Dendritic Cells/Macrophages-Targeting Feature of Ebola Glycoprotein and its Potential as Immunological Facilitator for Antiviral Vaccine Approach
Abstract
:1. Introduction
1.1. Dendritic cell (DC)-targeting Vaccines
1.2. Dendritic Cells (DCs)/Macrophages and Immune Responses
1.3. EBOV Infection and Immune Responses
2. EBOV GP: Bane or Benefit
3. The Interaction Between EBOV GP and DCs/Macrophages Can Induce Robust Innate and Adaptive Immune Responses
4. EBOV GP’s Affinity for Dendritic Cells and Macrophages in Ebola Virus Infection: An Insight for Vaccine Development
5. Ebola GP-Targeting DCs Can Facilitate Immune Responses for an Antiviral Vaccine Approach
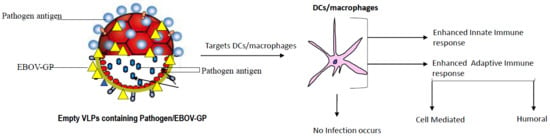
5.1. EBOV GP-Coated Virus-Like Particle Vaccine Approach (VLP)
5.2. EBOV GP and Vector-Based Vaccine
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Graham, B.S. Advances in antiviral vaccine development. Immunol. Rev. 2013, 255, 230–242. [Google Scholar] [CrossRef] [PubMed]
- Ada, G.L. The ideal vaccine. World J. Microbiol. Biotechnol. 1991, 7, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Norrby, E. Yellow fever and max theiler: The only nobel prize for a virus vaccine. J. Exp. Med. 2007, 204, 2779–2784. [Google Scholar] [CrossRef] [PubMed]
- He, H. Vaccines and antiviral agents. In Current Issues in Molecular Virology-Viral Genetics and Biotechnological Applications; InTech: London, UK, 2013. [Google Scholar] [CrossRef]
- World Health Organization. WHO Position paper on vaccines and vaccination against yellow fever. Weekly epidemiological record. Available online: https://www.who.int/wer/2013/wer8827.pdf?ua=1 (accessed on 5 July 2013).
- Grohskopf, L.A.; Sokolow, L.Z.; Broder, K.R.; Walter, E.B.; Fry, A.M.; Jernigan, D.B. Prevention and control of seasonal influenza with vaccines: Recommendations of the advisory committee on immunization practices-”united states, 2018–2019 influenza season. Mmwr Recomm. Rep. 2018, 67, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Sequeira, D.P.; Correia, R.; Carrondo, M.J.T.; Roldao, A.; Teixeira, A.P.; Alves, P.M. Combining stable insect cell lines with baculovirus-mediated expression for multi-ha influenza vlp production. Vaccine 2018, 36, 3112–3123. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, I.; Borggren, M.; Rosenstierne, M.W.; Trebbien, R.; Williams, J.A.; Vidal, E.; Vergara-Alert, J.; Foz, D.S.; Darji, A.; Sisteré-Oró, M.; et al. Protective effect of a polyvalent influenza DNA vaccine in pigs. Vet. Immunol. Immunopathol. 2018, 195, 25–32. [Google Scholar] [CrossRef]
- Jorba, J.; Diop, O.M.; Iber, J.; Henderson, E.; Sutter, R.W.; Wassilak, S.G.F.; Burns, C.C. Update on vaccine-derived polioviruses-worldwide, january 2016–june 2017. Mmwr. Morb. Mortal. Wkly. Rep. 2017, 66, 1185–1191. [Google Scholar] [CrossRef]
- Scott, H. James, Measles, mumps and rubella viruses. In Infectious Diseases; Elsevier: Amsterdam, The Netherlands, 2017; pp. 1399–1405.e1391. [Google Scholar]
- Van Damme, P.; Bonanni, P.; Bosch, F.X.; Joura, E.; Kjaer, S.K.G.; Meijer, C.J.L.M.; Petry, K.-U.; Soubeyrand, B.; Verstraeten, T.; Stanley, M. Use of the nonavalent hpv vaccine in individuals previously fully or partially vaccinated with bivalent or quadrivalent hpv vaccines. Vaccine 2016, 34, 757–761. [Google Scholar] [CrossRef]
- Uddin, M.N. Formulation of Bioactive Molecules: Antisense Oliginucleotide, Dexamethasone, and Human Papillomavirus (hpv) in a Novel Particulate Drug Delivery System. Ph.D. Thesis, Mercer University, Macon, GA, USA, September 2011. [Google Scholar]
- Zanetti, A.R.; Van Damme, P.; Shouval, D. The global impact of vaccination against hepatitis b: A historical overview. Vaccine 2008, 26, 6266–6273. [Google Scholar] [CrossRef]
- McAleer, W.J.; Buynak, E.B.; Maigetter, R.Z.; Wampler, D.E.; Miller, W.J.; Hilleman, M.R. Human hepatitis b vaccine from recombinant yeast. Nature 1984, 307, 178. [Google Scholar] [CrossRef]
- Mast, E.; Mahoney, F.; Kane, M.; Margolis, H. Hepatitis B vaccine. In Vaccines, 4th ed.; Plotkin, S.A., Orenstein, W.A., Eds.; W.B. Saunders Co: St. Louis, MO, USA, 2004; pp. 299–314. [Google Scholar]
- Gillet, Y.; Habermehl, P.; Thomas, S.; Eymin, C.; Fiquet, A. Immunogenicity and safety of concomitant administration of a measles, mumps and rubella vaccine (M-M-RvaxPro®) and a varicella vaccine (VARIVAX®) by intramuscular or subcutaneous routes at separate injection sites: A randomised clinical trial. BMC Med. 2009, 7, 16–27. [Google Scholar] [CrossRef] [PubMed]
- O‘Neal, C.M.; Crawford, S.E.; Estes, M.K.; Conner, M.E. Rotavirus virus-like particles administered mucosally induce protective immunity. J. Virol. 1997, 71, 8707–8717. [Google Scholar] [PubMed]
- Deen, J.; Lopez, A.L.; Kanungo, S.; Wang, X.-Y.; Anh, D.D.; Tapia, M.; Grais, R.F. Improving rotavirus vaccine coverage: Can newer-generation and locally produced vaccines help? Hum. Vaccines Immunother. 2018, 14, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Tohidi, F.; Sadat, S.M.; Bolhassani, A.; Yaghoubi, R.; Larijani, M.S. Induction of a robust humoral response using HIV-1 VLPMPER-V3 as a novel candidate vaccine in BALB/C mice. Curr. HIV Res. 2019, 17, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Zhu, Q.; Huang, X.; Yang, L.; Song, Y.; Zhu, P.; Zhou, P. In vivo electroporation in DNA-VLP prime-boost preferentially enhances HIV-1 envelope-specific IgG2a, neutralizing antibody and CD8 T cell responses. Vaccine 2017, 35, 2042–2051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, S.M.; Feldmann, H.; Ströher, U.; Geisbert, J.B.; Fernando, L.; Grolla, A.; Klenk, H.D.; Sullivan, N.J.; Volchkov, V.E.; Fritz, E.A.; et al. Live attenuated recombinant vaccine protects nonhuman primates against ebola and marburg viruses. Nat. Med. 2005, 11, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, S.B.; Bolay, F.; Kieh, M.; Grandits, G.; Badio, M.; Ballou, R.; Eckes, R.; Feinberg, M.; Follmann, D.; Grund, B.; et al. Phase 2 placebo-controlled trial of two vaccines to prevent ebola in liberia. N. Engl. J. Med. 2017, 377, 1438–1447. [Google Scholar] [CrossRef]
- Wang, M.; Jokinen, J.; Tretyakova, I.; Pushko, P.; Lukashevich, I.S. Alphavirus vector-based replicon particles expressing multivalent cross-protective lassa virus glycoproteins. Vaccine 2018, 36, 683–690. [Google Scholar] [CrossRef]
- McCormick, J.B.; Mitchell, S.W.; Kiley, M.P.; Ruo, S.; Fisher-Hoch, S.P. Inactivated lassa virus elicits a non protective immune response in rhesus monkeys. J. Med. Virol. 1992, 37, 1–7. [Google Scholar] [CrossRef]
- Cashman, K.A.; Wilkinson, E.R.; Wollen, S.E.; Shamblin, J.D.; Zelko, J.M.; Bearss, J.J.; Zeng, X.; Broderick, K.E.; Schmaljohn, C.S. DNA vaccines elicit durable protective immunity against individual or simultaneous infections with lassa and ebola viruses in guinea pigs. Hum. Vaccines Immunother. 2017, 13, 3010–3019. [Google Scholar] [CrossRef]
- Gans, H.; Yasukawa, L.; Rinki, M.; DeHovitz, R.; Forghani, B.; Beeler, J.; Audet, S.; Maldonado, Y.; Arvin, A.M. Immune responses to measles and mumps vaccination of infants at 6, 9, and 12 months. J. Infect. Dis. 2001, 184, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Meixlsperger, S.; Leung, C.S.; Rämer, P.C.; Pack, M.; Vanoaica, L.D.; Breton, G.; Pascolo, S.; Salazar, A.M.; Dzionek, A.; Schmitz, J. Cd141+ dendritic cells produce prominent amounts of ifn-γ after dsrna recognition and can be targeted via dec-205 in humanized mice. Blood 2013, 121, 5034–5044. [Google Scholar] [CrossRef] [PubMed]
- Banchereau, J.; Palucka, A.K. Dendritic cells as therapeutic vaccines against cancer. Nat. Rev. Immunol. 2005, 5, 296–306. [Google Scholar] [CrossRef] [PubMed]
- Brandão, J.G.; Scheper, R.J.; Lougheed, S.A.M.; Curiel, D.T.; Tillman, B.W.; Gerritsen, W.R.; Van Den Eertwegh, A.J.M.; Pinedo, H.M.; Haisma, H.J.; De Gruijl, T.D. Cd40-targeted adenoviral gene transfer to dendritic cells through the use of a novel bispecific single-chain FV antibody enhances cytotoxic T cell activation. Vaccine 2003, 21, 2268–2272. [Google Scholar] [CrossRef]
- Querec, T.; Bennouna, S.; Alkan, S.; Laouar, Y.; Gorden, K.; Flavell, R.; Akira, S.; Ahmed, R.; Pulendran, B. Yellow fever vaccine YF-17D activates multiple dendritic cell subsets via TLR2, 7, 8, and 9 to stimulate polyvalent immunity. J. Exp. Med. 2006, 203, 413–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, P.; Liu, X.; Sun, Y.; Zhou, P.; Wang, Y.; Zhang, Y. Dendritic cell targeted vaccines: Recent progresses and challenges. Hum. Vaccines Immunother. 2016, 12, 612–622. [Google Scholar] [CrossRef]
- Hawiger, D.; Inaba, K.; Dorsett, Y.; Guo, M.; Mahnke, K.; Rivera, M.; Ravetch, J.V.; Steinman, R.M.; Nussenzweig, M.C. Dendritic cells induce peripheral t cell unresponsiveness under steady state conditions in vivo. J. Exp. Med. 2001, 194, 769–780. [Google Scholar] [CrossRef] [PubMed]
- Zaneti, A.B.; Yamamoto, M.M.; Sulczewski, F.B.; Almeida, B.d.S.; Souza, H.F.S.; Ferreira, N.l.S.; Maeda, D.L.N.F.; Sales, N.S.; Rosa, D.S.; Ferreira, S.; et al. Dendritic cell targeting using a DNA vaccine induces specific antibodies and CD4+ T cells to the dengue virus envelope protein domain III. Front. Immunol. 2019, 10, 1–15. [Google Scholar] [CrossRef]
- Cheng, C.; Gall, J.G.D.; Kong, W.-P.; Sheets, R.L.; Gomez, P.L.; King, C.R.; Nabel, G.J. Mechanism of AD5 vaccine immunity and toxicity: Fiber shaft targeting of dendritic cells. PLoS Pathog. 2007, 3, e25–e32. [Google Scholar] [CrossRef]
- Boudewijns, S.; Westdorp, H.; Koornstra, R.H.T.; Aarntzen, E.H.J.G.; Schreibelt, G.; Creemers, J.H.A.; Punt, C.J.A.; Figdor, C.G.; de Vries, I.J.M.; Gerritsen, W.R. Immune-related adverse events of dendritic cell vaccination correlate with immunologic and clinical outcome in stage iii and iv melanoma patients. J. Immunother. (Hagerstown Md. 1997) 2016, 39, 241–248. [Google Scholar] [CrossRef]
- Almand, B.; Clark, J.I.; Nikitina, E.; van Beynen, J.; English, N.R.; Knight, S.C.; Carbone, D.P.; Gabrilovich, D.I. Increased production of immature myeloid cells in cancer patients: A mechanism of immunosuppression in cancer. J. Immunol. 2001, 166, 678–689. [Google Scholar] [CrossRef] [PubMed]
- Apostólico, J.d.S.; Lunardelli, V.A.S.; Yamamoto, M.M.; Souza, H.F.S.; Cunha-Neto, E.; Boscardin, S.B.; Rosa, D.S. Dendritic cell targeting effectively boosts t cell responses elicited by an hiv multiepitope DNA vaccine. Front. Immunol. 2017, 8, 101–117. [Google Scholar] [CrossRef]
- Graham, J.P.; Authie, P.; Palucka, A.K.; Zurawski, G. Targeting interferon-alpha to dendritic cells enhances a CD8+ T cell response to a human CD40-targeted cancer vaccine. Vaccine 2017, 35, 4532–4539. [Google Scholar] [CrossRef] [PubMed]
- Garu, A.; Moku, G.; Gulla, S.K.; Chaudhuri, A. Genetic immunization with in vivo dendritic cell-targeting liposomal DNA vaccine carrier induces long-lasting antitumor immune response. Mol. Ther. 2016, 24, 385–397. [Google Scholar] [CrossRef] [PubMed]
- Nchinda, G.; Kuroiwa, J.; Oks, M.; Trumpfheller, C.; Park, C.G.; Huang, Y.; Hannaman, D.; Schlesinger, S.J.; Mizenina, O.; Nussenzweig, M.C. The efficacy of DNA vaccination is enhanced in mice by targeting the encoded protein to dendritic cells. J. Clin. Investig. 2008, 118, 1427–1436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fossum, E.; Gradeland, G.; Terhorst, D.; Tveita, A.A.; Vikse, E.; Mjaaland, S.; Henri, S.; Malissen, B.; Bogen, B. Vaccine molecules targeting Xcr1 on cross-presenting dcs induce protective CD8+ T-cell responses against influenza virus. Eur. J. Immunol. 2014, 45, 624–635. [Google Scholar] [CrossRef]
- Gudjonsson, A.; Lysén, A.; Balan, S.; Sundvold-Gjerstad, V.; Arnold-Schrauf, C.; Richter, L.; Bækkevold, E.S.; Dalod, M.; Bogen, B.; Fossum, E. Targeting influenza virus hemagglutinin to Xcr1+ dendritic cells in the absence of receptor-mediated endocytosis enhances protective antibody responses. J. Immunol. 2017, 198, 2785–2795. [Google Scholar] [CrossRef] [PubMed]
- Ye, C.; Choi, J.G.; Abraham, S.; Shankar, P.; Manjunath, N. Targeting DNA vaccines to myeloid cells using a small peptide. Eur. J. Immunol. 2015, 45, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Varol, C.; Mildner, A.; Jung, S. Macrophages: Development and tissue specialization. Annu. Rev. Immunol. 2015, 33, 643–675. [Google Scholar] [CrossRef]
- Steinman, R.M.; Hemmi, H. Dendritic cells: Translating innate to adaptive immunity. In From Innate Immunity to Immunological Memor; Springer: Berlin, Heidelberg, 2006; pp. 17–58. [Google Scholar]
- Jego, G.; Palucka, A.K.; Blanck, J.-P.; Chalouni, C.; Pascual, V.; Banchereau, J. Plasmacytoid dendritic cells induce plasma cell differentiation through type i interferon and interleukin 6. Immunity 2003, 19, 225–234. [Google Scholar] [CrossRef]
- Fernandez, N.C.; Lozier, A.; Flament, C.; Ricciardi-Castagnoli, P.; Bellet, D.; Suter, M.; Perricaudet, M.; Tursz, T.; Maraskovsky, E.; Zitvogel, L. Dendritic cells directly trigger nk cell functions: Cross-talk relevant in innate anti-tumor immune responses in vivo. Nat. Med. 1999, 5, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Heink, S.; Yogev, N.; Garbers, C.; Herwerth, M.; Aly, L.; Gasperi, C.; Husterer, V.; Croxford, A.L.; Möller-Hackbarth, K.; Bartsch, H.S.; et al. Trans-presentation of IL-6 by dendritic cells is required for the priming of pathogenic TH17 cells. Nat. Immunol. 2017, 18, 74–85. [Google Scholar] [CrossRef] [PubMed]
- Humeniuk, P.; Dubiela, P.; Hoffmann-Sommergruber, K. Dendritic cells and their role in allergy: Uptake, proteolytic processing and presentation of allergens. Int. J. Mol. Sci. 2017, 18, 1491. [Google Scholar] [CrossRef] [PubMed]
- Chun, I.Y.; Becker, C.; Metang, P.; Marches, F.; Wang, Y.; Toshiyuki, H.; Banchereau, J.; Merad, M.; Palucka, K. Human CD141+ dendritic cells induce CD4+ T cells to produce type 2 cytokines. J. Immunol. 2014, 193, 4335–4343. [Google Scholar]
- Figdor, C.G.; van Kooyk, Y.; Adema, G.J. C-type lectin receptors on dendritic cells and langerhans cells. Nat. Rev. Immunol. 2002, 2, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, K.; Dhodapkar, K.M.; Dhodapkar, M.V. Targeting human dendritic cells in situ to improve vaccines. Immunol. Lett. 2014, 162, 59–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, C.L.; Aumeunier, A.M.; Mowat, A.M. Intestinal CD103+ dendritic cells: Master regulators of tolerance? Trends Immunol. 2011, 32, 412–419. [Google Scholar] [CrossRef]
- Christmas, P. Toll-like receptors: Sensors that detect infection. Nat. Educ. 2010, 3, 85. [Google Scholar]
- Arpaia, N.; Barton, G.M. The impact of toll-like receptors on bacterial virulence strategies. Curr. Opin. Microbiol. 2013, 16, 17–22. [Google Scholar] [CrossRef]
- Kawai, T.; Akira, S. The role of pattern-recognition receptors in innate immunity: Update on toll-like receptors. Nat. Immunol. 2010, 11, 373. [Google Scholar] [CrossRef]
- Fukuda, D.; Nishimoto, S.; Aini, K.; Tanaka, A.; Nishiguchi, T.; Kim-Kaneyama, J.-R.; Lei, X.-F.; Masuda, K.; Naruto, T.; Tanaka, K. Toll-like receptor 9 plays a pivotal role in angiotensin II-induced atherosclerosis. J. Am. Heart Assoc. 2019, 8, e010860–e010884. [Google Scholar] [CrossRef] [PubMed]
- Koblansky, A.A.; Jankovic, D.; Oh, H.; Hieny, S.; Sungnak, W.; Mathur, R.; Hayden, M.S.; Akira, S.; Sher, A.; Ghosh, S. Recognition of profilin by toll-like receptor 12 is critical for host resistance to toxoplasma gondii. Immunity 2013, 38, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, A.; Pierce, S.K. How location governs toll-like receptor signaling. Traffic 2009, 10, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Raetz, M.; Kibardin, A.; Sturge, C.R.; Pifer, R.; Li, H.; Burstein, E.; Ozato, K.; Larin, S.; Yarovinsky, F. Cooperation of TLR12 and TLR11 in the IRF8-dependent IL-12 response to toxoplasma gondii profilin. J. Immunol. 2013, 191, 4818–4827. [Google Scholar] [CrossRef]
- Majewska, M.; Szczepanik, M. The role of toll-like receptors (TLR) in innate and adaptive immune responses and their function in immune response regulation. Postepy Hig. I Med. Dosw. (Online) 2006, 60, 52–63. [Google Scholar] [PubMed]
- Okumura, A.; Pitha, P.M.; Yoshimura, A.; Harty, R.N. Interaction between ebola virus glycoprotein and host toll-like receptor 4 leads to induction of proinflammatory cytokines and socs1. J. Virol. 2010, 84, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.-Y.; Strange, D.P.; Wong, T.A.S.; Lehrer, A.T.; Verma, S. Ebola virus glycoprotein induces an innate immune response in vivo via TLR4. Front. Microbiol. 2017, 8, 1571–1586. [Google Scholar] [CrossRef] [PubMed]
- Goubau, D.; Schlee, M.; Deddouche, S.; Pruijssers, A.J.; Zillinger, T.; Goldeck, M.; Schuberth, C.; Van der Veen, A.G.; Fujimura, T.; Rehwinkel, J. Antiviral immunity via RIG-I-mediated recognition of RNA bearing 5’-diphosphates. Nature 2017, 514, 372–375. [Google Scholar] [CrossRef]
- Martinez, I.; Oliveros, J.C.; Cuesta, I.; de la Barrera, J.; Ausina, V.; Casals, C.; de Lorenzo, A.; Garcia, E.; Garcia-Fojeda; Garmendia, J. Apoptosis, toll-like, RIG-I-like and nod-like receptors are pathways jointly induced by diverse respiratory bacterial and viral pathogens. Front. Microbiol. 2017, 8, 276. [Google Scholar] [CrossRef]
- Weber, M.; Gawanbacht, A.; Habjan, M.; Rang, A.; Borner, C.; Schmidt, A.M.; Veitinger, S.; Jacob, R.; Devignot, S.P.; Kochs, G. Incoming RNA virus nucleocapsids containing a 5’-triphosphorylated genome activate RIG-I and antiviral signaling. Cell Host Microbe 2013, 13, 336–346. [Google Scholar] [CrossRef]
- He, F.; Melen, K.; Maljanen, S.; Lundberg, R.; Jiang, M.; Osterlund, P.; Kakkola, L.; Julkunen, I. Ebolavirus protein VP24 interferes with innate immune responses by inhibiting interferon-λ1 gene expression. Virology 2017, 509, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Ting, J.P.Y.; Duncan, J.A.; Lei, Y. How the noninflammasome nlrs function in the innate immune system. Science 2010, 327, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Inohara, N.; Ogura, Y.; Fontalba, A.; Gutierrez, O.; Pons, F.; Crespo, J.; Fukase, K.; Inamura, S.; Kusumoto, S.; Hashimoto, M. Host recognition of bacterial muramyl dipeptide mediated through NOD2 implications for crohn’s disease. J. Biol. Chem. 2003, 278, 5509–5512. [Google Scholar] [CrossRef] [PubMed]
- Heath, W.R.; Carbone, F.R. Dendritic cell subsets in primary and secondary T cell responses at body surfaces. Nat. Immunol. 2009, 10, 1237–1244. [Google Scholar] [CrossRef]
- Ueno, H.; Schmitt, N.; Palucka, A.K.; Banchereau, J. Dendritic cells and humoral immunity in humans. Immunol. Cell Biol. 2010, 88, 376–380. [Google Scholar] [CrossRef]
- Uematsu, S.; Fujimoto, K.; Jang, M.H.; Yang, B.-G.; Jung, Y.-J.; Nishiyama, M.; Sato, S.; Tsujimura, T.; Yamamoto, M.; Yokota, Y. Regulation of humoral and cellular gut immunity by lamina propria dendritic cells expressing toll-like receptor 5. Nat. Immunol. 2008, 9, 769–776. [Google Scholar] [CrossRef]
- Steinman, R.M.; Banchereau, J. Taking dendritic cells into medicine. Nature 2007, 449, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Dang, Y.; Wagner, W.M.; Gad, E.; Rastetter, L.; Berger, C.M.; Holt, G.E.; Disis, M.L. Dendritic cell-activating vaccine adjuvants differ in the ability to elicit antitumor immunity due to an adjuvant-specific induction of immunosuppressive cells. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2012, 18, 3122–3131. [Google Scholar] [CrossRef]
- Steinman, R.M.; Bona, C.; Inaba, K. Dendritic Cells: Important Adjuvants during DNA Vaccination; Landes Bioscience: Georgetown, TX, USA, 2002. [Google Scholar]
- Epelman, S.; Lavine, K.J.; Randolph, G.J. Origin and functions of tissue macrophages. Immunity 2014, 41, 21–35. [Google Scholar] [CrossRef]
- Sang, Y.; Miller, L.C.; Blecha, F. Macrophage polarization in virus-host interactions. J. Clin. Cell. Immunol. 2015, 6, 311–334. [Google Scholar]
- Delves, P.J.; Martin, S.J.; Burton, D.R.; Roitt, I.M. Essential Immunology; Chichester, West Sussex John Wiley & Sons: Hoboken, NJ, USA, 2017. [Google Scholar]
- Ferenbach, D.; Hughes, J. Macrophages and dendritic cells: What is the difference? Kidney Int. 2008, 74, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Quattrocchi, V.; Langellotti, C.; Pappalardo, J.S.N.; Olivera, V.; Di Giacomo, S.N.; Van Rooijen, N.; Mongini, C.; Waldner, C.; Zamorano, P.I.S. Role of macrophages in early protective immune responses induced by two vaccines against foot and mouth disease. Antivir. Res. 2011, 92, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Bermejo-Jambrina, M.; Eder, J.; Helgers, L.C.; Hertoghs, N.; Nijmeijer, B.M.; Stunnenberg, M.; Geijtenbeek, T.B.H. C-type lectin receptors in antiviral immunity and viral escape. Front. Immunol. 2018, 9, 590–602. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A. Ebola virus altered innate and adaptive immune response signalling pathways: Implications for novel therapeutic approaches. Infect. Disord. Drug Targets (Former. Curr. Drug Targets-Infect. Disord.) 2016, 16, 79–94. [Google Scholar] [CrossRef]
- Bosio, C.M.; Aman, M.J.; Grogan, C.; Hogan, R.; Ruthel, G.; Negley, D.; Mohamadzadeh, M.; Bavari, S.; Schmaljohn, A. Ebola and marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. J. Infect. Dis. 2003, 188, 1630–1638. [Google Scholar] [CrossRef] [PubMed]
- Marcinkiewicz, J.; Bryniarski, K.; Nazimek, K. Ebola haemorrhagic fever virus: Pathogenesis, immune responses, potential prevention. Folia Med. Cracov. 2014, 54, 39–48. [Google Scholar] [PubMed]
- Martinez, O.; Leung, L.W.; Basler, C.F. The role of antigen-presenting cells in filoviral hemorrhagic fever: Gaps in current knowledge. Antivir. Res. 2012, 93, 416–428. [Google Scholar] [CrossRef] [PubMed]
- Hensley, L.E.; Young, H.A.; Jahrling, P.B.; Geisbert, T.W. Proinflammatory response during ebola virus infection of primate models: Possible involvement of the tumor necrosis factor receptor superfamily. Immunol. Lett. 2002, 80, 169–179. [Google Scholar] [CrossRef]
- Marzi, A.; Muller, P.; Hanna, S.L.; Harrer, T.; Eisemann, J.; Steinkasserer, A.; Becker, S.; Baribaud, F.; Pohlmann, S. Analysis of the interaction of ebola virus glycoprotein with DC-SIGN (dendritic cell-specific intercellular adhesion molecule 3-grabbing nonintegrin) and its homologue dc-signr. J. Infect. Dis. 2007, 196, S237–S246. [Google Scholar] [CrossRef]
- Younan, P.; Iampietro, M.; Bukreyev, A. Disabling of lymphocyte immune response by Ebola virus. PLoS Pathog. 2018, 14, e1006932–e1006939. [Google Scholar] [CrossRef]
- Lubaki, N.M.; Ilinykh, P.; Pietzsch, C.; Tigabu, B.; Freiberg, A.N.; Koup, R.A.; Bukreyev, A. The lack of maturation of Ebola virus-infected dendritic cells results from the cooperative effect of at least two viral domains. J. Virol. 2013, 87, 7471–7485. [Google Scholar] [CrossRef] [PubMed]
- Lubaki, N.M.; Younan, P.; Santos, R.I.; Meyer, M.; Iampietro, M.; Koup, R.A.; Bukreyev, A. The ebola interferon inhibiting domains attenuate and dysregulate cell-mediated immune responses. PLoS Pathog. 2016, 12, e1006031–e1006065. [Google Scholar] [CrossRef] [PubMed]
- Groseth, A.; Marzi, A.; Hoenen, T.; Herwig, A.; Gardner, D.; Becker, S.; Ebihara, H.; Feldmann, H. The ebola virus glycoprotein contributes to but is not sufficient for virulence in vivo. PLoS Pathog. 2012, 8, e1002847–e1002859. [Google Scholar] [CrossRef] [PubMed]
- Baize, S.; Leroy, E.M.; Georges, A.J.; Georges-Courbot; Capron, M.; Bedjabaga, I.; Lansouda-Soukate, J.; Mavoungou, E. Inflammatory responses in ebola virus-infected patients. Clin. Exp. Immunol. 2002, 128, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Leroy, E.M.; Gonzalez, J.-P.; Baize, S. Ebola and marburg haemorrhagic fever viruses: Major scientific advances, but a relatively minor public health threat for africa. Clin. Microbiol. Infect. 2011, 17, 964–976. [Google Scholar] [CrossRef] [PubMed]
- Ludtke, A.; Ruibal, P.; Becker-Ziaja, B.; Rottstegge, M.; Wozniak, D.M.; Cabeza-Cabrerizo, M.; Thorenz, A.; Weller, R.; Kerber, R.; Idoyaga, J. Ebola virus disease is characterized by poor activation and reduced levels of circulating CD16+ monocytes. J. Infect. Dis. 2016, 214, S275–S280. [Google Scholar] [CrossRef] [PubMed]
- Lüdtke, A.; Ruibal, P.; Wozniak, D.M.; Pallasch, E.; Wurr, S.; Bockholt, S.; Gómez-Medina, S.; Qiu, X.; Kobinger, G.P.; RodrÃguez, E. Ebola virus infection kinetics in chimeric mice reveal a key role of T cells as barriers for virus dissemination. Sci. Rep. 2017, 7, 43776–43786. [Google Scholar] [CrossRef] [PubMed]
- Silvin, A.; Chun, I.Y.; Lahaye, X.; Imperatore, F.; Brault, J.-B.; Cardinaud, S.; Becker, C.; Kwan, W.-H.; Conrad, C.; Maurin, M. Constitutive resistance to viral infection in human CD141+ dendritic cells. Sci. Immunol. 2017, 2, eaai8071–eaai8099. [Google Scholar] [CrossRef] [PubMed]
- Wahl-Jensen, V.; Kurz, S.; Feldmann, F.; Buehler, L.K.; Kindrachuk, J.; DeFilippis, V.; da Silva Correia, J.; Fruh, K.; Kuhn, J.H.; Burton, D.R. Ebola virion attachment and entry into human macrophages profoundly effects early cellular gene expression. PLoS Negl. Trop. Dis. 2011, 5, e1359–e1375. [Google Scholar] [PubMed]
- Rao, M.; Bray, M.; Alving, C.R.; Jahrling, P.; Matyas, G.R. Induction of immune responses in mice and monkeys to ebola virus after immunization with liposome-encapsulated irradiated ebola virus: Protection in mice requires cd4+ t cells. J. Virol. 2002, 76, 9176–9185. [Google Scholar] [CrossRef] [PubMed]
- Ayithan, N.; Bradfute, S.B.; Anthony, S.M.; Stuthman, K.S.; Dye, J.M.; Bavari, S.; Bray, M.; Ozato, K. Ebola virus-like particles stimulate type i interferons and proinflammatory cytokine expression through the toll-like receptor and interferon signaling pathways. J. Interferon Cytokine Res. 2014, 34, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Regules, J.A.; Beigel, J.H.; Paolino, K.M.; Voell, J.; Castellano, A.R.; Hu, Z.; MuÃoz, P.; Moon, J.E.; Ruck, R.C.; Bennett, J.W. A recombinant vesicular stomatitis virus ebola vaccine. N. Engl. J. Med. 2017, 376, 330–341. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.E.; Fusco, M.L.; Hessell, A.J.; Oswald, W.B.; Burton, D.R.; Saphire, E.O. Structure of the ebola virus glycoprotein bound to an antibody from a human survivor. Nature 2008, 454, 177. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, A.; Trappier, S.G.; Mahy, B.W.; Peters, C.J.; Nichol, S.T. The virion glycoproteins of ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc. Natl. Acad. Sci. USA 1996, 93, 3602–3607. [Google Scholar] [CrossRef] [PubMed]
- Alazard-Dany, N.; Volchkova, V.; Reynard, O.; Carbonnelle, C.; Dolnik, O.; Ottmann, M.; Khromykh, A.; Volchkov, V.E. Ebola virus glycoprotein gp is not cytotoxic when expressed constitutively at a moderate level. J. Gen. Virol. 2006, 87, 1247–1257. [Google Scholar] [CrossRef] [PubMed]
- Volchkov, V.E.; Feldmann, H.; Volchkova, V.A.; Klenk, H.-D. Processing of the ebola virus glycoprotein by the proprotein convertase furin. Proc. Natl. Acad. Sci. USA 1998, 95, 5762–5767. [Google Scholar] [CrossRef]
- Lee, J.E.; Saphire, E.O. Ebolavirus glycoprotein structure and mechanism of entry. Future Virol. 2009, 4, 621–635. [Google Scholar] [CrossRef]
- Jeffers, S.A.; Sanders, D.A.; Sanchez, A. Covalent modifications of the ebola virus glycoprotein. J. Virol. 2002, 76, 12463–12472. [Google Scholar] [CrossRef]
- Martinez, O.; Tantral, L.; Mulherkar, N.; Chandran, K.; Basler, C.F. Impact of ebola mucin-like domain on antiglycoprotein antibody responses induced by Ebola virus-like particles. J. Infect. Dis. 2011, 204, S825–S832. [Google Scholar] [CrossRef]
- Lennemann, N.J.; Rhein, B.A.; Ndungo, E.; Chandran, K.; Qiu, X.; Maury, W. Comprehensive functional analysis of N-linked glycans on Ebola virus GP1. mBio 2014, 5, e00862-13. [Google Scholar] [CrossRef]
- Zhao, D.; Han, X.; Zheng, X.; Wang, H.; Yang, Z.; Liu, D.; Han, K.; Liu, J.; Wang, X.; Yang, W. The Myeloid LSECtin is a DAP12-coupled receptor that is crucial for inflammatory response induced by Ebola virus Glycoprotein. PLoS Pathog. 2016, 12, e1005487–e1005502. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, C.P.; Lasala, F.; Carrillo, J.; Muiz, O.; Corbi, A.L.; Delgado, R. C-type lectins DC-SIGN and L-SIGN mediate cellular entry by Ebola virus in cis and in trans. J. Virol. 2002, 76, 6841–6844. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Soto, A.A.; Aragoneses-Fenoll, L.; Martin-Gayo, E.; Martinez-Prats, L.; Colmenares, M.; Naranjo-Gomez, M.; Borras, F.E.; Munoz, P.; Zubiaur, M.; Toribio, M.L. The DC-SIGN-“related lectin LSECtin mediates antigen capture and pathogen binding by human myeloid cells. Blood 2007, 109, 5337–5345. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Imai, Y.; Higashi, N.; Kumamoto, Y.; Onami, T.M.; Hedrick, S.M.; Irimura, T. Lack of antigen-specific tissue remodeling in mice deficient in the macrophage galactose-type calcium-type LECtin 1/CD301A. Blood 2005, 106, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Imai, Y.; Higashi, N.; Kumamoto, Y.; Mukaida, N.; Irimura, T. Redistributions of macrophages expressing the macrophage galactose-type C-type lectin (MGL) during antigen-induced chronic granulation tissue formation. Int. Immunol. 2005, 17, 559–568. [Google Scholar] [CrossRef] [Green Version]
- Bornholdt, Z.A.; Ndungo, E.; Fusco, M.L.; Bale, S.; Flyak, A.I.; Crowe, J.E.; Chandran, K.; Saphire, E.O. Host-primed ebola virus gp exposes a hydrophobic npc1 receptor-binding pocket, revealing a target for broadly neutralizing antibodies. mBio 2016, 7, e02154-15. [Google Scholar] [CrossRef] [PubMed]
- Ao, Z.; Wang, L.; Mendoza, E.J.; Cheng, K.; Zhu, W.; Cohen, E.A.; Fowke, K.; Qiu, X.; Kobinger, G.; Yao, X. Incorporation of Ebola glycoprotein into hiv particles facilitates dendritic cell and macrophage targeting and enhances HIV-specific immune responses. PLoS ONE 2019, 14, e0216949–e0217067. [Google Scholar] [CrossRef]
- Wong, G.; Qiu, X.; Ebihara, H.; Feldmann, H.; Kobinger, G.P. Characterization of a bivalent vaccine capable of inducing protection against both Ebola and cross-clade H5N1 influenza in mice. J. Infect. Dis. 2015, 212, S435–S442. [Google Scholar] [CrossRef]
- Khataby, K.; Kasmi, Y.; Hammou, R.A.; Laasri, F.E.; Boughribi, S.; Ennaji, M.M. Ebola virus’s glycoproteins and entry mechanism. In Ebola; InTech: London, UK, 2016. [Google Scholar] [CrossRef]
- Majid, M.U.; Tahir, M.S.; Ali, Q.; Rao, A.Q.; Rashid, B.; Ali, A.; Nasir, I.A.; Husnain, T. Nature and history of Ebola virus: An overview. Arch. Neurosci. 2016, 3, e35027–e35038. [Google Scholar] [CrossRef]
- Ning, Y.-J.; Deng, F.; Hu, Z.; Wang, H. The roles of ebolavirus glycoproteins in viral pathogenesis. Virol. Sin. 2017, 32, 3–15. [Google Scholar] [CrossRef]
- Francica, J.R.; Varela-Rohena, A.; Medvec, A.; Plesa, G.; Riley, J.L.; Bates, P. Steric shielding of surface epitopes and impaired immune recognition induced by the Ebola virus glycoprotein. PLoS Pathog. 2010, 6, e1001098–e1001113. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.-Y.; Duckers, H.J.; Sullivan, N.J.; Sanchez, A.; Nabel, E.G.; Nabel, G.J. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat. Med. 2000, 6, 886–889. [Google Scholar] [CrossRef] [PubMed]
- Hood, C.L.; Abraham, J.; Boyington, J.C.; Leung, K.; Kwong, P.D.; Nabel, G.J. Biochemical and structural characterization of cathepsin L-processed ebola virus glycoprotein: Implications for viral entry and immunogenicity. J. Virol. 2010, 84, 2972–2982. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Ren, J.; Harlos, K.; Jones, D.M.; Zeltina, A.; Bowden, T.A.; Padilla-Parra, S.; Fry, E.E.; Stuart, D.I. Toremifene interacts with and destabilizes the Ebola virus glycoprotein. Nature 2016, 535, 169–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.; Nyenhuis, D.A.; Nelson, E.A.; Cafiso, D.S.; White, J.M.; Tamm, L.K. Structure of the Ebola virus envelope protein MPER/TM domain and its interaction with the fusion loop explains their fusion activity. Proc. Natl. Acad. Sci. USA 2017, 114, 177–182. [Google Scholar] [CrossRef]
- Wang, B.; Wang, Y.; Frabutt, D.A.; Zhang, X.; Yao, X.; Hu, D.; Zhang, Z.; Liu, C.; Zheng, S.; Xiang, S.-H. Mechanistic understanding of N-glycosylation in Ebola virus glycoprotein maturation and function. J. Biol. Chem. 2017, 292, 5860–5870. [Google Scholar] [CrossRef] [Green Version]
- De La Vega, M.-A.; Wong, G.; Kobinger, G.P.; Qiu, X. The multiple roles of sGP in Ebola pathogenesis. Viral Immunol. 2015, 28, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Radoshitzky, S.R.; Warfield, K.L.; Chi, X.; Dong, L.; Kota, K.; Bradfute, S.B.; Gearhart, J.D.; Retterer, C.; Kranzusch, P.J.; Misasi, J.N. Ebolavirus δ-peptide immunoadhesins inhibit marburgvirus and Ebolavirus cell entry. J. Virol. 2011, 85, 8502–8513. [Google Scholar] [CrossRef]
- Volchkova, V.A.; Feldmann, H.; Klenk, H.-D.; Volchkov, V.E. The nonstructural small glycoprotein sGP of Ebola virus is secreted as an antiparallel-orientated homodimer. Virology 1998, 250, 408–414. [Google Scholar] [CrossRef]
- Wahl-Jensen, V.; Kurz, S.K.; Hazelton, P.R.; Schnittler, H.-J.; StrÃher, U.; Burton, D.R.; Feldmann, H. Role of Ebola virus secreted glycoproteins and virus-like particles in activation of human macrophages. J. Virol. 2005, 79, 2413–2419. [Google Scholar] [CrossRef]
- Monath, T.P.; Fast, P.E.; Modjarrad, K.; Clarke, D.K.; Martin, B.K.; Fusco, J.; Nichols, R.; Heppner, D.G.; Simon, J.K.; Dubey, S. rVSV ”G-ZEBOV-GP (also designated V920) recombinant vesicular stomatitis virus pseudotyped with Ebola Zaire Glycoprotein: Standardized template with key considerations for a risk/benefit assessment. Vaccine X 2019, 1, 100009. [Google Scholar] [CrossRef] [PubMed]
- Ilinykh, P.A.; Shen, X.; Flyak, A.I.; Kuzmina, N.; Ksiazek, T.G.; Crowe, J.E.; Bukreyev, A. Chimeric filoviruses for identification and characterization of monoclonal antibodies. J. Virol. 2016, 90, 3890–3901. [Google Scholar] [CrossRef] [PubMed]
- Huttner, A.; Dayer, J.-A.; Yerly, S.; Combescure, C.; Auderset, F.; Desmeules, J.; Eickmann, M.; Finckh, A.; Goncalves, A.R.; Hooper, J.W. The effect of dose on the safety and immunogenicity of the VSV Ebola candidate vaccine: A randomised double-blind, placebo-controlled phase 1/2 trial. Lancet Infect. Dis. 2015, 15, 1156–1166. [Google Scholar] [CrossRef]
- Pallesen, J.; Murin, C.D.; de Val, N.; Cottrell, C.A.; Hastie, K.M.; Turner, H.L.; Fusco, M.L.; Flyak, A.I.; Zeitlin, L.; Crowe, J.E., Jr. Structures of Ebola virus GP and sGP in complex with therapeutic antibodies. Nat. Microbiol. 2017, 1, 16128–16151. [Google Scholar] [CrossRef]
- Davidson, E.; Bryan, C.; Fong, R.H.; Barnes, T.; Pfaff, J.; Mabila, M.; Rucker, J.B.; Doranz, B.J. Mechanism of binding to Ebola virus glycoprotein by the ZMapp, ZMAb, and MB-003 cocktail antibodies. J. Virol. 2015, 89, 10982–10992. [Google Scholar] [CrossRef]
- Hacke, M.; Björkholm, P.; Hellwig, A.; Himmels, P.; Ruiz de Almodóvar, C.; Brügger, B.; Wieland, F.; Ernst, A.M. Inhibition of Ebola virus glycoprotein-mediated cytotoxicity by targeting its transmembrane domain and cholesterol. Nat. Commun. 2015, 6, 7688–7697. [Google Scholar] [CrossRef]
- Mohan, G.S.; Li, W.; Ye, L.; Compans, R.W.; Yang, C. Antigenic subversion: A novel mechanism of host immune evasion by Ebola virus. PLoS Pathog. 2012, 8, e1003065–e1003079. [Google Scholar] [CrossRef]
- Speranza, E.; Connor, J.H. Host transcriptional response to Ebola virus infection. Vaccines 2017, 5, 30. [Google Scholar] [CrossRef]
- Agnandji, S.T.; Huttner, A.; Zinser, M.E.; Njuguna, P.; Dahlke, C.; Fernandes, J.F.; Yerly, S.; Dayer, J.-A.; Kraehling, V.; Kasonta, R. Phase 1 trials of rVSV Ebola vaccine in africa and europe. N. Engl. J. Med. 2016, 374, 1647–1660. [Google Scholar] [CrossRef]
- Marzi, A.; Engelmann, F.; Feldmann, F.; Haberthur, K.; Shupert, W.L.; Brining, D.; Scott, D.P.; Geisbert, T.W.; Kawaoka, Y.; Katze, M.G. Antibodies are necessary for rVSV/ZEBOV-GP-mediated protection against lethal Ebola virus challenge in nonhuman primates. Proc. Natl. Acad. Sci. USA 2012, 110, 1893–1898. [Google Scholar] [CrossRef]
- Venkatraman, N.; Silman, D.; Folegatti, P.M.; Hill, A.V.S. Vaccines against Ebola virus. Vaccine 2017, 36, 5454–5459. [Google Scholar] [CrossRef] [PubMed]
- Takada, A.; Kawaoka, Y. Antibody-dependent enhancement of viral infection: Molecular mechanisms and in vivo implications. Rev. Med Virol. 2003, 13, 387–398. [Google Scholar] [CrossRef] [PubMed]
- Alberts, B.; Johnson, A.; Lewis, J.; Raff, M.; Roberts, K.; Walter, P. Innate immunity. In Molecular Biology of the Cell, 4th ed.; Garland Science: New York, NY, USA, 2002; Chapter 25; p. 712. [Google Scholar]
- Henao-Restrepo, A.M.; Longini, I.M.; Egger, M.; Dean, N.E.; Edmunds, W.J.; Camacho, A.; Carroll, M.W.; Doumbia, M.; Draguez, B.; Duraffour, S. Efficacy and effectiveness of an rVSV-vectored vaccine expressing ebola surface glycoprotein: Interim results from the guinea ring vaccination cluster-randomised trial. Lancet 2015, 386, 857–866. [Google Scholar] [CrossRef]
- Sakabe, S.; Sullivan, B.M.; Hartnett, J.N.; Robles-Sikisaka, R.; Gangavarapu, K.; Cubitt, B.; Ware, B.C.; Kotliar, D.; Branco, L.M.; Goba, A. Analysis of CD8+ t cell response during the 2013–2016 Ebola epidemic in west africa. Proc. Natl. Acad. Sci. USA 2018, 115, E7578–E7586. [Google Scholar] [CrossRef] [PubMed]
- Dahlke, C.; Lunemann, S.; Kasonta, R.; Kreuels, B.; Schmiedel, S.; Ly, M.L.; Fehling, S.K.; Strecker, T.; Becker, S.; Altfeld, M. Comprehensive characterization of cellular immune responses following Ebola virus infection. J. Infect. Dis. 2016, 215, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Warfield, K.L.; Olinger, G.; Deal, E.M.; Swenson, D.L.; Bailey, M.; Negley, D.L.; Hart, M.K.; Bavari, S. Induction of humoral and CD8+ T cell responses are required for protection against lethal Ebola virus infection. J. Immunol. 2005, 175, 1184–1191. [Google Scholar] [CrossRef] [PubMed]
- Olejnik, J.; Forero, A.; Deflubé, L.R.; Hume, A.J.; Manhart, W.A.; Nishida, A.; Marzi, A.; Katze, M.G.; Ebihara, H.; Rasmussen, A.L. Ebolaviruses associated with differential pathogenicity induce distinct host responses in human macrophages. J. Virol. 2017, 91, e00179-17. [Google Scholar] [CrossRef]
- Rhein, B.A.; Maury, W.J. Ebola virus entry into host cells: Identifying therapeutic strategies. Curr. Clin. Microbiol. Rep. 2015, 2, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Baribaud, F.; Doms, R.W.; Pohlmann, S. The role of DC-sign and DC-signr in HIV and Ebola virus infection: Can potential therapeutics block virus transmission and dissemination? Expert Opin. Ther. Targets 2002, 6, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Raska, M.; Czernekova, L.; Moldoveanu, Z.; Zachova, K.; Elliott, M.C.; Novak, Z.; Hall, S.; Hoelscher, M.; Maboko, L.; Brown, R. Differential glycosylation of envelope GP120 is associated with differential recognition of HIV-1 by virus-specific antibodies and cell infection. Aids Res. Ther. 2018, 11, 23–39. [Google Scholar] [CrossRef]
- Shimojima, M.; Takada, A.; Ebihara, H.; Neumann, G.; Fujioka, K.; Irimura, T.; Jones, S.; Feldmann, H.; Kawaoka, Y. Tyro3 family-mediated cell entry of EBOLA and marburg viruses. J. Virol. 2006, 80, 10109–10116. [Google Scholar] [CrossRef] [PubMed]
- Dahlmann, F.; Biedenkopf, N.; Babler, A.; Jahnen-Dechent, W.; Karsten, C.B.; Gnirß, K.K.; Schneider, H.; Wrensch, F.; O’Callaghan, C.A.; Bertram, S. Analysis of Ebola virus entry into macrophages. J. Infect. Dis. 2015, 212, S247–S257. [Google Scholar] [CrossRef] [PubMed]
- de Witte, L.; Abt, M.; Schneider-Schaulies, S.; van Kooyk, Y.; van Kooyk, Y.; Geijtenbeek, T.B. Measles virus targets DC-sign to enhance dendritic cell infection. J. Virol. 2006, 80, 3477–3486. [Google Scholar] [CrossRef] [PubMed]
- Geijtenbeek, T.B.; van Kooyk, Y. DC-sign: A novel HIV receptor on dcs that mediates HIV-1 transmission. Curr. Top. Microbiol. Immunol. 2003, 276, 31–54. [Google Scholar] [PubMed]
- Rinaldo, C.R. Dendritic cell-based human immunodeficiency virus vaccine. J. Intern. Med. 2009, 265, 138–158. [Google Scholar] [CrossRef] [PubMed]
- Hillaire, M.L.; Nieuwkoop, N.J.; Boon, A.C.; de Mutsert, G.; Vogelzang-van Trierum, S.E.; Fouchier, R.A.; Osterhaus, A.D.; Rimmelzwaan, G.F. Binding of DC-sign to the hemagglutinin of influenza a viruses supports virus replication in DC-sign expressing cells. PLoS ONE 2013, 8, e56164–e56174. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Pineres, A.J.; Hildesheim, A.; Trivett, M.; Williams, M.; Wu, L.; Kewalramani, V.N.; Pinto, L.A.; Pinto, L.A. Role of DC-sign in the activation of dendritic cells by HPV-16 l1 virus-like particle vaccine. Eur. J. Immunol. 2006, 36, 437–445. [Google Scholar] [CrossRef]
- Fujihira, H.; Usami, K.; Matsuno, K.; Takeuchi, H.; Denda-Nagai, K.; Furukawa, J.-I.; Shinohara, Y.; Takada, A.; Kawaoka, Y.; Irimura, T. A critical domain of ebolavirus envelope glycoprotein determines glycoform and infectivity. Sci. Rep. 2018, 8, 5495–5508. [Google Scholar] [CrossRef]
- Lin, G.; Simmons, G.; Pohlmann, S.; Baribaud, F.; Ni, H.; Leslie, G.J.; Haggarty, B.S.; Bates, P.; Weissman, D.; Hoxie, J.A. Differential N-linked glycosylation of human immunodeficiency virus and Ebola virus envelope glycoproteins modulates interactions with DC-sign and DC-signr. J. Virol. 2003, 77, 1337–1346. [Google Scholar] [CrossRef]
- Varki, A.; Cummings, R.D.; Esko, J.D.; Freeze, H.H.; Stanley, P.; Bertozzi, C.R.; Hart, G.W.; Etzler, M.E. Nematoda-Essentials of Glycobiology; Cold Spring Harbor Laboratory Press: New York, NY, USA, 2009; pp. 1068–1072. [Google Scholar]
- Liu, W.; Tang, L.; Zhang, G.; Wei, H.; Cui, Y.; Guo, L.; Gou, Z.; Chen, X.; Jiang, D.; Zhu, Y. Characterization of a novel C-type lectin-like gene, lesctin: Demonstration of carbohydrate binding and expression in sinusoidal endothelial cells of liver and lymph node. J. Biol. Chem. 2004, 279, 18748–18758. [Google Scholar] [CrossRef]
- Domínguez-Soto, A.; Aragoneses-Fenoll, L.; Gómez-Aguado, F.; Corcuera, M.T.; Clária, J.; García-Monzón, C.; Bustos, M.; Corbí, A.L. The pathogen receptor liver and lymph node sinusoidal endotelial cell C-type Lectin is expressed in human kupffer cells and regulated by PU. 1. Hepatology 2009, 49, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Gramberg, T.; Soilleux, E.; Fisch, T.; Lalor, P.F.; Hofmann, H.; Wheeldon, S.; Cotterill, A.; Wegele, A.; Winkler, T.; Adams, D.H. Interactions of lsectin and DC-sign/DC-signr with viral ligands: Differential ph dependence, internalization and virion binding. Virology 2008, 373, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Sakakura, M.; Oo-Puthinan, S.; Moriyama, C.; Kimura, T.; Moriya, J.; Irimura, T.; Shimada, I. Carbohydrate binding mechanism of the macrophage galactose-type C-type LECtin 1 revealed by saturation transfer experiments. J. Biol. Chem. 2008, 283, 33665–33673. [Google Scholar] [CrossRef] [PubMed]
- Takada, A.; Fujioka, K.; Tsuiji, M.; Morikawa, A.; Higashi, N.; Ebihara, H.; Kobasa, D.; Feldmann, H.; Irimura, T.; Kawaoka, Y. Human macrophage c-type lectin specific for galactose and n-acetylgalactosamine promotes filovirus entry. J. Virol. 2004, 78, 2943–2947. [Google Scholar] [CrossRef]
- Usami, K.; Matsuno, K.; Matsuno, K.; Igarashi, M.; Irimura, T.; Irimura, T. Involvement of viral envelope GP2 in Ebola virus entry into cells expressing the macrophage galactose-type C-type lectin. Biochem. Biophys. Res. Commun. 2011, 407, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Jangid, K.; Anuradha. Ebola vaccine: How far are we? J. Clin. Diagn. Res. 2017, 11, DE01–DE04. [Google Scholar] [CrossRef] [PubMed]
- Weik, M.; Modrof, J.; Klenk, H.D.; Becker, S.; Mühlberger, E. Ebola virus VP30-mediated transcription is regulated by RNA secondary structure formation. J. Virol. 2002, 76, 8532–8539. [Google Scholar] [CrossRef]
- Warfield, K.L.; Bosio, C.M.; Welcher, B.C.; Deal, E.M.; Mohamadzadeh, M.; Schmaljohn, A.; Aman, M.J.; Bavari, S. Ebola virus-like particles protect from lethal ebola virus infection. Proc. Natl. Acad. Sci. USA 2003, 100, 15889–15894. [Google Scholar] [CrossRef]
- Schweneker, M.; Laimbacher, A.S.; Zimmer, G.; Wagner, S.; Schraner, E.M.; Wolferstotter, M.; Klingenberg, M.; Dirmeier, U.; Steigerwald, R.; Lauterbach, H.; et al. Recombinant modified vaccinia virus ankara generating ebola virus-like particles. J. Virol. 2017, 91, e00343-17. [Google Scholar] [CrossRef]
- Wang, Y.; Li, J.; Hu, Y.; Liang, Q.; Wei, M.; Zhu, F. Ebola vaccines in clinical trial: The promising candidates. Hum. Vaccines Immunother. 2017, 13, 153–168. [Google Scholar] [CrossRef]
- Chahal, J.S.; Khan, O.F.; Cooper, C.L.; McPartlan, J.S.; Tsosie, J.K.; Tilley, L.D.; Sidik, S.M.; Lourido, S.; Langer, R.; Bavari, S. Dendrimer-RNA nanoparticles generate protective immunity against lethal Ebola, H1N1 influenza, and toxoplasma gondii challenges with a single dose. Proc. Natl. Acad. Sci. USA 2016, 113, E4133–E4142. [Google Scholar] [CrossRef] [PubMed]
- Chepurnov, A.A.; Ternovoi, V.A.; Dadaeva, A.A.; Dmitriev, I.P.; Sizikova, L.P.; Volchkov, V.E.; Kudoiarova, N.M.; Rudzevich, T.N.; Netesov, S.V. Immunobiological properties of vp24 protein of ebola virus expressed by recombinant vaccinia virus. Vopr Virusol 1997, 42, 115–120. [Google Scholar] [PubMed]
- Suder, E.; Furuyama, W.; Feldmann, H.; Marzi, A.A.-O.; de Wit, E. The vesicular stomatitis virus-based ebola virus vaccine: From concept to clinical trials. Hum. Vaccines Immunother. 2018, 14, 2107–2113. [Google Scholar] [CrossRef] [PubMed]
- Ewer, K.; Rampling, T.; Venkatraman, N.; Bowyer, G.; Wright, D.; Lambe, T.; Imoukhuede, E.B.; Payne, R.; Fehling, S.K.; Strecker, T. A monovalent chimpanzee adenovirus Ebola vaccine boosted with mva. N. Engl. J. Med. 2016, 374, 1635–1646. [Google Scholar] [CrossRef] [PubMed]
- Tapia, M.D.; Sow, S.O.; Lyke, K.E.; Haidara, F.C.; Diallo, F.; Doumbia, M.; Traore, A.; Coulibaly, F.; Kodio, M.; Onwuchekwa, U. Use of ChAd3-EBO-Z ebola virus vaccine in malian and US adults, and boosting of Malian adults with MVA-BN-Filo: A phase 1, single-blind, randomised trial, a phase 1b, open-label and double-blind, dose-escalation trial, and a nested, randomised, double-blind, placebo-controlled trial. Lancet Infect. Dis. 2016, 16, 31–42. [Google Scholar] [PubMed]
- Zhu, F.-C.; Hou, L.-H.; Li, J.-X.; Wu, S.-P.; Liu, P.; Zhang, G.-R.; Hu, Y.-M.; Meng, F.-Y.; Xu, J.-J.; Tang, R. Safety and immunogenicity of a novel recombinant adenovirus type-5 vector-based ebola vaccine in healthy adults in china: Preliminary report of a randomised, double-blind, placebo-controlled, phase 1 trial. Lancet 2015, 385, 2272–2279. [Google Scholar] [CrossRef]
- Awate, S.; Babiuk, L.A.B.; Mutwiri, G. Mechanisms of action of adjuvants. Front. Immunol. 2013, 4, 1–10. [Google Scholar] [CrossRef] [PubMed]


| S/N | Viral Infection | Vaccine Development Strategy | Route of Administration | Vaccine Status | References |
|---|---|---|---|---|---|
| 1 | Yellow fever | Attenuated virus | Subcutaneous | Available in circulation | [5] |
| 2 | Influenza | Live attenuated virus, inactivated virus, recombinant influenza vaccine, VLP | Intramuscular, intranasal, intradermal, subcutaneous | Available in circulation VLP and DNA vaccine not in circulation (needs development of a novel universal vaccine) | [6,7,8] |
| 3. | Poliovirus | Live attenuated vaccine | Oral | Available in circulation | [9] |
| 4. | Measles, mumps and rubella | Live attenuated vaccine | Subcutaneous | Available in circulation | [10] |
| 5 | Human papilloma virus | VLP, inactivated vaccine | Intramuscular, oral | Monovalent, bivalent, tetravalent, nonavalent vaccines available in circulation | [11,12] |
| 6 | Hepatitis B virus | Live inactivated, recombinant DNA | Intramuscular | Available in circulation (it gives short-term protection; issue raised concerning its safety) | [13,14,15] |
| 7 | Varicella | Weakened live virus or attenuated virus | Subcutaneous, intramuscular | Available in circulation | [16] |
| 8 | Rotavirus | Live attenuated, VLP | Oral, intranasal | Available in circulation; VLP not in circulation | [17,18] |
| 9 | HIV | VLP, DNA vaccine | Subcutaneous, intramuscular | Not in circulation (development in progress) | [19,20] |
| 10 | EBOV | Live attenuated, VLP | Intramuscular | Available but not yet in circulation (phase trial in progress) | [21,22] |
| 11 | Lassa virus | VLP, live attenuated virus, DNA vaccine | Intradermal | No available vaccine | [23,24,25] |
| S/N. | Vaccine | Immune Responses Induced | Vaccine Development Strategy | Route of Administration | DC-Targeting Substance | Protection Percentage | Ref |
|---|---|---|---|---|---|---|---|
| 1 | Cancer vaccine | Cellular immune response and humoral responses | DNA vaccine | Not applicable | IFN-α | Not applicable | [38,39] |
| DNA vaccine | Subcutaneous | Liposome and melanoma | 80–100% | [39] | |||
| 2 | Yellow fever | Innate immune responses (proinflammatory cytokines interleukin (IL)-12p40, IL-6, and interferon-α), adaptive immune responses (T helper cell (Th)1/Th2 cytokine profile and antigen-specific CD8+ T cell) | Live attenuated vaccine | Subcutaneous | Not applicable | [30] | |
| 3 | Adenovirus | Cytolytic T lymphocyte cells | Recombinant vaccine | Not applicable | Recombinant single-chain (sc) mAb Fv fragments | Not applicable | [29] |
| 4 | HIV | IFN-γ, CD4+, and CD8+ T cell | Recombinant vaccinia virus (DNA vaccine) | Intranasal | Recombinant single-chain (sc) mAb Fv fragments (scFv) HIV gagp41-scFv | 100% | [40] |
| 5 | Influenza A | Cytotoxic CD8+T, cell CD4+ Th1, IgG2a antibodies | DNA vaccines | Intradermal | Xcl1-hemagglutinin (HA) | 100% | [41] |
| DNA vaccine | Intravenous tail injection and electroporation | Xcl1-HA or Xcl2-HA | 90% | [42] | |||
| 6 | West Nile Virus vaccine | Humoral and T-cell responses | DNA vaccine (immunodominant vaccinia B8R gene) | Intravenous injection | Rabies glycoprotein (GP) fused to protamine residue (RVG-P) | 80% | [43] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olukitibi, T.A.; Ao, Z.; Mahmoudi, M.; Kobinger, G.A.; Yao, X. Dendritic Cells/Macrophages-Targeting Feature of Ebola Glycoprotein and its Potential as Immunological Facilitator for Antiviral Vaccine Approach. Microorganisms 2019, 7, 402. https://doi.org/10.3390/microorganisms7100402
Olukitibi TA, Ao Z, Mahmoudi M, Kobinger GA, Yao X. Dendritic Cells/Macrophages-Targeting Feature of Ebola Glycoprotein and its Potential as Immunological Facilitator for Antiviral Vaccine Approach. Microorganisms. 2019; 7(10):402. https://doi.org/10.3390/microorganisms7100402
Chicago/Turabian StyleOlukitibi, Titus Abiola, Zhujun Ao, Mona Mahmoudi, Gary A. Kobinger, and Xiaojian Yao. 2019. "Dendritic Cells/Macrophages-Targeting Feature of Ebola Glycoprotein and its Potential as Immunological Facilitator for Antiviral Vaccine Approach" Microorganisms 7, no. 10: 402. https://doi.org/10.3390/microorganisms7100402