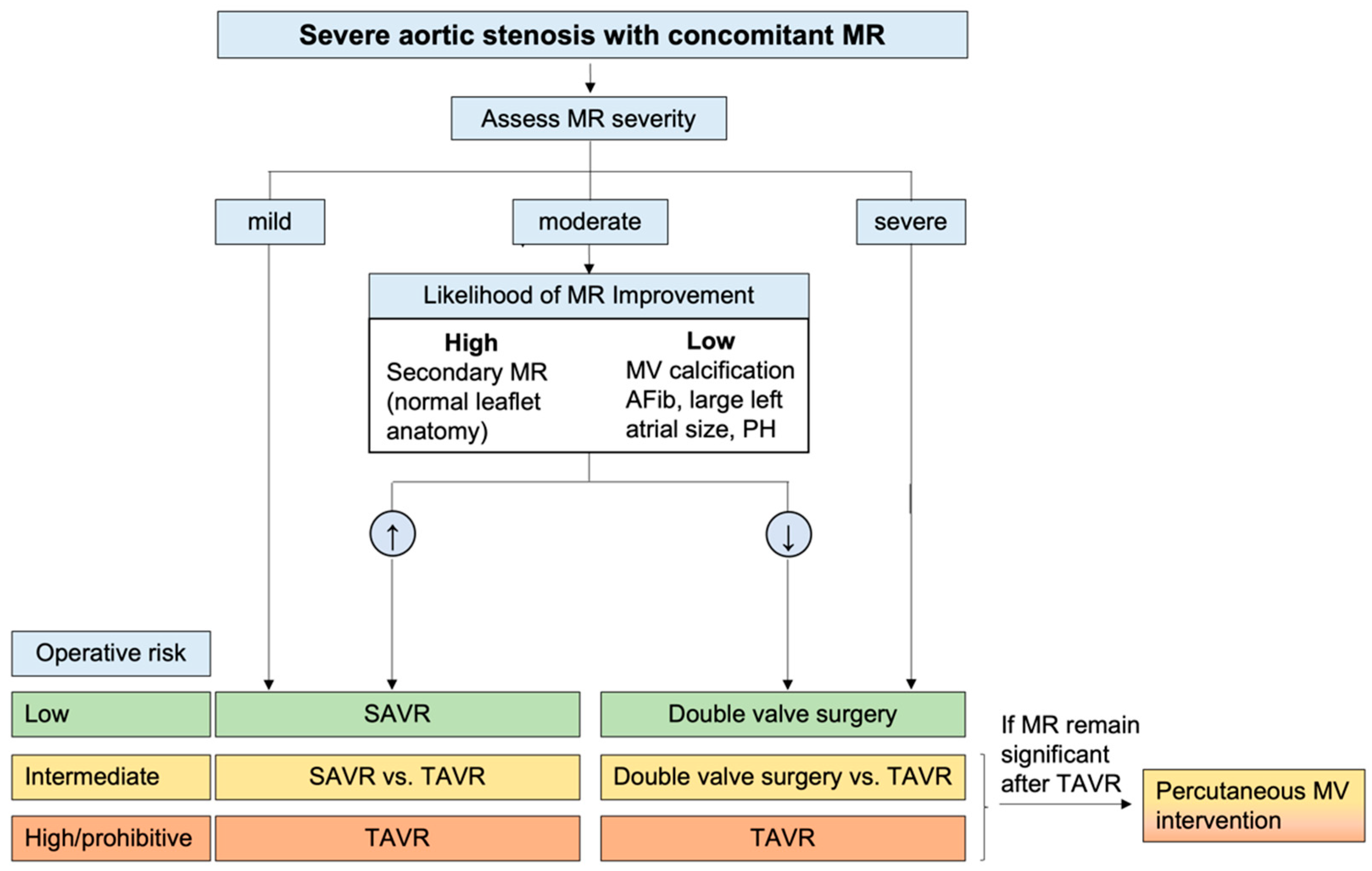
- Sannino, A.; Grayburn, P.A. Mitral Regurgitation in Patients with Severe Aortic Stenosis: Diagnosis and Management. Heart 2018, 104, 16–22. [Google Scholar] [CrossRef]
- Nombela-Franco, L.; Ribeiro, H.B.; Urena, M.; Allende, R.; Amat-Santos, I.; DeLarochellière, R.; Dumont, E.; Doyle, D.; DeLarochellière, H.; Laflamme, J.; et al. Significant Mitral Regurgitation Left Untreated at the Time of Aortic Valve Replacement. J. Am. Coll. Cardiol. 2014, 63, 2643–2658. [Google Scholar] [CrossRef] [Green Version]
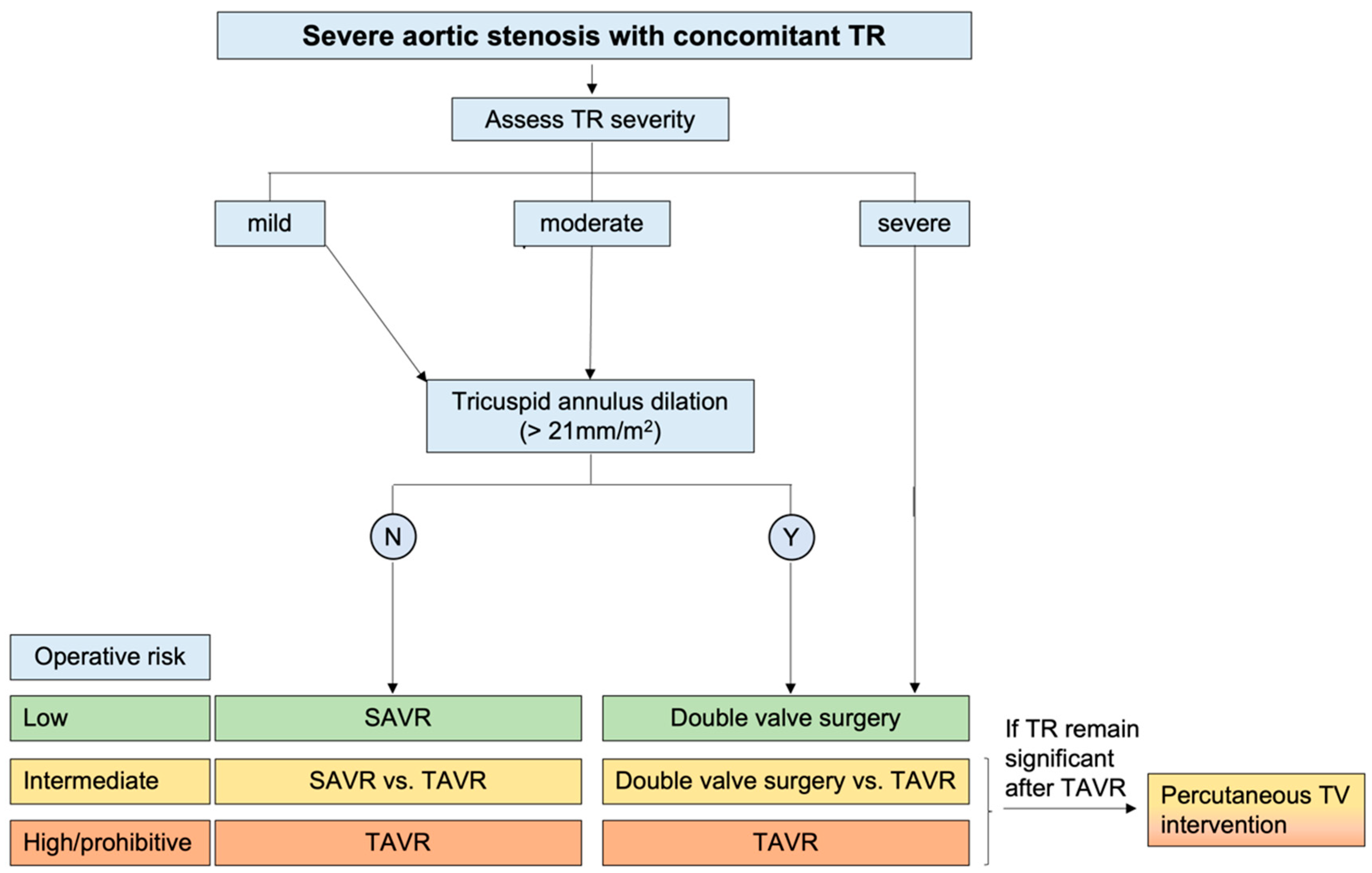
- Lindman, B.R.; Maniar, H.S.; Jaber, W.A.; Lerakis, S.; Mack, M.J.; Suri, R.M.; Thourani, V.H.; Babaliaros, V.; Kereiakes, D.J.; Whisenant, B.; et al. Effect of Tricuspid Regurgitation and the Right Heart on Survival after Transcatheter Aortic Valve Replacement: Insights from the Placement of Aortic Transcatheter Valves II Inoperable Cohort. Circ. Cardiovasc. Interv. 2015, 8, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dumont, C.; Galli, E.; Oger, E.; Fournet, M.; Flecher, E.; Leclercq, C.; Verhoye, J.-P.; Donal, E. Pre- and Postoperative Tricuspid Regurgitation in Patients with Severe Symptomatic Aortic Stenosis: Importance of Pre-Operative Tricuspid Annulus Diameter. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Kiriyama, H.; Daimon, M. Is Concomitant Mitral Regurgitation with Severe Aortic Stenosis Benign or Malignant? Circ. J. 2022, 86, 438–439. [Google Scholar] [CrossRef]
- Unger, P.; Clavel, M.A.; Lindman, B.R.; Mathieu, P.; Pibarot, P. Pathophysiology and Management of Multivalvular Disease. Nat. Rev. Cardiol. 2016, 13, 429–440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, D.J. 4D Flow CMR: The Final Frontier in Valvular Heart Disease? JACC Cardiovasc. Imaging 2021, 14, 1367–1368. [Google Scholar] [CrossRef]


| SAVR | TAVR |
|---|---|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bombace, S.; Meucci, M.C.; Fortuni, F.; Ilardi, F.; Manzo, R.; Canciello, G.; Esposito, G.; Grayburn, P.A.; Losi, M.A.; Sannino, A. Beyond Aortic Stenosis: Addressing the Challenges of Multivalvular Disease Assessment. Diagnostics 2023, 13, 2102. https://doi.org/10.3390/diagnostics13122102
Bombace S, Meucci MC, Fortuni F, Ilardi F, Manzo R, Canciello G, Esposito G, Grayburn PA, Losi MA, Sannino A. Beyond Aortic Stenosis: Addressing the Challenges of Multivalvular Disease Assessment. Diagnostics. 2023; 13(12):2102. https://doi.org/10.3390/diagnostics13122102
Chicago/Turabian StyleBombace, Sara, Maria Chiara Meucci, Federico Fortuni, Federica Ilardi, Rachele Manzo, Grazia Canciello, Giovanni Esposito, Paul A. Grayburn, Maria Angela Losi, and Anna Sannino. 2023. "Beyond Aortic Stenosis: Addressing the Challenges of Multivalvular Disease Assessment" Diagnostics 13, no. 12: 2102. https://doi.org/10.3390/diagnostics13122102






