Salivary Immune and Metabolic Marker Analysis (SIMMA): A Diagnostic Test to Predict Caries Risk
Abstract
:1. Introduction
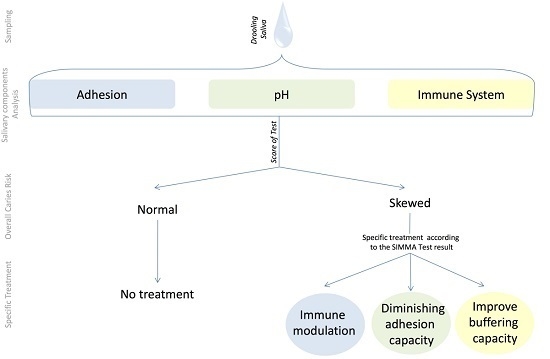
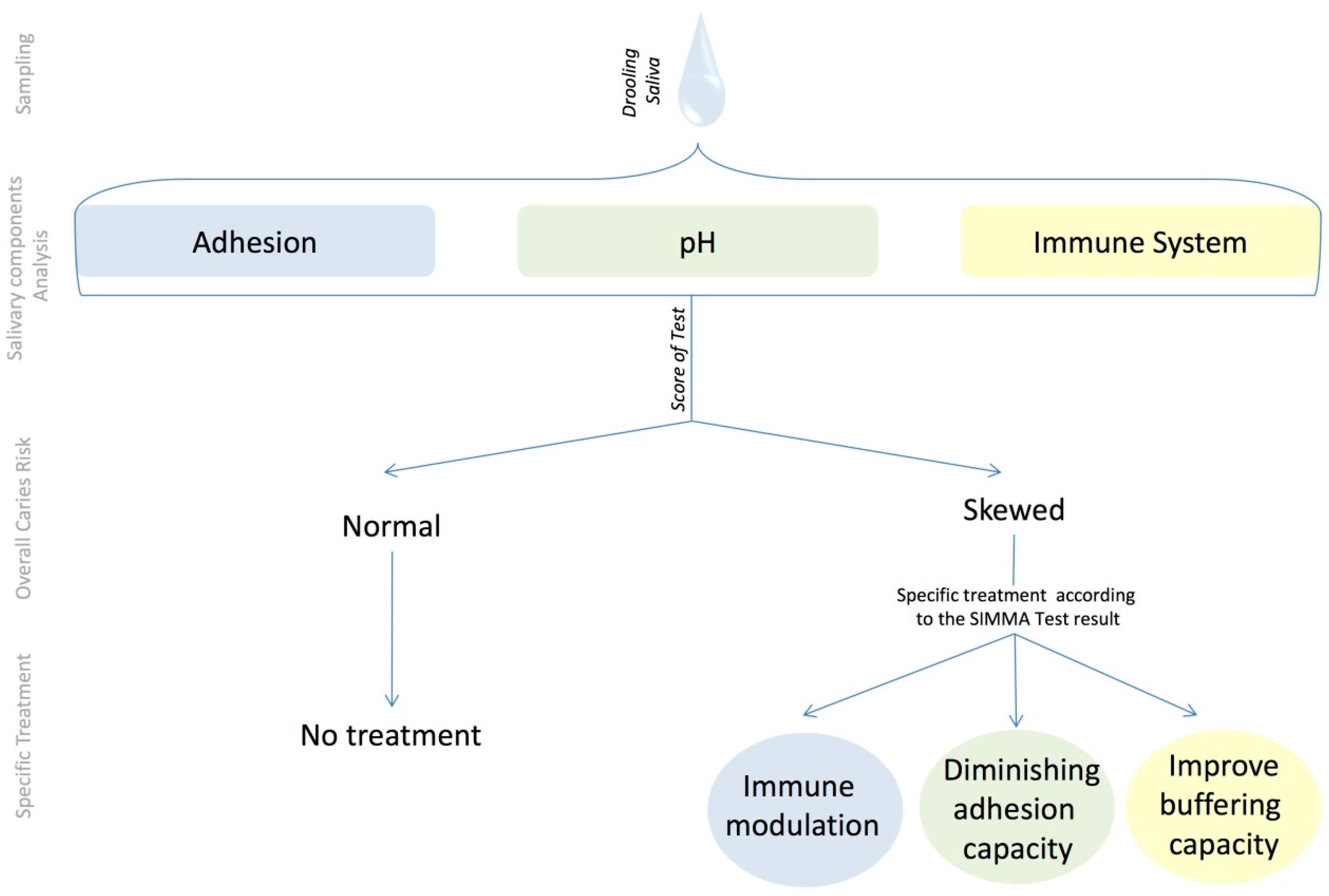
- Molecules related to the Immune System. These include immunoglobulins, antimicrobial peptides, and proteins of the component system, which constitute a protection barrier against oral pathogens [22].
- Molecules related to the adhesion capacity of micro-organisms. These include structural components of saliva that microorganisms use as targets for sticking to the tooth and forming the dental plaque [23].
- Molecules related to the acidity of saliva and plaque. These include enzymes that metabolize sugars, acidic compounds that are produced as a consequence of sugar fermentation, and those salivary components that can act as acid neutralizers [24].
2. Materials and Methods
2.1. Donor Selection and Sampling Procedure
2.2. Quantification of Salivary Immune Components
2.3. Statistical Analysis
3. Results
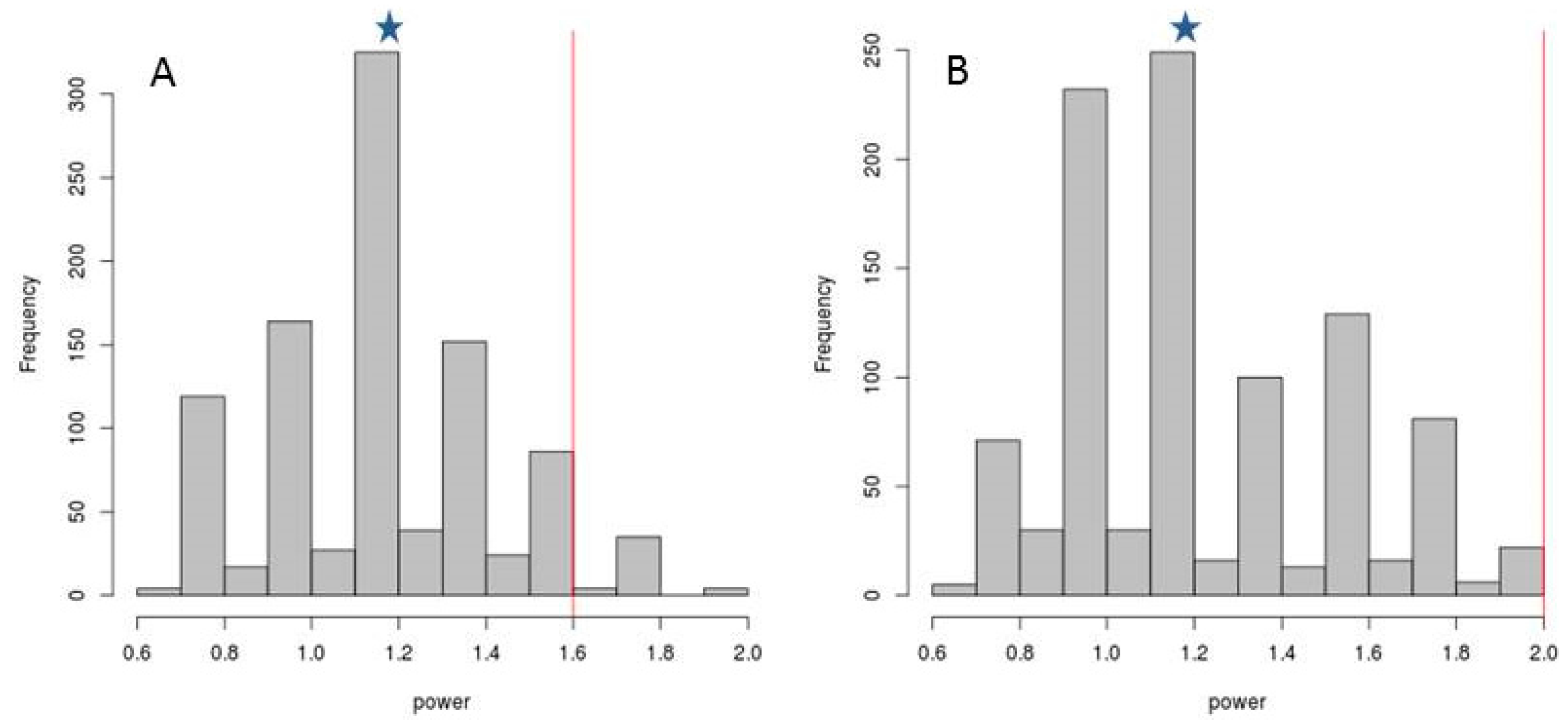
3.1. Selection of Sampling Time
3.2. Selection of Caries-Associated Biomarkers
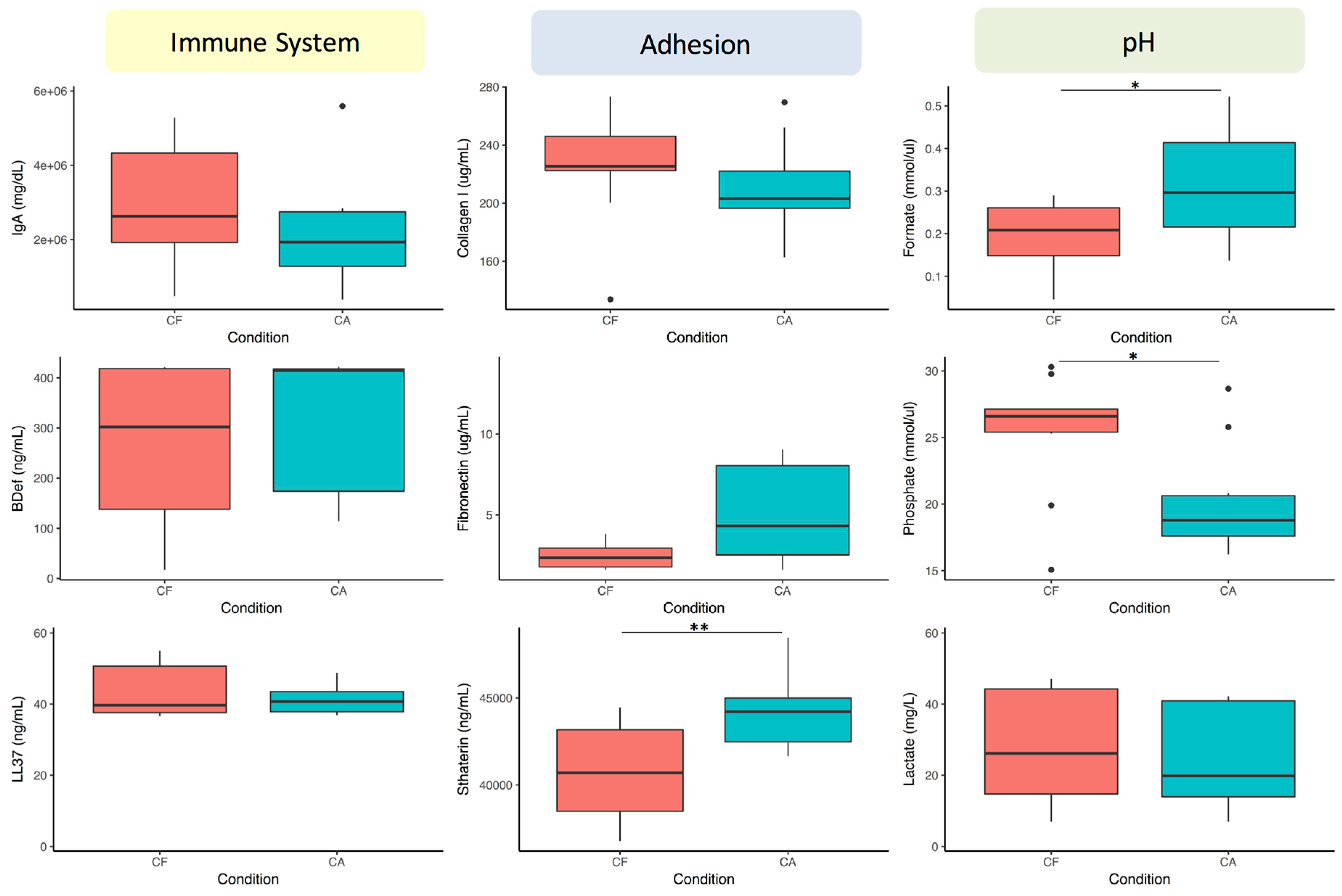
- At 6 h:
- Immune molecules: β-defensin 2 and LL-37.
- Adhesion molecules: Collagen I and Fibronectin.
- pH components: Formate and Phosphate.
- At 0.5 h:
- Immune molecules: LL-37 and IgA.
- Adhesion molecules: Statherin and Fibronectin (Statherin only if saliva is collected after a sugary solution rinse).
- pH components: Phosphate and Lactate (Phosphate and Formate if saliva is collected after a sugary solution rinse).
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Petersen, P.E. Challenges to improvement of oral health in the 21st century—The approach of the WHO Global Oral Health Programme. Int. Dent. J. 2004, 54, 329–343. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, N.; Nyvad, B. The Role of Bacteria in the Caries Process: Ecological Perspectives. J. Dent. Res. 2011, 90, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Keyes, P.H.; Jordan, H.V. Factors influencing initiation, transmission and inhibition of dental caries. In Mechanisms of Hard Tissue Destruction; Harris, R.J., Ed.; Academic Press: New York, NY, USA, 1963; pp. 261–283. [Google Scholar]
- Ditmyer, M.M.; Dounis, G.; Howard, K.M.; Mobley, C.; Cappelli, D. Validation of a multifactorial risk factor model used for predicting future caries risk with Nevada adolescents. BMC Oral Health 2011, 20, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Aas, J.A.; Paster, B.J.; Stokes, L.N.; Olsen, I.; Dewhirst, F.E. Defining the normal bacterial flora of the oral cavity. J. Clin. Microbiol. 2005, 43, 5721–5732. [Google Scholar] [CrossRef] [PubMed]
- Aas, J.A.; Griffen, A.L.; Dardis, S.R.; Lee, A.M.; Olsen, I.; Dewhirst, F.E.; Leys, E.J.; Paster, B.J. Bacteria of dental caries in primary and permanent teeth in children and young adults. J. Clin. Microbiol. 2008, 46, 1407–1417. [Google Scholar] [CrossRef] [PubMed]
- Crielaard, W.; Zaura, E.; Schuller, A.A.; Huse, S.M.; Montijn, R.C.; Keijser, B.J. Exploring the oral microbiota of children at various developmental stages of their dentition in the relation to their oral health. BMC Med. Genom. 2011, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Belda-Ferre, P.; Alcaraz, L.D.; Cabrera-Rubio, R.; Romero, H.; Simón-Soro, A.; Pignatelli, M.; Mira, A. The oral metagenome in health and disease. ISME J. 2012, 6, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Simón-Soro, A.; Tomás, I.; Cabrera-Rubio, R.; Catalan, M.D.; Nyvad, B.; Mira, A. Microbial geography of the oral cavity. J. Dent. Res. 2013, 92, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Plonka, K.A.; Pukallus, M.L.; Barnett, A.G.; Walsh, L.J.; Holcombe, T.H.; Seow, W.K. Mutans streptococci and lactobacilli colonization in predentate children from the neonatal period to seven months of age. Caries Res. 2012, 46, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Olson, J.C.; Cuff, C.F.; Lukomski, S.; Lukomska, E.; Canizales, Y.; Wu, B.; Crout, R.J.; Thomas, J.G.; McNeil, D.W.; Weyant, R.J.; et al. Use of 16S ribosomal RNA gene analyses to characterize the bacterial signature associated with poor oral health in West Virginia. BMC Oral Health 2011, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- Tellez, M.; Gray, S.L.; Gray, S.; Lim, S.; Ismail, A.I. Sealants and dental caries: Dentists’ perspectives on evidence-based recommendations. J. Am. Dent. Assoc. 2011, 142, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.G.; Shetty, P.C.; Ramachandra, C.S.; Bhat, N.S.; Laxmikanth, S.M. In vitro assessment of photocatalytic titanium oxide surface modified stainless steel orthodontic brackets for antiadherent and antibacterial properties against Lactobacillus acidophilus. Angle Orthod. 2011, 81, 1028–1035. [Google Scholar] [CrossRef] [PubMed]
- Simón-Soro, A.; Belda-Ferre, P.; Cabrera-Rubio, R.; Alcaraz, L.D.; Mira, A. A tissue-dependent hypothesis of dental caries. Caries Res. 2013, 47, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Yoshizawa, J.M.; Schafer, C.A.; Schafer, J.J.; Farrell, J.J.; Paster, B.J.; Wong, D.T. Salivary biomarkers: Toward future clinical and diagnostic utilities. Clin. Microbiol. Rev. 2013, 26, 781–791. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Yang, F.; Zeng, X.; Chen, J.; Li, R.; Wen, T.; Li, C.; Wei, W.; Liu, J.; Chen, L.; et al. Preliminary characterization of the oral microbiota of Chinese adults with and without gingivitis. BMC Oral Health 2011, 11, 33. [Google Scholar] [CrossRef] [PubMed]
- Simón-Soro, A.; Guillen-Navarro, M.; Mira, A. Metatranscriptomics reveals overall active bacterial composition in caries lesions. J. Oral Microbiol. 2014, 6, 25443. [Google Scholar] [CrossRef] [PubMed]
- Schafer, C.A.; Schafer, J.J.; Yakob, M.; Lima, P.; Camargo, P.; Wong, D.T. Saliva diagnostics: Utilizing oral fluids to determine health status. Monogr. Oral Sci. 2014, 24, 88–98. [Google Scholar] [PubMed]
- Guo, L.; Shi, W. Salivary biomarkers for caries risk assessment. J. Calif. Dent. Assoc. 2013, 41, 107–109, 112–118. [Google Scholar] [PubMed]
- Gao, X.; Jiang, S.; Koh, D.; Hsu, C.Y. Salivary biomarkers for dental caries. Periodontol. 2000 2016, 70, 128–141. [Google Scholar] [CrossRef] [PubMed]
- Diaz de Guillory, C.; Schoolfield, J.D.; Johnson, D.; Yeh, C.K.; Chen, S.; Cappelli, D.P.; Bober-Moken, I.G.; Dang, H. Co-relationships between glandular salivary flow rates and dental caries. Gerodontology 2014, 31, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Tao, R.; Jurevic, R.J.; Coulton, K.K.; Tsutsui, M.T.; Roberts, M.C.; Kimball, J.R.; Wells, N.; Berndt, J.; Dale, B.A. Salivary antimicrobial peptide expression and dental caries experience in children. Antimicrob. Agents Chemother. 2005, 49, 3883–3888. [Google Scholar] [CrossRef] [PubMed]
- Jenkinson, H.F.; Lamont, R.J. Oral microbial communities in sickness and in health. Trends Microbiol. 2005, 13, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Loke, C.; Lee, J.; Sander, S.; Mei, L.; Farella, M. Factors affecting intra-oral pH—A review. J. Oral Rehabil. 2016, 43, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Khurshid, Z.; Zohaib, S.; Najeeb, S.; Zafar, M.S.; Slowey, P.D.; Almas, K. Human Saliva Collection Devices for Proteomics: An Update. Int. J. Mol. Sci. 2016, 17, 846. [Google Scholar] [CrossRef] [PubMed]
- Dawes, C. Circadian rhythms in human salivary flow rate and composition. J. Physiol. 1972, 220, 529–545. [Google Scholar] [CrossRef] [PubMed]
- Greene, J.C.; Vermillion, J.R. The Simplified Oral Hygiene Index. J. Am. Dent. Assoc. 1964, 68, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Loë, H.; Silness, J. Periodontal disease in pregnancy. Acta Odontol. Scand. 1963, 21, 533. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Oral Health Surveys—Basic Methods, 4th ed.; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Navazesh, M.; Christensen, C.M. A comparison of whole mouth resting and stimulated salivary measurement procedures. J. Dent. Res. 1982, 61, 1158–1162. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2014; Available online: http://www.R-project.org/ (accessed on 7 October 2015).
- Trevino, V.; Falciani, F. Galgo: Genetic Algorithms for Multivariate Statistical Models from Large-scale Functional Genomics Data. R Package Version 1.2. 2014. Available online: http://bioinformatica.mty.itesm.mx/?q=node/82 (accessed on 7 October 2015).
- Venables, W.N.; Ripley, B.D. Modern Applied Statistics with S, 4th ed.; Springer: New York, NY, USA, 2002. [Google Scholar]
- Ashraf, R.; Shah, N.P. Immune system stimulation by probiotic microorganisms. Crit. Rev. Food Sci. Nutr. 2014, 54, 938–956. [Google Scholar] [CrossRef] [PubMed]
- Guan, Y.H.; Lath, D.L.; Graaf, T.; Lilley, T.H.; Brook, A.H. Moderation of oral bacterial adhesion on saliva-coated hydroxyapatite by polyaspartate. J. Appl. Microbiol. 2003, 94, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Santarpia, R.P.; Lavender, S.; Gittins, E.; Vandeven, M.; Cummins, D.; Sullivan, R. A 12-week clinical study assessing the clinical effects on plaque metabolism of a dentifrice containing 1.5% arginine, an insoluble calcium compound and 1450 ppm fluoride. Am. J. Dent. 2014, 27, 100–105. [Google Scholar] [PubMed]
- Featherstone, J.D. The caries balance: The basis for caries management by risk assessment. Oral Health Prev. Dent. 2004, 2, 259–264. [Google Scholar] [PubMed]
- Young, D.A.; Featherstone, J.D. Implementing caries risk assessment and clinical interventions. Dent. Clin. N. Am. 2010, 54, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Heikkinen, A.M.; Nwhator, S.O.; Rathnayake, N.; Mäntylä, P.; Vatanen, P.; Sorsa, T. Pilot Study on Oral Health Status as Assessed by an Active Matrix Metalloproteinase-8 Chairside Mouthrinse Test in Adolescents. J. Periodontol. 2016, 87, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Crall, J.J.; Donly, K.J. Dental sealants guidelines development: 2002–2014. Pediatr. Dent. 2015, 37, 111–115. [Google Scholar] [PubMed]
- Divaris, K. Predicting Dental Caries Outcomes in Children: A “Risky” Concept. J. Dent. Res. 2016, 95, 248–254. [Google Scholar] [CrossRef] [PubMed]


| Category | Salivary Compound | Manufacturer | Sample Dilution |
|---|---|---|---|
| Immune System | IgA | Assaypro | 1:1000 |
| IgG | Assaypro | 1:10 | |
| IgM | Assaypro | 1 | |
| Alpha-defensin 1-3 | Assaypro | 1:10 | |
| β-defensin 1 | Sun Red | 1 | |
| β-defensin 2 | Sun Red | 1 | |
| β-defensin 3 | Sun Red | 1 | |
| Cathelicidin LL-37 | Assaypro | 1:200 | |
| Lactoferrin | Assaypro | 1:20 | |
| Calprotectin | Assaypro | 1 | |
| Lysozyme | Assaypro | 1:8000 | |
| C3a | Sun Red | 1:10 | |
| Adhesion | PRB1 | Sun Red | 1:10 |
| Statherin | Sun Red | 1:200 | |
| Collagen type I | Sun Red | 1 | |
| Mucin C7 | Sun Red | 1:50 | |
| Mucin C5B | Sun Red | 1:100 | |
| Alpha-2 macroglobulin | Assaypro | 1:4 | |
| Fibronectin | Assaypro | 1:20 | |
| pH | Lactate | BioVision | 1:20 |
| Formate | BioVision | 1:5 | |
| Calcium | BioVision | 1 | |
| Phosphate | BioVision | 1:200 | |
| Urea | BioVision | 1:25 | |
| Alpha-amylase | Biovision | 1:10 |
| Category | Compound | 0.5 h | 6 h |
|---|---|---|---|
| Immune System | Cathelicidin LL-37 | 0.007 | 0.002 |
| IgA | 0.007 | 0.353 | |
| α-Defensin 1-3 | 0.105 | 0.853 | |
| IgM | 0.326 | 1.000 | |
| β-Defensin 1 | 0.393 | 0.796 | |
| Lactoferrin | 0.393 | 1.000 | |
| C3a | 0.393 | 0.315 | |
| Calprotectin | 0,405 | 0.326 | |
| β-Defensin 3 | 0.520 | 0.970 | |
| IgG | 0.520 | 0.121 | |
| β-Defensin 2 | 0.971 | 7.57 × 10−5 | |
| Lysozyme | 0.796 | 0.280 | |
| Adhesion | Statherin | 0.063 | 0.247 |
| Fibronectin | 0.123 | 0.121 | |
| Mucin 5B | 0.218 | 0.684 | |
| Mucin 7 | 0.247 | 0.571 | |
| Collagen I | 0.273 | 0.104 | |
| Alpha-2 Macroglobulin | 0.393 | 0.796 | |
| PRB1 | 0.912 | 0.190 | |
| pH | Phosphate | 0.140 | 0.054 |
| Lactate | 0.353 | 0.123 | |
| Urea | 0.393 | 0.393 | |
| Calcium | 0.631 | 0.315 | |
| Formate | 0.853 | 0.029 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mira, A.; Artacho, A.; Camelo-Castillo, A.; Garcia-Esteban, S.; Simon-Soro, A. Salivary Immune and Metabolic Marker Analysis (SIMMA): A Diagnostic Test to Predict Caries Risk. Diagnostics 2017, 7, 38. https://doi.org/10.3390/diagnostics7030038
Mira A, Artacho A, Camelo-Castillo A, Garcia-Esteban S, Simon-Soro A. Salivary Immune and Metabolic Marker Analysis (SIMMA): A Diagnostic Test to Predict Caries Risk. Diagnostics. 2017; 7(3):38. https://doi.org/10.3390/diagnostics7030038
Chicago/Turabian StyleMira, Alex, Alejandro Artacho, Anny Camelo-Castillo, Sandra Garcia-Esteban, and Aurea Simon-Soro. 2017. "Salivary Immune and Metabolic Marker Analysis (SIMMA): A Diagnostic Test to Predict Caries Risk" Diagnostics 7, no. 3: 38. https://doi.org/10.3390/diagnostics7030038