Nontuberculous Mycobacteria as Sapronoses: A Review
Abstract
:1. Introduction
2. History of the Term “Sapronosis” and Relative Terms
2.1. Saprozoonosis
- Sapro-zoonoses: the pathogens are transmitted indirectly by means of a vehicle (in particular soil, water, food, or plants);
- Direct zoonoses: the pathogens are transmitted to humans by infected vertebrates (the causative agent is unchanged, i.e., rabies, brucellosis, or trichinosis);
- Cyclo-zoonoses: the pathogens require more than one vertebrate host for successful transmission and for completion of its life cycle, and there is no need for transmission of invertebrate intermediate hosts (i.e., echinococcosis or taeniasis);
- Meta-zoonoses: pathogen is transmitted by an invertebrate vector in which the pathogen multiplies and/or develops (i.e., leishmaniosis, human plague, and schistosomiasis);
- Anthroponoses: the pathogen only causes disease in humans but can be transmitted from lower vertebrates (mice, etc.) and invertebrates (fleas, etc.) to humans (i.e., human plague);
2.2. Zoophilous Sapronosis
2.3. Soil-Borne Pathogens: Division According to Bultman et al.
- Permanent pathogens (present in soil permanently) are a permanent part of the soil environment, i.e., the soil microflora. Their occurrence is constant in certain areas, accompanied by their multiplication in the soil;
- Periodic pathogens (occurring in the soil temporarily during their development) need to spend some time outside the host as part of their life cycle;
- Transient pathogens (surviving but not reproducing in soil, i.e., pathogens passing through the soil) can survive in soil outside the host organism for a long time but cannot proliferate in it;
- Incidental pathogens (occurring in the soil by accident) occur in soil and other related environments by chance, mostly in connection with human activity. They enter the soil most commonly via human waste and poor municipal hygiene and insufficiently processed animal waste.
2.4. Euedaphic and Soil Transmitted Pathogens
- 1.
- Euedaphic pathogens (transmitted by soil contact only);
- 2.
- Soil transmitted pathogens (passive mode of soil transmission, i.e., the pathogen survives in soil while maintaining its infectivity to the host organism, but these infections are not exclusive to soil contact and other sources of infection exist).
3. Saprophytic and Saprozoic Mycobacteria
3.1. Mycobacteria as Saprophytic Bacteria
3.2. Mycobacteria as Saprozoic Bacteria
4. Mycobacteria and Sapronoses
4.1. First Published Information about Mycobacteria and Sapronoses
4.2. Current Research in Ecology of Mycobacteria
4.3. Mycobacteria Present in Water, Biofilms etc.
4.4. Mycobacteria Present in Soil
4.5. Sources of Mycobacteria in Plants and Plants’ Tissues
4.5.1. Internalisation of Mycobacteria in Plant Tissues
4.5.2. Surface Contamination of Plants
4.6. Mycobacteria with Unknown Natural Source
5. Geophagia
5.1. Geophagia in Humans
5.2. Geophagia in Animals
5.3. Geophagia in Animals and Nontuberculous Mycobacteria
6. Conditions for Survival and Multiplication of Mycobacteria in the Environment
6.1. Environment Temperature
6.1.1. Psychrophilic Mycobacterial Species
6.1.2. Mesophilic Mycobacterial Species
6.1.3. Thermophilic Mycobacterial Species
6.1.4. Extremely Thermophilic Mycobacterial Species
6.2. Environmental pH
7. Chemical Conditions for Survival and Multiplication of Mycobacteria in the Environment
7.1. Content of Organic Carbon (OC) in the Environment
7.2. Phosphorus as Important Element for Mycobacterial Growth
7.3. The Impact of Metallic Chemical Elements for Mycobacterial Growth
8. Clinical Relevance of Mycobacteria
8.1. Soil-Borne Mycobacteria: Division According to Bultman et al.
8.1.1. Permanent Pathogens (Present in Soil Permanently)
8.1.2. Periodic Pathogens (Occurring in the Soil Temporarily during Their Development)
8.1.3. Transient Pathogens (Surviving but Not Reproducing in Soil; Pathogens Passing through the Soil)
8.1.4. Incidental Pathogens (Occurring in the Soil by Accident)
8.2. Euedaphic and Soil Transmitted Mycobacteria: Division according to Jeffery and Van Der Putten
8.2.1. Euedaphic Pathogens (Transmitted by Soil Only)
8.2.2. Soil Transmitted Pathogens (Passive Mode of Soil Transmission, i.e., That the Pathogen in the Soil Survives Longer while Maintaining Its Infectivity to the Host Organism)
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Iivanainen, E. Isolation of mycobacteria from acidic forest soil samples–comparison of culture methods. J. Appl. Bacteriol. 1995, 78, 663–668. [Google Scholar] [CrossRef]
- Iivanainen, E.K.; Martikainen, P.J.; Raisanen, M.L.; Katila, M.L. Mycobacteria in boreal coniferous forest soils. FEMS Microbiol. Ecol. 1997, 23, 325–332. [Google Scholar] [CrossRef]
- Kendall, B.A.; Winthrop, K.L. Update on the epidemiology of pulmonary nontuberculous mycobacterial infections. Semin. Respir. Crit. Care Med. 2013, 34, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.R.; Heo, S.T.; Lee, K.H.; Kim, J.; Sung, J.K.; Kim, Y.R.; Kim, J.W. Skin and soft tissue infection due to rapidly growing mycobacteria: Case series and literature review. Infect. Chemother. 2013, 45, 85–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falkinham, J.O., 3rd. Environmental sources of nontuberculous mycobacteria. Clin. Chest Med. 2015, 36, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Hamada, S.; Ito, Y.; Hirai, T.; Murase, K.; Tsuji, T.; Fujita, K.; Mio, T.; Maekawa, K.; Fujii, T.; Ono, S.; et al. Impact of industrial structure and soil exposure on the regional variations in pulmonary nontuberculous mycobacterial disease prevalence. Int. J. Mycobacteriol. 2016, 5, 170–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamilton, K.A.; Weir, M.H.; Haas, C.N. Dose response models and a quantitative microbial risk assessment framework for the Mycobacterium avium complex that account for recent developments in molecular biology, taxonomy, and epidemiology. Water Res. 2017, 109, 310–326. [Google Scholar] [CrossRef] [PubMed]
- Nishiuchi, Y.; Iwamoto, T.; Maruyama, F. Infection sources of a common non-tuberculous mycobacterial pathogen, Mycobacterium avium complex. Front. Med. 2017, 4, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claeys, T.A.; Robinson, R.T. The many lives of nontuberculous mycobacteria. J. Bacteriol. 2018, 200, e00739-17. [Google Scholar] [CrossRef] [Green Version]
- Shah, J.A.; Lindestam Arlehamn, C.S.; Horne, D.J.; Sette, A.; Hawn, T.R. Nontuberculous mycobacteria and heterologous immunity to tuberculosis. J. Infect. Dis. 2019, 220, 1091–1098. [Google Scholar] [CrossRef] [PubMed]
- Parikh, A.; Vinnard, C.; Fahrenfeld, N.; Davidow, A.L.; Patrawalla, A.; Lardizabal, A.; Gow, A.; Panettieri, R.; Gennaro, M. Revisiting John Snow to meet the challenge of nontuberculous mycobacterial lung disease. Int. J. Environ. Res. Public Health 2019, 16, 4250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shin, J.I.; Shin, S.J.; Shin, M.K. Differential genotyping of Mycobacterium avium complex and its implications in clinical and environmental epidemiology. Microorganisms 2020, 8, 98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Munjal, S.; Munjal, S.; Gao, J.; Venketaraman, V. Exploring potential COPD immunosuppression pathways causing increased susceptibility for MAC infections among COPD patients. Clin. Pract. 2021, 11, 77. [Google Scholar] [CrossRef] [PubMed]
- Mortaz, E.; Moloudizargari, M.; Varahram, M.; Movassaghi, M.; Garssen, J.; Kazempour Dizagie, M.; Mirsaeidi, M.; Adcock, I.M. What immunological defects predispose to non-tuberculosis mycobacterial infections? Iran J. Allergy Asthma Immunol. 2018, 17, 100–109. [Google Scholar] [PubMed]
- Pontiroli, A.; Khera, T.T.; Oakley, B.B.; Mason, S.; Dowd, S.E.; Travis, E.R.; Erenso, G.; Aseffa, A.; Courtenay, O.; Wellington, E.M. Prospecting environmental mycobacteria: Combined molecular approaches reveal unprecedented diversity. PLoS ONE 2013, 8, e68648. [Google Scholar] [CrossRef] [Green Version]
- McClure, R.; Naylor, D.; Farris, Y.; Davison, M.; Fansler, S.J.; Hofmockel, K.S.; Jansson, J.K. Development and analysis of a stable, reduced complexity model soil microbiome. Front. Microbiol. 2020, 11, 1987. [Google Scholar] [CrossRef]
- Bartelme, R.P.; Custer, J.M.; Dupont, C.L.; Espinoza, J.L.; Torralba, M.; Khalili, B.; Carini, P. Influence of substrate concentration on the culturability of heterotrophic soil microbes isolated by High-Throughput Dilution-to-Extinction cultivation. mSphere 2020, 5, e00024-20. [Google Scholar] [CrossRef] [Green Version]
- Terskikh, V.I. Diseases of humans and animals caused by microbes able to reproduce in an abiotic environment that represents their living habitat. Zh. Mikrobiol. Epidemiol. Immunobiol. 1958, 8, 118–122. (In Russian) [Google Scholar]
- Litvin, V.Y.; Pushkareva, V.I. The possible mechanism in the formation of epidemic variants of the causative agents of sapronoses in the soil or water. Zh. Mikrobiol. Epidemiol. Immunobiol. 1994, 5, 89–95. (In Russian) [Google Scholar]
- Buzolyova, L.S.; Somov, G.P. Autotrophic assimilation of CO2 and C1-compounds by pathogenic bacteria. Biochemistry 1999, 64, 1146–1149. [Google Scholar]
- Iurova, M.A.; Pushkareva, V.I.; Poliakov, V.I. Presence of Yersinia enterocolitica in conditions of agro complex. Zh. Mikrobiol. Epidemiol. Immunobiol. 2013, 3, 31–38. (In Russian) [Google Scholar]
- Kuris, A.M.; Lafferty, K.D.; Sokolow, S.H. Sapronosis: A distinctive type of infectious agent. Trends Parasitol. 2014, 30, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.K.; Mehta, P.K.; Patel, J.G.; Kashyap, S.K.; Chatterjee, S.K. Studies on saprozoonosis. I. A survey on Aspergillus species with special reference to occupational habits. J. Environ. Sci. Health B 1979, 14, 97–117. [Google Scholar] [CrossRef] [PubMed]
- Kakoma, I.; Ristic, M. Human-Bovine Ecosystems: Reflections on Zoonoses in the Tropics. In Diseases of Cattle in the Tropics. Current Topics in Veterinary Medicine and Animal Science; Ristic, M., McIntyre, W.I.M., Eds.; Springer: Dordrecht, Germany, 1981; Volume 6, pp. 39–51. [Google Scholar]
- Jaffry, K.T.; Ali, S.; Rasool, A.; Raza, A.; Gill, Z.J. Zoonoses. Int. J. Agric. Biol. 2009, 11, 217–220. [Google Scholar]
- Pavlik, I.; Ayele, W.Y.; Parmova, I.; Melicharek, I.; Hanzlikova, M.; Kormendy, B.; Nagy, G.; Cvetnic, Z.; Katalinic-Jankovic, V.; Ocepek, M.; et al. Mycobacterium tuberculosis in animal and human populations in six Central European countries during 1990–1999. Vet. Med-Czech. 2003, 48, 83–89. [Google Scholar] [CrossRef] [Green Version]
- Pavlik, I.; Trcka, I.; Parmova, I.; Svobodova, J.; Melicharek, I.; Nagy, G.; Cvetnic, Z.; Ocepek, M.; Pate, M.; Lipiec, M. Detection of bovine and human tuberculosis in cattle and other animals in six Central European countries during the years 2000–2004. Vet. Med-Czech. 2005, 50, 291–299. [Google Scholar] [CrossRef] [Green Version]
- Moravkova, M.; Slany, M.; Trcka, I.; Havelkova, M.; Svobodova, J.; Skoric, M.; Heinigeova, B.; Pavlik, I. Human-to-human and human-to-dog Mycobacterium tuberculosis transmission studied by IS6110 RFLP analysis: A case report. Vet. Med-Czech. 2011, 56, 314–317. [Google Scholar] [CrossRef] [Green Version]
- Karimova, T.Y.; Neronov, V.M.; Popov, V.P. Development of views on natural focality of plague. Biol. Bull. 2010, 37, 725–732. [Google Scholar] [CrossRef]
- Bultman, M.W.; Fischer, S.F.; Pappagianis, F.S. The ecology of soil-borne human pathogens. In Essentials of Medical Geology: Impacts of the Natural Environment on Public Health; Selenius, O., Ed.; Elsevier Academic Press: Cambridge, MA, USA, 2005; Chapter 19; pp. 481–497. [Google Scholar]
- Selinus, O. (Ed.) Essentials of Medical Geology, 2nd ed.; Springer: Heidelberg, Germany; Dordrecht, The Netherlands; London, UK; New York, NY, USA, 2013; 805p. [Google Scholar]
- Jeffery, S.; Van der Putten, W.H. Soil Borne Human Diseases; Publications Office of the European Union: Luxembourg, 2011; 56p. [Google Scholar]
- Kazda, J. The Ecology of Mycobacteria; Kluwer Academic Publishers: Dordrecht, The Netherlands; Boston, MA, USA; London, UK, 2000; 72p. [Google Scholar]
- Alvarez, E.; Tavel, E. Recherches sur le bacille de Lustgarten. Arch. Physiol. Normal Pathol. 1885, 6, 303–321. [Google Scholar]
- Lehmann, K.B.; Neumann, R. Lehmann’s Medizin Handatlanten. X. Atlas und GrundriB der Bakteriologie und Lehrbuch der Speziellen Bakteriologischen Diagnostik, 2nd ed; München, Germany, 1899. [Google Scholar]
- Kazda, J. The chronology of mycobacteria and the development of mycobacterial ecology. In The Ecology of Mycobacteria: Impact on Animal’s and Human’s Health, 1st ed.; Kazda, J., Pavlik, I., Falkinham, J., Hruska, K., Eds.; Springer: Dordrecht, The Netherlands; Berlin/Heidelberg, Germany; London, UK; New York, NY, USA, 2009; Chapter 1; pp. 1–11. [Google Scholar]
- Steinert, M.; Birkness, K.; White, E.; Fields, B.; Quinn, F. Mycobacterium avium bacilli grow saprozoically in coculture with Acanthamoeba polyphaga and survive within cyst walls. Appl. Environ. Microbiol. 1998, 64, 2256–2261. [Google Scholar] [CrossRef] [Green Version]
- Ashbolt, N.J. Environmental (saprozoic) pathogens of engineered water systems: Understanding their ecology for risk assessment and management. Pathogens 2015, 4, 390–405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kazda, J.; Pavlik, I. The ecology of obligate pathogens. In The Ecology of Mycobacteria: Impact on Animal’s and Human’s Health, 1st ed.; Kazda, J., Pavlik, I., Falkinham, J., Hruska, K., Eds.; Springer: Dordrecht, The Netherlands; Berlin/Heidelberg, Germany; London, UK; New York, NY, USA, 2009; Chapter 2; pp. 13–19. [Google Scholar]
- LPSN: List of Prokaryotic Names with Standing in Nomenclature. Available online: https://lpsn.dsmz.de/ (accessed on 10 October 2021).
- Pavlik, I.; Kazda, J.; Falkinham, J. The ecology of potentially pathogenic mycobacteria. In The Ecology of Mycobacteria: Impact on Animal’s and Human’s Health, 1st ed.; Kazda, J., Pavlik, I., Falkinham, J., Hruska, K., Eds.; Springer: Dordrecht, The Netherlands; Berlin/Heidelberg, Germany; London, UK; New York, NY, USA, 2009; Chapter 3; pp. 21–79. [Google Scholar]
- Hubalek, Z. Emerging human infectious diseases: Anthroponoses, zoonoses, and sapronoses. Emerg. Infect. Dis. 2003, 9, 403–404. [Google Scholar] [CrossRef] [PubMed]
- Hubalek, Z.; Rudolf, I. (Eds.) Microbial Zoonoses and Sapronoses; Springer: Heidelberg, Germany; Dordrecht, The Netherlands; London, UK; New York, NY, USA, 2011; 457p. [Google Scholar]
- Allen, A.R.; Ford, T.; Skuce, R.A. Does Mycobacterium tuberculosis var. bovis survival in the environment confound bovine tuberculosis control and eradication? A literature review. Vet. Med. Int. 2021, 2021, 8812898. [Google Scholar] [PubMed]
- Wong, E.B. It is time to focus on asymptomatic tuberculosis. Clin. Infect. Dis. 2021, 15, e1044–e1046. [Google Scholar] [CrossRef]
- Honda, J.R.; Virdi, R.; Chan, E.D. Global environmental nontuberculous mycobacteria and their contemporaneous man-made and natural niches. Front. Microbiol. 2018, 9, 2029. [Google Scholar] [CrossRef] [Green Version]
- Varghese, B.; Al-Hajoj, S. A global update on rare non-tuberculous mycobacteria in humans: Epidemiology and emergence. Int. J. Tuberc. Lung Dis. 2020, 24, 214–223. [Google Scholar] [CrossRef]
- Dolezalova, K.; Gopfertova, D. Ten years’ experience with the discontinuation of the Bacillus Calmette-Guérin vaccination in the Czech Republic. Int. J. Mycobacteriol. 2021, 10, 193–198. [Google Scholar]
- Pavlik, I.; Falkinham, J.; Kazda, J. Transmission of mycobacteria from the environment to susceptible hosts. In The Ecology of Mycobacteria: Impact on Animal’s and Human’s Health, 1st ed.; Kazda, J., Pavlik, I., Falkinham, J., Hruska, K., Eds.; Springer: Dordrecht, The Netherlands; Berlin/Heidelberg, Germany; London, UK; New York, NY, USA, 2009; Chapter 7; pp. 283–312. [Google Scholar]
- Zinsstag, J.; Borna, M.; Pavlik, I. Mycobacterioses. In Oxford Textbook of Zoonoses. Biology, Clinical Practice and Public Health Control, 2nd ed.; Palmer, S.R., Soulsby, L., Torgerson, P.R., Brown, D.W.G., Eds.; Oxford University Press: Oxford, UK, 2011; Chapter 15; pp. 128–135. [Google Scholar]
- Al-Anazi, K.A.; Al-Jasser, A.M.; Al-Anazi, W.K. Infections caused by non-tuberculous mycobacteria in recipients of hematopoietic stem cell transplantation. Front. Oncol. 2014, 10, 311. [Google Scholar] [CrossRef] [Green Version]
- Mara, D.; Horan, N. Handbook of Water and Wastewater Microbiology; Academic Press: London, UK, 2003; 610p. [Google Scholar]
- Pedley, S.; Bartram, J.; Rees, G.; Dufou, A.; Cotruvo, J.A. Pathogenic Mycobacteria in Water; WHO: Geneva, Switzerland; TJ International (Ltd.): Cornwall, UK, 2004; 237p. [Google Scholar]
- Whiley, H.; Keegan, A.; Giglio, S.; Bentham, R. Mycobacterium avium complex-the role of potable water in disease transmission. J. Appl. Microbiol. 2012, 113, 223–232. [Google Scholar] [CrossRef]
- Falkinham, J.O., 3rd. Living with Legionella and other waterborne pathogens. Microorganisms 2020, 18, 2026. [Google Scholar] [CrossRef]
- Ijaz, M.K.; Zargar, B.; Wright, K.E.; Rubino, J.R.; Sattar, S.A. Generic aspects of the airborne spread of human pathogens indoors and emerging air decontamination technologies. Am. J. Infect. Control. 2016, 44 (Suppl. S9), S109–S120. [Google Scholar] [CrossRef] [PubMed]
- Gopalaswamy, R.; Shanmugam, S.; Mondal, R.; Subbian, S. Of tuberculosis and non-tuberculous mycobacterial infections—A comparative analysis of epidemiology, diagnosis and treatment. J. Biomed. Sci. 2020, 27, 74. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Bedard, E.; Prevost, M.; Camper, A.K.; Hill, V.R.; Pruden, A. Methodological approaches for monitoring opportunistic pathogens in premise plumbing: A review. Water Res. 2017, 117, 68–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loret, J.F.; Dumoutier, N. Non-tuberculous mycobacteria in drinking water systems: A review of prevalence data and control means. Int. J. Hyg. Environ. Health 2019, 222, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.M.; Armbruster, C.R.; Arduino, M.J. Plumbing of hospital premises is a reservoir for opportunistically pathogenic microorganisms: A review. Biofouling 2013, 29, 147–162. [Google Scholar] [CrossRef]
- Juzga-Corrales, D.C.; Moliner-Calderon, E.; Coll-Figa, P.; Leon-Vintro, X. Mycobacterium malmoense parotid gland infection. Enferm. Infect. Microbiol. Clin. 2019, 37, 545–547, (In English and Spanish). [Google Scholar] [CrossRef]
- Scanlon, M.M.; Gordon, J.L.; McCoy, W.F.; Cain, M.F. Water management for construction: Evidence for risk characterization in community and healthcare settings: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 2168. [Google Scholar] [CrossRef] [Green Version]
- Maalouly, C.; Devresse, A.; Martin, A.; Rodriguez-Villalobos, H.; Kanaan, N.; Belkhir, L. Coinfection of Mycobacterium malmoense and Mycobacterium chimaera in a kidney transplant recipient: A case report and review of the literature. Transpl. Infect. Dis. 2020, 22, e13241. [Google Scholar] [CrossRef]
- Piyumal Samaranayake, W.A.M.; Kesson, A.M.; Karpelowsky, J.S.; Outhred, A.C.; Marais, B.J. Port-site infection due to nontuberculous mycobacteria following laparoscopic surgery. Int. J. Mycobacteriol. 2020, 9, 231–238. [Google Scholar] [CrossRef]
- Arfaatabar, M.; Karami, P.; Khaledi, A. An update on prevalence of slow-growing mycobacteria and rapid-growing mycobacteria retrieved from hospital water sources in Iran—A systematic review. Germs 2021, 11, 97–104. [Google Scholar] [CrossRef]
- Habermann, S.; Ferran, E.; Hatcher, J.; Lyall, H.; De La Fuente, J.; Whittaker, E. Outbreak of non-tuberculous mycobacteria in a paediatric bone marrow transplant unit associated with water contamination of needle-free connectors and literature review. Bone Marrow Transpl. 2021, 56, 2305–2308. [Google Scholar] [CrossRef] [PubMed]
- Shuval, H.I. Effects of wastewater irrigation of pastures on the health of farm animals and humans. Rev. Sci. Technol. 1991, 10, 847–866. [Google Scholar] [CrossRef] [PubMed]
- Pachepsky, Y.; Shelton, D.R.; McLain, J.E.T.; Patel, J.; Mandrell, R.E. Irrigation waters as a source of pathogenic microorganisms in produce: A review. Adv. Agron. 2011, 113, 73–138. [Google Scholar]
- Richards, J.P.; Ojha, A.K. Mycobacterial biofilms. Microbiol. Spectr. 2014, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ojha, A.K.; Jacobs, W.R., Jr.; Hatfull, G.F. Genetic dissection of mycobacterial biofilms. Methods. Mol. Biol. 2015, 1285, 215–226. [Google Scholar] [PubMed]
- Esteban, J.; Garcia-Coca, M. Mycobacterium biofilms. Front. Microbiol. 2018, 8, 2651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bittner, M.J.; Preheim, L.C. Other slow-growing nontuberculous mycobacteria. Microbiol. Spectr. 2016, 4. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.C.; Whang, K.S. Mycobacterium aquiterrae sp. nov., a rapidly growing bacterium isolated from groundwater. Int. J. Syst. Evol. Microbiol. 2017, 67, 4104–4110. [Google Scholar]
- Cydzik-Kwiatkowska, A.; Zielinska, M. Bacterial communities in full-scale wastewater treatment systems. World J. Microbiol. Biotechnol. 2016, 32, 66. [Google Scholar] [CrossRef] [Green Version]
- Chen, G.Q.; Wu, Y.H.; Wang, Y.H.; Chen, Z.; Tong, X.; Bai, Y.; Luo, L.W.; Xu, C.; Hu, H.Y. Effects of microbial inactivation approaches on quantity and properties of extracellular polymeric substances in the process of wastewater treatment and reclamation: A review. J. Hazard. Mater. 2021, 413, 125283. [Google Scholar] [CrossRef]
- Falkinham, J. Physiological ecology of environmental saprophytic and potentially pathogenic mycobacteria. In The Ecology of Mycobacteria: Impact on Animal’s and Human’s Health, 1st ed.; Kazda, J., Pavlik, I., Falkinham, J., Hruska, K., Eds.; Springer: Dordrecht, The Netherlands; Berlin/Heidelberg, Germany; London, UK; New York, NY, USA, 2009; Chapter 4; pp. 81–87. [Google Scholar]
- Beerwerth, W. Mycobacterial soil flora in the course of the seasons. Prax. Pneumol. 1971, 25, 661–668. (In German) [Google Scholar] [PubMed]
- Pavlik, I.; Falkinham, J.; Kazda, J. Environments providing favourable conditions for the multiplication and transmission of mycobacteria. In The Ecology of Mycobacteria: Impact on Animal’s and Human’s Health, 1st ed.; Kazda, J., Pavlik, I., Falkinham, J., Hruska, K., Eds.; Springer: Dordrecht, The Netherlands; Berlin/Heidelberg, Germany; London, UK; New York, NY, USA, 2009; Chapter 5; pp. 89–197. [Google Scholar]
- Beerwerth, W.; Kessel, U. Mycobacteria in the environment of man and animal. Zentralbl. Bakteriol. 1976, 235, 177–183. (In German) [Google Scholar]
- Beerwerth, W.; Schurmann, J. Contribution to the ecology of mycobacteria. Zentralbl. Bakteriol. 1969, 211, 58–69. (In German) [Google Scholar]
- Kaevska, M.; Hruska, K. Mycobacteria in water, feedstocks and food: Analysis of publications. Vet. Med-Czech. 2010, 55, 571–580. [Google Scholar] [CrossRef] [Green Version]
- Pereira, A.C.; Ramos, B.; Reis, A.C.; Cunha, M.V. Non-tuberculous mycobacteria: Molecular and physiological bases of virulence and adaptation to ecological niches. Microorganisms 2020, 8, 1380. [Google Scholar] [CrossRef]
- Falkinham, J.O., III. Ecology of Nontuberculous Mycobacteria. Microorganisms 2021, 9, 2262. [Google Scholar] [CrossRef]
- Kauker, E.; Rheinwald, W. Studies on the occurrence of atypical mycobacteria, group 3 Runyon, in the bedding material (sawdust) and feed of swine in North Hesse. Berl. Munch. Tierarztl. Wochenschr. 1972, 85, 384–387. (In German) [Google Scholar]
- Kaevska, M.; Lvoncik, S.; Slana, I.; Kulich, P.; Kralik, P. Microscopy, culture, and quantitative real-time PCR examination confirm internalization of mycobacteria in plants. Appl. Environ. Microbiol. 2014, 80, 3888–3894. [Google Scholar] [CrossRef] [Green Version]
- Kaevska, M.; Lvoncik, S.; Lamka, J.; Pavlik, I.; Slana, I. Spread of Mycobacterium avium subsp. paratuberculosis through soil and grass on a mouflon (Ovis aries) pasture. Curr. Microbiol. 2014, 69, 495–500. [Google Scholar]
- Bouam, A.; Armstrong, N.; Levasseur, A.; Drancourt, M. Mycobacterium terramassiliense, Mycobacterium rhizamassiliense and Mycobacterium numidiamassiliense sp. nov., three new Mycobacterium simiae complex species cultured from plant roots. Sci. Rep. 2018, 8, 9309. [Google Scholar] [CrossRef]
- Tran, P.M.; Dahl, J.L. Mycobacterium sarraceniae sp. nov. and Mycobacterium helvum sp. nov., isolated from the pitcher plant Sarracenia purpurea. Int. J. Syst. Evol. Microbiol. 2016, 66, 4480–4485. [Google Scholar] [CrossRef]
- Walsh, C.M.; Gebert, M.J.; Delgado-Baquerizo, M.; Maestre, F.T.; Fierer, N. A global survey of mycobacterial diversity in soil. Appl. Environ. Microbiol. 2019, 85, e01180-19. [Google Scholar] [CrossRef] [Green Version]
- Honda, J.R.; Hasan, N.A.; Davidson, R.M.; Williams, M.D.; Epperson, L.E.; Reynolds, P.R.; Smith, T.; Iakhiaeva, E.; Bankowski, M.J.; Wallace, R.J., Jr.; et al. Environmental nontuberculous mycobacteria in the Hawaiian Islands. PLoS Negl. Trop. Dis. 2016, 10, e0005068. [Google Scholar] [CrossRef] [Green Version]
- Baker, A.W.; Lewis, S.S.; Alexander, B.D.; Chen, L.F.; Wallace, R.J., Jr.; Brown-Elliott, B.A.; Isaacs, P.J.; Pickett, L.C.; Patel, C.B.; Smith, P.K.; et al. Two-phase hospital-associated outbreak of Mycobacterium abscessus: Investigation and mitigation. Clin. Infect. Dis. 2017, 64, 902–911. [Google Scholar] [CrossRef] [Green Version]
- Doyle, R.M.; Rubio, M.; Dixon, G.; Hartley, J.; Klein, N.; Coll, P.; Harris, K.A. Cross-transmission is not the source of new Mycobacterium abscessus infections in a Multicenter Cohort of Cystic Fibrosis Patients. Clin. Infect. Dis. 2020, 70, 1855–1864. [Google Scholar] [CrossRef] [Green Version]
- Vaerewijck, M.J.; Huys, G.; Palomino, J.C.; Swings, J.; Portaels, F. Mycobacteria in drinking water distribution systems: Ecology and significance for human health. FEMS Microbiol. Rev. 2005, 29, 911–934. [Google Scholar] [CrossRef]
- Quintás Viqueira, A.; Pérez Romero, C.; Toro Rueda, C.; Sánchez Calles, A.M.; Blázquez González, J.A.; Alejandre Leyva, M. Mycobacterium chimaera in heater-cooler devices: An experience in a tertiary hospital in Spain. New Microbes New Infect. 2020, 39, 100757. [Google Scholar] [CrossRef]
- Lange, C.; Böttger, E.C.; Cambau, E.; Griffith, D.E.; Guglielmetti, L.; van Ingen, J.; Knight, S.L.; Marras, T.K.; Olivier, K.N.; Santin, M.; et al. Consensus management recommendations for less common non-tuberculous mycobacterial pulmonary diseases. Lancet Infect. Dis. 2022, 22, e178–e190. [Google Scholar] [CrossRef]
- Abrahams, P.W. Involuntary soil ingestion and geophagia: A source and sink of mineral nutrients and potentially harmful elements to consumers of earth materials. Appl. Geochem. 2012, 27, 954–968. [Google Scholar] [CrossRef]
- Wilson, M.J. Clay mineralogical and related characteristics of geophagic materials. J. Chem. Ecol. 2003, 29, 1525–1547. [Google Scholar] [CrossRef]
- Karoui, A.; Karoui, H. Pica in Tunisian children. Results of a survey performed in a polyclinic of the Tunisian social security national administration. Pediatrie 1993, 48, 565–569. (In French) [Google Scholar] [PubMed]
- Karoui, A.; Karoui, H. Geophagia in Tunisian children—Results of a prospective-study in children day-care-center. Pediatrie. 1993, 48, 565–569. [Google Scholar] [PubMed]
- Glickman, L.T.; Camara, A.O.; Glickmancand, N.; McCabe, G.P. Nematode intestinal parasites of children in rural Guinea, Africa: Prevalence and relationship to geophagia. Int. J. Epidemiol. 1999, 28, 169–174. [Google Scholar] [CrossRef] [Green Version]
- Njiru, H.; Elchalal, U.; Paltiel, O. Geophagy during pregnancy in Africa: A literature review. Obstet. Gynecol. Surv. 2011, 66, 452–459. [Google Scholar] [CrossRef]
- Kortei, N.K.; Koryo-Dabrah, A.; Akonor, P.T.; Manaphraim, N.Y.B.; Ayim-Akonor, M.; Boadi, N.O.; Essuman, E.K.; Tettey, C. Potential health risk assessment of toxic metals contamination in clay eaten as pica (geophagia) among pregnant women of Ho in the Volta Region of Ghana. BMC Pregnancy Childbirth 2020, 20, 160. [Google Scholar] [CrossRef]
- Abrahams, P.W.; Davies, T.C.; Solomon, A.O.; Trow, A.J.; Wragg, J. Human geophagia, Calabash chalk and undongo: Mineral element nutritional implications. PLoS ONE 2013, 8, e53304. [Google Scholar]
- Abrahams, P.W.; Parsons, J.A. Geophagy in the tropics: A literature review. Geogr. J. 1996, 162, 63–72. [Google Scholar] [CrossRef]
- Narh, C.T.; Dzamalala, C.P.; Mmbaga, B.T.; Menya, D.; Mlombe, Y.; Finch, P.; Nyakunga, G.; Schuz, J.; McCormack, V. Geophagia and risk of squamous cell esophageal cancer in the African esophageal cancer corridor: Findings from the ESCCAPE multicountry case-control studies. Int. J. Cancer. 2021, 149, 1274–1283. [Google Scholar] [CrossRef]
- Vermeer, D. A note on geophagy among the Afenmai and adjacent peoples of Bendel State, Nigeria. Afr. Notes 1979, 8, 13–14. [Google Scholar]
- Abrahams, P.W.; Follansbee, M.H.; Hunt, A.; Smith, B.; Wragg, J. Iron nutrition and possible lead toxicity: An appraisal of geophagy undertaken by pregnant women of UK Asian communities. Appl. Geochem. 2006, 21, 98–108. [Google Scholar] [CrossRef]
- Dean, J.R.; Deary, M.E.; Gbefa, B.K.; Scott, W.C. Characterisation and analysis of persistent organic pollutants and major, minor and trace elements in Calabash chalk. Chemosphere 2004, 57, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Felten, M.K.; Knoetze, K. Mycobacteria in sputum and soil ingestion. Lancet 1987, 1, 334–335. [Google Scholar] [CrossRef]
- Knezevich, M. Geophagy as a therapeutic mediator of endoparasitism in a free-ranging group of rhesus macaques (Macaca mulatta). Am. J. Primatol. 1998, 44, 71–82. [Google Scholar] [CrossRef]
- Mahaney, W.C.; Bezada, M.; Hancock, R.G.V.; Aufreiter, S.; Perez, F.L. Geophagy of Holstein hybrid cattle in the northern Andes, Venezuela. Mt. Res. Dev. 1996, 16, 177–180. [Google Scholar] [CrossRef]
- Diamond, J.; Bishop, K.D.; Gilardi, J.D. Geophagy in New Guinea birds. Ibis 1999, 141, 181–193. [Google Scholar] [CrossRef]
- Gilardi, J.D.; Duffey, S.S.; Munn, C.A.; Tell, L.A. Biochemical functions of geophagy in parrots: Detoxification of dietary toxins and cytoprotective effects. J. Chem. Ecol. 1999, 25, 897–922. [Google Scholar] [CrossRef]
- Trckova, M.; Matlova, L.; Dvorska, L.; Pavlik, I. Kaolin, bentonite, and zeolites as feed supplements for animals: Health advantages and risks. Vet. Med-Czech. 2004, 49, 389–399. [Google Scholar] [CrossRef] [Green Version]
- Trckova, M.; Vondruskova, H.; Zraly, Z.; Alexa, P.; Hamrik, J.; Kummer, V.; Maskova, J.; Mrlik, V.; Krizova, K.; Slana, I.; et al. The effect of kaolin feeding on efficiency, health status and course of diarrhoeal infections caused by enterotoxigenic Escherichia coli strains in weaned piglets. Vet. Med-Czech. 2009, 54, 47–63. [Google Scholar] [CrossRef] [Green Version]
- Vondruskova, H.; Slamova, R.; Trckova, M.; Zraly, Z.; Pavlik, I. Alternatives to antibiotic growth promoters in prevention of diarrhoea in weaned piglets: A review. Vet. Med-Czech. 2010, 55, 199–224. [Google Scholar] [CrossRef] [Green Version]
- Slamova, R.; Trckova, M.; Vondruskova, H.; Zraly, Z.; Pavlik, I. Clay minerals in animal nutrition. Appl. Clay Sci. 2011, 51, 395–398. [Google Scholar] [CrossRef]
- Trckova, M.; Matlova, L.; Hudcova, H.; Faldyna, M.; Zraly, Z.; Dvorska, L.; Beran, V.; Pavlik, I. Peat as a feed supplement for animals: A literature review. Vet. Med-Czech. 2005, 50, 361–377. [Google Scholar] [CrossRef] [Green Version]
- Pavlik, I.; Falkinham, J. The occurrence of pathogenic and potentially pathogenic mycobacteria in animals and the role of the environment in the spread of infection. In The Ecology of Mycobacteria: Impact on Animal’s and Human’s Health, 1st ed.; Kazda, J., Pavlik, I., Falkinham, J., Hruska, K., Eds.; Springer: Dordrecht, The Netherlands; Berlin/Heidelberg, Germany; London, UK; New York, NY, USA, 2009; Chapter 6; pp. 199–281. [Google Scholar]
- Pavlik, I.; Hruska, K. Photographs. In The Ecology of Mycobacteria: Impact on Animal’s and Human’s Health, 1st ed.; Kazda, J., Pavlik, I., Falkinham, J., Hruska, K., Eds.; Springer: Dordrecht, The Netherlands; Berlin/Heidelberg, Germany; London, UK; New York, NY, USA, 2009; Chapter 10; pp. 339–519. [Google Scholar]
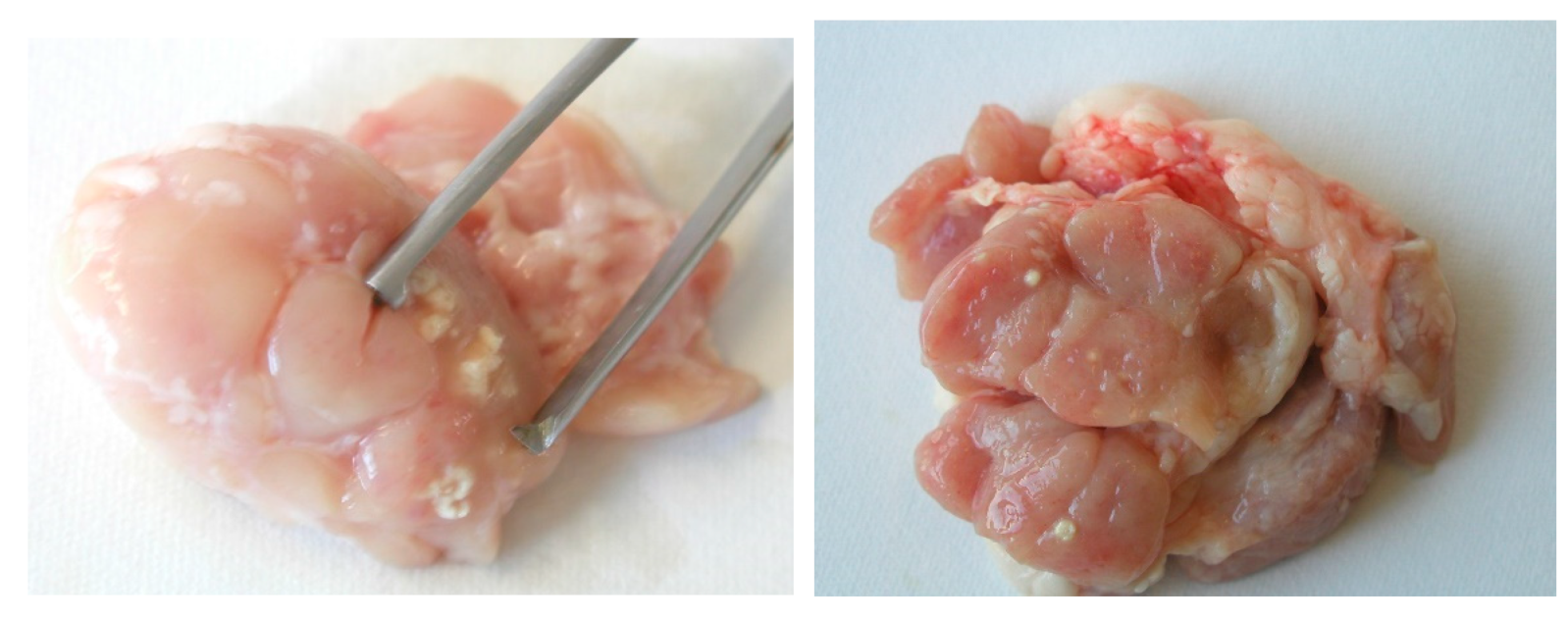
- Matlova, L.; Dvorska, L.; Ayele, W.Y.; Bartos, M.; Amemori, T.; Pavlik, I. Distribution of Mycobacterium avium complex isolates in tissue samples of pigs fed peat naturally contaminated with mycobacteria as a supplement. J. Clin. Microbiol. 2005, 43, 1261–1268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trckova, M.; Zraly, Z.; Matlova, L.; Beran, V.; Moravkova, M.; Svobodova, J.; Pavlik, I. Effects of peat feeding on the performance and health status of fattening pigs and environmentally derived mycobacteria. Vet. Med-Czech. 2006, 51, 533–543. [Google Scholar] [CrossRef] [Green Version]
- Agdestein, A.; Johansen, T.B.; Polacek, V.; Lium, B.; Holstad, G.; Vidanovic, D.; Aleksic-Kovacevic, S.; Jorgensen, A.; Zultauskas, J.; Nilsen, S.F.; et al. Investigation of an outbreak of mycobacteriosis in pigs. BMC Vet. Res. 2011, 7, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agdestein, A.; Olsen, I.; Jorgensen, A.; Djonne, B.; Johansen, T.B. Novel insights into transmission routes of Mycobacterium avium in pigs and possible implications for human health. Vet. Res. 2014, 45, 46. [Google Scholar] [CrossRef] [Green Version]
- Johansen, T.B.; Agdestein, A.; Lium, B.; Jorgensen, A.; Djonne, B. Mycobacterium avium subsp. hominissuis infection in swine associated with peat used for bedding. Biomed. Res. Int. 2014, 2014, 189649. [Google Scholar]
- Wagner, K.M.; Schulz, J.; Kemper, N. Examination of the hygienic status of selected organic enrichment materials used in pig farming with special emphasis on pathogenic bacteria. Porcine Health Manag. 2018, 4, 24. [Google Scholar] [CrossRef]
- Matlova, L.; Kaevska, M.; Moravkova, M.; Beran, V.; Shitaye, J.E.; Pavlik, I. Mycobacteria in peat used as a supplement for pigs: Failure of different decontamination methods to eliminate the risk. Vet. Med-Czech. 2012, 57, 212–217. [Google Scholar] [CrossRef] [Green Version]
- Matlova, L.; Dvorska, L.; Bartos, M.; Docekal, J.; Trckova, M.; Pavlik, I. Tuberculous lesions in pig lymph nodes caused by kaolin fed as supplement. Vet. Med-Czech. 2004, 49, 379–388. [Google Scholar] [CrossRef] [Green Version]
- Yu, Z.; Stewart, G.R.; Mohn, W.W. Apparent contradiction: Psychrotolerant bacteria from hydrocarbon-contaminated arctic tundra soils that degrade diterpenoids synthesized by trees. Appl. Environ. Microbiol. 2000, 66, 5148–5154. [Google Scholar] [CrossRef] [Green Version]
- Ferrera-Rodriguez, O.; Greer, C.W.; Juck, D.; Consaul, L.L.; Martinez-Romero, E.; Whyte, L.G. Hydrocarbon-degrading potential of microbial communities from Arctic plants. J. Appl. Microbiol. 2013, 114, 71–83. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Cao, T.; Ying, J.; Yang, Y.; Ma, L. Diversity and novelty of Actinobacteria in Arctic marine sediments. Antonie Van Leeuwenhoek 2014, 105, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Muangchinda, C.; Chavanich, S.; Viyakarn, V.; Watanabe, K.; Imura, S.; Vangnai, A.S.; Pinyakong, O. Abundance and diversity of functional genes involved in the degradation of aromatic hydrocarbons in Antarctic soils and sediments around Syowa Station. Environ. Sci. Pollut. Res. Int. 2015, 22, 4725–4735. [Google Scholar] [CrossRef] [PubMed]
- Haas, B.; Soto, K.J.; Day, D.S.; Roy, A.C.; Gagnon, M.C.; Alt, J.R.; Labrie, P. Mycobacterium hassiacum: A thermophilic Mycobacterium species to demonstrate thermal disinfection of medical devices. BMC Res. Notes 2020, 13, 140. [Google Scholar] [CrossRef] [PubMed]
- Ermolenko, Z.M.; Kholodenko, V.P.; Chugunov, V.A.; Zhirkova, N.A.; Rasulova, G.E. A mycobacterial strain isolated from the oil of the Ukhtinskoe oil field: Identification and degradative properties. Microbiology 1997, 66, 542–545. [Google Scholar]
- George, K.L.; Parker, B.C.; Gruft, H.; Falkinham, J.O., 3rd. Epidemiology of infection by nontuberculous mycobacteria. II. Growth and survival in natural waters. Am. Rev. Respir. Dis. 1980, 122, 89–94. [Google Scholar]
- Clark, H.F.; Shepard, C.C. Effect of environmental temperatures on infection with Mycobacterium marinum (balnei) of mice and a number of poikilothermic species. J. Bacteriol. 1963, 86, 1057–1069. [Google Scholar] [CrossRef] [Green Version]
- Kim, T.H.; Kubica, G.P. Long-term preservation and storage of mycobacteria. Appl. Microbiol. 1972, 24, 311–317. [Google Scholar] [CrossRef]
- Shinu, P.; AshokKumar Singh, V.; Nair, A.; Farooq, R.; Ishaq, S. Long-term storage at −80 °C: Effect on rate of recovery of Mycobacterium tuberculosis from direct acid-fast bacilli smear-positive sputum samples. J. Clin. Lab. Anal. 2016, 30, 567–576. [Google Scholar] [CrossRef] [Green Version]
- Pennings, L.J.; Zweijpfenning, S.; Ruth, M.M.; Wattenberg, M.; Boeree, M.J.; Hoefsloot, W.; van Ingen, J. Mycobacterium avium complex bacteria remain viable in sputum during storage and refrigeration. Diagn. Microbiol. Infect. Dis. 2018, 92, 309–310. [Google Scholar] [CrossRef]
- Barbier, E.; Rochelet, M.; Gal, L.; Boschiroli, M.L.; Hartmann, A. Impact of temperature and soil type on Mycobacterium bovis survival in the environment. PLoS ONE 2017, 12, e0176315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, R.; de Carvalho, C.C.; Stevenson, A.; Grant, I.R.; Hallsworth, J.E. Extraordinary solute-stress tolerance contributes to the environmental tenacity of mycobacteria. Environ. Microbiol. Rep. 2015, 7, 746–764. [Google Scholar] [CrossRef] [PubMed]
- Thorel, M.F.; Falkinham, J.O., 3rd; Moreau, R.G. Environmental mycobacteria from alpine and subalpine habitats. FEMS Microbiol. Ecol. 2004, 49, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Tortoli, E. Impact of genotypic studies on mycobacterial taxonomy: The new mycobacteria of the 1990s. Clin. Microbiol. Rev. 2003, 16, 319–354. [Google Scholar] [CrossRef] [Green Version]
- Tortoli, E. Microbiological features and clinical relevance of new species of the genus Mycobacterium. Clin. Microbiol. Rev. 2014, 27, 727–752. [Google Scholar] [CrossRef] [Green Version]
- Pavlik, I.; Svastova, P.; Bartl, J.; Dvorska, L.; Rychlik, I. Relationship between IS901 in the Mycobacterium avium complex strains isolated from birds, animals, humans and environment and virulence for poultry. Clin. Diag. Lab. Immunol. 2000, 7, 212–217. [Google Scholar] [CrossRef] [Green Version]
- Schwabacher, H. A strain of Mycobacterium isolated from skin lesions of a cold-blooded animal, Xenopus laevis, and its relation to atypical acid-fast bacilli occurring in man. J. Hyg. 1959, 57, 57–67. [Google Scholar] [CrossRef] [Green Version]
- Cook, G.M.; Berney, M.; Gebhard, S.; Heinemann, M.; Cox, R.A.; Danilchanka, O.; Niederweis, M. Physiology of mycobacteria. Adv. Microb. Physiol. 2009, 55, 81–182, discussion 318–319. [Google Scholar]
- Archuleta, R.J.; Mullens, P.; Primm, T.P. The relationship of temperature to desiccation and starvation tolerance of the Mycobacterium avium complex. Arch. Microbiol. 2002, 178, 311–314. [Google Scholar] [CrossRef]
- Argueta, C.; Yoder, S.; Holtzman, A.E.; Aronson, T.W.; Glover, N.; Berlin, O.G.; Stelma, G.N., Jr.; Froman, S.; Tomasek, P. Isolation and identification of nontuberculous mycobacteria from foods as possible exposure sources. J. Food Prot. 2000, 63, 930–933. [Google Scholar] [CrossRef]
- Zwielehner, J.; Handschur, M.; Michaelsen, A.; Irez, S.; Demel, M.; Denner, E.B.; Haslberger, A.G. DGGE and real-time PCR analysis of lactic acid bacteria in bacterial communities of the phyllosphere of lettuce. Mol. Nutr. Food Res. 2008, 52, 614–623. [Google Scholar] [CrossRef] [PubMed]
- Yoder, S.; Argueta, C.; Holtzman, A.; Aronson, T.; Berlin, O.G.; Tomasek, P.; Glover, N.; Froman, S.; Stelma, G., Jr. PCR comparison of Mycobacterium avium isolates obtained from patients and foods. Appl. Environ. Microbiol. 1999, 65, 2650–2653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cerna-Cortes, J.F.; Leon-Montes, N.; Cortes-Cueto, A.L.; Salas-Rangel, L.P.; Helguera-Repetto, A.C.; Lopez-Hernandez, D.; Rivera-Gutierrez, S.; Fernandez-Rendon, E.; Gonzalez-y-Merchand, J.A. Microbiological quality of ready-to-eat vegetables collected in Mexico City: Occurrence of aerobic-mesophilic bacteria, fecal coliforms, and potentially pathogenic nontuberculous mycobacteria. Biomed. Res. Int. 2015, 2015, 789508. [Google Scholar] [CrossRef] [Green Version]
- Lund, P.A.; De Biase, D.; Liran, O.; Scheler, O.; Mira, N.P.; Cetecioglu, Z.; Fernández, E.N.; Bover-Cid, S.; Hall, R.; Sauer, M.; et al. Understanding how microorganisms respond to acid pH is central to their control and successful exploitation. Front. Microbiol. 2020, 11, 556140. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A.T.; Nyongesa, S.; Morneau, I.; Reed, M.B.; Tocheva, E.I.; Veyrier, F.J. The mycobacterial cell envelope: A relict from the past or the result of recent evolution? Front. Microbiol. 2018, 9, 2341. [Google Scholar] [CrossRef] [Green Version]
- Niederweis, M. Mycobacterial porins—New channel proteins in unique outer membranes. Mol. Microbiol. 2003, 49, 1167–1177. [Google Scholar] [CrossRef]
- Pule, C.M.; Sampson, S.L.; Warren, R.M.; Black, P.A.; van Helden, P.D.; Victor, T.C.; Louw, G.E. Efflux pump inhibitors: Targeting mycobacterial efflux systems to enhance TB therapy. J. Antimicrob. Chemother. 2016, 71, 17–26. [Google Scholar] [CrossRef] [Green Version]
- Forrellad, M.A.; Klepp, L.I.; Gioffre, A.; Sabio y Garcia, J.; Morbidoni, H.R.; de la Paz Santangelo, M.; Cataldi, A.A.; Bigi, F. Virulence factors of the Mycobacterium tuberculosis complex. Virulence 2013, 4, 3–66. [Google Scholar] [CrossRef] [Green Version]
- Rao, M.; Streur, T.L.; Aldwell, F.E.; Cook, G.M. Intracellular pH regulation by Mycobacterium smegmatis and Mycobacterium bovis BCG. Microbiology 2001, 147 Pt 4, 1017–1024. [Google Scholar] [CrossRef] [Green Version]
- Portaels, F.; Pattyn, S.R. Growth of mycobacteria in relation to the pH of the medium. Ann. Microbiol. 1982, 133, 213–221. [Google Scholar]
- Kyselkova, M.; Chronakova, A.; Volna, L.; Nemec, J.; Ulmann, V.; Scharfen, J.; Elhottova, D. Tetracycline resistance and presence of tetracycline resistance determinants tet(V) and tap in rapidly growing mycobacteria from agricultural soils and clinical isolates. Microbes Environ. 2012, 27, 413–422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.J.; Danelishvili, L.; Wagner, D.; Petrofsky, M.; Bermudez, L.E. Identification of virulence determinants of Mycobacterium avium that impact on the ability to resist host killing mechanisms. J. Med. Microbiol. 2010, 59 Pt 1, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Parsons, L.M.; Jankowski, C.S.; Derbyshire, K.M. Conjugal transfer of chromosomal DNA in Mycobacterium smegmatis. Mol. Microbiol. 1998, 28, 571–582. [Google Scholar] [CrossRef] [PubMed]
- Hatfull, G.F. Molecular genetics of mycobacteriophages. Microbiol. Spectr. 2014, 2, 1–36. [Google Scholar] [CrossRef] [Green Version]
- Iivanainen, E.; Martikainen, P.J.; Vaananen, P.; Katila, M.L. Environmental factors affecting the occurrence of mycobacteria in brook sediments. J. Appl. Microbiol. 1999, 86, 673–681. [Google Scholar] [CrossRef]
- Rinaldi, P.S.; Nisa’Akromah, Z.; Ramadhan, H.; Husna, S.; Syamsudin, D.L.; Panggabean, P.B.; Murdianti, R.A.; Fatahillah, M.H.; Perala, I.; Rizqia, E.K.; et al. Physical and chemical analysis of land in forest peat swamp in Resort Pondok soar, Tanjung Puting National Park, Central Kalimantan. IOP Conf. Series: Earth Environ. Sci. 2019, 394, 012037. [Google Scholar] [CrossRef]
- Wong, E.A.; Shin, G.A. Removal of Mycobacterium avium subspecies hominissuis (MAH) from drinking water by coagulation, flocculation and sedimentation processes. Lett. Appl. Microbiol. 2015, 60, 273–278. [Google Scholar] [CrossRef]
- Bodmer, T.; Miltner, E.; Bermudez, L.E. Mycobacterium avium resists exposure to the acidic conditions of the stomach. FEMS Microbiol. Lett. 2000, 182, 45–49. [Google Scholar] [CrossRef] [Green Version]
- Ulmann, V.; Modra, H.; Babak, V.; Weston, R.T.; Pavlik, I. Recovery of mycobacteria from heavily contaminated environmental matrices. Microorganism 2021, 9, 2178. [Google Scholar] [CrossRef]
- Pavlik, I.; Ulmann, V.; Modra, H.; Gersl, M.; Rantova, B.; Zukal, J.; Zukalova, K.; Konecny, O.; Kana, V.; Kubalek, P.; et al. Nontuberculous mycobacteria prevalence in bats’ guano from caves and attics of buildings studied by culture and qPCR examinations. Microorganisms 2021, 9, 2236. [Google Scholar] [CrossRef]
- Santucci, P.; Johansen, M.D.; Point, V.; Poncin, I.; Viljoen, A.; Cavalier, J.F.; Kremer, L.; Canaan, S. Nitrogen deprivation induces triacylglycerol accumulation, drug tolerance and hypervirulence in mycobacteria. Sci. Rep. 2019, 9, 8667. [Google Scholar] [CrossRef] [PubMed]
- DePas, W.H.; Bergkessel, M.; Newman, D.K. Aggregation of nontuberculous mycobacteria is regulated by carbon-nitrogen balance. mBio 2019, 10, e01715-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghosh, J.; Larsson, P.; Singh, B.; Pettersson, B.M.; Islam, N.M.; Sarkar, S.N.; Dasgupta, S.; Kirsebom, L.A. Sporulation in mycobacteria. Proc. Natl. Acad. Sci. USA 2009, 106, 10781–10786. [Google Scholar] [CrossRef] [Green Version]
- Torvinen, E.; Lehtola, M.J.; Martikainen, P.J.; Miettinen, I.T. Survival of Mycobacterium avium in drinking water biofilms as affected by water flow velocity, availability of phosphorus, and temperature. Appl. Environ. Microbiol. 2007, 73, 6201–6207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carson, L.A.; Petersen, N.J.; Favero, M.S.; Aguero, S.M. Growth characteristics of atypical mycobacteria in water and their comparative resistance to disinfectants. Appl. Environ. Microbiol. 1978, 36, 839–846. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amon, J.; Titgemeyer, F.; Burkovski, A. A genomic view on nitrogen metabolism and nitrogen control in mycobacteria. J. Mol. Microbiol. Biotechnol. 2009, 17, 20–29. [Google Scholar] [CrossRef]
- Kumar, S.; Matange, N.; Umapathy, S.; Visweswariah, S.S. Linking carbon metabolism to carotenoid production in mycobacteria using Raman spectroscopy. FEMS Microbiol. Lett. 2015, 362, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Priestman, M.; Thomas, P.; Robertson, B.D.; Shahrezaei, V. Mycobacteria modify their cell size control under sub-optimal carbon sources. Front. Cell. Dev. Biol. 2017, 5, 64. [Google Scholar] [CrossRef] [Green Version]
- Kazda, J.; Falkinham, J. Biological role of mycobacteria in the environment. In The Ecology of Mycobacteria: Impact on Animal’s and Human’s Health, 1st ed.; Kazda, J., Pavlik, I., Falkinham, J., Hruska, K., Eds.; Springer: Dordrecht, The Netherlands; Berlin/Heidelberg, Germany; London, UK; New York, NY, USA, 2009; Chapter 8; pp. 313–329. [Google Scholar]
- Liu, Y.; Deng, B.; Du, J.; Zhang, G.; Hou, L. Nutrient burial and environmental changes in the Yangtze Delta in response to recent river basin human activities. Environ. Pollut. 2019, 249, 225–235. [Google Scholar] [CrossRef]
- Ogbeide, O.; Tongo, I.; Ezemonye, L. Risk assessment of agricultural pesticides in water, sediment, and fish from Owan River, Edo State, Nigeria. Environ. Monit. Assess 2015, 187, 654. [Google Scholar] [CrossRef]
- Pasquier, V.; Sansjofre, P.; Lebeau, O.; Liorzou, C.; Rabineau, M. Acid digestion on river influenced shelf sediment organic matter: Carbon and nitrogen contents and isotopic ratios. Rapid Commun. Mass Spectrom. 2018, 32, 86–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, Z.; Wang, X.; Han, G.; Liu, X.; Zhang, E. Organic and inorganic carbon and their stable isotopes in surface sediments of the Yellow River Estuary. Sci. Rep. 2018, 8, 10825. [Google Scholar] [CrossRef] [PubMed]
- Norton, C.D.; LeChevallier, M.W.; Falkinham, J.O., 3rd. Survival of Mycobacterium avium in a model distribution system. Water Res. 2004, 38, 1457–1466. [Google Scholar] [CrossRef]
- Williams, K.; Pruden, A.; Falkinham, J.O.; Edwards, M.; Williams, K.; Pruden, A.; Falkinham, J.O., III.; Edwards, M. Relationship between organic carbon and opportunistic pathogens in simulated glass water heaters. Pathogens 2015, 4, 355–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Voss, J.J.; Rutter, K.; Schroeder, B.G.; Barry, C.E., 3rd. Iron acquisition and metabolism by mycobacteria. J. Bacteriol. 1999, 181, 4443–4451. [Google Scholar] [CrossRef] [Green Version]
- Neyrolles, O.; Wolschendorf, F.; Mitra, A.; Niederweis, M. Mycobacteria, metals, and the macrophage. Immunol. Rev. 2015, 264, 249–263. [Google Scholar] [CrossRef]
- European Union. Directive 2000/54/EC of the European Parliament and of the Council of 18 September 2000 on the protection of workers from risks related to exposure to biological agents at work. Off. J. Eur. Communities 2000, L262, 21–45. [Google Scholar]
- Sing, A. (Ed.) Zoonoses—Infections Affecting Humans and Animals: Focus on Public Health Aspects; Springer: Heidelberg, Germany; Dordrecht, The Netherlands; London, UK; New York, NY, USA, 2015; 1143p. [Google Scholar]
- Ortel, S. Significance of new results in the research on human listeriosis. Zentralbl. Gynakol. 1983, 105, 1295–1306. (In German) [Google Scholar]
- Schaefer, H.E. Introduction into pathology of ocular zoonoses. Int. J. Med. Sci. 2009, 6, 120–122. [Google Scholar] [CrossRef] [Green Version]
- White, D. (Ed.) George Lucas (A & E Biography); Lerner Pub Group: Minneapolis, MN, USA, 1999; 128p. [Google Scholar]



| Species | Temperature 1 | Species | Temperature 1 |
|---|---|---|---|
| M. arabiense | 5–37 °C | M. murale | 10–37 °C |
| M. frederiksbergense | 15–37 °C | M. sediminis | 5–37 °C |
| M. hodleri | 18–37 °C |
| Species | Temperature 1 | Species | Temperature 1 |
|---|---|---|---|
| M. algericum | 25–40 °C | M. madagascariense | 22–31 °C |
| M. alsiense | 25–36 °C | M. mantenii | 25–37 °C |
| M. alvei | 25–37 °C | M. minnesotense | 27–34 °C |
| M. bohemicum | 25–40 °C | M. mucogenicum | 28–37 °C |
| M. brumae | 25–37 °C | M. noviomagense | 37 °C |
| M. celeriflavum | 37 °C | M. paraffinicum | 22–35 °C |
| M. chlorophenolicum | 18–37 °C | M. paragordonae | 25–30 °C |
| M. conspicuum | 22–31 °C | M. parakoreense | 37 °C |
| M. cookii | 22–31 °C | M. paraseoulense | 25–37 °C |
| M. doricum | 25–37 °C | M. paraterrae | 25–37 °C |
| M. engbaekii | 25–37 °C | M. peregrinum | 28–35 °C |
| M. europaeum | 30–37 °C | M. riyadhense | 25–36 °C |
| M. fragae | 30–37 °C | M. rufum | 28 °C |
| M. franklinii | 25–37 °C | M. salmoniphilum | 20–30 °C |
| M. fortuitum | 28–35 °C | M. senuense | 25–37 °C |
| M. heidelbergense | 30–37 °C | M. seoulense | 25–37 °C |
| M. heraklionense | 25–37 °C | M. septicum | 28–35 °C |
| M. hiberniae | 22–37 °C | M. setense | 25–37 °C |
| M. hippocampi | 25 °C | M. sherrisii | 25–37 °C |
| M. holsaticum | 20–40 °C | M. shigaense | 25–37 °C |
| M. immunogenum | 30–35 °C | M. shinjukuense | 30–37 °C |
| M. insubricum | 25–37 °C | M. shottsii | 23–30 °C |
| M. iranicum | 25–40 °C | M. simulans | 37 °C |
| M. interjectum | 31–37 °C | M. sinense | 28–37 °C |
| M. koreense | 25–37 °C | M. stomatepiae | 25–30 °C |
| M. kubicae | 28–37 °C | M. triplex | 37 °C |
| M. lentiflavum | 22–37 °C | M. tusciae | 25–32 °C |
| M. liflandii | 25–37 °C | M. vanbaalenii | 24–37 °C |
| M. litorale | 37 °C | M. yongonense | 37 °C |
| M. llatzerense | 22–30 °C |
| Species | Temperature 1 | Species | Temperature 1 |
|---|---|---|---|
| M. arosiense | 36–42 °C | M. indicus pranii | 25–45 °C |
| M. barrassiae | 25–42 °C | M. intermedium | 25–41 °C |
| M. bouchedurhonense | 30–45 °C | M. kumamotonense | 25–42 °C |
| M. bourgelatii | 25–42 °C | M. kyorinense | 28–42 °C |
| M. botniense | 36–50 °C | M. lacus | 25–42 °C |
| M. branderi | 25–45 °C | M. mageritense | 22–45 °C |
| M. celatum | 33–42 °C | M. marseillense | 30–45 °C |
| M. confluentis | 22–41 °C | M. monacense | 25–45 °C |
| M. elephantis | 25–45 °C | M. novocastrense | 25–43 °C |
| M. genavense | 25–42 °C | M. palustre | 22–42 °C |
| M. goodii | 30–45 °C | M. rutilum | 28–45 °C |
| M. hassiacum | 30–65 °C | M. timonense | 30–45 °C |
| M. heckeshornense | 30–45 °C | M. wolinskyi | 30–45 °C |
| Species | Species | Species | Species | Species |
|---|---|---|---|---|
| M. agri | M. confluentis | M. hiberniae | M. murale | M. rhodesiae |
| M. aichiense | M. cookii | M. hodleri | M. nebraskense | M. riyadhense |
| M. algericum | M. cosmeticum | M. holsaticum | M. neumannii | M. rufum |
| M. alvei | M. crocinum | M. insubricum | M. noviomagense | M. rutilum |
| M. aquaticum | M. diernhoferi | M. iranicum | M. obuense | M. salmoniphilum |
| M. aquiterrae | M. doricum | M. komossense | M. oryzae | M. sarraceniae |
| M. arabiense | M. duvalii | M. koreense | M. pallens | M. sediminis |
| M. arcueilense | M. eburneum | M. kumamotonense | M. paraffinicum | M. senuense |
| M. aromaticivorans | M. engbaekii | M. lacus | M. parafortuitum | M. seoulense |
| M. aurum | M. europaeum | M. lehmannii | M. paragordonae | M. shottsii |
| M. austroafricanum | M. fallax | M. litorale | M. parakoreense | M. sphagni |
| M. bohemicum | M. fluoranthenivorans | M. llatzerense | M. paraseoulense | M. stomatepiae |
| M. botniense | M. fragae | M. longobardum | M. paraterrae | M. talmoniae |
| M. bouchedurhonense | M. frederiksbergense | M. lutetiense | M. parmense | M. terrae |
| M. bourgelatii | M. gadium | M. madagascariense | M. phlei | M. thermoresistibile |
| M. brumae | M. gilvum | M. malmesburyense | M. poriferae | M. tokaiense |
| M. chitae | M. gordonae | M. minnesotense | M. pseudoshottsii | M. triviale |
| M. chlorophenolicum | M. grossiae | M. montefiorense | M. psychrotolerans | M. tusciae |
| M. chubuense | M. hassiacum | M. montmartrense | M. pulveris | M. vanbaalenii |
| M. conceptionense | M. helvum | M. moriokaense | M. pyrenivorans |
| Species | Species | Species | Species | Species |
|---|---|---|---|---|
| M. abscessus (M. abscessus ssp. abscessus, M. chelonae ssp. abscessus) | M. chelonae ssp. chelonae (M. chelonae) | M. hippocampi | M. mucogenicum | M. setense |
| M. alsense | M. chimaera | M. houstonense | M. neoaurum | M. sherrisii |
| M. arosiense | M. colombiense | M. immunogenum | M. neworleansense | M. shimoidei |
| M. arupense | M. conspicuum | M. interjectum | M. nonchromogenicum | M. shinjukuense |
| M. asiaticum | M. elephantis | M. intermedium | M. novocastrense | M. simiae |
| M. aubagnense | M. farcinogenes | M. intracellulare | M. palustre | M. smegmatis |
| M. avium ssp. avium (M. avium) | M. flavescens | M. kansasii | M. paraense | M. stephanolepidis |
| M. avium ssp. paratuberculosis (M. paratuberculosis) | M. florentinum | M. kubicae | M. paraintracellulare | M. szulgai |
| M. avium ssp. silvaticum | M. fortuitum ssp. acetamidolyticum | M. kyorinense | M. parascrofulaceum | M. timonense |
| M. bacteremicum | M. fortuitum ssp. fortuitum | M. lentiflavum | M. peregrinum | M. triplex |
| M. boenickei | M. franklinii | M. lepraemurium | M. persicum | M. vaccae |
| M. bolletii (M. abscessus ssp. bolletii) | M. gastri | M. mageritense | M. phocaicum | M. virginiense |
| M. branderi | M. genavense | M. malmoense | M. porcinum | M. vulneris |
| M. brisbanense | M. goodii | M. mantenii | M. saopaulense | M. wolinskyi |
| M. canariasense | M. haemophilum | M. marinum | M. saskatchewanense | M. xenopi |
| M. celatum | M. heckeshornense | M. marseillense | M. scrofulaceum | |
| M. celeriflavum | M. heidelbergense | M. massiliense (M. abscessus ssp. massiliense) | M. senegalense | |
| M. chelonae ssp. bovis | M. heraklionense | M. monacense | M. septicum |
| Species | Species |
|---|---|
| M. africanum | M. pinnipedii |
| M. bovis | M. tuberculosis (M. tuberculosis ssp. tuberculosis) |
| M. caprae (M. tuberculosis ssp. caprae) | M. microti |
| M. leprae | M. ulcerans |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pavlik, I.; Ulmann, V.; Hubelova, D.; Weston, R.T. Nontuberculous Mycobacteria as Sapronoses: A Review. Microorganisms 2022, 10, 1345. https://doi.org/10.3390/microorganisms10071345
Pavlik I, Ulmann V, Hubelova D, Weston RT. Nontuberculous Mycobacteria as Sapronoses: A Review. Microorganisms. 2022; 10(7):1345. https://doi.org/10.3390/microorganisms10071345
Chicago/Turabian StylePavlik, Ivo, Vit Ulmann, Dana Hubelova, and Ross Tim Weston. 2022. "Nontuberculous Mycobacteria as Sapronoses: A Review" Microorganisms 10, no. 7: 1345. https://doi.org/10.3390/microorganisms10071345






