Joining Forces against Antibiotic Resistance: The One Health Solution
Abstract
:1. Examining the Global Impact of Antibiotic Resistance
- Incomplete Treatment: When individuals do not complete their prescribed antibiotic course, it creates an environment for the survival of the resistant bacteria, leading to the proliferation of resistant strains.
- Use in Agriculture: Antibiotics are extensively used in livestock and agriculture to promote growth and prevent infections in animals. This widespread use contributes to the development of resistant bacteria that can be transmitted to humans through the food chain. In addition, mobile elements conferring antibiotic resistance can move from livestock-associated lineages to human lineages [28,29].
- Global Travel and Trade: Resistant bacteria can spread quickly across borders through international travel and trade, making antibiotic resistance a global issue [30].
- Lack of New Antibiotics: The development of new antibiotics has slowed significantly in recent decades, reducing the arsenal of drugs available to combat resistant infections [31].
- Carbapenem-resistant Acinetobacter
- Clostridioides difficile
- Carbapenem-resistant Enterobacterales (CRE)
- Drug-resistant Neisseria gonorrhoeae
2. Antibiotic Resistance: A Threat to Human and Animal Health
3. Combating Antimicrobial Resistance: A One Health Approach for Global Health Security
4. Collaborative Strategies for Tackling Antibiotic Resistance
5. Prospective and Prevention Strategies
- One Health Governance
- Comprehensive Surveillance Systems
- Stewardship Programs and Education
- Research and Development
- Preventive Measures
- Public Education and Awareness
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- CLSI. Appropriate Reference Is—Performance Standards for Antimicrobial Susceptibility Testing; Approved Standard M100-S20; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020. [Google Scholar]
- MacGowan, A.; Macnaughton, E. Antibiotic resistance. Medicine 2017, 45, 622–628. [Google Scholar] [CrossRef]
- Akova, M. Epidemiology of antimicrobial resistance in bloodstream infections. Virulence 2016, 7, 252–266. [Google Scholar] [CrossRef] [PubMed]
- Frieri, M.; Kumar, K.; Boutin, A. Antibiotic resistance. J. Infect. Public Health 2017, 10, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Buschhardt, T.; Günther, T.; Skjerdal, T.; Torpdahl, M.; Gethmann, J.; Filippitzi, M.-E.; Maassen, C.; Jore, S.; Ellis-Iversen, J.; Filter, M. A one health glossary to support communication and information exchange between the human health, animal health and food safety sectors. One Health 2021, 13, 100263. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, J.S.; Jeggo, M. The One Health Approach—Why Is It So Important? Trop. Med. Infect. Dis. 2019, 4, 88. [Google Scholar] [CrossRef]
- Larsson, D.G.J.; Flach, C.-F. Antibiotic resistance in the environment. Nat. Rev. Genet. 2021, 20, 257–269. [Google Scholar] [CrossRef]
- Berendonk, T.U.; Manaia, C.M.; Merlin, C.; Fatta-Kassinos, D.; Cytryn, E.; Walsh, F.; Bürgmann, H.; Sørum, H.; Norström, M.; Pons, M.N.; et al. Tackling Antibiotic Resistance: The Environmental Framework. Nat. Rev. Microbiol. 2015, 13, 310–317. [Google Scholar] [CrossRef]
- Wellington, E.M.H.; Boxall, A.B.A.; Cross, P.; Feil, E.J.; Gaze, W.H.; Hawkey, P.M.; Johnson-Rollings, A.S.; Jones, D.L.; Lee, N.M.; Otten, W.; et al. The role of the natural environment in the emergence of antibiotic resistance in gram-negative bacteria. Lancet Infect. Dis. 2013, 13, 155–165. [Google Scholar] [CrossRef]
- Bengtsson-Palme, J.; Larsson, D.G.J. Antibiotic resistance genes in the environment: Prioritizing risks. Nat. Rev. Microbiol. 2015, 13, 396. [Google Scholar] [CrossRef]
- Chow, L.K.M.; Ghaly, T.M.; Gillings, M.R. A survey of sub-inhibitory concentrations of antibiotics in the environment. J. Environ. Sci. 2021, 99, 21–27. [Google Scholar] [CrossRef]
- Andersson, D.I.; Balaban, N.Q.; Baquero, F.; Courvalin, P.; Glaser, P.; Gophna, U.; Kishony, R.; Molin, S.; Tønjum, T. Antibiotic resistance: Turning evolutionary principles into clinical reality. FEMS Microbiol. Rev. 2020, 44, 171–188. [Google Scholar] [CrossRef] [PubMed]
- Singer, A.C.; Shaw, H.; Rhodes, V.; Hart, A. Review of antimicrobial resistance in the environment and its relevance to environmental regulators. Front. Microbiol. 2016, 7, 1728. [Google Scholar] [CrossRef] [PubMed]
- Graham, D.W.; Bergeron, G.; Bourassa, M.W.; Dickson, J.; Gomes, F.; Howe, A.; Kahn, L.H.; Morley, P.S.; Scott, H.M.; Sim-jee, S.; et al. Complexities in understanding antimicrobial resistance across domesticated animal, human, and environmental systems. Ann. N. Y. Acad. Sci. 2019, 1441, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Ivančić, I.; Paliaga, P.; Pfannkuchen, M.; Djakovac, T.; Najdek, M.; Steiner, P.; Korlević, M.; Markovski, M.; Baričević, A.; Tanković, M.S.; et al. Environmental dimensions of antibiotic resistance: Assessment of basic science gaps. FEMS Microbiol. Ecol. 2018, 94, fiy195. [Google Scholar] [CrossRef]
- United Nations Environment Programme. Frontiers 2017: Emerging Issues of Environmental Concern. 2017. Available online: https://www.unep.org/resources/frontiers-2017-emerging-issues-environmental-concern (accessed on 23 July 2023).
- European Parliament. Strategic Approach to Pharmaceuticals in the Environment; European Parliament: Strasbourg, France, 2020. [Google Scholar]
- Global Antimicrobial Resistance and Use Surveillance System (GLASS). Available online: https://www.who.int/initiatives/glass (accessed on 14 August 2023).
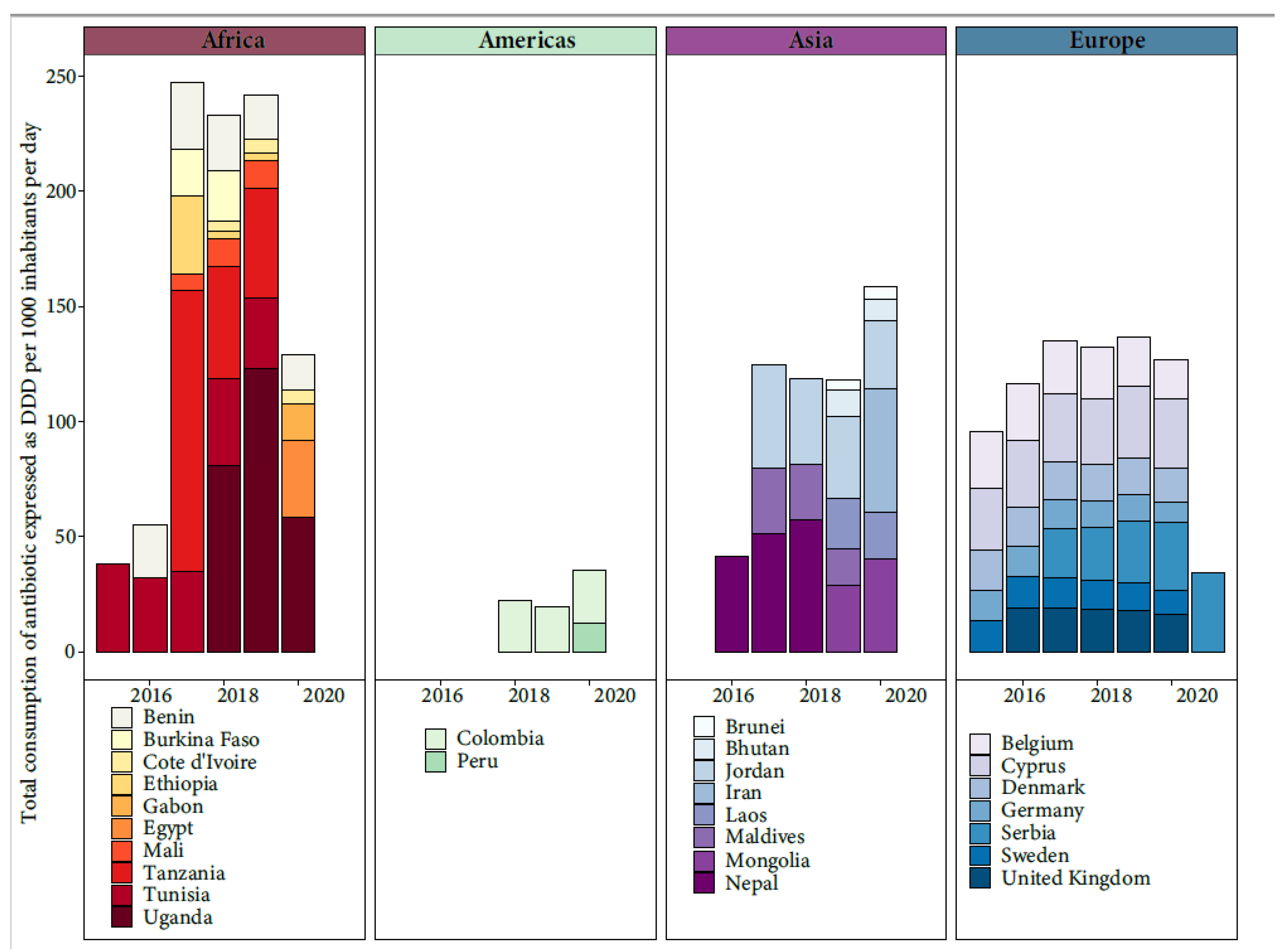
- Sulis, G.; Sayood, S.; Gandra, S. Antimicrobial resistance in low- and middle-income countries: Current status and future directions. Expert Rev. Anti-Infect. Ther. 2021, 20, 147–160. [Google Scholar] [CrossRef]
- Van Boeckel, T.P.; Pires, J.; Silvester, R.; Zhao, C.; Song, J.; Criscuolo, N.G.; Gilbert, M.; Bonhoeffer, S.; Laxminarayan, R. Global trends in antimicrobial resistance in animals in low- and middle-income countries. Science 2019, 365, eaaw1944. [Google Scholar] [CrossRef]
- Ribeiro, S.M.; Felício, M.R.; Boas, E.V.; Gonçalves, S.; Costa, F.F.; Samy, R.P.; Santos, N.C.; Franco, O.L. New frontiers for anti-biofilm drug development. Pharmacol. Ther. 2016, 160, 133–144. [Google Scholar] [CrossRef]
- Lipsitch, M.; Samore, M.H. Antimicrobial use and antimicrobial resistance: A population perspective. Emerg. Infect. Dis. 2002, 8, 347–354. [Google Scholar] [CrossRef]
- Karakonstantis, S.; Kalemaki, D. Antimicrobial overuse and misuse in the community in Greece and link to antimicrobial resistance using methicillin-resistant S. aureus as an example. J. Infect. Public Health 2019, 12, 460–464. [Google Scholar] [CrossRef]
- English, B.K.; Gaur, A.H. The use and abuse of antibiotics and the development of antibiotic resistance. Adv. Exp. Med. Biol. 2010, 659, 73–82. [Google Scholar]
- Chang, Y.; Chusri, S.; Sangthong, R.; McNeil, E.; Hu, J.; Du, W.; Li, D.; Fan, X.; Zhou, H.; Chongsuvivatwong, V.; et al. Clinical pattern of antibiotic overuse and misuse in primary healthcare hospitals in the southwest of China. PLoS ONE 2019, 14, e0214779. [Google Scholar] [CrossRef] [PubMed]
- Ray, M.J.; Tallman, G.B.; Bearden, D.T.; Elman, M.R.; McGregor, J.C. Antibiotic prescribing without documented indication in ambulatory care clinics: National cross sectional study. BMJ 2019, 367, l6461. [Google Scholar] [CrossRef]
- Fleming-Dutra, K.E.; Hersh, A.L.; Shapiro, D.J.; Bartoces, M.; Enns, E.A.; File, T.M.; Finkelstein, J.A.; Gerber, J.S.; Hyun, D.Y.; Linder, J.A.; et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010–2011. JAMA 2016, 315, 1864–1873. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.J.; Thottathil, S.E.; Newman, T.B. Antibiotics Overuse in Animal Agriculture: A Call to Action for Health Care Providers. Am. J. Public Health 2015, 105, 2409–2410. [Google Scholar] [CrossRef] [PubMed]
- Chang, Q.; Wang, W.; Regev-Yochay, G.; Lipsitch, M.; Hanage, W.P. Antibiotics in agriculture and the risk to human health: How worried should we be? Evol. Appl. 2015, 8, 240–247. [Google Scholar] [CrossRef]
- Acar, J.; Röstel, B. Antimicrobial resistance: An overview. Rev. Sci. Tech. 2001, 20, 797–810. [Google Scholar] [CrossRef]
- WHO. Lack of Innovation Set to Undermine Antibiotic Performance and Health Gains. 2022. Available online: https://www.who.int/news/item/22-06-2022-22-06-2022-lack-of-innovation-set-to-undermine-antibiotic-performance-and-health-gains (accessed on 8 July 2023).
- WHO. Antibiotic Resistance. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance (accessed on 8 July 2023).
- CDC. 2019 Antibiotic Resistance Threats Report | CDC. 2019. Available online: https://www.cdc.gov/drugresistance/biggest-threats.html (accessed on 8 July 2023).
- CDC. COVID-19 U.S. Impact on Antimicrobial Resistance—2022 Special Report; CDC: Atlanta, GA, USA, 2022. [Google Scholar]
- McEwen, S.A.; Collignon, P.J. Antimicrobial Resistance: A One Health Perspective. Microbiol. Spectr. 2018, 6, 2. [Google Scholar] [CrossRef]
- Jasovský, D.; Littmann, J.; Zorzet, A.; Cars, O. Antimicrobial resistance-a threat to the world’s sustainable development. Ups. J. Med. Sci. 2016, 121, 159–164. [Google Scholar] [CrossRef]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.M.; Wertheim, H.F.L.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic resistance-the need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef]
- Weese, J.S.; Giguère, S.; Guardabassi, L.; Morley, P.S.; Papich, M.; Ricciuto, D.R.; Sykes, J.E. ACVIM consensus statement on therapeutic antimicrobial use in animals and antimicrobial resistance. J. Vet. Intern. Med. 2015, 29, 487–498. [Google Scholar] [CrossRef]
- Vidovic, N.; Vidovic, S. Antimicrobial Resistance and Food Animals: Influence of Livestock Environment on the Emergence and Dissemination of Antimicrobial Resistance. Antibiotics 2020, 9, 52. [Google Scholar] [CrossRef] [PubMed]
- Larsen, J.; Raisen, C.L.; Ba, X.; Sadgrove, N.J.; Padilla-González, G.F.; Simmonds, M.S.J.; Loncaric, I.; Kerschner, H.; Ap-falter, P.; Hartl, R.; et al. Emergence of methicillin resistance predates the clinical use of antibiotics. Nature 2022, 602, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Harrison, E.M.; Coll, F.; Toleman, M.S.; Blane, B.; Brown, N.M.; Török, M.E.; Parkhill, J.; Peacock, S.J. Genomic surveillance reveals low prevalence of livestock-associated methicillin-resistant Staphylococcus aureus in the East of England. Sci. Rep. 2017, 7, 7406. [Google Scholar] [CrossRef] [PubMed]
- Velazquez-Meza, M.E.; Galarde-López, M.; Carrillo-Quiróz, B.; Alpuche-Aranda, C.M. Antimicrobial resistance: One Health approach. Vet. World 2022, 15, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Cabello, F.C.; Godfrey, H.P.; Tomova, A.; Ivanova, L.; Dölz, H.; Millanao, A.; Buschmann, A.H. Antimicrobial use in aquaculture re-examined: Its relevance to antimicrobial resistance and to animal and human. Health Environ. Microbiol. 2013, 15, 1917–1942. [Google Scholar] [CrossRef]
- Welch, T.J.; Evenhuis, J.; White, D.G.; McDermott, P.F.; Harbottle, H.; Miller, R.A.; Griffin, M.; Wise, D. IncA/C plasmid-mediated florfenicol resistance in the catfish pathogen Edwardsiella ictaluri. Antimicrob. Agents Chemother. 2009, 53, 845–846. [Google Scholar] [CrossRef]
- Booton, R.D.; Meeyai, A.; Alhusein, N.; Buller, H.; Feil, E.; Lambert, H.; Mongkolsuk, S.; Pitchforth, E.; Reyher, K.K.; Sakcamduang, W.; et al. One Health drivers of antibacterial resistance: Quantifying the relative impacts of human, animal and environmental use and transmission. One Health 2021, 12, 100220. [Google Scholar] [CrossRef]
- Manyi-Loh, C.; Mamphweli, S.; Meyer, E.; Okoh, A. Antibiotic Use in Agriculture and Its Consequential Resistance in Environmental Sources: Potential Public Health Implications. Mol. A J. Synth. Chem. Nat. Product. Chem. 2018, 23, 795. [Google Scholar] [CrossRef]
- Majumder, M.A.A.; Rahman, S.; Cohall, D.; Bharatha, A.; Singh, K.; Haque, M.; Gittens-St Hilaire, M. Antimicrobial Stewardship: Fighting Antimicrobial Resistance and Protecting Global Public Health. Infect. Drug Resist. 2020, 13, 4713–4738. [Google Scholar] [CrossRef]
- Allel, K.; Day, L.; Hamilton, A.; Lin, L.; Furuya-Kanamori, L.; Moore, C.E.; Van Boeckel, T.; Laxminarayan, R.; Yakob, L. Global antimicrobial-resistance drivers: An ecological country-level study at the human–animal interface. Lancet Planet. Health 2023, 7, e291–e303. [Google Scholar] [CrossRef]
- Aslam, B.; Khurshid, M.; Arshad, M.I.; Muzammil, S.; Rasool, M.; Yasmeen, N.; Shah, T.; Chaudhry, T.H.; Rasool, M.H.; Shahid, A.; et al. Antibiotic Resistance: One Health One World Outlook. Front. Cell Infect. Microbiol. 2021, 11, 771510. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. European Survelliance of Veterinary Antimicrobial Consumption. Sales of Veterinary Antimicro-bial Agents in 31 European Countries in 2018. 21 October 2020. Tenth ESVAC report. 21 October.
- ECDC/EFSA/EMA. ECDC/EFSA/EMA first joint report on the integrated analysis of the consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from humans and food-producing animals. EFSA J. 2015, 13. [Google Scholar] [CrossRef]
- Van Boeckel, T.P.; Brower, C.; Gilbert, M.; Grenfell, B.T.; Levin, S.A.; Robinson, T.P. Global trends in antimicrobial use in food animals. Proc. Natl. Acad. Sci. USA 2015, 112, 5649–5654. [Google Scholar] [CrossRef] [PubMed]
- McEwen, S.A.; Fedorka-Cray, P.J. Antimicrobial Use and Resistance in Animals. Clin. Infect. Dis. 2002, 34, S93–S106. [Google Scholar] [CrossRef]
- Food and Agriculture Organization (FAO). Drivers, Dynamics and Epidemiology of Antimicrobial Resistance in Animal Production. In Fao. 2016. Available online: http://www.fao.org/documents/card/es/c/d5f6d40d-ef08-4fcc-866b-5e5a92a12dbf/ (accessed on 30 July 2023).
- Reddy, S.B.; Kumari, N.K. Methicillin-resistant Staphylococcus Aureus (MRSA) isolated from dogs with recurrent pyoderma. J. Dairy Vet. Anim. Res. 2016, 3, 62–65. [Google Scholar] [CrossRef]
- Collignon, P.J.; McEwen, S.A. One Health-Its Importance in Helping to Better Control Antimicrobial Resistance. Trop. Med. Infect. Dis. 2019, 4, 22. [Google Scholar] [CrossRef]
- Abushaheen, M.A.; Muzaheed; Fatani, A.J.; Alosaimi, M.; Mansy, W.; George, M.; Acharya, S.; Rathod, S.; Divakar, D.D.; Jhugroo, C.; et al. Antimicrobial resistance, mechanisms and its clinical significance. Dis. Mon. 2020, 66, 100971. [Google Scholar] [CrossRef]
- Scott, H.M.; Acuff, G.; Bergeron, G.; Bourassa, M.W.; Gill, J.; Graham, D.W.; Kahn, L.H.; Morley, P.S.; Salois, M.J.; Simjee, S.; et al. Critically important antibiotics: Criteria and approaches for measuring and reducing their use in food animal agriculture. Ann. N. Y. Acad. Sci. 2019, 1441, 8–16. [Google Scholar] [CrossRef]
- Landers, T.F.; Cohen, B.; Wittum, T.E.; Larson, E.L. A Review of Antibiotic Use in Food Animals: Perspective, Policy, and Potential. Public Health Rep. 2012, 127, 4–22. [Google Scholar] [CrossRef]
- Zay Ya, K.; Win, P.T.N.; Bielicki, J.; Lambiris, M.; Fink, G. Association Between Antimicrobial Stewardship Programs and Antibiotic Use Globally: A Systematic Review and Meta-Analysis. JAMA Netw. Open. 2023, 6, e2253806. [Google Scholar] [CrossRef]
- U.S. National Action Plan for Combating Antibiotic-Resistant Bacteria|CDC. Available online: https://www.cdc.gov/drugresistance/us-activities/national-action-plan.html (accessed on 15 August 2023).
- National Action Plan for Combating Antibiotic-Resistant Bacteria Progress Report: Year 5|ASPE. Available online: https://aspe.hhs.gov/reports/carb-year-5-report (accessed on 15 August 2023).
- Uchil, R.R.; Kohli, G.S.; Katekhaye, V.M.; Swami, O.C. Strategies to combat antimicrobial resistance. J. Clin. Diagn. Res. 2014, 8, ME01–ME04. [Google Scholar] [CrossRef] [PubMed]
- Tacconelli, E.; Carrara, E.; Savoldi, A. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018, 18, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Bordier, M.; Binot, A.; Pauchard, Q.; Nguyen, D.T.; Trung, T.N.; Fortané, N.; Goutard, F.L. Antibiotic resistance in Vietnam: Moving towards a One Health surveillance system. BMC Public Health 2018, 18, 1136. [Google Scholar] [CrossRef] [PubMed]
- AL-Eitan, L.; Sendyani, S.; Alnemri, M. Applications of the One Health concept: Current status in the Middle East. J. Biosaf. Biosecur. 2023, 5, 21–31. [Google Scholar] [CrossRef]
- Mouiche, M.M.M.; Moffo, F.; Akoachere, J.F.T.K.; Okah-Nnane, N.H.; Mapiefou, N.P.; Ndze, V.N.; Wade, A.; Djuikwo-Teukeng, F.F.; Toghoua, D.G.T.; Zambou, H.R.; et al. Antimicrobial resistance from a one health perspective in Cameroon: A systematic review and meta-analysis. BMC Public Health 2019, 19, 1135. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Fu, Y.H.; Sheng, H.J.; Topp, E.; Jiang, X.; Zhu, Y.G.; Tiedje, J.M. Antibiotic resistance in the soil ecosystem: A One Health perspective. Curr. Opin. Environ. Sci. Health 2021, 20, 100230. [Google Scholar] [CrossRef]
- Shabangu, K.; Essack, S.Y.; Duma, S.E. Barriers to implementing National Action Plans on antimicrobial resistance using a One Health Approach: Policymakers’ perspectives from South Africa and Eswatini. J. Glob. Antimicrob. Resist. 2023, 33, 130–136. [Google Scholar] [CrossRef]
- Topp, E. Antimicrobial Resistance and One Health: Agriculture and Agri-Food Canada’s research program on antimicrobial resistance. Can. Commun. Dis. Rep. 2017, 43, 224–227. [Google Scholar] [CrossRef]
- Patel, J.; Sridhar, D. The pandemic legacy of antimicrobial resistance in the USA. Lancet Microbe 2022, 3, e726–e727. [Google Scholar] [CrossRef]
- Yasobant, S.; Bruchhausen, W.; Saxena, D.; Falkenberg, T. One health collaboration for a resilient health system in India: Learnings from global initiatives. One Health 2019, 8, 100096. [Google Scholar] [CrossRef]
- Targeting Innovation in Antibiotic Drug Discovery and Development: The Need for a One Health—One Europe—One World Framework. Available online: https://apps.who.int/iris/handle/10665/326318 (accessed on 15 August 2023).
- Hernando-Amado, S.; Coque, T.M.; Baquero, F.; Martínez, J.L. Antibiotic Resistance: Moving from Individual Health Norms to Social Norms in One Health and Global Health. Front. Microbiol. 2020, 11, 547252. [Google Scholar] [CrossRef]
- Nyokabi, N.S.; Moore, H.; Berg, S.; Lindahl, J.; Phelan, L.; Worku, G.G.; Mihret, A.; Wood, J.L.N. Implementing a one health approach to strengthen the management of zoonoses in Ethiopia. One Health 2023, 16, 100521. [Google Scholar] [CrossRef]
- Shen, L.; Wei, X.; Yin, J.; Haley, D.R.; Sun, Q.; Lundborg, C.S. Interventions to optimize the use of antibiotics in China: A scoping review of evidence from humans, animals, and the environment from a One Health perspective. One Health 2022, 14, 100388. [Google Scholar] [CrossRef] [PubMed]
- Achi, C.R.; Ayobami, O.; Mark, G.; Egwuenu, A.; Ogbolu, D.; Kabir, J. Operationalising One Health in Nigeria: Reflections From a High-Level Expert Panel Discussion Commemorating the 2020 World Antibiotics Awareness Week. Front. Public Health 2021, 9, 673504. [Google Scholar] [CrossRef] [PubMed]
- Cars, O.; Xiao, Y.; Stålsby Lundborg, C.; Nilsson, L.E.; Shen, J.; Sun, Q.; Bi, Z.; Börjesson, S.; Greko, C.; Wang, Y.; et al. Building bridges to operationalise one health—A Sino-Swedish collaboration to tackle antibiotic resistance. One Health 2016, 2, 139–143. [Google Scholar] [CrossRef]
- Marvasi, M.; Casillas, L.; Vassallo, A.; Purchase, D. Educational Activities for Students and Citizens Supporting the One-Health Approach on Antimicrobial Resistance. Antibiotics 2021, 10, 1519. [Google Scholar] [CrossRef]
- Eriksen, J.; Björkman, I.; Röing, M.; Essack, S.Y.; Lundborg, C.S. Exploring the One Health Perspective in Sweden’s Policies for Containing Antibiotic Resistance. Antibiotics 2021, 10, 526. [Google Scholar] [CrossRef] [PubMed]
- Algammal, A.M.; Hetta, H.F.; Elkelish, A.; Alkhalifah, D.H.H.; Hozzein, W.N.; Batiha, G.E.S.; Nahhas, N. El Methicillin-resistant staphylococcus aureus (MRSA): One health perspective approach to the bacterium epidemiology, virulence factors, antibiotic-resistance, and zoonotic impact. Infect. Drug Resist. 2020, 13, 3255–3265. [Google Scholar] [CrossRef]
- Hernández-González, I.L.; Castillo-Ramírez, S. Antibiotic-resistant Acinetobacter baumannii is a One Health problem. Lancet Microbe 2020, 1, e279. [Google Scholar] [CrossRef]
- Price, L.; Gozdzielewska, L.; Young, M.; Smith, F.; MacDonald, J.; McParland, J.; Williams, L.; Langdridge, D.; Davis, M.; Flowers, P. Effectiveness of interventions to improve the public’s antimicrobial resistance awareness and behaviours associated with prudent use of antimicrobials: A systematic review. J. Antimicrob. Chemother. 2018, 73, 1464–1478. [Google Scholar] [CrossRef]
- Gupta, A.; Nelson, J.M.; Barrett, T.J.; Tauxe, R.V.; Rossiter, S.P.; Friedman, C.R.; Joyce, K.W.; Smith, K.E.; Jones, T.F.; Haw-kins, M.A.; et al. Antimicrobial Resistance among Campylobacter Strains, United States, 1997–2001. Emerg. Infect. Dis. 2004, 10, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Engberg, J.; Aarestrup, F.M.; Taylor, D.E.; Gerner-Smidt, P.; Nachamkin, I. Quinolone and macrolide resistance in Campylobacter jejuni and C. coli: Resistance mechanisms and trends in human isolates. Emerg. Infect. Dis. 2001, 7, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.X.; Li, X.C.; Zhang, Q.Y.; Liu, J.S.; Han, L.F.; Lederman, Z.; Schurer, J.M.; Poeta, P.; Rahman, M.T.; Li, S.Z.; et al. Tackling global health security by building an academic community for One Health action. Infect. Dis. Poverty 2023, 12, 70. [Google Scholar] [CrossRef] [PubMed]
- Li, O.Y.; Wang, X.C.; Yang, K.; Liu, D.M.; Shi, H.C. The approaching pilot for One Health governance index. Infect. Dis. Poverty 2023, 12, 16. [Google Scholar] [CrossRef]
- Elnaiem, A.; Mohamed-Ahmed, O.; Zumla, A.; Mecaskey, J.; Charron, N.; Abakar, M.F.; Raji, T.; Bahalim, A.; Manikam, L.; Risk, O.; et al. Global and regional governance of One Health and implications for global health security. Lancet 2023, 401, 688–704. [Google Scholar] [CrossRef]
- McArthur, A.G.; Tsang, K.K. Antimicrobial resistance surveillance in the genomic age. Ann. N. Y. Acad. Sci. 2017, 1388, 78–91. [Google Scholar] [CrossRef]
- Su, M.; Satola, S.W.; Read, T.D. Genome-based prediction of bacterial antibiotic resistance. J. Clin. Microbiol. 2019, 57, e01405-18. [Google Scholar] [CrossRef]
- Hendriksen, R.S.; Bortolaia, V.; Tate, H.; Tyson, G.H.; Aarestrup, F.M.; McDermott, P.F. Using Genomics to Track Global Antimicrobial Resistance. Front. Public Health 2019, 7, 242. [Google Scholar] [CrossRef]
- Ransom, E.M.; Potter, R.F.; Dantas, G.; Burnham, C.A.D. Genomic Prediction of Antimicrobial Resistance: Ready or Not, Here It Comes! Clin. Chem. 2020, 66, 1278–1289. [Google Scholar] [CrossRef]
- Su, J.Q.; Cui, L.; Chen, Q.L.; An, X.L.; Zhu, Y.G. Application of genomic technologies to measure and monitor antibiotic resistance in animals. Ann. N. Y. Acad. Sci. 2017, 1388, 121–135. [Google Scholar] [CrossRef]
- Ackers, L.; Ackers-Johnson, G.; Welsh, J.; Kibombo, D.; Opio, S. Infection Prevention Control (IPC) and Antimicrobial Resistance (AMR). Anti-Microb. Resist. Glob. Perspect. 2020, 53–80. [Google Scholar] [CrossRef]

| Resistant Bacteria | 2020 Threat Estimate and 2019–2020 Change | |
|---|---|---|
| URGENT | Carbapenem-resistant Acinetobacter | 7500 cases, 700 deaths. Overall: 35% increase * Hospital onset: 78% increase |
| Clostridioides difficile | ** | |
| Carbapenem-resistant Enterobacterales (CRE) | 12,700 cases, 1100 deaths. Overall: Stable Hospital onset: 35% increase | |
| Drug-resistant Neisseria gonorrhoeae | ** | |
| SERIOUS | Drug-resistant Campylobacter | 26% of infections were resistant, a 10% decrease, |
| ESBL-producing Enterobacterales | 197,500 cases, 9300 deaths. Overall: 10% increase * Hospital onset: 32% increase * | |
| Vancomycin-resistant Enterococcus | 50,300 cases, 5000 deaths. Overall: 16% increase * Hospital onset: 14% increase * | |
| Multidrug-resistant Pseudomonas aeruginosa | 28,800 cases, 2500 deaths. Overall: Stable * Hospital onset: 32% increase * | |
| Drug-resistant nontyphoidal Salmonella | 14% of infections were resistant, a 3% decrease. | |
| Drug-resistant Salmonella serotype Typhi | 85% of infections were resistant, a 10% increase. | |
| Drug-resistant Shigella | 46% of infections were resistant, a 2% increase. | |
| Methicillin-resistant Staphylococcus aureus | 279,300 cases, 9800 deaths. Overall: Stable * Hospital onset: 13% increase * | |
| Drug-resistant Streptococcus pneumoniae | ** | |
| Drug-resistant Tuberculosis (TB) | 661 cases, decrease. | |
| CONCERNING | Erythromycin-resistant group A Streptococcus | ** |
| Clindamycin-resistant group B Streptococcus | ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cella, E.; Giovanetti, M.; Benedetti, F.; Scarpa, F.; Johnston, C.; Borsetti, A.; Ceccarelli, G.; Azarian, T.; Zella, D.; Ciccozzi, M. Joining Forces against Antibiotic Resistance: The One Health Solution. Pathogens 2023, 12, 1074. https://doi.org/10.3390/pathogens12091074
Cella E, Giovanetti M, Benedetti F, Scarpa F, Johnston C, Borsetti A, Ceccarelli G, Azarian T, Zella D, Ciccozzi M. Joining Forces against Antibiotic Resistance: The One Health Solution. Pathogens. 2023; 12(9):1074. https://doi.org/10.3390/pathogens12091074
Chicago/Turabian StyleCella, Eleonora, Marta Giovanetti, Francesca Benedetti, Fabio Scarpa, Catherine Johnston, Alessandra Borsetti, Giancarlo Ceccarelli, Taj Azarian, Davide Zella, and Massimo Ciccozzi. 2023. "Joining Forces against Antibiotic Resistance: The One Health Solution" Pathogens 12, no. 9: 1074. https://doi.org/10.3390/pathogens12091074






