Semantic Visualization in Functional Recovery Prediction of Intravenous Thrombolysis following Acute Ischemic Stroke in Patients by Using Biostatistics: An Exploratory Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wainwright, J.M.; Murray, V.; Berge, E.; del Zoppo, G.; Sandercock, P.; Lindley, R.L.; Cohen, G. Recombinant tissue plasminogen activator for acute ischaemic stroke: An updated systematic review and meta-analysis. Lancet 2012, 379, 2364–2372. [Google Scholar] [CrossRef]
- Ifejika-Jones, N.L.; Harun, N.; Mohammed-Rajput, N.A.; Noser, E.A.; Grotta, J.C. Thrombolysis with intravenous tissue plasminogen activator predicts a favorable discharge disposition in patients with acute ischemic stroke. Stroke 2011, 42, 700–704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hung, L.-C.; Hu, Y.-H.; Sung, S.-F. Exploring the impact of intravenous thrombolysis on length of stay for acute ischemic stroke: A retrospective cohort study. BMC Health Serv. Res. 2015, 15, 404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, F.-I.; Lien, L.-M.; Chen, S.-T.; Bai, C.-H.; Sun, M.-C.; Tseng, H.-P.; Chen, Y.-W.; Chen, C.-H.; Jeng, J.-S.; Tsai, S.-Y.; et al. Get with the guidelines-stroke performance indicators: Surveillance of stroke care in the Taiwan stroke registry get with the guidelines-stroke in Taiwan. Circulation 2010, 122, 1116–1123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, C.-Y.; Chen, C.-H.; Chen, Y.-C.; Yang, Y.-H.K. National survey of thrombolytic therapy for acute ischemic stroke in Taiwan 2003–2010. J. Stroke Cerebrovas. Dis. 2013, 22, e620–e627. [Google Scholar] [CrossRef]
- Alshekhlee, A.; Mohammadi, A.; Mehta, S.; Edgell, R.C.; Vora, N.; Feen, E.; Kale, S.; Shakir, Z.A.; Cruz-Flores, S. Is thrombolysis safe in the elderly? Analysis of a national database. Stroke 2010, 41, 2259–2264. [Google Scholar] [CrossRef]
- Strbian, D.; Meretoja, A.; Ahlhelm, F.; Pitkäniemi, J.; Lyrer, P.; Kaste, M.; Tatlisumak, T. Predicting outcome of IV thrombolysis–treated ischemic stroke patients The DRAGON score. Neurology 2012, 78, 427–432. [Google Scholar] [CrossRef]
- Saposnik, G.; Guzik, A.K.; Reeves, M.; Ovbiagele, B.; Johnston, S.C. Stroke Prognostication using Age and NIH Stroke Scale SPAN-100. Neurology 2013, 80, 21–28. [Google Scholar] [CrossRef] [Green Version]
- Cheng, C.-A.; Chien, W.-C.; Hsu, C.-Y.; Lin, H.-C.; Chiu, H.-W. Risk analysis of carotid stent from a population-based database in Taiwan. Medicine 2016, 95, e4747. [Google Scholar] [CrossRef]
- Iasonos, A.; Schrag, D.; Raj, G.V.; Panageas, K.S. How to build and interpret a nomogram for cancer prognosis. J. Clin. Oncol. 2008, 26, 1364–1370. [Google Scholar] [CrossRef]
- König, I.R.; Ziegler, A.; Bluhmki, E.; Hacke, W.; Bath, P.M.; Sacco, R.L.; Diener, H.C.; Weimer, C. Predicting long-term outcome after acute ischemic stroke a simple index works in patients from controlled clinical trials. Stroke 2008, 39, 1821–1826. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Chiodini, P.; Ceriello, A.; Giugliano, D. A nomogram to estimate the proportion of patients at hemoglobin A1c target < 7% with noninsulin antidiabetic drugs in type 2 diabetes: A systematic review of 137 randomized controlled trials with 39 845 patients. Acta Diabetol. 2014, 51, 305–311. [Google Scholar] [PubMed]
- Yeo, L.L.; Chien, S.-C.; Lin, J.-R.; Liow, C.-W.; Lee, J.-D.; Peng, T.-I.; Luen, T.H.; Sharma, V.; Chan, B.; Lee, T.-H. Derivation and Validation of a Scoring System for Intravenous Tissue Plasminogen Activator Use in Asian Patients. J. Stroke Cerebrovas. Dis. 2017, 26, 1695–1703. [Google Scholar] [CrossRef]
- Park, H.; Baek, J.-H.; Kim, B.M. Endovascular Treatment of Acute Stroke due to Intracranial Atherosclerotic Stenosis–Related Large Vessel Occlusion. Front. Neurol. 2019, 10, 308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrell, F. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis; Springer: Berlin/Heidelberg, Germany, 2015. [Google Scholar]
- Hendriksen, J.; Geersing, G.; Moons, K.; Groot, J.A. Diagnostic and prognostic prediction models. J. Thromb. Haemost. 2013, 11, 129–141. [Google Scholar] [CrossRef]
- Lee, Y.-H.; Bang, H.; Kim, D.J. How to establish clinical prediction models. Endocrinol. Metab. 2016, 31, 38–44. [Google Scholar] [CrossRef]
- Price, C.I.; Rae, V.; Duckett, J.; Wood, R.; Gray, J.; McMeekin, P.; Rodgers, H.; Portas, K.; Ford, G.A. An observational study of patient characteristics associated with the mode of admission to acute stroke services in North East, England. PLoS ONE 2013, 8, e76997. [Google Scholar] [CrossRef] [Green Version]
- Saposnik, G.; Di Legge, S.; Webster, F.; Hachinski, V. Predictors of major neurologic improvement after thrombolysis in acute stroke. Neurology 2005, 65, 1169–1174. [Google Scholar] [CrossRef]
- Lou, M.; Safdar, A.; Mehdiratta, M.; Kumar, S.; Schlaug, G.; Caplan, L.; Searls, D.; Selim, M. The HAT Score A simple grading scale for predicting hemorrhage after thrombolysis. Neurology 2008, 71, 1417–1423. [Google Scholar] [CrossRef] [Green Version]
- Hu, H. Taiwan Guidelines for the Management of Stroke 2008. Taiwan Stroke Soc. Taipei 2008. [Google Scholar]
- Menon, B.K.; Saver, J.L.; Prabhakaran, S.; Reeves, M.; Liang, L.; Olson, D.M.; Peterson, E.D.; Hernandez, A.F.; Fonarow, G.C.; Schwamm, L.H.; et al. Risk score for intracranial hemorrhage in patients with acute ischemic stroke treated with intravenous tissue-type plasminogen activator. Stroke 2012, 43, 2293–2299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chao, A.-C.; Hsu, H.-Y.; Chung, C.-P.; Liu, C.-H.; Chen, C.-H.; Teng, M.M.-H.; Peng, G.-S.; Sheng, W.-Y.; Hu, H.H. Outcomes of thrombolytic therapy for acute ischemic stroke in Chinese patients the Taiwan thrombolytic Therapy for Acute Ischemic Stroke (TTT-AIS) Study. Stroke 2010, 41, 885–890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saposnik, G.; Fang, J.; Kapral, M.K.; Tu, J.V.; Mamdani, M.; Austin, P.; Johnston, C. The iScore predicts effectiveness of thrombolytic therapy for acute ischemic stroke. Stroke 2012, 43, 1315–1322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ntaios, G.; Faouzi, M.; Ferrari, J.; Lang, W.; Vemmos, K.; Michel, P. An integer-based score to predict functional outcome in acute ischemic stroke The ASTRAL score. Neurology 2012, 78, 1916–1922. [Google Scholar] [CrossRef]
- Ntaios, G.; Gioulekas, F.; Papavasileiou, V.; Strbian, D.; Michel, P. ASTRAL, DRAGON and SEDAN scores predict stroke outcome more accurately than physicians. Eur. J. Neurol. 2016, 23, 1651–1657. [Google Scholar] [CrossRef] [PubMed]
- Pexman, J.W.; Barber, P.A.; Hill, M.D.; Sevick, R.J.; Demchuk, A.M.; Hudon, M.E.; Hu, W.Y.; Buchan, A.M. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. Am. J. Neuroradiol. 2001, 22, 1534–1542. [Google Scholar]
- Asuzu, D.; Nyström, K.; Schindler, J.; Wira, C.; Greer, D.; Halliday, J.; Sheth, K.N. TURN score predicts 90-day outcome in acute ischemic stroke patients after IV thrombolysis. Neurocrit. Care 2015, 23, 172–178. [Google Scholar] [CrossRef]
- Möbius, C.; Blinzler, C.; Schwab, S.; Köhrmann, M.; Breuer, L. Re-evaluation of the stroke prognostication using age and NIH Stroke Scale index (SPAN-100 index) in IVT patients-the-SPAN 10065 index. BMC Neurol. 2018, 18, 129. [Google Scholar] [CrossRef]
- Osaki, M.; Miyashita, F.; Koga, M.; Fukuda, M.; Shigehatake, Y.; Nagatsuka, K.; Minematsu, K.; Toyoda, K. Simple clinical predictors of stroke outcome based on National Institutes of Health Stroke Scale score during 1-h recombinant tissue-type plasminogen activator infusion. Eur. J. Neurol. 2014, 21, 411–418. [Google Scholar] [CrossRef]
- Cooray, C.; Fekete, K.; Mikulik, R.; Lees, K.R.; Wahlgren, N.; Ahmed, N. Threshold for NIH stroke scale in predicting vessel occlusion and functional outcome after stroke thrombolysis. Int. J. Stroke 2015, 10, 822–829. [Google Scholar] [CrossRef]
- Toyoda, K.; Koga, M.; Naganuma, M.; Shiokawa, Y.; Nakagawara, J.; Furui, E.; Kimura, K.; Yamagami, H.; Okada, Y.; Hasegawa, Y.; et al. Routine use of intravenous low-dose re-combinant tissue plasminogen activator in Japanese patients. Stroke 2009, 40, 3591–3595. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.-A.; Cheng, C.G.; Lin, H.-C.; Lee, J.-T.; Lin, H.C.; Cheng, C.C.; Chien, W.-C.; Chiu, H.-W. New-onset atrial fibrillation-related ischemic stroke occurring after hospital discharge in septicemia survivors. QJM Int. J. Med. 2017, 110, 453–457. [Google Scholar] [CrossRef]
- Liu, C.-C.; Chen, Y.-H.; Chang, Y.-H.; Chien, W.-C.; Lin, H.-C.; Cheng, C.-G.; Cheng, C.-A. New-Onset Atrial Fibrillation Is a Risk Factor of Ischemic Stroke in Chronic Obstructive Pulmonary Disease. Healthcare 2022, 10, 381. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.; See, L.; Tu, H.; Yeh, Y.; Chang, S.; Wu, L.; Lee, H.; Wang, C.; Kuo, C.; Kuo, C. Efficacy and Safety of Apixaban, Dabigatran, Rivaroxaban, and Warfarin in Asians with Nonvalvular Atrial Fibrillation. J. Am. Heart Assoc. 2018, 7, e008150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whiteley, W.N.; Thompson, D.; Murray, G.; Cohen, G.; Lindley, R.I.; Wardlaw, J.; Sandercock, P. Targeting Recombinant Tissue-Type Plasminogen Activator in Acute Ischemic Stroke Based on Risk of Intracranial Hemorrhage or Poor Functional Outcome An Analysis of the Third International Stroke Trial. Stroke 2014, 45, 1000–1006. [Google Scholar] [CrossRef] [Green Version]
- Aoki, S.; Hosomi, N.; Sueda, Y.; Kono, T.; Takamatsu, K.; Ohyama, H.; Torii, T.; Kitamura, T.; Nomura, E.; Noda, K.; et al. Multicenter Study of Intravenous Recombinant Tissue Plasminogen Activator Infusion around Hiroshima, Japan: The Hiroshima Acute Stroke Retrospective and Prospective Registry Study. J. Stroke Cerebrovasc. Dis. 2015, 24, 2747–2753. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Unfavorable (66) | Favorable (65) | p | |
|---|---|---|---|
| Age | 67.29 ± 9.98 | 59.94 ± 12.99 | 0.0004 * |
| NIHSS score | 18(7–25) | 13(7–27) | <0.0001 * |
| Hemoglobin | 13.98 ± 1.70 | 14.21 ± 1.65 | 0.432 |
| Onset of treatment time | 136 ± 34 | 123 ± 38 | 0.048 * |
| Dose (mg/kgw) | 0.68 ± 0.1 | 0.67 ± 0.12 | 0.539 |
| Estimated GFR | 78.18 ± 27.75 | 88.53 ± 31.18 | 0.047 * |
| Gender (Male) | 38 (57.6%) | 40 (61.5%) | 0.776 |
| ICA occlusion | 10 (15.2%) | 7 (10.8%) | 0.627 |
| Hypertension | 51 (77.3%) | 39 (60%) | 0.052 |
| Diabetes mellitus | 17 (25.8%) | 9 (13.8%) | 0.136 |
| Previous stroke | 8 (12.1%) | 12 (18.5%) | 0.444 |
| Hyperlipidemia | 44 (66.7%) | 49 (75.4%) | 0.365 |
| Coronary artery disease | 17 (25.8%) | 13 (20%) | 0.565 |
| Atrial fibrillation | 33 (50%) | 18 (27.7%) | 0.015 * |
| Anemia | 7 (10.6%) | 7 (10.8%) | 0.8 |
| Middle cerebral artery sign | 21 (31.8%) | 10 (15.4%) | 0.0778 |
| Hospitalization survey | |||
| Stroke type | 0.538 | ||
| Embolic | 34 (51.5%) | 27( 41.5%) | |
| Large vessel | 28 (42.4%) | 25 (38.5%) | |
| Lacunar | 4 (6.1%) | 13 (20%) | |
| Intracranial hemorrhage | 26 (39.4%) | 3 (4.6%) | <0.001 * |
| Training | Validation | p | |
|---|---|---|---|
| Total | 131 | 54 | |
| Age | 63.64 ± 12.1 | 63.74 ± 10.12 | 0.96 |
| NIHSS score | 15 (7–27) | 12 (4–26) | 0.0003 * |
| Gender (Male) | 78 (59.54%) | 26 (48.15%) | 0.287 |
| Recovery | 65 (49.62%) | 39 (72%) | 0.008 * |
| Survival | 116 (88.55%) | 51 (94.44%) | 0.3385 |
| Factors | Odds Ratio (95% C.I.) | p | Adjusted Odds Ratio (95% C.I.) | p |
|---|---|---|---|---|
| Diabetes mellitus | 0.342 (0.122 to 0.956) | 0.033 * | ||
| Age | 0.95 (0.917 to 0.984) | 0.002 * | 0.9477 (0.9155 to 0.9809) | 0.0023 * |
| NIHSS score | 0.861 (0.792 to 0.936) | 0.0002 * | 0.8643 (0.7997 to 0.9342) | 0.0002 * |
| Anemia | 0.611 (0.4228 to 4.325) | 0.61 | ||
| Hypertension | 0.4889 (0.2074 to 1.1523) | 0.0986 | ||
| Gender (Male) | 0.8777 (0.4039 to 1.9072) | 0.7417 | ||
| Previous stroke | 1.8214 (0.5998 to 5.5314) | 0.285 | ||
| Atrial fibrillation | 0.5079 (0.2311 to 1.1164) | 0.0887 | ||
| Middle cerebral artery sign | 0.4181 (0.1741 to 1.0041) | 0.046 * | ||
| Stroke type | ||||
| Embolic | reference | |||
| Lacunar | 4.093 (1.197 to13.992) | 0.025 * | ||
| Large vessel | 1.124 (0.537 to 2.354) | 0.756 |
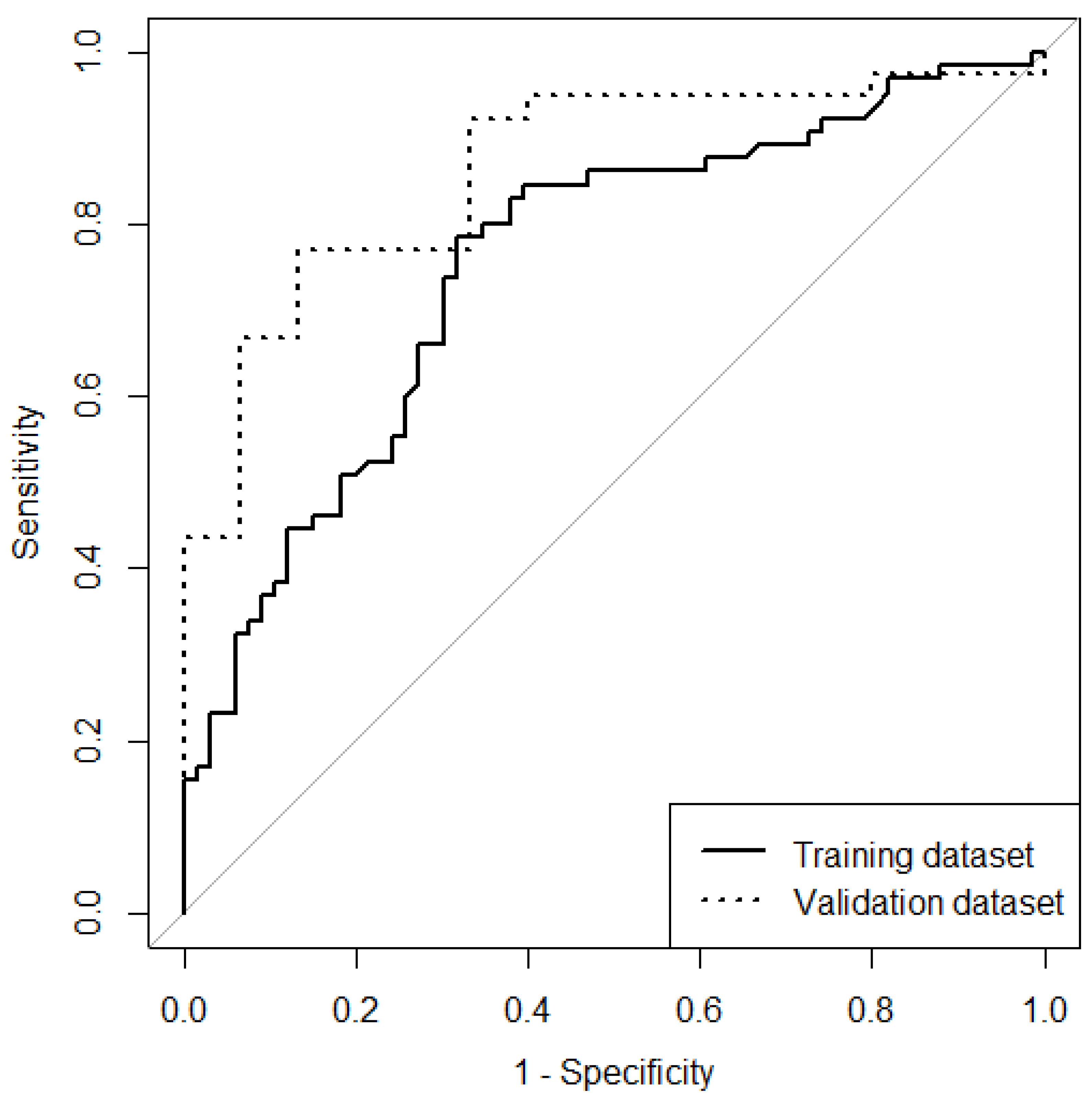
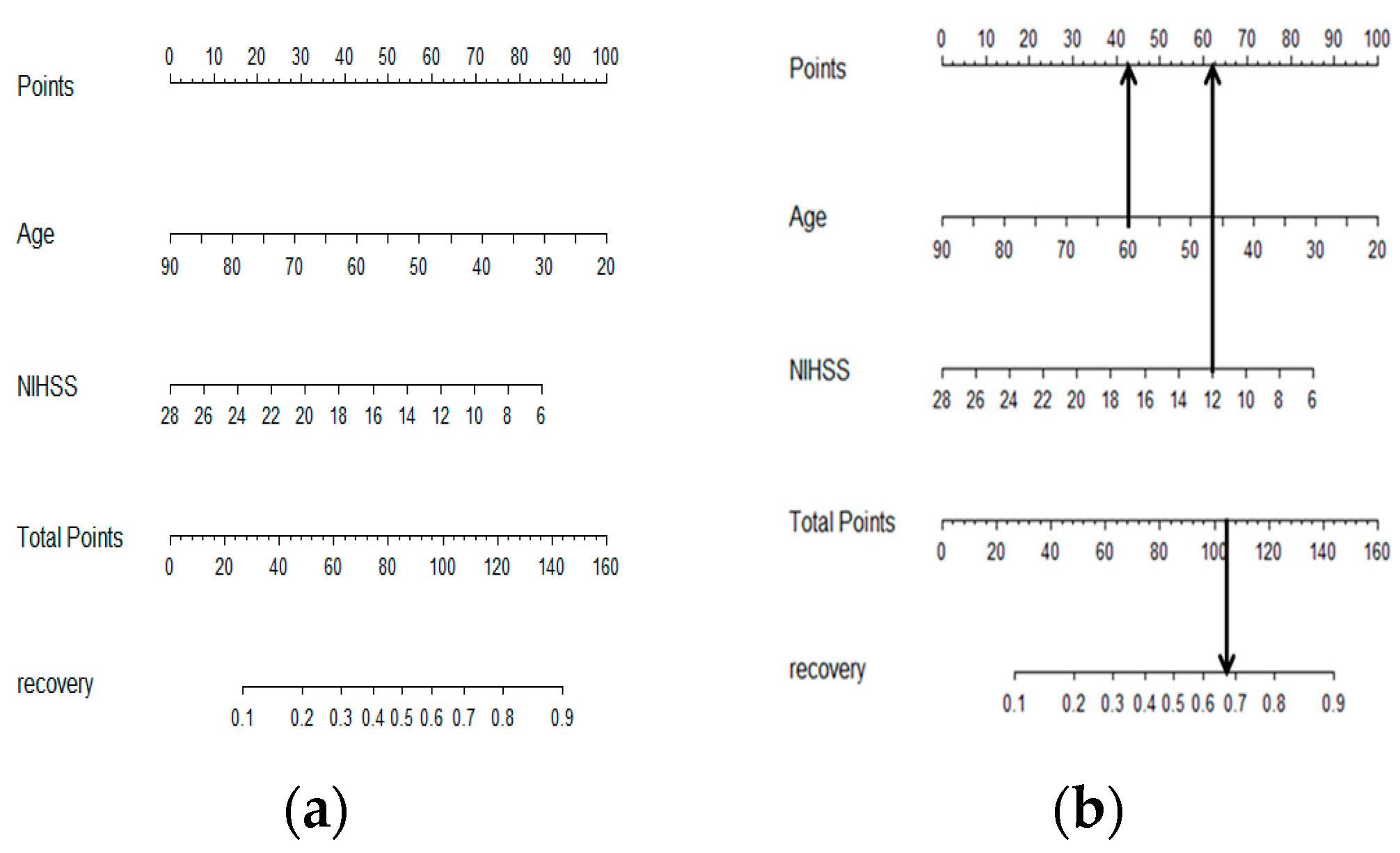
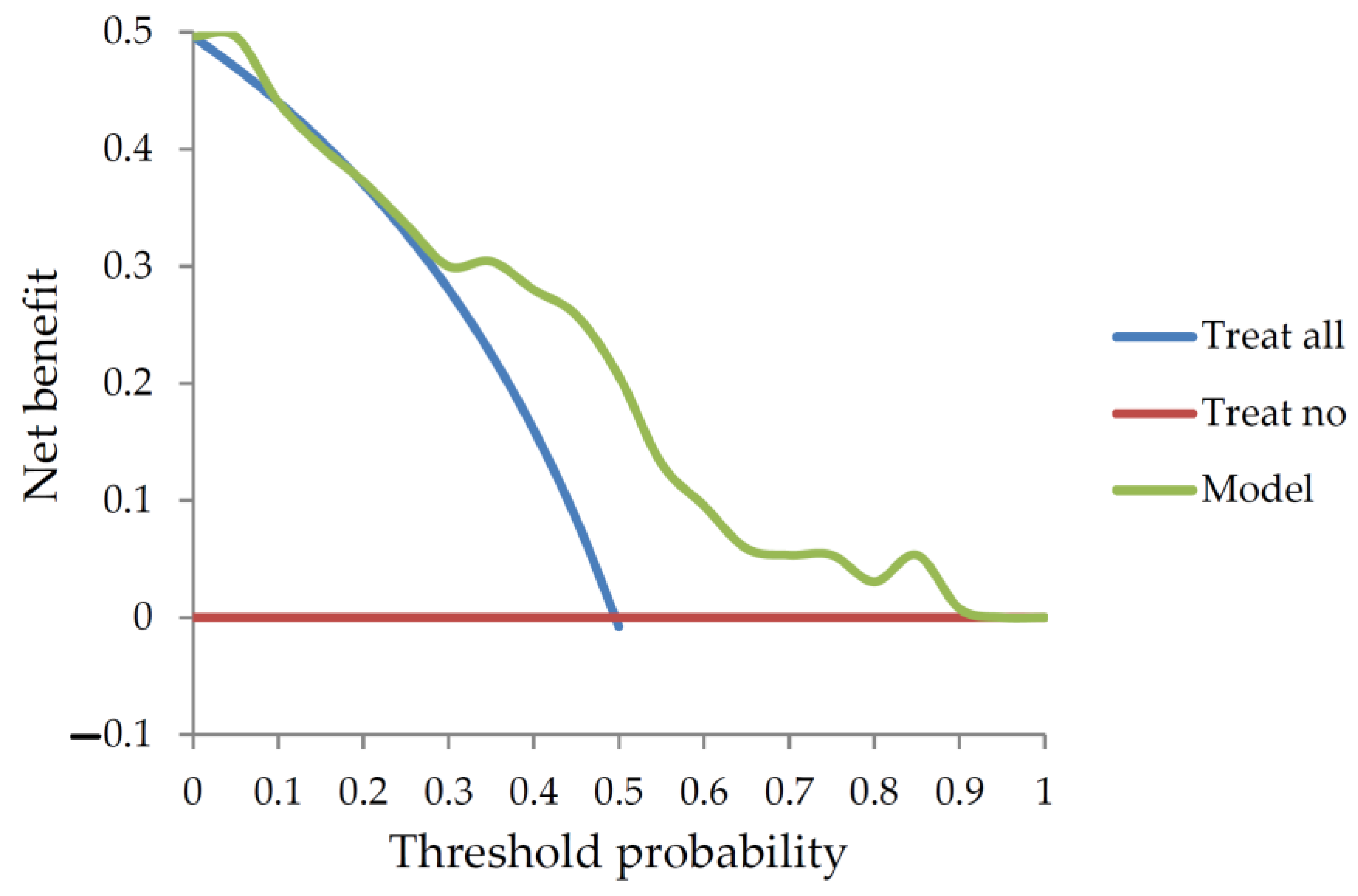
| Parameters | Cases | Sensitivity and Specificity | Area under ROC (95% C.I.) | Probability of Good Outcome | Semantic Visualization | |
|---|---|---|---|---|---|---|
| Current study | Age, NIHSS | Training dataset:131 | 72.31% and 69.1% | 0.753 (0.671–0.825) | Nomogram | Yes |
| Validation dataset:54 | 71.79% and 86.67% | 0.867 (0.765–0.968) | ||||
| SPAN-100 used current datasets (compared with nomogram) | Age + NIHSS = 100 | Training: 0.515 (0.416–0.614), p < 0.001; Validation: 0.533 (0.356–0.711), p < 0.001 | ||||
| NIHSS used current datasets (compared with nomogram) | NIHSS = 12 | Training: 0.659 (0.565–0.753), p = 0.01 Validation: 0.674 (0.515–0.843), p = 0.004 | ||||
| SPAN-100 [8] | Age, NIHSS | 644 | 0.64 | No | ||
| recent SPAN-100 [29] | 1002 | 27% and 96% | 0.74 (0.71–0.77) | No | ||
| Major neurological improvement [19] | Female | 219 | 0.77 (0.7–0.79) | No | ||
| Lack of cortical involvement | ||||||
| Glu < 8 mmol/dL) | ||||||
| DRAGON [7] | Age, Glu, OTT, Dense sign, NIHSS | 1319 | 0.84 (0.8–0.87) | No | ||
| Internal validation: 0.8 (0.74–0.86) | ||||||
| iScore [24] | Age: 1 every one-year-old | 1696 | ≦139: more than 50% | No | ||
| Gender: male:10 | ||||||
| NIHSS: 9–13:40; 14–22:65; >22:105 | ||||||
| Subtype: non-lacunar:30; undeterminated:35 | ||||||
| Af:10 | ||||||
| CHF:10 | ||||||
| Cancer:10 | ||||||
| Dialysis:35 | ||||||
| Dependent:15 | ||||||
| Glu > 150 mg/dl:15 | ||||||
| ASPECTS [27] | Early change of computer tomography of brain: | 156 | 78% and 96% | No | ||
| Basal ganglion involvement:3 | ||||||
| Middle cerebal artery involvement:7 | ||||||
| TURN [28] | −4.65 + (mRS × 0.27) + (NIHSS × 0.1) | 303 | 0.8 (0.74–0.85) | No | ||
| NIHSS [31] | 11632 | 69.4% and 73.4% | 0.775 | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsiao, C.-C.; Cheng, C.-G.; Chen, C.-C.; Chiu, H.-W.; Lin, H.-C.; Cheng, C.-A. Semantic Visualization in Functional Recovery Prediction of Intravenous Thrombolysis following Acute Ischemic Stroke in Patients by Using Biostatistics: An Exploratory Study. J. Pers. Med. 2023, 13, 624. https://doi.org/10.3390/jpm13040624
Hsiao C-C, Cheng C-G, Chen C-C, Chiu H-W, Lin H-C, Cheng C-A. Semantic Visualization in Functional Recovery Prediction of Intravenous Thrombolysis following Acute Ischemic Stroke in Patients by Using Biostatistics: An Exploratory Study. Journal of Personalized Medicine. 2023; 13(4):624. https://doi.org/10.3390/jpm13040624
Chicago/Turabian StyleHsiao, Chih-Chun, Chun-Gu Cheng, Cheng-Chueh Chen, Hung-Wen Chiu, Hui-Chen Lin, and Chun-An Cheng. 2023. "Semantic Visualization in Functional Recovery Prediction of Intravenous Thrombolysis following Acute Ischemic Stroke in Patients by Using Biostatistics: An Exploratory Study" Journal of Personalized Medicine 13, no. 4: 624. https://doi.org/10.3390/jpm13040624






