A Preliminary Diagnostic Model for Forward Head Posture among Adolescents Using Forward Neck Tilt Angle and Radiographic Sagittal Alignment Parameters
Abstract
:1. Introduction
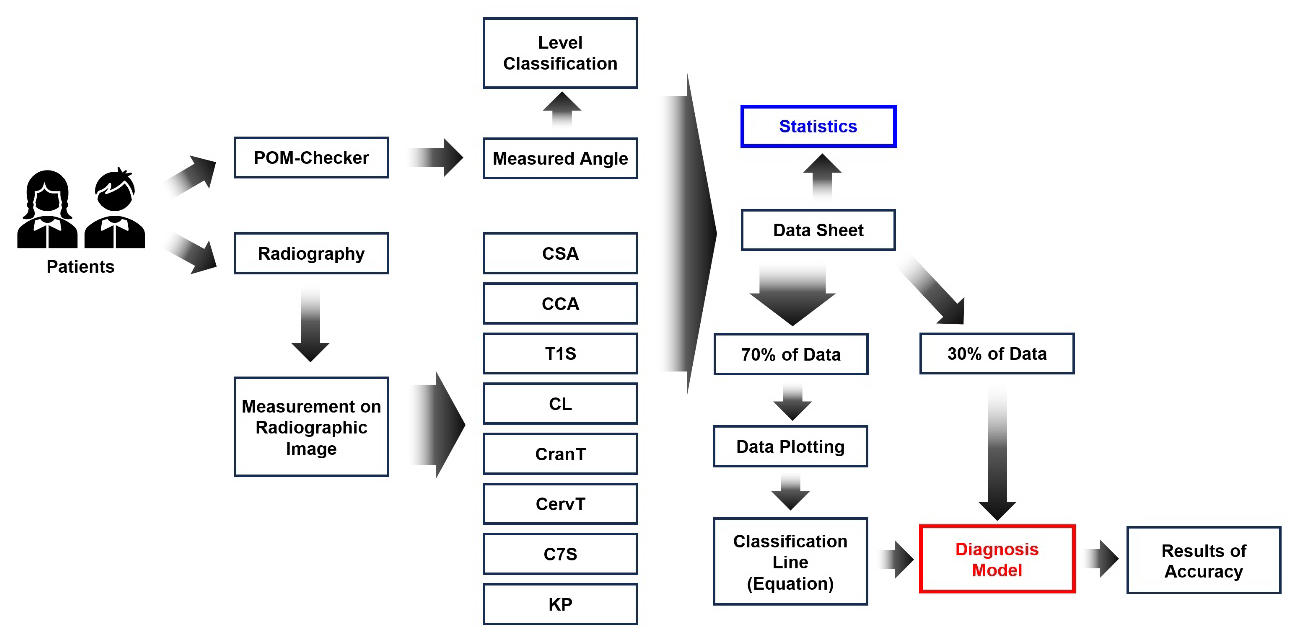
2. Materials and Methods
2.1. Ethics Approval and Consent to Participate
2.2. Forward Neck Tilt Angle Measurement Using a Depth-Based Body Angle Measurement System
2.3. Radiographic Measurements
2.4. Statistical Analysis
2.5. Establishment of a Preliminary Diagnostic Model for FHP
2.6. Accuracy Evaluation for Diagnostic Model
3. Results
3.1. Statistical Results
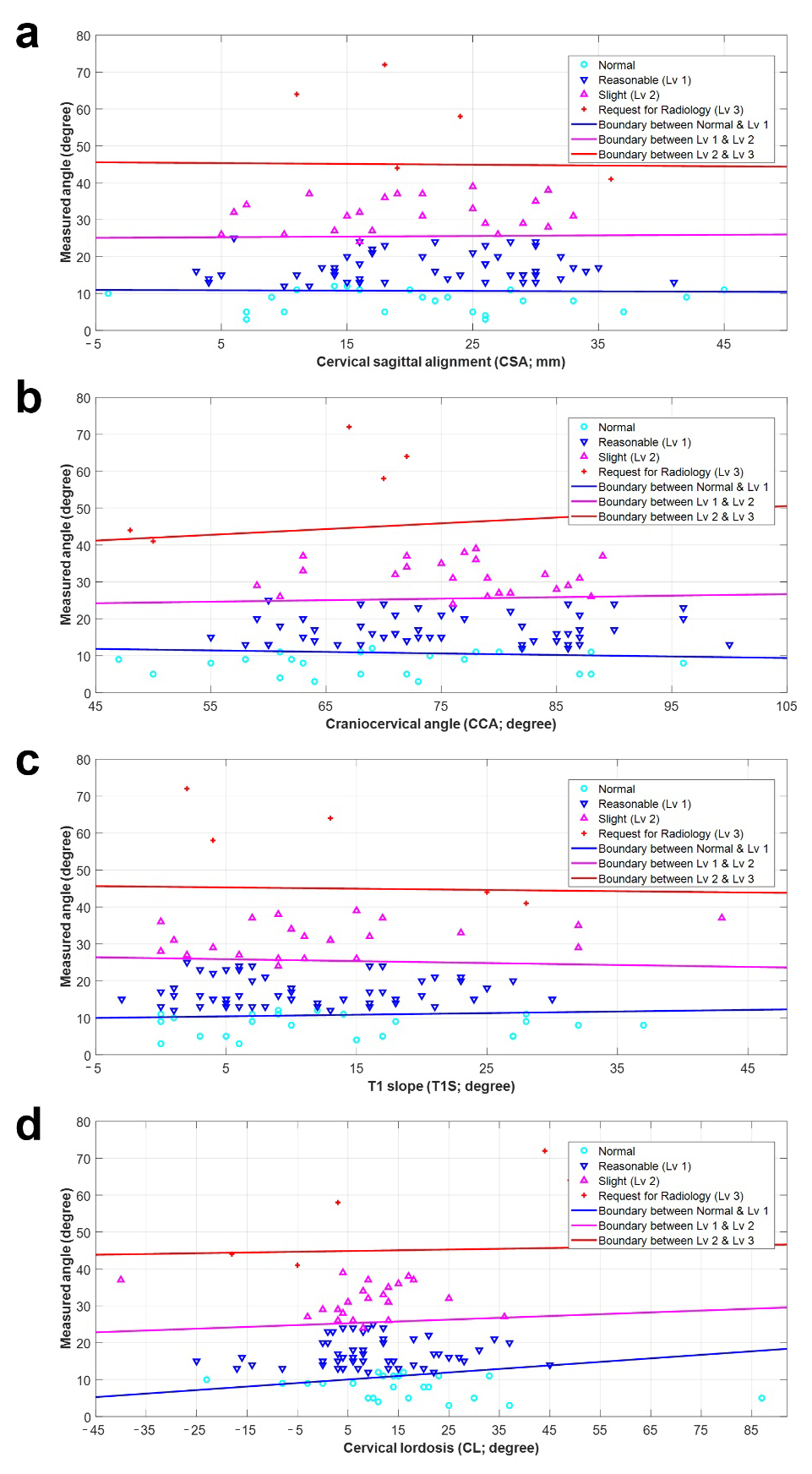
3.2. Preliminary Diagnostic Model for FHP
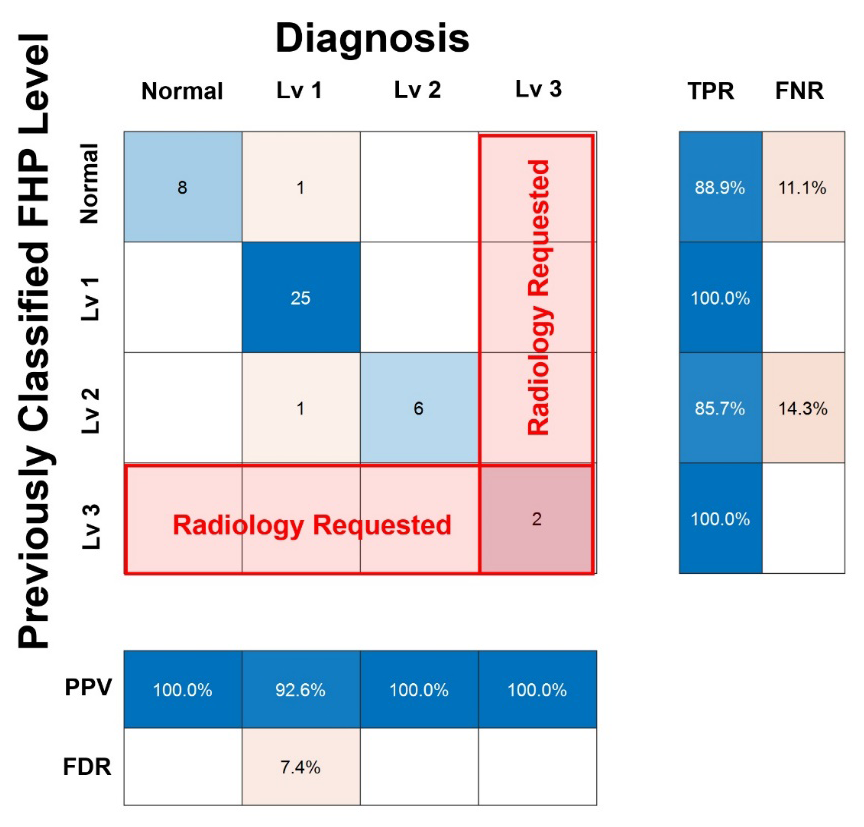
3.3. Accuracy of the Preliminary Diagnostic Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fischer-Grote, L.; Kothgassner, O.D.; Felnhofer, A. The impact of problematic smartphone use on children’s and adolescents’ quality of life: A systematic review. Acta Paediatr. 2021, 110, 1417–1424. [Google Scholar] [CrossRef] [PubMed]
- Toh, S.H.; Coenen, P.; Howie, E.K.; Smith, A.J.; Mukherjee, S.; Mackey, D.A.; Straker, L.M. A prospective longitudinal study of mobile touch screen device use and musculoskeletal symptoms and visual health in adolescents. Appl. Ergon. 2020, 85, 103028. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, E.; Thomée, S.; Grimby-Ekman, A.; Hagberg, M. Texting on mobile phones and musculoskeletal disorders in young adults: A five-year cohort study. Appl. Ergon. 2017, 58, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Betsch, M.; Kalbhen, K.; Michalik, R.; Schenker, H.; Gatz, M.; Quack, V.; Siebers, H.; Wild, M.; Migliorini, F. The influence of smartphone use on spinal posture—A laboratory study. Gait Posture 2021, 85, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kang, H.; Shin, G. Head flexion angle while using a smartphone. Ergonomics 2015, 58, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Hansraj, K.K. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg. Technol. Int. 2014, 25, 277–279. [Google Scholar] [PubMed]
- Okada, E.; Matsumoto, M.; Ichihara, D.; Chiba, K.; Toyama, Y.; Fujiwara, H.; Momoshima, S.; Nishiwaki, Y.; Hashimoto, T.; Ogawa, J.; et al. Does the sagittal alignment of the cervical spine have an impact on disk degeneration? Minimum 10-year follow-up of asymptomatic volunteers. Eur. Spine J. 2009, 18, 1644–1651. [Google Scholar] [CrossRef] [PubMed]
- Dolphens, M.; Cagnie, B.; Coorevits, P.; Vanderstraeten, G.; Cardon, G.; D’hooge, R.; Danneels, L. Sagittal standing posture and its association with spinal pain: A school-based epidemiological study of 1196 Flemish adolescents before age at peak height velocity. Spine (Phila Pa 1976) 2012, 37, 1657–1666. [Google Scholar] [CrossRef]
- Chu, H.; Joo, S.; Kim, J.; Kim, J.K.; Kim, C.; Seo, J.; Kang, D.G.; Lee, H.S.; Sung, K.K.; Lee, S. Validity and reliability of POM-Checker in measuring shoulder range of motion: Protocol for a single center comparative study. Medicine (Baltim) 2018, 97, e11082. [Google Scholar] [CrossRef] [PubMed]
- Dang, N.R.; Moreau, M.J.; Hill, D.L.; Mahood, J.K.; Raso, J. Intra-observer reproducibility and interobserver reliability of the radiographic parameters in the Spinal Deformity Study Group’s AIS Radiographic Measurement Manual. Spine (Phila Pa 1976) 2005, 30, 1064–1069. [Google Scholar] [CrossRef] [PubMed]
- Marques, C.; Granström, E.; MacDowall, A.; Moreira, N.C.; Skeppholm, M.; Olerud, C. Accuracy and reliability of X-ray measurements in the cervical spine. Asian Spine J. 2020, 14, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Alijani, B.; Rasoulian, J. The sagittal balance of the cervical spine: Radiographic analysis of interdependence between the occipitocervical and spinopelvic alignment. Asian Spine J. 2020, 14, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The relationship between forward head posture and neck pain: A systematic review and meta-analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef] [PubMed]
- Richards, K.V.; Beales, D.J.; Smith, A.J.; O’Sullivan, P.B.; Straker, L.M. Neck posture clusters and their association with biopsychosocial factors and neck pain in Australian adolescents. Phys. Ther. 2016, 96, 1576–1587. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.C.; Silva, A.G. Neck muscle endurance and head posture: A comparison between adolescents with and without neck pain. Man. Ther. 2016, 22, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Joy, T.E.; Tanuja, S.; Pillai, R.R.; Dhas Manchil, P.R.; Raveendranathan, R. Assessment of craniocervical posture in TMJ disorders using lateral radiographic view: A cross-sectional study. Cranio 2021, 39, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Bueno, C.H.; Pereira, D.D.; Pattussi, M.P.; Grossi, P.K.; Grossi, M.L. Gender differences in temporomandibular disorders in adult populational studies: A systematic review and meta-analysis. J. Oral. Rehabil. 2018, 45, 720–729. [Google Scholar] [CrossRef] [PubMed]
- Sheikhhoseini, R.; Shahrbanian, S.; Sayyadi, P.; O’Sullivan, K. Effectiveness of therapeutic exercise on forward head posture: A systematic review and meta-analysis. J. Manip. Physiol. Ther. 2018, 41, 530–539. [Google Scholar] [CrossRef] [PubMed]
- Diab, A.A. The role of forward head correction in management of adolescent idiopathic scoliotic patients: A randomized controlled trial. Clin. Rehabil. 2012, 26, 1123–1132. [Google Scholar] [CrossRef] [PubMed]
- Cil, A.; Yazici, M.; Uzumcugil, A.; Kandemir, U.; Alanay, A.; Alanay, Y.; Acaroglu, R.E.; Surat, A. The evolution of sagittal segmental alignment of the spine during childhood. Spine (Phila Pa 1976) 2005, 30, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Hey, H.W.D.; Lau, E.T.; Wong, G.C.; Tan, K.A.; Liu, G.K.; Wong, H.K. Cervical alignment variations in different postures and predictors of normal cervical kyphosis: A new understanding. Spine (Phila Pa 1976) 2017, 42, 1614–1621. [Google Scholar] [CrossRef] [PubMed]
- Ling, F.P.; Chevillotte, T.; Leglise, A.; Thompson, W.; Bouthors, C.; Le Huec, J.C. Which parameters are relevant in sagittal balance analysis of the cervical spine? A literature review. Eur. Spine J. 2018, 27 (Suppl. S1), 8–15. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Qin, S.; Li, Y.; Shen, Y. Modic changes of the cervical spine: T1 slope and its impact on axial neck pain. J. Pain Res. 2017, 10, 2041–2045. [Google Scholar] [CrossRef] [PubMed]
- Kitiş, S.; Çevik, S.; Kaplan, A.; Yılmaz, H.; Katar, S.; Cömert, S.; Ünsal, Ü.Ü. Relationship Between Degeneration or Sagittal Balance with Modic Changes in the Cervical Spine. Cureus 2021, 13, e12949. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.F.; Szeto, G.; Madeleine, P.; Tsang, S. Spinal kinematics during smartphone texting—A comparison between young adults with and without chronic neck-shoulder pain. Appl. Ergon. 2018, 68, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Abelin-Genevois, K.; Idjerouidene, A.; Roussouly, P.; Vital, J.M.; Garin, C. Cervical spine alignment in the pediatric population: A radiographic normative study of 150 asymptomatic patients. Eur. Spine J. 2014, 23, 1442–1448. [Google Scholar] [CrossRef] [PubMed]
- Mac-Thiong, J.M.; Berthonnaud, E.; Dimar, J.R., 2nd; Betz, R.R.; Labelle, H. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976) 2004, 29, 1642–1647. [Google Scholar] [CrossRef] [PubMed]
- Sarig Bahat, H.; Levy, A.; Yona, T. The association between forward head posture and non-specific neck pain: A cross-sectional study. Physiother. Theory Pract. 2023, 39, 1736–1745. [Google Scholar] [CrossRef] [PubMed]
- Chu, E.C.; Lo, F.S.; Bhaumik, A. Plausible impact of forward head posture on upper cervical spine stability. J. Family Med. Prim. Care 2020, 9, 2517–2520. [Google Scholar] [CrossRef] [PubMed]


| N * (p) | S * (FNTA) | p | P * (FNTA) | p | S * (FHP Lv) | p | P * (FHP Lv) | p | |
|---|---|---|---|---|---|---|---|---|---|
| CSA | 0.6031 | 0.00 | 0.9781 | 0.00 | 0.9779 | −0.06 | 0.4921 | −0.02 | 0.7805 |
| CCA | 0.6798 | −0.02 | 0.8047 | −0.06 | 0.4660 | −0.08 | 0.3223 | −0.10 | 0.2256 |
| T1S | 0.1063 | 0.11 | 0.1753 | 0.07 | 0.4306 | 0.04 | 0.6702 | 0.02 | 0.8409 |
| CL | 0.0638 | 0.13 | 0.1200 | 0.02 | 0.8125 | 0.07 | 0.4219 | −0.01 | 0.9435 |
| CranT | 0.0848 | 0.02 | 0.8215 | 0.01 | 0.9335 | 0.03 | 0.7216 | 0.01 | 0.8637 |
| CervT | 0.1379 | −0.11 | 0.1702 | 0.01 | 0.9479 | −0.11 | 0.2065 | −0.01 | 0.9375 |
| C7S | 0.9129 | 0.16 | 0.0500 | 0.14 | 0.0890 | 0.11 | 0.1711 | 0.12 | 0.1584 |
| TK | 0.2849 | −0.11 | 0.1801 | −0.04 | 0.6374 | −0.09 | 0.2582 | −0.05 | 0.5832 |
| N * | L1 * | L2 * | L3 * † | |
|---|---|---|---|---|
| Age | 13.91 ± 2.04 | 13.93 ± 2.17 | 13.45 ± 1.68 | 13.14 ± 2.12 |
| CSA | 19.61 ± 10.62 | 19.20 ± 10.38 | 19.62 ± 7.76 | 22.14 ± 9.75 |
| CCA | 71.64 ± 12.18 | 76.25 ± 11.19 | 76.55 ± 8.50 | 64.86 ± 13.55 |
| T1S | 12.88 ± 10.12 | 10.67 ± 8.09 | 13.76 ± 10.51 | 13.00 ± 11.37 |
| CL | 14.18 ± 17.67 | 10.11 ± 13.46 | 8.07 ± 13.44 | 16.71 ± 26.32 |
| CranT | 6.03 ± 7.51 | 5.76 ± 5.82 | 5.97 ± 4.72 | 12.29 ± 7.48 |
| CervT | 7.64 ± 7.88 | 6.08 ± 7.75 | 7.76 ± 9.22 | 3.43 ± 7.57 |
| C7S | 14.03 ± 9.93 | 12.72 ± 7.97 | 16.03 ± 10.58 | 14.71 ± 12.65 |
| TK | 18.45 ± 10.16 | 16.59 ± 10.21 | 20.72 ± 10.74 | 17.43 ± 15.02 |
| FNTA | 8.61 ± 5.04 | 17.25 ± 3.82 | 31.24 ± 4.36 | 54.71 ± 12.34 |
| Color | K | L1 | L2 | LE | RE | IA | EA | |
|---|---|---|---|---|---|---|---|---|
| CSA | Blue(B) | 4.7059 | −0.0041 | −0.4309 | −5 | 50 | 11.0 | 10.4 |
| Pink(P) | 17.0615 | 0.0112 | −0.6780 | −5 | 50 | 25.1 | 26.0 | |
| Red(R) | 52.0386 | −0.0249 | −1.1452 | −5 | 50 | 45.5 | 44.4 | |
| CCA | B | 5.8290 | −0.0175 | −0.4254 | 45 | 105 | 11.9 | 9.4 |
| P | 15.3719 | 0.0281 | −0.6869 | 45 | 105 | 24.2 | 26.7 | |
| R | 41.0884 | 0.1879 | −1.2028 | 45 | 105 | 41.2 | 50.6 | |
| T1S | B | 4.3672 | 0.0187 | −0.4290 | −5 | 48 | 10.0 | 12.3 |
| P | 17.8022 | −0.0355 | −0.6815 | −5 | 48 | 26.4 | 23.6 | |
| R | 52.2012 | −0.0393 | −1.1483 | −5 | 48 | 45.6 | 43.8 | |
| CL | B | 4.3264 | 0.0432 | −0.4527 | −45 | 92 | 5.30 | 18.3 |
| P | 17.4075 | 0.0341 | −0.6955 | −45 | 92 | 22.8 | 29.5 | |
| R | 51.7508 | 0.0232 | −1.1564 | −45 | 92 | 43.8 | 46.6 | |
| CranT | B | 4.7627 | −0.0175 | −0.4333 | −15 | 35 | 11.6 | 9.6 |
| P | 17.7856 | −0.0508 | −0.6855 | −15 | 35 | 27.1 | 23.4 | |
| R | 54.5616 | −0.2062 | −1.1743 | −15 | 35 | 49.1 | 40.3 | |
| CervT | B | 4.4493 | 0.0301 | −0.4330 | −25 | 50 | 8.5 | 13.8 |
| P | 17.3439 | −0.0097 | −0.6775 | −25 | 50 | 26.0 | 24.9 | |
| R | 51.4267 | 0.1307 | −1.1542 | −25 | 50 | 41.7 | 50.2 | |
| C7S | B | 4.4401 | 0.0147 | −0.4315 | −25 | 54 | 9.4 | 12.1 |
| P | 17.5074 | −0.0172 | −0.6774 | −25 | 54 | 26.5 | 24.5 | |
| R | 50.9228 | 0.0547 | −1.1472 | −25 | 54 | 43.2 | 47.0 | |
| TK | B | 5.2067 | −0.0249 | −0.4419 | −5 | 56 | 12.1 | 8.6 |
| P | 19.4449 | −0.0732 | −0.7108 | −5 | 56 | 27.9 | 21.6 | |
| R | 55.2256 | −0.0951 | −1.1870 | −5 | 56 | 46.9 | 42.0 |
| FNTA | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | N | L1 | L2 | L3 | PC | D | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 13 | 1 | 1 | 1 | 0.1 | 1 | 0.1 | 1 | 1 | 2 | 8 | 0 | 0 | 1 | 1 |
| 2 | 15 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 3 | 17 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 4 | 17 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 5 | 12 | 1 | 1 | 0.1 | 0.1 | 1 | 0.1 | 0.1 | 0.1 | 5 | 8 | 0 | 0 | 1 | 1 |
| 6 | 21 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 7 | 21 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 8 | 11 | 1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 7 | 8 | 0 | 0 | 0 | 1 |
| 9 | 33 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 8 | 0 | 2 | 2 |
| 10 | 31 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 8 | 0 | 2 | 2 |
| 11 | 23 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1.2 | 0 | 8 | 1 | 0 | 1 | 1 |
| 12 | 17 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | 8 | 0 | 0 | 1 | 1 |
| 13 | 10 | 0 | 0.1 | 0 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 8 | 6 | 0 | 0 | 0 | 0 |
| 14 | 23 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1.2 | 0 | 8 | 1 | 0 | 1 | 1 |
| 15 | 15 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 16 | 36 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 8 | 0 | 2 | 2 |
| 17 | 23 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1.2 | 0 | 8 | 1 | 0 | 1 | 1 |
| 18 | 29 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 8 | 0 | 2 | 2 |
| 19 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 0 | 0 |
| 20 | 16 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 21 | 13 | 1 | 1 | 1 | 0.1 | 1 | 0.1 | 1 | 1 | 2 | 8 | 0 | 0 | 1 | 1 |
| 22 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 0 | 0 |
| 23 | 17 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 24 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 0 | 0 |
| 25 | 25 | 1 | 1.2 | 1.2 | 1.2 | 1.2 | 1.2 | 1.2 | 1.2 | 0 | 8 | 7 | 0 | 2 | 1 |
| 26 | 27 | 2 | 2 | 2 | 1.2 | 1.2 | 2 | 2 | 1.2 | 0 | 3 | 8 | 0 | 2 | 2 |
| 27 | 31 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 8 | 0 | 2 | 2 |
| 28 | 12 | 1 | 1 | 0.1 | 0.1 | 1 | 0.1 | 0.1 | 0.1 | 5 | 8 | 0 | 0 | 1 | 1 |
| 29 | 52 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 0 | 0 | 0 | 8 | 3 | 3 |
| 30 | 13 | 1 | 1 | 1 | 0.1 | 1 | 0.1 | 1 | 1 | 2 | 8 | 0 | 0 | 1 | 1 |
| 31 | 20 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 32 | 7 | 0 | 0 | 0 | 0.1 | 0 | 0 | 0 | 0 | 8 | 1 | 0 | 0 | 0 | 0 |
| 33 | 15 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 34 | 19 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 35 | 9 | 0 | 0 | 0 | 0.1 | 0 | 0.1 | 0 | 0.1 | 8 | 3 | 0 | 0 | 0 | 0 |
| 36 | 13 | 1 | 1 | 1 | 0.1 | 1 | 0.1 | 1 | 1 | 2 | 8 | 0 | 0 | 1 | 1 |
| 37 | 19 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 38 | 21 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 39 | 21 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | 0 | 0 | 1 | 1 |
| 40 | 22 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1.2 | 0 | 8 | 1 | 0 | 1 | 1 |
| 41 | 10 | 0 | 0.1 | 0 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 8 | 6 | 0 | 0 | 0 | 0 |
| 42 | 62 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 0 | 0 | 0 | 8 | 3 | 3 |
| 43 | 10 | 0 | 0.1 | 0 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 8 | 6 | 0 | 0 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moon, Y.J.; Ahn, T.Y.; Suh, S.W.; Park, K.-B.; Chang, S.Y.; Yoon, D.-K.; Kim, M.-S.; Kim, H.; Jeon, Y.D.; Yang, J.H. A Preliminary Diagnostic Model for Forward Head Posture among Adolescents Using Forward Neck Tilt Angle and Radiographic Sagittal Alignment Parameters. Diagnostics 2024, 14, 394. https://doi.org/10.3390/diagnostics14040394
Moon YJ, Ahn TY, Suh SW, Park K-B, Chang SY, Yoon D-K, Kim M-S, Kim H, Jeon YD, Yang JH. A Preliminary Diagnostic Model for Forward Head Posture among Adolescents Using Forward Neck Tilt Angle and Radiographic Sagittal Alignment Parameters. Diagnostics. 2024; 14(4):394. https://doi.org/10.3390/diagnostics14040394
Chicago/Turabian StyleMoon, Young Jae, Tae Young Ahn, Seung Woo Suh, Kun-Bo Park, Sam Yeol Chang, Do-Kun Yoon, Moo-Sub Kim, Hyeonjoo Kim, Yong Dae Jeon, and Jae Hyuk Yang. 2024. "A Preliminary Diagnostic Model for Forward Head Posture among Adolescents Using Forward Neck Tilt Angle and Radiographic Sagittal Alignment Parameters" Diagnostics 14, no. 4: 394. https://doi.org/10.3390/diagnostics14040394






