Journal Description
Journal of Personalized Medicine
Journal of Personalized Medicine
is an international, peer-reviewed, open access journal on personalized medicine, published monthly online by MDPI. The Inter-American Society for Minimally Invasive Spine Surgery (SICCMI), Korean Society of Brain Neuromodulation Therapy (KBNT), American Board of Precision Medicine (ABOPM) and Brazilian Society of Personalized Medicine (SBMP) are affiliated with JPM and their members receive a discount on article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, PubMed, PMC, Embase, and other databases.
- Journal Rank: CiteScore - Q1 (Medicine (miscellaneous))
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21.5 days after submission; acceptance to publication is undertaken in 3.5 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
Latest Articles
Application of Treatment Response Biomarkers from Major Depression to Perinatal Depression
J. Pers. Med. 2025, 15(12), 607; https://doi.org/10.3390/jpm15120607 (registering DOI) - 6 Dec 2025
Abstract
Background/Objectives: Perinatal depression poses significant risks to maternal and fetal health, yet biomarkers for treatment response in the field remain limited. Given the overlap in symptoms with major depressive disorder (MDD) and the comparatively more vast MDD literature, identifying promising MDD biomarkers
[...] Read more.
Background/Objectives: Perinatal depression poses significant risks to maternal and fetal health, yet biomarkers for treatment response in the field remain limited. Given the overlap in symptoms with major depressive disorder (MDD) and the comparatively more vast MDD literature, identifying promising MDD biomarkers for treatment response and examining corresponding perinatal depression biomarkers can reveal translational opportunities. Methods: PUBMED searches were conducted for individual biomarkers and MDD and perinatal depression, as well as with treatment response to antidepressant pharmacological treatment and neuromodulation treatments. When available, evidence from meta-analyses and systematic reviews were preferentially summarized. Review: This narrative review presents the current evidence on MDD and perinatal depression treatment response biomarkers, including brain-derived neurotrophic factor (BDNF), S100 calcium-binding protein B (S100B), electroencephalography, event-related potentials, metabolomics, hypothalamic–pituitary–adrenal axis hormones, neuroimaging markers, inflammatory markers, and neuroactive steroids. Conclusions: Biomarker research in MDD yields insights on promising biomarkers for treatment response, including BDNF, S100B, theta band density and cordance, inflammatory markers IL-8, CRP, and TNF- α, and neuroactive steroids.
Full article
(This article belongs to the Special Issue Multiple Biomarkers for the Diagnosis and Precision Treatment of Depression)
Open AccessSystematic Review
Immunotherapy and IVF Outcomes in Unexplained Recurrent Pregnancy Loss: A Systematic Review with Implications for Personalized Reproductive Medicine
by
Giosuè Giordano Incognito, Carla Ettore, Marco D’Asta, Ferdinando Antonio Gulino, Roberta Foti, Roberto Tozzi, Orazio De Tommasi, Pierluigi Chieppa, Stefano Di Michele and Giuseppe Ettore
J. Pers. Med. 2025, 15(12), 606; https://doi.org/10.3390/jpm15120606 (registering DOI) - 6 Dec 2025
Abstract
Background/Objectives: Recurrent pregnancy loss (RPL) is one of the most challenging conditions in reproductive medicine, particularly when no identifiable cause can be determined after diagnostic evaluation. Although the role of immunological dysregulation has been hypothesized, the implementation of immunotherapies in clinical practice is
[...] Read more.
Background/Objectives: Recurrent pregnancy loss (RPL) is one of the most challenging conditions in reproductive medicine, particularly when no identifiable cause can be determined after diagnostic evaluation. Although the role of immunological dysregulation has been hypothesized, the implementation of immunotherapies in clinical practice is controversial due to inconsistent findings and methodological heterogeneity across studies. This systematic review aims to provide an overview of the main characteristics of existing research on the role of immunological interventions in relation to In Vitro Fertilization (IVF) outcomes in women with RPL. Given the marked inter-individual variability in immunological mechanisms among affected women, evaluating these treatments may help identify future directions for personalized reproductive medicine. Methods: A comprehensive bibliographic search was systematically conducted from inception to October 2025 across databases, including Medline, Embase, Scopus, the Cochrane Database of Systematic Reviews, and ClinicalTrials.gov. Studies were included if they evaluated the efficacy of immunological treatments in women with unexplained RPL, comparing IVF outcomes between case and control groups. Results: Six cohort studies were included, four retrospective and two prospective. The immunological treatments investigated were granulocyte colony-stimulating factor (G-CSF), intravenous intralipid (with or without prednisolone), and lymphocyte immunization therapy (LIT). Despite some promising results, particularly for G-CSF and LIT, the studies were limited by small sample sizes, heterogeneous diagnostic criteria for RPL, and inconsistent treatment protocols. Furthermore, not all IVF outcomes, such as implantation and biochemical pregnancy rates, were reported. Conclusions: Current evidence is insufficient to support the use of immunotherapy in clinical practice for improving IVF outcomes in women with unexplained RPL. The variability in study design, patient selection, and immunotherapy regimens hinders the ability to draw firm conclusions. Well-designed randomized controlled trials with standardized definitions and outcome measures are needed to determine whether and for whom immunological treatments may offer clinical benefit.
Full article
(This article belongs to the Special Issue Personalized Medicine in Reproductive Medicine)
►▼
Show Figures
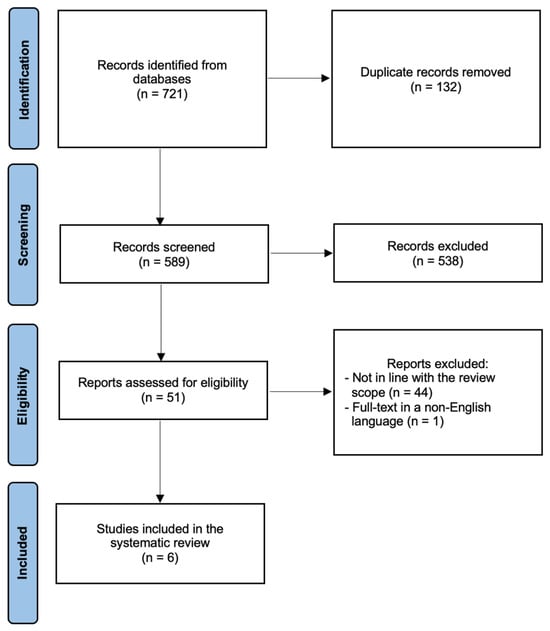
Figure 1
Open AccessSystematic Review
The Role of Artificial Intelligence in Imaging-Based Diagnosis of Retinal Dystrophy and Evaluation of Gene Therapy Efficacy
by
Weronika Chuchmacz, Barbara Bobowska, Alicja Forma, Eliasz Dzierżyński, Damian Puźniak, Barbara Teresińska, Jacek Baj and Joanna Dolar-Szczasny
J. Pers. Med. 2025, 15(12), 605; https://doi.org/10.3390/jpm15120605 - 5 Dec 2025
Abstract
Introduction: Inherited retinal dystrophies (IRDs) are genetically determined conditions leading to progressive vision loss. Developments in gene therapy are creating new treatment options for IRD, but require precise imaging diagnosis and monitoring. According to recent studies, artificial intelligence, especially deep neural networks, could
[...] Read more.
Introduction: Inherited retinal dystrophies (IRDs) are genetically determined conditions leading to progressive vision loss. Developments in gene therapy are creating new treatment options for IRD, but require precise imaging diagnosis and monitoring. According to recent studies, artificial intelligence, especially deep neural networks, could become an important tool for analyzing imaging data. Material and Methods: A systematic literature review was conducted in accordance with PRISMA guidelines, using PubMed, Scopus, and Web of Science databases to identify publications from 2015 to 2025 on the application of artificial intelligence in diagnosing inherited retinal dystrophies and monitoring the effects of gene therapy. The included articles passed a two-stage selection process and met the methodological quality criteria. Results: Among all the included studies it can be noticed that the use of artificial intelligence in diagnostics and therapy of IRDs is rather effective. The most common method was deep learning with its subtype convolutional neural networks (CNNs). However, there is still a place for improvement due to various limitations occurring in the studies. Conclusions: The review points to the growing potential of AI models in optimizing the diagnostic and therapeutic pathway in IRDs, while noting current limitations such as low data availability, the need for clinical validation, and the interpretability of the models. AI may play a key role in personalized ophthalmic medicine in the near future, supporting both clinical decisions and interventional study design.
Full article
(This article belongs to the Special Issue Innovative and Future Trends in Personalized Medicine for Retinal Diseases)
►▼
Show Figures

Figure 1
Open AccessArticle
Computational Modeling of Uncertainty and Volatility Beliefs in Escape-Avoidance Learning: Comparing Individuals with and Without Suicidal Ideation
by
Miguel Blacutt, Caitlin M. O’Loughlin and Brooke A. Ammerman
J. Pers. Med. 2025, 15(12), 604; https://doi.org/10.3390/jpm15120604 - 5 Dec 2025
Abstract
Background/Objectives: Computational studies using drift diffusion models on go/no-go escape tasks consistently show that individuals with suicidal ideation (SI) preferentially engage in active escape from negative emotional states. This study extends these findings by examining how individuals with SI update beliefs about
[...] Read more.
Background/Objectives: Computational studies using drift diffusion models on go/no-go escape tasks consistently show that individuals with suicidal ideation (SI) preferentially engage in active escape from negative emotional states. This study extends these findings by examining how individuals with SI update beliefs about action–outcome contingencies and uncertainty when trying to escape an aversive state. Methods: Undergraduate students with (n = 58) and without (n = 62) a lifetime history of SI made active (go) or passive (no-go) choices in response to stimuli to escape or avoid an unpleasant state in a laboratory-based negative reinforcement task. A Hierarchical Gaussian Filter (HGF) was used to estimate trial-by-trial trajectories of contingency and volatility beliefs, along with their uncertainties, prediction errors (precision-weighted), and dynamic learning rates, as well as fixed parameters at the person level. Bayesian mixed-effects models were used to examine the relationship between trial number, SI history, trial type, and all two-way interactions on HGF parameters. Results: We did not find an effect of SI history, trial type, or their interactions on perceived volatility of reward contingencies. At the trial level, however, participants with a history of SI developed progressively stronger contingency beliefs while simultaneously perceiving the environment as increasingly stable compared to those without SI experiences. Despite this rigidity, they maintained higher uncertainty during escape trials. Participants with an SI history had higher dynamic learning rates during escape trials compared to those without SI experiences. Conclusions: Individuals with an SI history showed a combination of cognitive inflexibility and hyper-reactivity to prediction errors in escape-related contexts. This combination may help explain difficulties in adapting to changing environments and in regulating responses to stress, both of which are relevant for suicide risk.
Full article
(This article belongs to the Special Issue Computational Behavioral Modeling in Precision Psychiatry)
►▼
Show Figures

Figure 1
Open AccessArticle
Hemodynamic Impact of the Aberrant Subclavian Artery: A CFD Investigation
by
Edoardo Ugolini, Giorgio La Civita, Marco Ferraresi, Moad Alaidroos, Alessandro Carlo Luigi Molinari, Maria Katsarou, Giovanni Rossi and Emanuele Ghedini
J. Pers. Med. 2025, 15(12), 603; https://doi.org/10.3390/jpm15120603 - 5 Dec 2025
Abstract
Background/Objectives: The aberrant subclavian artery (ASA) represents the most common congenital anomaly of the aortic arch, and is frequently associated with a Kommerell diverticulum, an aneurysmal dilation at the anomalous vessel origin. This condition carries a significant risk of rupture and dissection,
[...] Read more.
Background/Objectives: The aberrant subclavian artery (ASA) represents the most common congenital anomaly of the aortic arch, and is frequently associated with a Kommerell diverticulum, an aneurysmal dilation at the anomalous vessel origin. This condition carries a significant risk of rupture and dissection, and growing evidence indicates that local hemodynamic alterations may contribute to its development and progression. Computational Fluid Dynamics (CFD) provides a valuable non-invasive modality to assess biomechanical stresses and elucidate the pathophysiological mechanisms underlying these vascular abnormalities. Methods: In this study, twelve thoracic CT angiography scans were analyzed: six from patients with ASA and six from individuals with normal aortic anatomy. CFD simulations were performed using OpenFOAM, with standardized boundary conditions applied across all cases to isolate the influence of anatomical differences in flow behavior. Four key hemodynamic metrics were evaluated—Wall Shear Stress (WSS), Oscillatory Shear Index (OSI), Drag Forces (DF), and Turbulent Viscosity Ratio (TVR). The aortic arch was subdivided into Ishimaru zones 0–3, with an adapted definition accounting for ASA anatomy. For each region, time- and space-averaged quantities were computed to characterize mean values and oscillatory behavior. Conclusions: The findings demonstrate that patients with ASA exhibit markedly altered hemodynamics in zones 1–3 compared to controls, with consistently elevated WSS, OSI, DF, and TVR. The most pronounced abnormalities occurred in zones 2–3 near the origin of the aberrant vessel, where disturbed flow patterns and off-axis mechanical forces were observed. These features may promote chronic wall stress, endothelial dysfunction, and localized aneurysmal degeneration. Notably, two patients (M1 and M6) displayed particularly elevated drag forces and TVR in the distal arch, correlating with the presence of a distal aneurysm and right-sided arch configuration, respectively. Overall, this work supports the hypothesis that aberrant hemodynamics contribute to Kommerell diverticulum formation and progression, and highlights the CFD’s feasibility for clarifying disease mechanisms, characterizing flow patterns, and informing endovascular planning by identifying hemodynamically favorable landing zones.
Full article
(This article belongs to the Special Issue Biomedical Tools in Diagnosis and Personalized Therapy of Cardiovascular Disease)
►▼
Show Figures
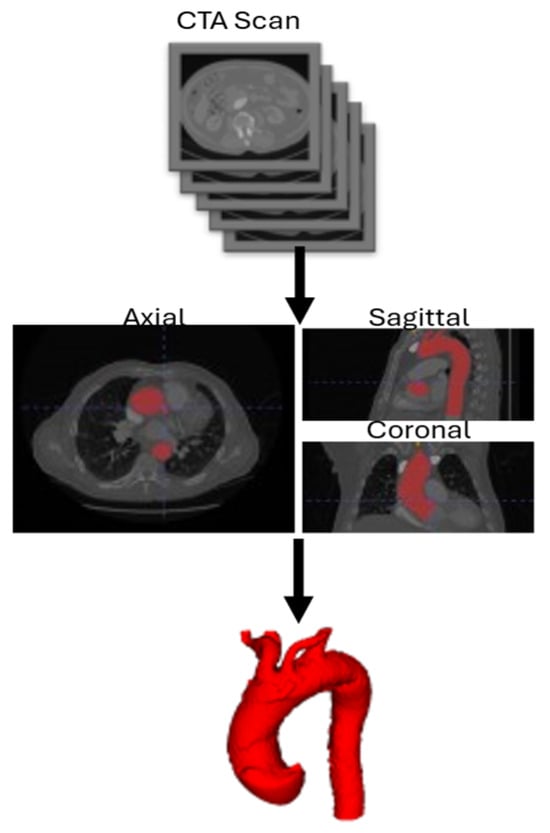
Figure 1
Open AccessReview
Management Strategies for Failed Pilon Fractures: A Personalized Approach to Revision Reconstruction
by
Lauren Luther, Richard S. Moore III, Sriranjani Darbha, Bethany Gallagher and Daniel J. Stinner
J. Pers. Med. 2025, 15(12), 602; https://doi.org/10.3390/jpm15120602 - 5 Dec 2025
Abstract
Despite advances in staged protocols and fixation techniques, treatment of pilon fractures remains a significant challenge in orthopedic trauma, with up to 21% of patients requiring revision surgery. Management of a pilon fracture that has failed initial treatment involves navigating a myriad of
[...] Read more.
Despite advances in staged protocols and fixation techniques, treatment of pilon fractures remains a significant challenge in orthopedic trauma, with up to 21% of patients requiring revision surgery. Management of a pilon fracture that has failed initial treatment involves navigating a myriad of complicating variables, including infection, bone loss, malalignment, and nonunion. Although no single surgical approach can be aptly applied to the broad range of pathology and severity spanned by these patients, this narrative review provides a systematic framework for developing a revision pilon reconstruction plan. We present a protocol for pre-operative assessment and review current techniques for infection eradication, bone defect management, deformity correction, and joint-preserving versus joint-sparing surgery. These fundamental strategies form the foundation of a successful salvage plan and can be personalized to address specific fracture morphology, host factors, and goals of care.
Full article
(This article belongs to the Special Issue Orthopedic Diseases: Advances in Limb Reconstruction)
►▼
Show Figures

Figure 1
Open AccessReview
Multimodal Imaging in Epilepsy Surgery for Personalized Neurosurgical Planning
by
Joaquin Fiallo Arroyo and Jose E. Leon-Rojas
J. Pers. Med. 2025, 15(12), 601; https://doi.org/10.3390/jpm15120601 - 5 Dec 2025
Abstract
Drug-resistant epilepsy affects nearly one-third of individuals with epilepsy and remains a major cause of neurological morbidity worldwide. Surgical intervention offers a potential cure, but its success critically depends on the precise identification of the epileptogenic zone and the preservation of eloquent cortical
[...] Read more.
Drug-resistant epilepsy affects nearly one-third of individuals with epilepsy and remains a major cause of neurological morbidity worldwide. Surgical intervention offers a potential cure, but its success critically depends on the precise identification of the epileptogenic zone and the preservation of eloquent cortical and subcortical regions. This review aims to provide a comprehensive synthesis of current evidence on the role of multimodal neuroimaging in the personalized presurgical evaluation and planning of epilepsy surgery. We analyze how structural, functional, metabolic, and electro-physiological imaging modalities contribute synergistically to improving localization accuracy and surgical outcomes. Structural MRI remains the cornerstone of presurgical assessment, with advanced sequences, post-processing techniques, and ultra-high-field (7 T) MRI enhancing lesion detection in previously MRI-negative cases. Functional and metabolic imaging, including FDG-PET, ictal/interictal SPECT, and arterial spin labeling MRI, offer complementary insights by revealing regions of altered metabolism or perfusion associated with seizure onset. Functional MRI enables non-invasive mapping of language, memory, and motor networks, while diffusion tensor imaging and tractography delineate critical white-matter pathways to minimize postoperative deficits. Electrophysiological integration through EEG source imaging and magnetoencephalography refines localization when combined with MRI and PET data, forming the basis of multimodal image integration platforms used for surgical navigation. Our review also briefly explores emerging intraoperative applications such as augmented and virtual reality, intraoperative MRI, and laser interstitial thermal therapy, as well as advances driven by artificial intelligence, such as automated lesion detection and predictive modeling of surgical outcomes. By consolidating recent developments and clinical evidence, this review underscores how multimodal imaging transforms epilepsy surgery from a lesion-centered to a patient-centered discipline. The purpose is to highlight best practices, identify evidence gaps, and outline future directions toward precision-guided, minimally invasive, and function-preserving neurosurgical strategies for patients with drug-resistant focal epilepsy.
Full article
(This article belongs to the Section Personalized Therapy in Clinical Medicine)
►▼
Show Figures
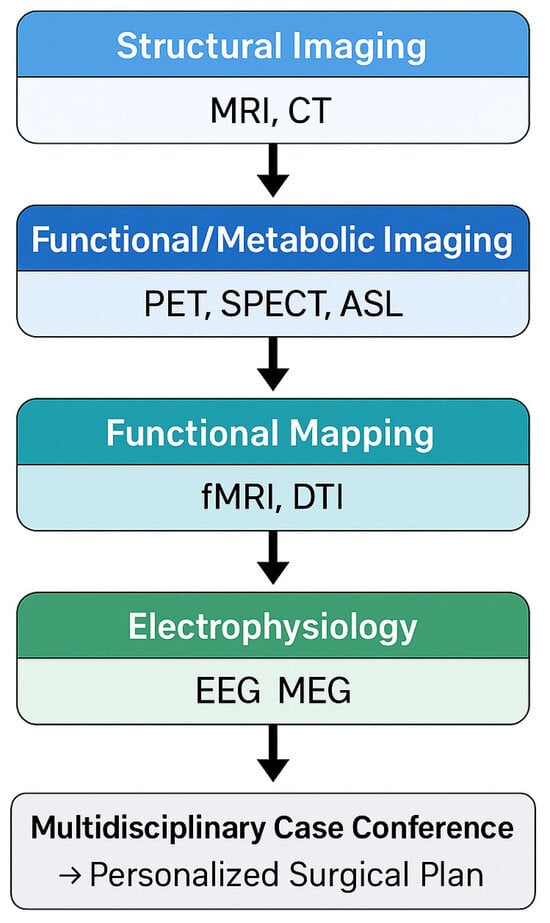
Figure 1
Open AccessArticle
The Hidden Burden of Gastroparesis in Chronic Kidney Disease: Evidence from Inpatient and Outpatient Cohorts for Personalized Care
by
Xiaoliang Wang, Omar Almetwali, Armando Marino-Melendez, Darwin Tan, Jiayan Wang and Gengqing Song
J. Pers. Med. 2025, 15(12), 600; https://doi.org/10.3390/jpm15120600 - 4 Dec 2025
Abstract
Background/Objectives: Patients with chronic kidney disease (CKD) frequently experience upper gastrointestinal (GI) symptoms such as epigastric discomfort, nausea, vomiting, and early satiety. These symptoms can contribute to malabsorption and intermittent dehydration, ultimately accelerating the decline of residual renal function. However, they are often
[...] Read more.
Background/Objectives: Patients with chronic kidney disease (CKD) frequently experience upper gastrointestinal (GI) symptoms such as epigastric discomfort, nausea, vomiting, and early satiety. These symptoms can contribute to malabsorption and intermittent dehydration, ultimately accelerating the decline of residual renal function. However, they are often attributed to electrolyte imbalances or fluid overload, and the possibility of underlying gastroparesis is frequently overlooked by both patients and caregivers. This study aimed to provide new insights into the relationship between CKD and gastroparesis through a dual, population-based retrospective analysis that incorporated both inpatient and outpatient data. Methods: From the National Inpatient Sample (NIS) database, 3,579,372 patients diagnosed with gastroparesis, with or without CKD, were identified. From the TriNetX database, 6,263,251 patients presenting to ambulatory clinics with a chief complaint of nausea and vomiting were included. In both datasets, gastroparesis was defined using ICD-10-CM codes. Results: In the inpatient cohort, the prevalence of gastroparesis increased in proportion to CKD severity, with the highest likelihood observed in advanced stages compared to patients without CKD. An increased risk of gastroparesis was also observed in the outpatient CKD cohort from an independent TriNetX database, while the severity-dependent phenotype was not consistent. However, after rigorous propensity score matching, advanced CKD remained significantly associated with higher odds of gastroparesis, with the greatest risk observed in patients with end-stage renal disease (ESRD). Conclusions: These findings, validated across two large and independent datasets representing both inpatient and outpatient populations, demonstrate a consistent association between CKD severity and gastroparesis. They highlight the importance of routine screening and early management of gastroparesis in patients with advanced CKD to improve outcomes and reduce disease burden for CKD patients with sign of early satiety or dyspepsia.
Full article
(This article belongs to the Special Issue Personalized Diagnosis and Treatment of Digestive System Disorders)
►▼
Show Figures
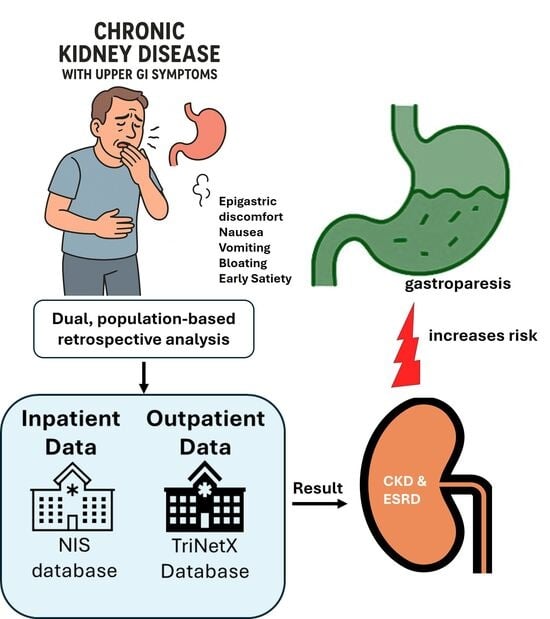
Graphical abstract
Open AccessArticle
Intolerance of Uncertainty Mediates the Relationship Between Social Anxiety and Problematic Smartphone Use Severity in College Students
by
Sana Alavinikoo, Elyse F. Hutcheson and Jon D. Elhai
J. Pers. Med. 2025, 15(12), 599; https://doi.org/10.3390/jpm15120599 - 4 Dec 2025
Abstract
Objectives: Prior research has found that social anxiety and intolerance of uncertainty (IU) are both related to problematic smartphone use (PSU) severity. However, research about the mediating effect of IU from social anxiety to PSU is limited. Methods: We conducted a
[...] Read more.
Objectives: Prior research has found that social anxiety and intolerance of uncertainty (IU) are both related to problematic smartphone use (PSU) severity. However, research about the mediating effect of IU from social anxiety to PSU is limited. Methods: We conducted a cross-sectional analysis of self-report online data from 329 college students in the United States, evaluating IU, social anxiety, and PSU through structural equation modeling. Results: We found that confirmatory factor analytic models of social anxiety, IU and PSU each fit well. Our overall structural equation model also indicated good fit, and IU acted as a significant mediator of the link between social anxiety and PSU severity. To test model specificity, we compared it with an alternative model that added a direct path from social anxiety to PSU. Although the alternative model showed slightly better fit, the improvement was minimal, and theoretical grounds supported keeping the simpler initial model. Conclusions: These results indicate that IU may represent a critical cognitive–affective mechanism linking social anxiety to PSU. PSU might function as a coping mechanism for some individuals to alleviate the negative emotion associated with social anxiety and IU.
Full article
(This article belongs to the Special Issue Mental Health: Clinical Advances in Personalized Medicine)
►▼
Show Figures
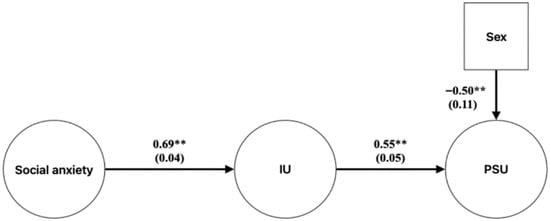
Figure 1
Open AccessReview
Anticipating Clinical Onset in Multiple Sclerosis: Challenges and Opportunities
by
Viviana Nociti and Marina Romozzi
J. Pers. Med. 2025, 15(12), 598; https://doi.org/10.3390/jpm15120598 - 4 Dec 2025
Abstract
Multiple sclerosis (MS) is a chronic, immune-mediated disorder of the central nervous system, increasingly recognized as a disease continuum that begins years before the first neurological event. Genetic susceptibility, environmental exposures, and silent neuroinflammation contribute to early disease activity. Recent studies have highlighted
[...] Read more.
Multiple sclerosis (MS) is a chronic, immune-mediated disorder of the central nervous system, increasingly recognized as a disease continuum that begins years before the first neurological event. Genetic susceptibility, environmental exposures, and silent neuroinflammation contribute to early disease activity. Recent studies have highlighted a preclinical phase that includes both a biological stage, characterized by elevated biomarkers such as serum neurofilament light chain up to 10 years before onset, and a prodromal phase, marked by subtle but measurable symptoms. Population-based cohorts consistently show increased healthcare use, higher prevalence of psychiatric and cognitive disturbances, fatigue, pain, and gastrointestinal disorders years before diagnosis, which may represent prodromal symptoms. Radiologically isolated syndrome (RIS), defined by incidental demyelinating lesions in asymptomatic individuals, represents the visible form of this phase and provides a unique opportunity to study the transition to clinical disease. Approximately half of RIS patients develop MS within a decade, with predictors including younger age, male sex, CSF oligoclonal bands, and spinal cord involvement. Recent randomized controlled trials demonstrated that early use of disease-modifying therapies in RIS significantly reduces conversion risk. Defining the preclinical and prodromal phases of MS offers a major opportunity to refine risk stratification, enable earlier intervention, and ultimately prevent or delay the onset of clinically definite MS.
Full article
(This article belongs to the Special Issue Personalized Therapeutic and Rehabilitation Approaches in Multiple Sclerosis: Challenges and Future Directions)
►▼
Show Figures

Figure 1
Open AccessReview
The Personalized Management of Primary Biliary Cholangitis in the Era of Precision Medicine: Current Challenges and Future Perspectives
by
Mario Romeo, Fiammetta Di Nardo, Claudio Basile, Carmine Napolitano, Paolo Vaia, Giuseppina Martinelli, Alessia De Gregorio, Luigi Di Puorto, Mattia Indipendente, Marcello Dallio and Alessandro Federico
J. Pers. Med. 2025, 15(12), 597; https://doi.org/10.3390/jpm15120597 - 3 Dec 2025
Abstract
Primary biliary cholangitis (PBC) is a heterogeneous autoimmune liver disease in which clinical presentation, disease progression, and response to therapy vary markedly from patient to patient. This heterogeneity reflects its complex, multifactorial, and not-completely elucidated pathogenesis. Currently, serological markers are available to non-invasively
[...] Read more.
Primary biliary cholangitis (PBC) is a heterogeneous autoimmune liver disease in which clinical presentation, disease progression, and response to therapy vary markedly from patient to patient. This heterogeneity reflects its complex, multifactorial, and not-completely elucidated pathogenesis. Currently, serological markers are available to non-invasively diagnose PBC, reserving liver biopsy for selected cases with atypical presentations or diagnostic uncertainty. Anyway, the accurate non-invasive prediction of liver-related and non-liver-related (i.e., extra-hepatic, including pruritus) outcomes remains an open challenge, as well as an urgent need, considering the great variability in clinical course and prognosis reported in PBC patients. Moreover, although ursodeoxycholic acid (UDCA) remains the standard first-line treatment, not all individuals respond equally, either in terms of therapeutic efficacy or timing of biochemical improvement. This further variability in treatment response underscores the inadequacy of uniform management approaches and reinforces the urgent need for personalized medicine, where treatment decisions are guided by patient-specific biological and clinical parameters. In this scenario, the identification and validation of non-invasive predictive biomarkers capable of detecting early therapeutic responsiveness are pivotal for optimizing care pathways. Finally, a growing portion of patients show an insufficient UDCA response or are UDCA intolerant, making the identification of novel strategies of care an urgent need. Concerning this, very recently, new therapeutic options beyond UDCA targeting, among the other pathways, bile acid metabolism (including the modern Peroxisome Proliferator-Activated Receptor agonists), immune regulation, and fibrogenesis, have expanded the treatment landscape. In the Era of Precision Medicine, these diagnostic, prognostic, and therapeutic innovations, by reflecting the complexity of PBC pathogenesis, underline the cruciality of a patient-tailored strategy to improve outcomes and mitigate disease progression. The present review reports recent advances, highlights ongoing challenges, and outlines future perspectives in the management of PBC.
Full article
(This article belongs to the Special Issue Novel Challenges and Therapeutic Options for Digestive and Liver Diseases—2nd Edition)
►▼
Show Figures

Figure 1
Open AccessReview
The Search for Predictive Biomarkers in Response to Immune Checkpoint Inhibitors and Associated Adverse Events
by
Marco Agostini, Pietro Traldi and Mahmoud Hamdan
J. Pers. Med. 2025, 15(12), 596; https://doi.org/10.3390/jpm15120596 - 3 Dec 2025
Abstract
The introduction of immune checkpoint inhibitors (ICIs) as a part of immunotherapy represented a therapeutic breakthrough in the landscape of cancer treatment. The action of these inhibitors consists of blocking certain inhibitory receptors in the immune system. Blocking these inhibitory pathways, ICIs induce
[...] Read more.
The introduction of immune checkpoint inhibitors (ICIs) as a part of immunotherapy represented a therapeutic breakthrough in the landscape of cancer treatment. The action of these inhibitors consists of blocking certain inhibitory receptors in the immune system. Blocking these inhibitory pathways, ICIs induce an enhanced T cell-mediated response necessary to neutralize tumor cells. Over the last 10 years, programmed death cell protein1 (PD-1), PD ligand 1 (PD-L1), and cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) have been among the inhibitory receptors most targeted by ICIs. Currently, this innovative therapeutic approach faces two major challenges: early identification of cancer patients who are likely to get a significant therapeutic benefit through the use of these inhibitors, and the second challenge is the early prediction of likely immune-related adverse events (irAEs) associated with such therapy. The aim of the present text is to discuss the current research efforts to discover and develop much needed effective biomarkers, which may represent an important step towards more efficient and risk-free immunotherapy. We also highlight the increasing role in clinical analyses of liquid biopsy sampling combined with mass spectrometry-based proteomics and how such combination is contributing to current research efforts to enhance the role of immunotherapy.
Full article
(This article belongs to the Special Issue Recent Developments in Cancer Biomarkers for Diagnosis and Prognosis)
►▼
Show Figures
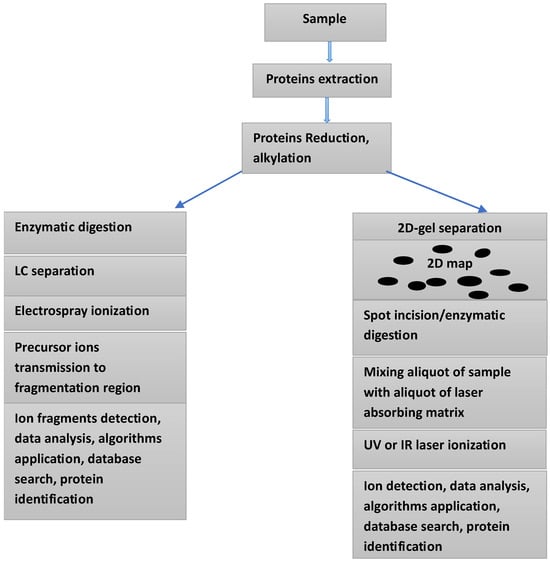
Figure 1
Open AccessReview
Heart Failure and Cognitive Impairment Through the Lens of the Gut Microbiome: A Narrative Review
by
Ali Reza Rahmani, Seyed Avid Madani, Ethan Aminov, Lasha Gogokhia, Travis Bench and Andreas Kalogeropoulos
J. Pers. Med. 2025, 15(12), 595; https://doi.org/10.3390/jpm15120595 - 3 Dec 2025
Abstract
Heart failure (HF) affects over 55 million individuals globally, with prevalence projected to exceed 11 million in the United States by 2050 and is increasingly recognized as a systemic disorder extending beyond hemodynamic dysfunction to encompass profound alterations in neural and gut physiology.
[...] Read more.
Heart failure (HF) affects over 55 million individuals globally, with prevalence projected to exceed 11 million in the United States by 2050 and is increasingly recognized as a systemic disorder extending beyond hemodynamic dysfunction to encompass profound alterations in neural and gut physiology. Cognitive impairment affects nearly half of HF patients and represents a major determinant of morbidity, self-care capacity, and mortality. Recent advances suggest that the gut microbiome serves as a pivotal intermediary in the heart–brain crosstalk, influencing neurocognitive outcomes through inflammatory, metabolic, and neurohumoral pathways. Dysbiosis in HF disrupts intestinal barrier integrity, facilitating translocation of endotoxins and microbial metabolites such as trimethylamine-N-oxide (TMAO), short-chain fatty acids (SCFAs), and bile acids, which in turn modulate neuroinflammation, cerebral perfusion, and neuronal signaling. The gut–heart–brain axis provides an integrative framework linking HF and cognitive impairment pathophysiology through dysbiosis-driven systemic inflammation and metabolite dysregulation. Gut-derived biomarkers and microbiome-targeted interventions represent promising strategies for detection of early alterations and precision treatment, highlighting the urge for prospective, multi-omics studies to establish causality and therapeutic efficacy. This review synthesizes current evidence connecting gut microbiome dysbiosis and metabolite alterations to both HF and cognitive impairment pathophysiology and proposes translational strategies for integrating microbiome-targeted therapies in HF patients with cognitive dysfunction.
Full article
(This article belongs to the Special Issue Personalized Management of Heart Failure: From Biomarkers to Clinical Practice)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Role of Polymer-Free Drug-Eluting Stents in Insulin-Dependent Diabetic Patients Undergoing Percutaneous Coronary Intervention: An Observational Study
by
Filippo Luca Gurgoglione, Davide Donelli, Marco Frazzetto, Luigi Vignali, Giorgio Benatti, Iacopo Tadonio, Andrea Denegri, Marco Covani, Mattia De Gregorio, Gabriella Dallaglio, Giampaolo Niccoli, Bernardo Cortese and Emilia Solinas
J. Pers. Med. 2025, 15(12), 594; https://doi.org/10.3390/jpm15120594 - 3 Dec 2025
Abstract
Background/Objectives: Diabetes mellitus (DM), especially insulin-dependent DM (IDDM), is strongly associated with adverse outcomes following percutaneous coronary intervention (PCI) failure. Polymer-free drug-eluting stents (PF-DESs) have emerged as a promising strategy to mitigate long-term coronary inflammation. This study aimed to evaluate the role
[...] Read more.
Background/Objectives: Diabetes mellitus (DM), especially insulin-dependent DM (IDDM), is strongly associated with adverse outcomes following percutaneous coronary intervention (PCI) failure. Polymer-free drug-eluting stents (PF-DESs) have emerged as a promising strategy to mitigate long-term coronary inflammation. This study aimed to evaluate the role of PF-DES, as compared to permanent-polymer DES (PP-DES) and biodegradable-polymer DES (BP-DES), in a real-world cohort of IDDM patients with obstructive coronary artery disease (CAD) undergoing PCI. Methods: IDDM patients with CAD who underwent PCI with DES at Parma University Hospital were divided into two study groups: PF-DES group vs. BP/PP-DES group. The primary endpoint was target vessel failure (TVF) at the 4-year follow-up. Survival analyses and propensity score matching (PSM) were performed to account for baseline differences. Results: A total of 170 IDDM patients with 215 treated lesions (31.6% PF-DES; 68.4% BP/PP-DES) were included. The PF-DES group experienced significantly lower rates of TVF (10.3% vs. 27.2%, p < 0.01, log rank p = 0.0072) compared with the BP/PP-DES group. PSM analysis confirmed the good clinical performance of PF-DES (HR 0.27, p < 0.01). Conclusions: In this PSM-based observational study, PF-DESs were associated with significantly lower rates of TVF compared with BP/PP-DESs in IDDM patients undergoing PCI for CAD. These suggest that PF-DES may represent a personalized PCI strategy for IDDM patients, with prognostic benefits that become increasingly pronounced as the clinical and anatomical risk profile worsens.
Full article
(This article belongs to the Special Issue Personalized Prevention and Treatment of Cardiovascular Diseases)
►▼
Show Figures
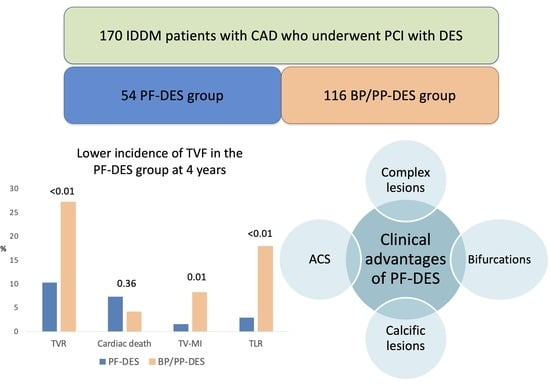
Graphical abstract
Open AccessArticle
Extracranial Hemodynamic Responses to a Noxious Cold Pressor Task Differ Between Persistent Post-Traumatic Headache and Healthy Controls
by
Aaron W. Parr, David B. Berry, Bahar Shahidi, Dawn M. Schiehser and Katrina S. Monroe
J. Pers. Med. 2025, 15(12), 593; https://doi.org/10.3390/jpm15120593 - 3 Dec 2025
Abstract
Background/Objectives: Headache after a traumatic brain injury (TBI) is one of the most common post-concussive symptoms and is associated with altered pain processing and elevated disability levels. Understanding physiologic correlates of nociception in individuals with persistent post-traumatic headache (pPTH) may help identify novel
[...] Read more.
Background/Objectives: Headache after a traumatic brain injury (TBI) is one of the most common post-concussive symptoms and is associated with altered pain processing and elevated disability levels. Understanding physiologic correlates of nociception in individuals with persistent post-traumatic headache (pPTH) may help identify novel treatment targets for pain-related disability. The objective of this case–control study was to compare extra- and intracranial hemodynamic responses to a noxious cold pressor task (CPT) between individuals with pPTH and healthy controls (HC) using functional near-infrared spectroscopy (fNIRS). Methods: Ten individuals with pPTH were compared to ten HC with no history of TBI, persistent headache, or chronic pain. fNIRS optodes over the medial prefrontal cortex (PFC) measured extra- and intracranial peak-to-peak hemodynamic responses during tepid- (control) and cold-water (CPT) hand immersion. Evoked pain responses during the CPT were assessed with numeric pain ratings. Linear mixed effects modeling assessed the role of group and evoked pain on hemodynamic responses. Results: pPTH group membership (p = 0.031) predicted greater extracranial hemodynamic responses to the CPT, whereas intracranial PFC responses did not differ between groups. Regardless of group membership, greater increases in pain intensity during the CPT were associated with increased hemodynamic responses for the dorsomedial PFC (p = 0.031). Conclusions: Compared to controls, individuals with pPTH responded to a noxious cold stimulus with elevated systemic hemodynamic responses regulated by the autonomic nervous system. Irrespective of group, hemodynamic responses within the dmPFC were associated with evoked pain responses to the CPT and may provide a useful biomarker for individual variations in cortical pain processing for healthy and clinical populations.
Full article
(This article belongs to the Section Disease Biomarkers)
►▼
Show Figures
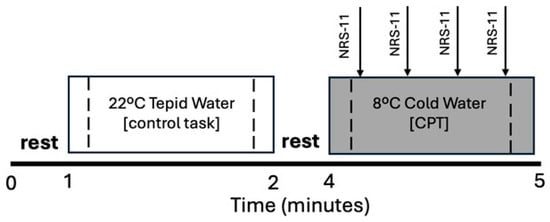
Figure 1
Open AccessReview
When Blood Remembers Its Sex: Toward Truly Personalized Transfusion Medicine
by
Sotirios P. Fortis, Styliani Kokoris, Pavlos Kelepousidis, Georgios Dryllis, Maria-Aspasia Kosma, Theodoros Pittaras, Anastasios G. Kriebardis and Serena Valsami
J. Pers. Med. 2025, 15(12), 592; https://doi.org/10.3390/jpm15120592 - 3 Dec 2025
Abstract
Background: Biological sex differences are well-recognized as non-negligible factors in implementing precision medicine practice. Sex chromosomes influence protein expression and signaling, and thus cellular pathways are often regulated differently. Additionally, the importance of sex as a biological variable has gained significant traction
[...] Read more.
Background: Biological sex differences are well-recognized as non-negligible factors in implementing precision medicine practice. Sex chromosomes influence protein expression and signaling, and thus cellular pathways are often regulated differently. Additionally, the importance of sex as a biological variable has gained significant traction in biomedical research, including transfusion medicine. Regarding transfusion medicine, several studies reveal the role of gender in blood transfusion, blood donors’ behavior towards donation, blood products’ composition and storage, transfusion therapy, and possibly post-transfusion patient outcomes. Methods: In this review, the role of sex and gender in the whole transfusion chain (from the blood donor to the blood product and the patient) is assessed and summarized using data from observational studies, registry analyses, and randomized trials. Results: Female donors face higher deferral rates due to biological factors (iron deficiency, low hemoglobin, pregnancy) and sociocultural factors (caregiving responsibilities, misinformation). However, women are more likely to donate based on empathy, moral duty, or community responsibility and are more consistent in sustaining voluntary donation during crises. Men donate more frequently, typically driven by external motivators, and provide red blood cell (RBC) products with higher hemoglobin content, whereas RBCs from female donors exhibit greater metabolic stability and reduced hemolysis during storage. Plasma from multiparous women possibly contains alloantibodies associated with adverse transfusion reactions, namely transfusion-related acute lung injury (TRALI). Platelet function also varies by sex, though its possible clinical impact is still unknown. Although observational studies suggest sex-mismatched transfusions are associated with increased morbidity and mortality—particularly in transfusions from female donors to male recipients—large registries and randomized controlled trials show inconsistent or negligible effect on survival. Conclusions: Donor and recipient sex are emerging variables of possible clinical importance in transfusion practice. Incorporating sex-informed insights into donor recruitment, blood product handling and transfusion policies may improve safety while advancing precision medicine. Further large-scale trials are needed to elucidate the impact of sex in transfusion, identify and eliminate possible risks, and bridge the gap between biological insights and clinical practice.
Full article
(This article belongs to the Special Issue Advances in Transfusion Medicine and Immunological Research)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Cell-in-Cell Structures in Colorectal Cancer: A Proposed Assessment Method and Correlation with Established Poor Prognostic Factors
by
Arseniy Potapov, Ruslan Spashchanskii, Aleksey Kazakov, Anastasiya Shepeleva, Uliana Lisitsa, Marina Bugrova and Irina Druzhkova
J. Pers. Med. 2025, 15(12), 591; https://doi.org/10.3390/jpm15120591 - 3 Dec 2025
Abstract
Background: Cell-in-cell (CIC) structure is a histological picture of a whole cell inside another cell. Homotypic CIC structures formed by cancer cells are consistently demonstrated to be a factor of poor prognosis and resistance to chemo- and immunotherapy in colorectal cancer (CRC).
[...] Read more.
Background: Cell-in-cell (CIC) structure is a histological picture of a whole cell inside another cell. Homotypic CIC structures formed by cancer cells are consistently demonstrated to be a factor of poor prognosis and resistance to chemo- and immunotherapy in colorectal cancer (CRC). However, the absence of a standardized counting method limits the use of this factor in the applied research. Objective: To propose an adapted method for quantifying CIC structures in CRC surgical specimens and to evaluate their correlation with established adverse prognostic factors. Methods: A total of 250 histological slides of surgical specimens from 58 patients with pT1-pT4 colorectal adenocarcinoma were studied. Identification of tumor cells and visualization of CIC structures were performed by immunohistochemistry (CK20). Quantitative assessment was performed on digital scans of H&E stained slides. Quantitative assessment was performed on digital slide scans stained with H&E. CIC structures were counted in 5 fields of view corresponding to a ×40 objective (0.975 mm2). A correlation analysis of CIC structures with CRC poor prognosis factors was performed. Results: Immunohistochemical study (CK20) confirmed the formation and prevalence of homotypic structures (95%) over heterotypic ones (5%) (p < 0.001). This finding informed the evaluation of H&E-stained slides and the formulation of criteria for CIC structure identification. A significant predominance of CIC structures in the invasive front was established compared to the tumor central zone (16.7 ± 5.2 and 1.2 ± 1.3 per 5 fields of view, respectively, p < 0.0001). Correlation analysis revealed weak but statistically significant relationships with the tumor-stromal ratio, the tumor buds number and the density of tumor-infiltrating lymphocytes. No correlations were found with the right- or left-sided location, pTNM, grading, lymphovascular and perineural invasion. Conclusions: The paper presents the adapted CIC structures counting method for surgical specimens of CRC, defines the criteria of the CIC, and demonstrates a higher number of CIC structures in the tumor invasive front. Weak correlations between the CIC structures and established factors of CRC poor prognosis are obtained.
Full article
(This article belongs to the Special Issue Advances in Colorectal Cancer: Diagnosis and Personalized Treatment)
►▼
Show Figures
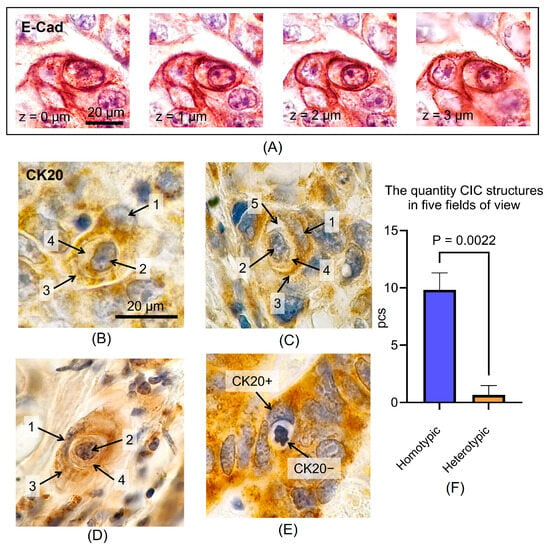
Figure 1
Open AccessArticle
Malignant Eyelid Tumors in Italy (2020–2024): Toward Personalized Epidemiologic Insights from Two Referral Centers
by
Lina Corgiolu, Luca Pilloni, Alessandra Di Maria, Maria Angela Romeo, Alessandro Gaeta, Giuseppe Giannaccare and Alberto Cuccu
J. Pers. Med. 2025, 15(12), 590; https://doi.org/10.3390/jpm15120590 - 2 Dec 2025
Abstract
Background/Objectives: Eyelid malignancies represent a clinically relevant subset of cutaneous tumors of the head and neck, with significant functional and cosmetic implications. While basal cell carcinoma (BCC) is the predominant subtype, geographic differences in the relative frequency of squamous cell carcinoma (SCC) and
[...] Read more.
Background/Objectives: Eyelid malignancies represent a clinically relevant subset of cutaneous tumors of the head and neck, with significant functional and cosmetic implications. While basal cell carcinoma (BCC) is the predominant subtype, geographic differences in the relative frequency of squamous cell carcinoma (SCC) and rarer histotypes have been reported. This study aimed at comparing the distribution of malignant eyelid tumors diagnosed in two Italian referral centers, namely Cagliari (Sardinia) and Milan (Lombardy) between 2020 and 2024, and to explore demographic and epidemiologic correlates. Methods: A total of 250 malignant eyelid tumors were analyzed: 130 from Cagliari and 120 from Milan. BCC was the most common histological subtype overall (83.2%), followed by SCC (12.4%) and other malignancies (4.4%). The proportion of SCC was significantly higher in Milan (18.3%) compared to Cagliari (6.9%, p = 0.04). Logistic regression confirmed Milan as an independent risk factor for SCC (OR 3.79; 95% CI 1.57–9.18; p = 0.003). Male gender also emerged as a predictor of SCC (OR 2.50; 95% CI 1.10–5.67; p = 0.029). Most cases occurred in patients ≥70 years; cases under 50 years were rare (≈3%). Conclusions: BCC remains the predominant malignant eyelid tumor in Italy; significant inter-regional variability exists, with a higher proportion of SCC in northern Italy. These findings highlight the role of environmental, demographic, and organizational factors, and emphasize the need for multicenter registries. Region-specific insights may inform personalized prevention and surveillance strategies for eyelid malignancies. These findings may support the development of region-tailored prevention models and contribute to the growing field of personalized oncology within ophthalmology.
Full article
(This article belongs to the Special Issue Head and Neck Oncologic Surgery: Clinical Updates and New Perspectives in Precision Medicine Era)
►▼
Show Figures
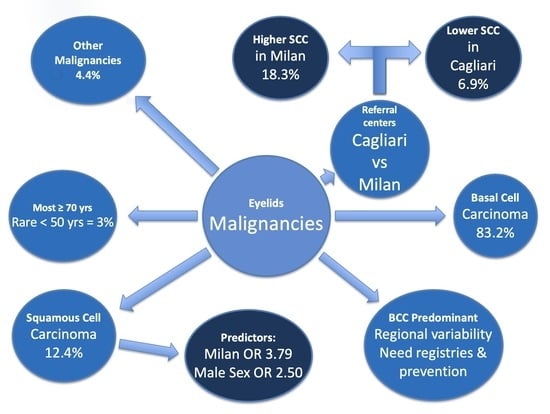
Graphical abstract
Open AccessArticle
Pregnancy and Neonatal Outcomes for Women Without Male Partners Undergoing Fertility Care via Intrauterine Insemination: A Retrospective Cohort Study
by
Wendy Y. Zhang, Megan McCracken, Amy Zhang, Lisandra Veliz Dominguez and Lusine Aghajanova
J. Pers. Med. 2025, 15(12), 589; https://doi.org/10.3390/jpm15120589 - 2 Dec 2025
Abstract
Objective: The objective of this study is to examine the detailed pregnancy and neonatal outcomes of women without male partners undergoing intrauterine insemination (IUI) compared to women with male partners. Methods: This is a retrospective cohort study of all patients who completed an
[...] Read more.
Objective: The objective of this study is to examine the detailed pregnancy and neonatal outcomes of women without male partners undergoing intrauterine insemination (IUI) compared to women with male partners. Methods: This is a retrospective cohort study of all patients who completed an IUI cycle from 2017 to 2023. 2414 cycles were included in the study: 149 cycles for women without male partners (including single and lesbian women) and 2265 cycles for women with male partners. Primary outcomes were the rates of clinical pregnancy, miscarriage, and live birth. Secondary outcomes were obstetric complication rates and neonatal outcomes. Results: Women without male partners undergoing IUI were significantly older than the reference cohort (median age 42 years versus 38 years, p < 0.0001). 84.1% of women without male partners did not have a diagnosis of the common causes of female infertility. Both cohorts had similar cycle characteristics and number of IUI cycles until pregnancy and live birth. The mean clinical pregnancy rate per cycle for women without male partners was 11.4% versus 12.5% for the reference group (p = 0.56), and the mean live birth rate was 8.1% versus 8.2% (p = 0.95). Multiple pregnancy, cumulative pregnancy, and clinical miscarriage rates were also similar. Similarities persisted after adjusting for confounders: age, BMI, race, and infertility diagnosis. Importantly, there were no statistically significant differences in obstetric complications (such as hypertensive disorders of pregnancy, gestational diabetes, placental disorders) and neonatal outcomes. Conclusions: Compared to women with male partners undergoing IUI, women without male partners had similar rates of clinical pregnancy (per cycle and cumulative), miscarriage, and live birth; there were no significant differences in obstetric complications or neonatal outcomes.
Full article
(This article belongs to the Section Personalized Therapy in Clinical Medicine)
►▼
Show Figures

Figure 1
Open AccessArticle
Two-Plate Splintless Repositioning in Bimaxillary Surgery: Accuracy and Influence of Segmental Osteotomies in a Consecutive Single-Centre Cohort
by
Hylke van der Wel, Tom Lucas Zwijnenberg, Johan Jansma, Rutger Hendrik Schepers and Haye Hendrik Glas
J. Pers. Med. 2025, 15(12), 588; https://doi.org/10.3390/jpm15120588 - 2 Dec 2025
Abstract
Background/Objectives: The primary objective of this study was to evaluate the accuracy of maxillary repositioning using a two-plate patient-specific osteosynthesis system. The secondary objective was to determine whether accuracy is influenced by the number of maxillary segments. Methods: A retrospective single-centre
[...] Read more.
Background/Objectives: The primary objective of this study was to evaluate the accuracy of maxillary repositioning using a two-plate patient-specific osteosynthesis system. The secondary objective was to determine whether accuracy is influenced by the number of maxillary segments. Methods: A retrospective single-centre cohort study was conducted on patients undergoing bimaxillary orthognathic surgery with a maxilla-first two-plate PSO system. Virtual Surgical Planning was performed based on the Cone-Beam Computed Tomography (CBCT) data of the patient, with patient-specific plates being designed and manufactured accordingly. Postoperative CBCT scans (7–10 days post-op) were registered to the preoperative plan, and deviations in translation and rotation between the plan and results were determined. Sub-group analyses were performed on one-, two- and three-segment maxillary osteotomy patient groups. Results: The inclusion criteria were met by 61 patients, of whom 47 were included for analysis (mean age 27.9 ± 9.4 years). Sub-millimetre median translational accuracies were found: anteroposterior 0.7 mm, transverse 0.4 mm, vertical 0.6 mm. The median rotational deviations were ≤1° for yaw and roll, and 1.6° for pitch. Accuracy was consistent across the one-, two-, and three-segment osteotomy groups. Conclusions: The two-plate PSO system is clinically accurate in bimaxillary surgery. There is no significant difference in accuracy between one-piece and segmental osteotomies of the maxilla when using the two-plate system.
Full article
(This article belongs to the Section Personalized Medical Care)
►▼
Show Figures
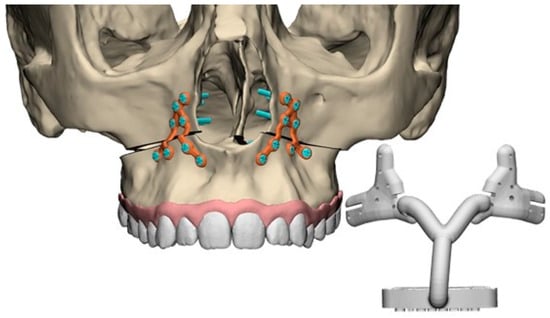
Figure 1

Journal Menu
► ▼ Journal Menu-
- JPM Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal BrowserHighly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Applied Sciences, IJERPH, JCM, JPM, Technologies, Healthcare
Smart Healthcare: Technologies and Applications, 2nd Edition
Topic Editors: Gang Kou, Shuai Ding, Li Luo, Tian Lu, Yogesan KanagasingamDeadline: 20 January 2026
Topic in
Biomedicines, Diagnostics, Endocrines, JCM, JPM, IJMS
Development of Diagnosis and Treatment Modalities in Obstetrics and Gynecology
Topic Editors: Osamu Hiraike, Fuminori TaniguchiDeadline: 20 March 2026
Topic in
Diagnostics, Geriatrics, JCDD, Medicina, JPM, Medicines
New Research on Atrial Fibrillation
Topic Editors: Michele Magnocavallo, Domenico G. Della Rocca, Stefano Bianchi, Pietro Rossi, Antonio BisignaniDeadline: 31 March 2026
Topic in
Healthcare, JCM, JPM, Oral
Advances in Dental Health, 2nd Edition
Topic Editors: Sabina Saccomanno, Gianni GallusiDeadline: 25 July 2026

Conferences
Special Issues
Special Issue in
JPM
Complications in Vascular Surgery: Current Updates and Perspectives
Guest Editor: Yamume TshombaDeadline: 10 December 2025
Special Issue in
JPM
Advances in Oral Health: Innovative and Personalized Approaches
Guest Editors: Eleftherios G. Kaklamanos, Heleni Vastardis, Miltiadis A. MakrygiannakisDeadline: 15 December 2025
Special Issue in
JPM
Plastic Surgery: New Perspectives and Innovative Techniques
Guest Editors: Joseph M. Escandón, Oscar ManriqueDeadline: 20 December 2025
Special Issue in
JPM
Personalized Medicine in Psychiatry: Challenges and Opportunities
Guest Editor: Gniewko WięckiewiczDeadline: 20 December 2025