1. Introduction
Shared decision-making (SDM) has become a central element of patient-centered care. Research, policies, and clinical guidelines have strongly advocated the implementation of SDM. The SDM model is a clinical decision-making model that ensures that healthcare professionals do not make decisions solely based on knowledge, experience, and the latest scientific evidence, but also by allowing patients to participate in all essential aspects of the medical decision. Patients need and have the right to understand available treatment options and participate in decision-making regarding their health.
The objective of the SDM process is to find the best treatment for a specific patient by encouraging the patient to play a more active role in the process of medical consultation [
1]. Thus, eliciting patient preferences is a vital component of SDM [
2]. However, recent findings show that patient preferences cannot be efficiently or accurately judged based on communicative exchanges during routine office visits, even for patients seeking to expand their decision-making role [
3]. Patient decision aids (PDA) are tools used to inform patients who want to actively participate in health decision-making and help them make clear choices. These tools are most effective when used together with counseling from a healthcare provider. They provide information about a health condition using the latest quality-rated scientific evidence and options and outcomes regarding the diagnosis and treatment of the disease. In addition, they help clarify patients’ values and understanding of the relative importance of the benefits and risks of these options.
In the digital era, many of the processes regarding patient-informed health decision-making may benefit from being available online, such as understanding the disease; knowledge of related healthcare alternatives, benefits, risks, and uncertainties; personal preferences and values; and participation according to the role. When applied to patient education and decision aids, “digital” usually refers to software and platforms for teaching and learning that can be used with video or audio players, computers, or mobile devices. An increasing number of digital consumer and patient health tools are being developed for use on electronic devices such as computers and smartphones as standalone software or websites. Online resources to facilitate SDM have been advocated [
4]; however, concerns have been raised over the effectiveness of electronic assessment tools at improving the shared decision-making process [
5]. Various techniques have been designed to help patients obtain the information they need to enable them to play an active role in their care under a more equitable partnership. Although SDM has been increasingly popular in healthcare practice in Asia [
6] and Taiwan [
7], barriers may still be encountered [
8], and the integration of digital and online processes on a hospital-wide implementation scale has scarcely been reported. Leaders in healthcare organizations are keen to run their service more efficiently and respond to patients’ needs.
This study aimed to assess the effectiveness of integrating an online SDM process into existing practice with a participating design approach in a university-affiliated medical center.
4. Discussion
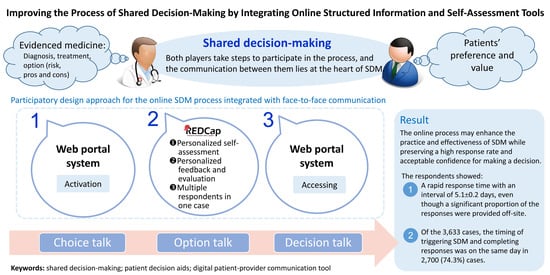
In this study, we found that a significant proportion (about one-fourth) of the participants of SDM chose additional off-site assessments of the options and their preferences before expressing that they were prepared to make a decision rather than proceeding directly to on-site decision talks right after the option and decision talks. The provision of off-site case-specific online access to the SDM and PDA contents achieved a high response rate regarding the participants’ preparedness for decision-making. In addition, the output of the electronic SDM topics allowed for more than one response from the participants and their family to be captured. Therefore, the online self-assessment SDM process integrated with face-to-face communication enhanced the practice and effectiveness of the institutional SDM processes while preserving high response rates and achieving acceptable confidence when making decisions.
SDM processes involve face-to-face communication and discussions of the options for medical interventions or treatments throughout the three stages of the encounter, including the choice talk, options talk, and decision talk [
15]. While this scenario provides direct explanation and feedback, the patients or their surrogates may face pressure to respond quickly before leaving the consultation. In addition, repeatedly introducing and explaining the decision needs and options may impose a burden on the SDM team. The decision quality may also be hindered by a suboptimal understanding of the options, the benefits and risks of the interventions, and the expression of personal matters, values, and preferences on such a fraught occasion. Therefore, our institutional approach of implementing online access for the SDM and PDA contents and assessment processes may provide a complementary mechanism for the patients and surrogates to more confidently prepare to make a decision. Furthermore, the patients, members of their family, and surrogates could also access the SDM and PDA contents at any time based on their needs for optimal understanding in order that they felt well-prepared to provide a response. We analyzed all the electronic SDM cases performed during the study period, and therefore we were able to describe the whole picture of the institutional implementation of the electronic SDM process and the trends of particular SDM topics.
Reports in the literature have shown the importance and benefits of online SDM tools, such as lung cancer screening [
16], neurosurgical procedures [
17], orthopedic interventions [
18], and especially as a valuable adjunct to clinical discussions [
19]. Online SDM tools have been reported to be cost-effective for patients with inguinal hernia, gallstones, and knee or hip osteoarthritis [
20]. The online SDM and PDA services in our institution provide a full range of information and assessment tools coupled with real-time capturing of their responses, and this may allow clinicians of the SDM team to proceed with arranging the decision talk in a timely manner. The electronic process integrated with the usual face-to-face process provided a structured, guided approach for SDM. As clinicians might not be familiar with the concept and goal of SDM, they might need these structured processes and feedback from the patients, surrogates, and family members through the assessment forms. The real-time nature of the capture of online responses by the REDCap system allows SDM teams and clinicians caring for patients to receive real-time feedback and proceed in timely decision talks.
Although it is important to assess the effectiveness of the systematic implementation of this online process, in this hospital the development of online SDM and PDA contents and the integration of these contents into the REDCap platform required the active participation of the clinical department and healthcare workers in our hospital. Therefore, we considered that—since the online system has been optimized based on the needs of the clinicians—a before–after assessment by the participating clinicians might not be required. Nevertheless, our interviews with the clinicians provide their comments after the implementation of the online mechanism.
This report focused on the hospital-wide implementation of the online process by integrating it into the existing face-to-face process and thus a variety of SDM topics and practices from the departments of this hospital were involved. Therefore, the assessment of patient outcomes might be difficult as a result of a significantly mixed patient population and different clinician practices. Furthermore, the impact of SDM on clinical outcomes remained undetermined, whereas researchers also emphasized the measurement of patient-centered outcomes.
In this study, we found a preference for off-site access to SDM and PDA compared with face-to-face practice among different patient and surrogate populations and care scenarios. Explanations include the severity of illness and urgency requiring timely decision making, the health literacy that might determine the speed and degree of understanding the options and preferences, the familiarity of digital and online platforms, and the number of participating persons for the decision in addition to the patient. We also found that age and gender might play significant roles in the online responses. Female responders tended to provide a lower score for the feedback evaluation of the SDM process, whereas older responders tended to require a longer interval to finish their online reviews and responses. These findings might reflect the cultural characteristics of Taiwan in terms of making decisions. These speculations require support from further research.
The implementation of the online SDM process in our institution highlighted that more time was needed to achieve preparedness for the final decision-making, suggesting the time-consuming nature of SDM. This is in line with other studies that have shown that SDM is more time-consuming but that patients may make better decisions [
21]. In addition, providing sufficient time to re-assess options and preferences suggests that SDM is a more patient-centered approach [
22]. Nevertheless, the implementation of SDM still faces multiple barriers [
8]. Further integration of online content may be promising, and standardized videos could be considered [
23]. Furthermore, scientifically analyzing the decision-making process may also be required in the future [
24]. Healthcare professionals may also require better understanding and training on the SDM process and practice. Establishing an online SDM process may improve the completeness and correctness of practicing SDM in the real world [
25]. The integration of artificial intelligence into PDA may also be a promising mechanism to enhance the effectiveness of SDM [
26,
27]. Nevertheless, challenges of SDM might exist, such as patients with multiple disease conditions and limited health literacy and older patients who require specially designed SDM tools [
28], those lacking socioeconomic resources and family support, and the rapidly emerging management options for specific medical problems that demand timely updates for SDM, as well as healthcare settings facing the COVID pandemic [
29]. Indeed, a versatile and convenient platform both for the providers and patients might be necessary for the era of digital transformation in the healthcare practice.
SDM has been an emerging and increasingly popular clinical practice in Taiwan, and several healthcare organizations have deployed online processes to help enhance the practice and outcomes. Nevertheless, since the National Taiwan University Hospital contributes to the REDCap community by translating Traditional Chinese language for REDCap, to our knowledge there was a lack of reports on the implementation of REDCap-based online SDM process that integrated into the face-to-face process for healthcare scenarios in Taiwan. The REDCap system applied in our healthcare system is a standardized server software that allows non-profit organizations to join the global REDCap consortium and to install and administer REDCap on their local servers in order to use for work at the organization. Therefore, the generalization of our model can be modified as a broader design approach with participants from different hospitals in Taiwan, involving the stakeholders and users from clinical departments, quality management, and IT engineers in the design process to co-design the online SDM integration and make sure the technical structure meets their needs and is applicable in their healthcare organizations.
There are several limitations to this study. First, this study was based on analysis of records related to the electronic SDM process, while data related to the patients, such as diagnosis, comorbidities, interventions, and socioeconomic status, were lacking. Therefore, we did not know whether the patients received any of the interventions listed in the PDA contents to facilitate the SDM process. In addition, we did not know the exact time when the formal decisions were made, such as signing informed consent for interventions. Second, after completing the choice and option talks, we did not track whether there was additional contact between the SDM team and patients or surrogates. Therefore, whether the high off-site response rate to the online assessment process was due purely to the online process remains to be elucidated. Third, although the hospital-wide SDM processes were designed to be structural, we do not know how completely and correctly the SDM teams performed the choice and option talks for the patients and surrogates. Fourth, we do not have data on how often the patients and their surrogates accessed the online materials, nor did we know whether the responses were from single respondents or a collective opinion after a group discussion between family members and surrogates. Fifth, we did not access the clinical data to assess possible outcome changes brought by the implementation of the online process. This report focused on the hospital-wide implementation of the online process by integrating it into the existing face-to-face process, and thus a variety of SDM topics and practices from the departments of this hospital were involved. Therefore, the assessment of patient outcomes might be difficult as a result of a significantly mixed patient population and different clinician practices. Furthermore, the impact of SDM on clinical outcomes remains undetermined, whereas researchers have also emphasized the measurement of patient-centered outcomes. A variety of outcome assessments have been proposed for the evaluation of SDM processes [
30,
31,
32,
33]; therefore, the evaluation of this system can be further improved by establishing the measurements proposed by the experts and researchers. Last, this was a single center study. The generalization of our model and findings might need more robust designs, such as multicenter, randomized controlled trials [
34], cluster randomized controlled trials [
35], and multicentered, stepped wedge trials [
20,
36].