Administration Routes and Doses of the Attenuated African Swine Fever Virus Strain PSA-1NH Influence Cross-Protection of Pigs against Heterologous Challenge
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Viruses
2.2. Animal Experiments and Ethics Statement
2.3. Experimental Designs
2.4. Clinical Evaluation
2.5. Sample Collection
2.6. Determination of the Infectious Activities of ASFV
2.7. Detection of Anti-ASFV Antibodies
2.8. Real-Time Polymerase Chain Reaction (Real-Time PCR)
2.9. Statistical Analysis
3. Results
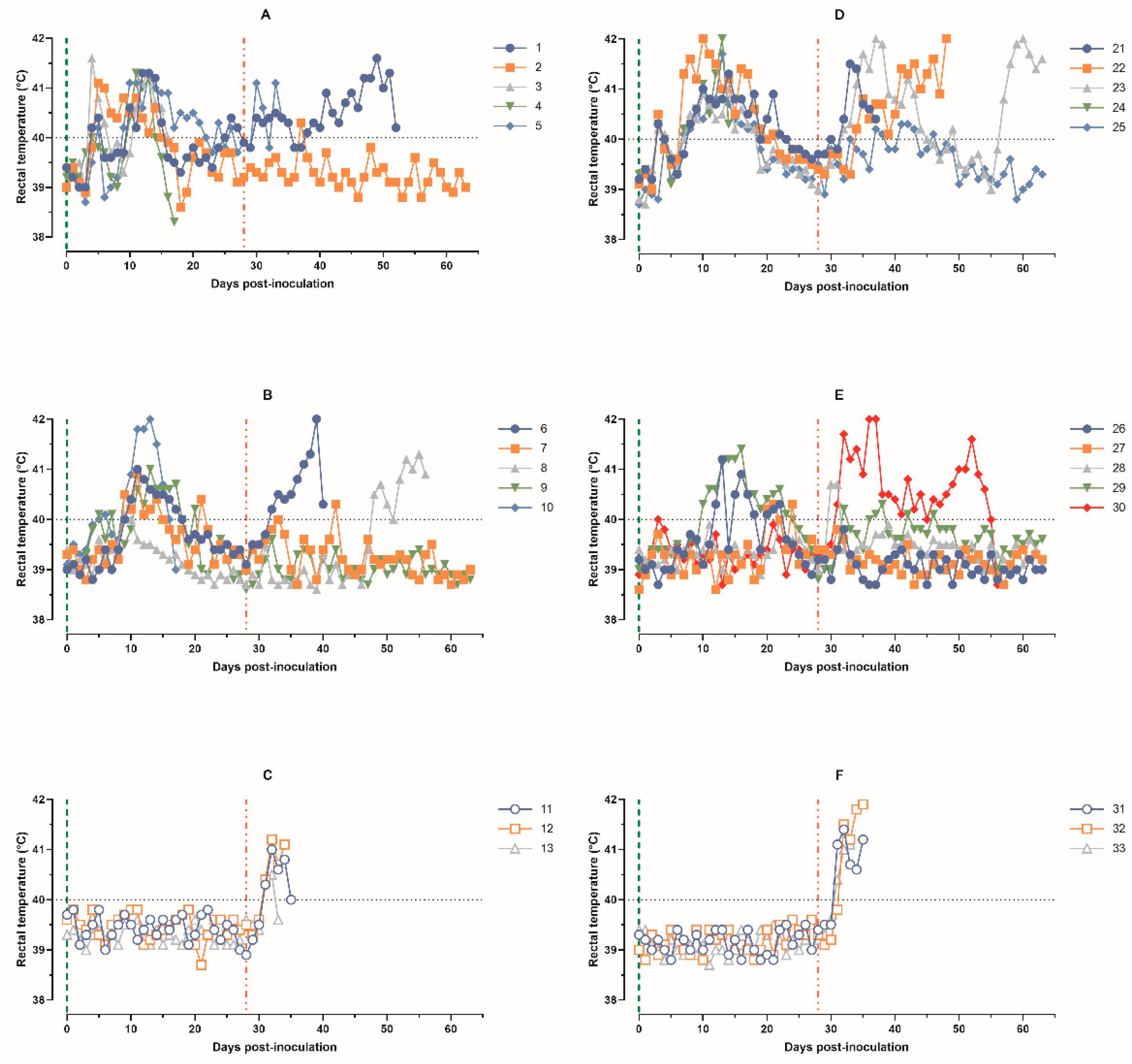
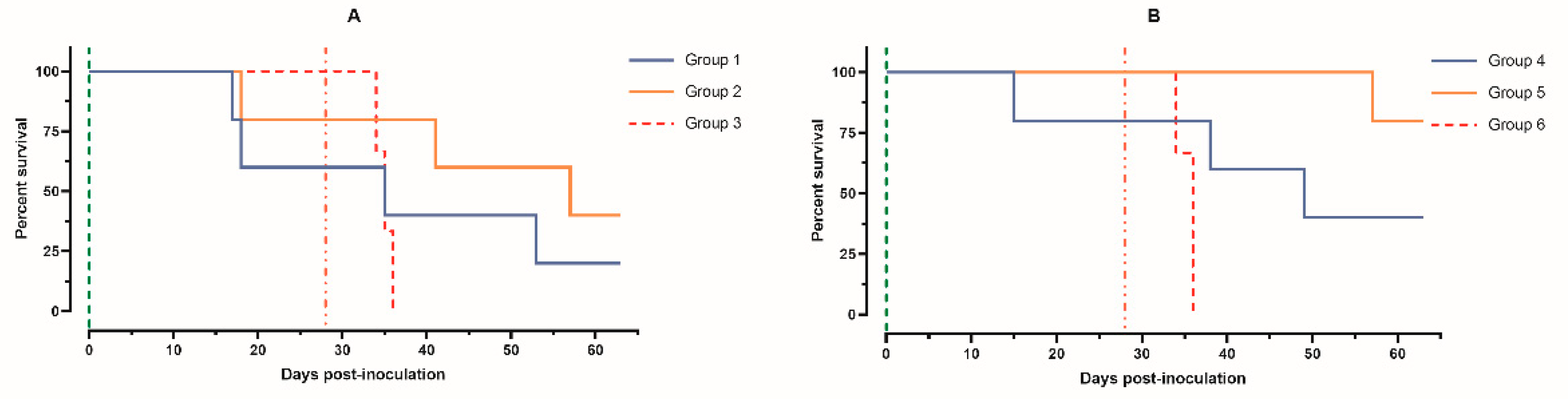
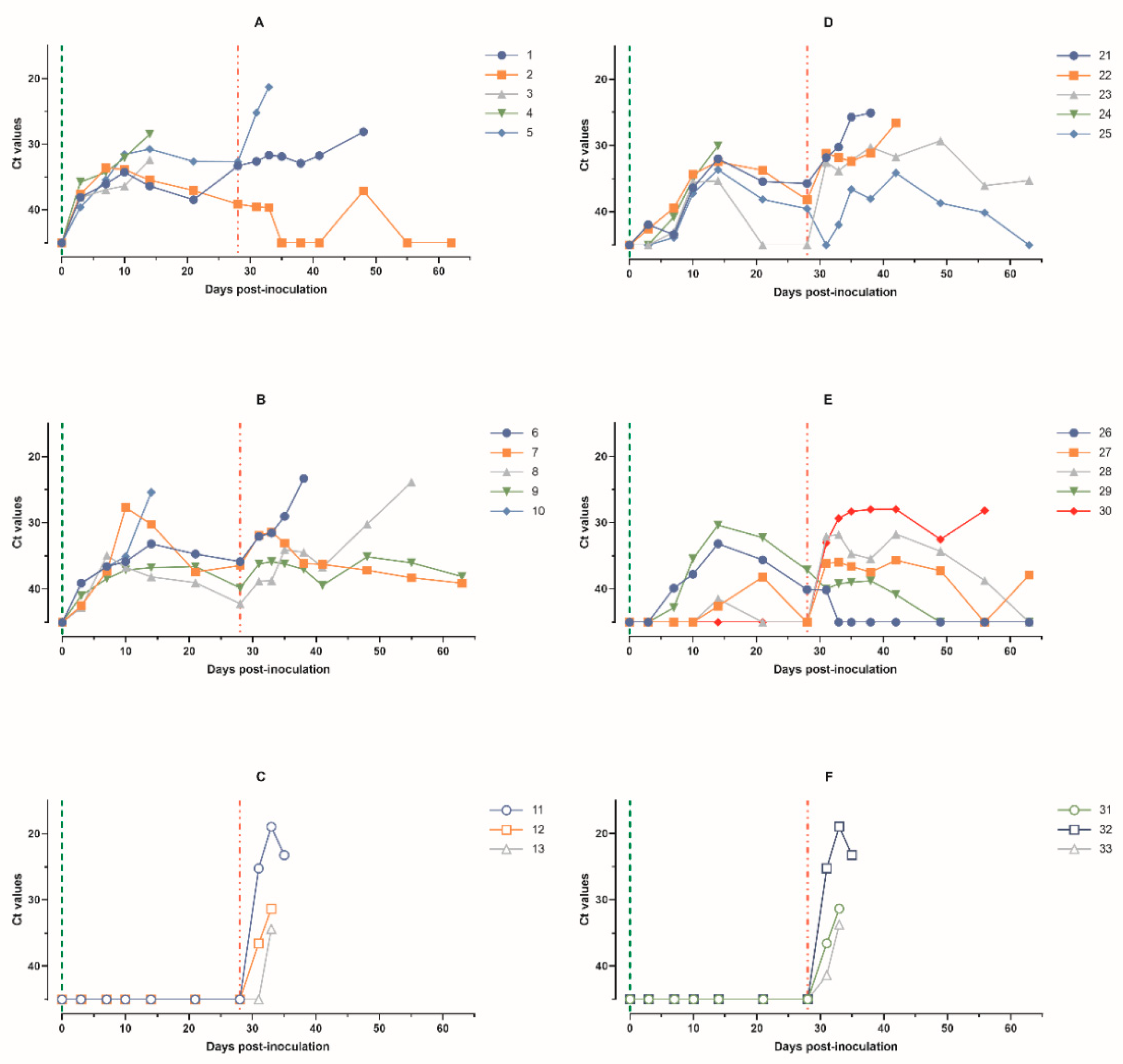
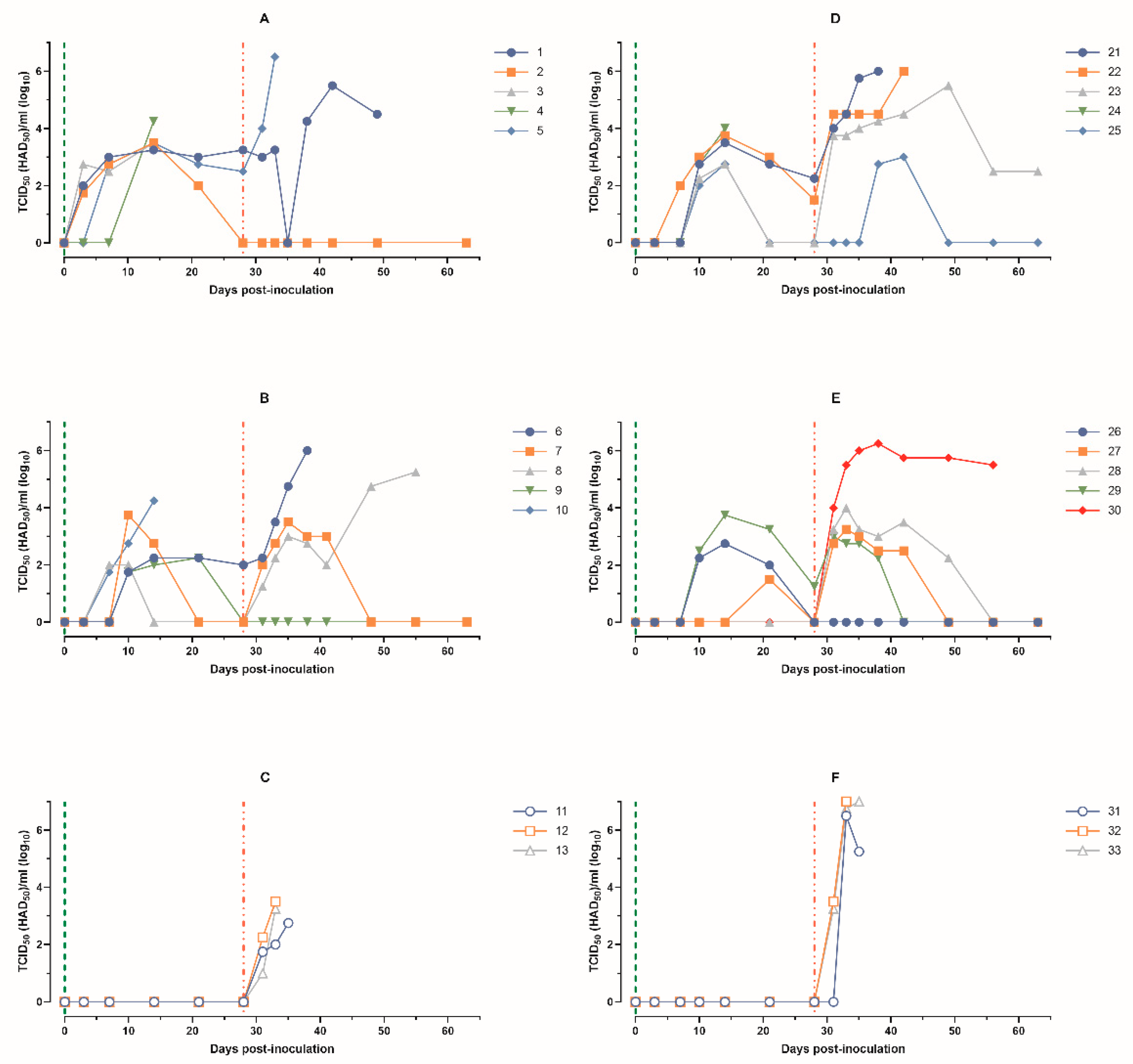
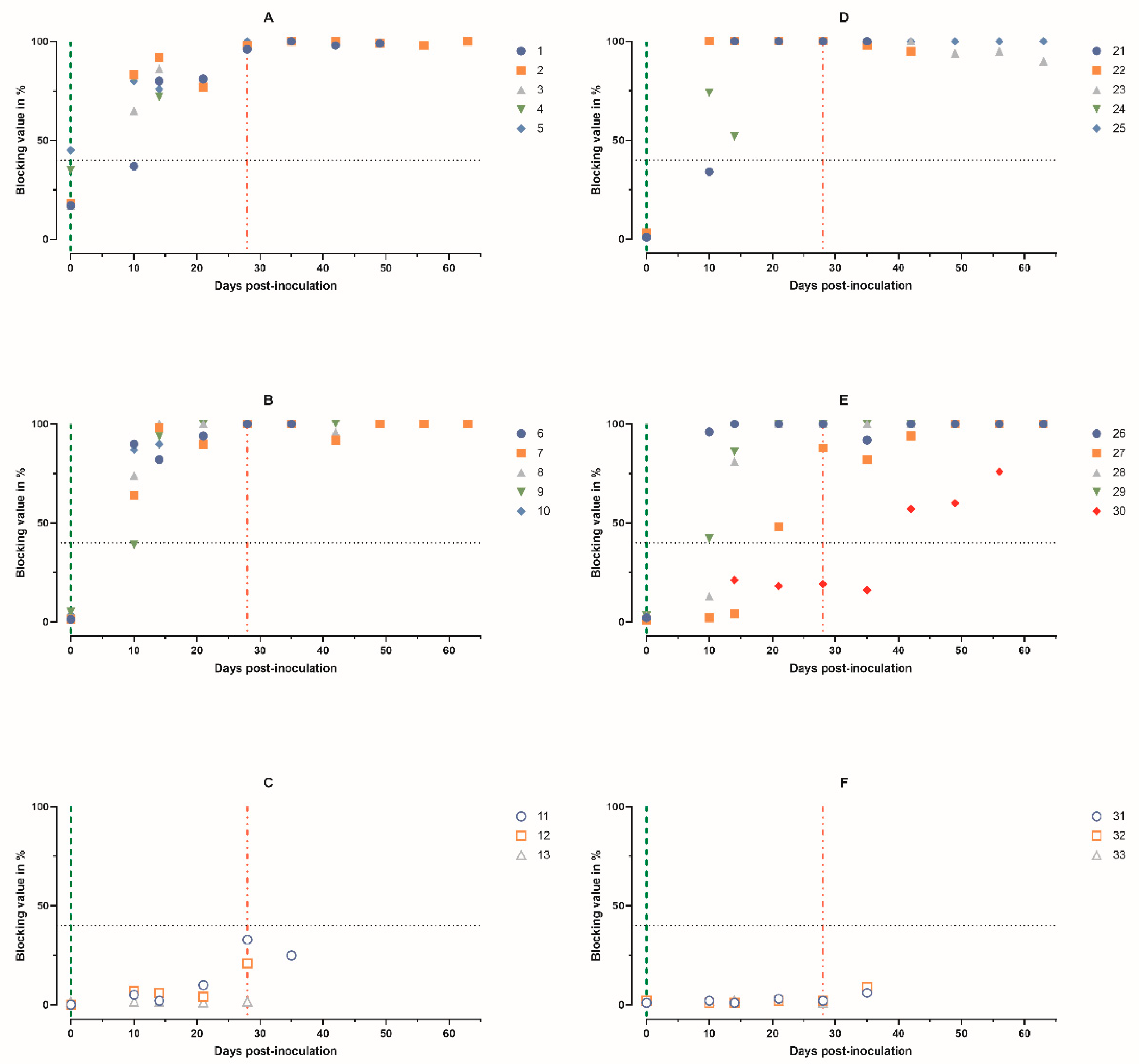
3.1. Immunobiological Indicators in Pigs after Intramuscular Inoculation of Different Doses of ASFV-PSA-1NH and Challenge with ASFV-Stavropol 01/08
3.2. Immunobiological Indicators in Pigs after Intranasal Administration of Different Doses of ASFV-PSA-1NH and Intramuscular Challenge with ASFV-Stavropol 01/08
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carrascosa, J.L.; Carazo, J.M.; Carrascosa, A.L.; García, N.; Santisteban, A.; Viñuela, E. General Morphology and Capsid Fine Structure of African Swine Fever Virus Particles. Virology 1984, 132, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Chapman, D.A.G.; Darby, A.C.; Da Silva, M.; Upton, C.; Radford, A.D.; Dixon, L.K. Genomic Analysis of Highly Virulent Georgia 2007/1 Isolate of African Swine Fever Virus. Emerg. Infect. Dis. 2011, 17, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Chapman, D.A.G.; Tcherepanov, V.; Upton, C.; Dixon, L.K. Comparison of the Genome Sequences of Non-Pathogenic and Pathogenic African Swine Fever Virus Isolates. J. Gen. Virol. 2008, 89, 397–408. [Google Scholar] [CrossRef] [PubMed]
- Bishop, R.P.; Fleischauer, C.; de Villiers, E.P.; Okoth, E.A.; Arias, M.; Gallardo, C.; Upton, C. Comparative Analysis of the Complete Genome Sequences of Kenyan African Swine Fever Virus Isolates within P72 Genotypes IX and X. Virus Genes 2015, 50, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Dixon, L.K.; Sun, H.; Roberts, H. African Swine Fever. Antivir. Res. 2019, 165, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Ogata, H.; Toyoda, K.; Tomaru, Y.; Nakayama, N.; Shirai, Y.; Claverie, J.-M.; Nagasaki, K. Remarkable Sequence Similarity between the Dinoflagellate-Infecting Marine Girus and the Terrestrial Pathogen African Swine Fever Virus. Virol. J. 2009, 6, 178. [Google Scholar] [CrossRef]
- Malogolovkin, A.; Burmakina, G.; Titov, I.; Sereda, A.; Gogin, A.; Baryshnikova, E.; Kolbasov, D. Comparative Analysis of African Swine Fever Virus Genotypes and Serogroups. Emerg. Infect. Dis. 2015, 21, 312–315. [Google Scholar] [CrossRef]
- Dixon, L.K.; Chapman, D.A.G.; Netherton, C.L.; Upton, C. African Swine Fever Virus Replication and Genomics. Virus Res. 2013, 173, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, J.E.; Gallardo, C.; Nieto-Pelegrín, E.; Rivera-Arroyo, B.; Degefa-Negi, T.; Arias, M.; Jenberie, S.; Mulisa, D.D.; Gizaw, D.; Gelaye, E.; et al. Identification of a New Genotype of African Swine Fever Virus in Domestic Pigs from Ethiopia. Transbound. Emerg. Dis. 2017, 64, 1393–1404. [Google Scholar] [CrossRef]
- Bastos, A.D.S.; Penrith, M.-L.; Crucière, C.; Edrich, J.L.; Hutchings, G.; Roger, F.; Couacy-Hymann, E.; Thomson, R.G. Genotyping Field Strains of African Swine Fever Virus by Partial P72 Gene Characterisation. Arch. Virol. 2003, 148, 693–706. [Google Scholar] [CrossRef]
- Quembo, C.J.; Jori, F.; Vosloo, W.; Heath, L. Genetic Characterization of African Swine Fever Virus Isolates from Soft Ticks at the Wildlife/Domestic Interface in Mozambique and Identification of a Novel Genotype. Transbound. Emerg. Dis. 2018, 65, 420–431. [Google Scholar] [CrossRef]
- King, K.; Chapman, D.; Argilaguet, J.M.; Fishbourne, E.; Hutet, E.; Cariolet, R.; Hutchings, G.; Oura, C.A.L.; Netherton, C.L.; Moffat, K.; et al. Protection of European Domestic Pigs from Virulent African Isolates of African Swine Fever Virus by Experimental Immunisation. Vaccine 2011, 29, 4593–4600. [Google Scholar] [CrossRef] [PubMed]
- Rock, D.L. Challenges for African Swine Fever Vaccine Development—“…Perhaps the End of the Beginning.”. Vet. Microbiol. 2017, 206, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Malmquist, W.A. Serologic and Immunologic Studies with African Swine Fever Virus. Am. J. Vet. Res. 1963, 24, 450–459. [Google Scholar] [PubMed]
- Sereda, A.D.; Balyshev, V.M. Antigenic diversity of African swine fever viruses. Vopr. Virusol. 2011, 56, 38–42. [Google Scholar] [PubMed]
- Sereda, A.D.; Namsrayn, S.; Balyshev, V.M.; Vlasov, M.E.; Sindryakova, I.P.; Koltsova, G.; Kolbasov, D.V. Seroimmunotyping of African Swine Fever Virus. Front. Microbiol. 2023, 14, 1225587. [Google Scholar] [CrossRef] [PubMed]
- Malogolovkin, A.; Burmakina, G.; Tulman, E.R.; Delhon, G.; Diel, D.G.; Salnikov, N.; Kutish, G.F.; Kolbasov, D.; Rock, D.L. African Swine Fever Virus CD2v and C-Type Lectin Gene Loci Mediate Serological Specificity. J. Gen. Virol. 2015, 96, 866–873. [Google Scholar] [CrossRef]
- Simulundu, E.; Chambaro, H.M.; Sinkala, Y.; Kajihara, M.; Ogawa, H.; Mori, A.; Ndebe, J.; Dautu, G.; Mataa, L.; Lubaba, C.H.; et al. Co-Circulation of Multiple Genotypes of African Swine Fever Viruses among Domestic Pigs in Zambia (2013–2015). Transbound. Emerg. Dis. 2018, 65, 114–122. [Google Scholar] [CrossRef]
- Mulumba-Mfumu, L.K.; Achenbach, J.E.; Mauldin, M.R.; Dixon, L.K.; Tshilenge, C.G.; Thiry, E.; Moreno, N.; Blanco, E.; Saegerman, C.; Lamien, C.E.; et al. Genetic Assessment of African Swine Fever Isolates Involved in Outbreaks in the Democratic Republic of Congo between 2005 and 2012 Reveals Co-Circulation of P72 Genotypes I, IX and XIV, Including 19 Variants. Viruses 2017, 9, 31. [Google Scholar] [CrossRef]
- Sereda, A.D.; Balyshev, V.M.; Kazakova, A.S.; Imatdinov, A.R.; Kolbasov, D.V. Protective Properties of Attenuated Strains of African Swine Fever Virus Belonging to Seroimmunotypes I–VIII. Pathogens 2020, 9, 274. [Google Scholar] [CrossRef]
- Bech-Nielsen, S.; Fernandez, J.; Martinez-Pereda, F.; Espinosa, J.; Perez Bonilla, Q.; Sanchez-Vizcaino, J.M. A Case Study of an Outbreak of African Swine Fever in Spain. Br. Vet. J. 1995, 151, 203–214. [Google Scholar] [CrossRef] [PubMed]
- Gonzalvo, F.R.; Carnero, M.E.; Bruyel, V. Immunological Responses of Pigs to Partially Attenuated ASF Virus and Their Resistance to Virulent Homologous and Heterologous Viruses; FAO: Rome, Italy, 1983. [Google Scholar]
- Monteagudo, P.L.; Lacasta, A.; López, E.; Bosch, L.; Collado, J.; Pina-pedrero, S.; Correa-fiz, F.; Accensi, F.; Navas, M.J.; Vidal, E.; et al. BA71ΔCD2: A New Recombinant Live Attenuated African Swine Fever Virus with Cross-Protective Capabilities. J. Virol. 2017, 91, e01058-17. [Google Scholar] [CrossRef] [PubMed]
- Gallardo, C.; Sánchez, E.G.; Pérez-Núñez, D.; Nogal, M.; de León, P.; Carrascosa, Á.L.; Nieto, R.; Soler, A.; Arias, M.L.; Revilla, Y. African Swine Fever Virus (ASFV) Protection Mediated by NH/P68 and NH/P68 Recombinant Live-Attenuated Viruses. Vaccine 2018, 36, 2694–2704. [Google Scholar] [CrossRef] [PubMed]
- Arias, M.; de la Torre, A.; Dixon, L.; Gallardo, C.; Jori, F.; Laddomada, A.; Martins, C.; Parkhouse, R.M.; Revilla, Y.; Rodriguez, F.A.J.-M.; et al. Approaches and Perspectives for Development of African Swine Fever Virus Vaccines. Vaccines 2017, 5, 35. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Cordón, P.J.; Chapman, D.; Jabbar, T.; Reis, A.L.; Goatley, L.; Netherton, C.L.; Taylor, G.; Montoya, M.; Dixon, L. Different Routes and Doses Influence Protection in Pigs Immunised with the Naturally Attenuated African Swine Fever Virus Isolate OURT88/3. Antivir. Res. 2017, 138, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Leitão, A.; Cartaxeiro, C.; Coelho, R.; Cruz, B.; Parkhouse, R.M.E.; Portugal, F.C.; Vigário, J.D.; Martins, C.L.V. The Non-Haemadsorbing African Swine Fever Virus Isolate ASFV/NH/P68 Provides a Model for Defining the Protective Anti-Virus Immune Response. J. Gen. Virol. 2001, 82, 513–523. [Google Scholar] [CrossRef]
- Vigário, J.D.; Terrinha, A.M.; Bastos, A.L.; Moura-Nunes, J.F.; Marques, D.; Silva, J.F. Serological Behaviour of Isolated African Swine Fever Virus. Brief Report. Arch. Gesamte Virusforsch. 1970, 31, 387–389. [Google Scholar] [CrossRef] [PubMed]
- Balyshev, V.M.; Kalantaenko, Y.F.; Bolgova, M.V.; Prodnikova, E.Y. Seroimmunological Affiliation of African Swine Fever Virus Isolated in the Russian Federation. Russ. Agric. Sci. 2011, 37, 427–429. [Google Scholar] [CrossRef]
- National Research Council. Guide for the Care and Use of Laboratory Animals; National Academies Press: Washington, DC, USA, 2011; ISBN 978-0-309-15400-0. Available online: https://nap.nationalacademies.org/catalog/12910/guide-for-the-care-and-use-of-laboratory-animals-eighth (accessed on 21 April 2024).
- Fernández-Pinero, J.; Gallardo, C.; Elizalde, M.; Robles, A.; Gómez, C.; Bishop, R.; Heath, L.; Couacy-Hymann, E.; Fasina, F.O.; Pelayo, V.; et al. Molecular Diagnosis of African Swine Fever by a New Real-Time PCR Using Universal Probe Library. Transbound. Emerg. Dis. 2013, 60, 48–58. [Google Scholar] [CrossRef]
- Ashmarin, I.; Vasil’yev, I.; Ambrosov, V. Rapid Methods of Statistical Processing and Planning Experiments, 2nd ed.; Leningrad University Publishing House: Leningrad, Russia, 1975. [Google Scholar]
- Sun, E.; Huang, L.; Zhang, X.; Zhang, J.; Shen, D.; Zhang, Z.; Wang, Z.; Huo, H.; Wang, W.; Huangfu, H.; et al. Genotype I African Swine Fever Viruses Emerged in Domestic Pigs in China and Caused Chronic Infection. Emerg. Microbes Infect. 2021, 10, 2183–2193. [Google Scholar] [CrossRef]
- de Carvalho Ferreira, H.C.; Weesendorp, E.; Elbers, A.R.W.; Bouma, A.; Quak, S.; Stegeman, J.A.; Loeffen, W.L.A. African Swine Fever Virus Excretion Patterns in Persistently Infected Animals: A Quantitative Approach. Vet. Microbiol. 2012, 160, 327–340. [Google Scholar] [CrossRef] [PubMed]
- Vlasov, M.E.; Sindryakova, I.P.; Kudrjashov, D.A.; Morgunov, S.Y.; Kolbasova, O.L.; Lyska, V.M.; Zhivoderov, S.P.; Pivova, E.Y.; Balyshev, V.M.; Sereda, A.D.; et al. Inoculation with ASFV-Katanga-350 Partially Protects Pigs from Death during Subsequent Infection with Heterologous Type ASFV-Stavropol 01/08. Viruses 2023, 15, 430. [Google Scholar] [CrossRef] [PubMed]
- Dórea, F.C.; Swanenburg, M.; Horigan, H.; de Vos, C.; Gale, P.; Lilja, T.; Comin, A.; Bahuon, C.; Zientara, S.; Young, B.; et al. Data Collection for Risk Assessments on Animal Health (Acronym: DACRAH): Final Report—Dórea—2017—EFSA Supporting Publications—Wiley Online Library. Available online: https://efsa.onlinelibrary.wiley.com/doi/10.2903/sp.efsa.2017.EN-1171 (accessed on 5 March 2024).
- Sánchez-Cordón, P.J.; Floyd, T.; Hicks, D.; Crooke, H.R.; McCleary, S.; McCarthy, R.R.; Strong, R.; Dixon, L.K.; Neimanis, A.; Wikström-Lassa, E.; et al. Evaluation of Lesions and Viral Antigen Distribution in Domestic Pigs Inoculated Intranasally with African Swine Fever Virus Ken05/Tk1 (Genotype X). Pathogens 2021, 10, 768. [Google Scholar] [CrossRef] [PubMed]
- Howey, E.B.; O’Donnell, V.; de Carvalho Ferreira, H.C.; Borca, M.V.; Arzt, J. Pathogenesis of Highly Virulent African Swine Fever Virus in Domestic Pigs Exposed via Intraoropharyngeal, Intranasopharyngeal, and Intramuscular Inoculation, and by Direct Contact with Infected Pigs. Virus Res. 2013, 178, 328–339. [Google Scholar] [CrossRef] [PubMed]
- Borca, M.V.; Carrillo, C.; Zsak, L.; Laegreid, W.W.; Kutish, G.F.; Neilan, J.G.; Burrage, T.G.; Rock, D.L. Deletion of a CD2-like Gene, 8-DR, from African Swine Fever Virus Affects Viral Infection in Domestic Swine. J. Virol. 1998, 72, 2881–2889. [Google Scholar] [CrossRef] [PubMed]
- Genovesi, E.V.; Knudsen, R.C.; Whyard, T.C.; Mebus, C.A. Moderately Virulent African Swine Fever Virus Infection: Blood Cell Changes and Infective Virus Distribution among Blood Components. Am. J. Vet. Res. 1988, 49, 338–344. [Google Scholar] [PubMed]
- Wardley, R.C.; Wilkinson, P.J. The Association of African Swine Fever Virus with Blood Components of Infected Pigs. Arch. Virol. 1977, 55, 327–334. [Google Scholar] [CrossRef]
- Gallardo, C.; Soler, A.; Nieto, R.; Sánchez, M.A.; Martins, C.; Pelayo, V.; Carrascosa, A.; Revilla, Y.; Simón, A.; Briones, V.; et al. Experimental Transmission of African Swine Fever (ASF) Low Virulent Isolate NH/P68 by Surviving Pigs. Transbound. Emerg. Dis. 2015, 62, 612–622. [Google Scholar] [CrossRef] [PubMed]
- Oura, C.A.L.; Denyer, M.S.; Takamatsu, H.; Parkhouse, R.M.E. In Vivo Depletion of CD8+ T Lymphocytes Abrogates Protective Immunity to African Swine Fever Virus. J. Gen. Virol. 2005, 86, 2445–2450. [Google Scholar] [CrossRef]
- Martins, C.L.; Lawman, M.J.; Scholl, T.; Mebus, C.A.; Lunney, J.K. African Swine Fever Virus Specific Porcine Cytotoxic T Cell Activity. Arch. Virol. 1993, 129, 211–225. [Google Scholar] [CrossRef]
- Sereda, A.D.; Kazakova, A.S.; Imatdinov, A.R.; Kolbasov, D.V. Humoral and Cell Immune Mechanisms under African Swine Fever (Review). Agric. Biol. 2015, 50, 709–718. [Google Scholar] [CrossRef]
- Wardley, R.C.; Norley, S.G.; Wilkinson, P.J.; Williams, S. The Role of Antibody in Protection against African Swine Fever Virus. Vet. Immunol. Immunopathol. 1985, 9, 201–212. [Google Scholar] [CrossRef]
- Sereda, A.; Kazakova, A.; Imatdinov, I.; Kolbasov, D. Serotype-Specific and Haemadsorption Protein of the African Swine Fever Virus. Slov. Vet. Res. 2018, 55, 141–150. [Google Scholar] [CrossRef]
- Rathakrishnan, A.; Reis, A.L.; Petrovan, V.; Goatley, L.C.; Moffat, K.; Lui, Y.; Vuong, M.T.; Ikemizu, S.; Davis, S.J.; Dixon, L.K. A Protective Multiple Gene-Deleted African Swine Fever Virus Genotype II, Georgia 2007/1, Expressing a Modified Non-Haemadsorbing CD2v Protein. Emerg. Microbes Infect. 2023, 12, 2265661. [Google Scholar] [CrossRef] [PubMed]
- Sereda, A.; Imatdinov, A.; Makarov, V.V. The Haemadsorption at African Swine Fever (Review). Selskokhozyaistvennaya Biol. 2016, 51, 763–774. [Google Scholar] [CrossRef]
- Liu, H.; Wang, A.; Yang, W.; Liang, C.; Zhou, J.; Chen, Y.; Liu, Y.; Zhou, Y.; Zhang, G. Expression of Extracellular Domain of ASFV CD2v Protein in Mammalian Cells and Identification of B Cell Epitopes. Virus Res. 2023, 323, 199000. [Google Scholar] [CrossRef]
- Sanchez-Vizcaino, J.M.; Arias, M. African Swine Fever Virus. In Diseases of Swine; John Wiley & Sons: Hoboken, NJ, USA, 2012; Volume 10, pp. 396–404. ISBN 978-1-118-34714-0. [Google Scholar]
- Havas, K.A.; Gogin, A.E.; Basalaeva, J.V.; Sindryakova, I.P.; Kolbasova, O.L.; Titov, I.A.; Lyska, V.M.; Morgunov, S.Y.; Vlasov, M.E.; Sevskikh, T.A.; et al. An Assessment of Diagnostic Assays and Sample Types in the Detection of an Attenuated Genotype 5 African Swine Fever Virus in European Pigs over a 3-Month Period. Pathogens 2022, 11, 404. [Google Scholar] [CrossRef]

| Organs | Number of Pigs | |||||||
|---|---|---|---|---|---|---|---|---|
| 6 | 7 | 8 | 9 | |||||
| Ct | Titers | Ct | Titers | Ct | Titers | Ct | Titers | |
| Spleen | 29.02 | 5.25 | N/A * | 0.00 | 18.84 | 6.50 | 38.70 | 0.00 |
| Lungs | 20.77 | 4.50 | N/A | 0.00 | 18.38 | 4.75 | 32.47 | 0.00 |
| Tonsils | 26.20 | 3.25 | N/A | 0.00 | 22.60 | 2.50 | N/A | 0.00 |
| Salivary glands | 28.23 | 3.25 | 41.64 | 0.00 | 20.01 | 6.00 | 40.22 | 0.00 |
| L/n ** mesenteric | 22.60 | 4.25 | N/A | 0.00 | 24.11 | 2.75 | N/A | 0.00 |
| L/n portal | 23.05 | 4.75 | N/A | 0.00 | 22.10 | 3.50 | N/A | 0.00 |
| L/n parotid | 27.45 | 4.75 | 44.42 | 0.00 | 27.45 | 4.25 | 36.79 | 0.00 |
| L/n submandibular | 23.14 | 4.00 | N/A | 0.00 | 41.47 | 2.50 | N/A | 0.00 |
| Organs | Number of Pigs | |||||||
|---|---|---|---|---|---|---|---|---|
| 26 | 27 | 28 | 29 | |||||
| Ct | Titers | Ct | Titers | Ct | Titers | Ct | Titers | |
| Spleen | N/A * | 0 | 36.29 | 0 | 36.52 | 0 | N/A | 0 |
| Lungs | N/A | 0 | 36.13 | 0 | 40.43 | 0 | N/A | 0 |
| Tonsils | 41,27 | 0 | 35.95 | 1.75 | 34.30 | 1.75 | 38.04 | 0 |
| Salivary glands | 43.88 | 0 | 39.03 | 0 | 36.01 | 1.75 | 38.56 | 0 |
| L/n ** mesenteric | N/A | 0 | 39.96 | 0 | 42.91 | 0 | N/A | 0 |
| L/n portal | 40.20 | 0 | 36.54 | 0 | 39.45 | 0 | 42.58 | 0 |
| L/n parotid | 39.54 | 0 | 43.59 | 0 | 44.22 | 0 | 39.30 | 0 |
| L/n submandibular | 38.92 | 0 | 40.35 | 0 | 37.44 | 0 | 42.11 | 0 |
| Indicators | Intranasal, TCID50 | Intramuscular, TCID50 | ||
|---|---|---|---|---|
| 105 Group 4 | 103 Group 5 | 105 Group 1 | 103 Group 2 | |
| Rectal temperature | ||||
| Baseline temperature, °C | 39.0 ± 0.3 | 39.0 ± 0.3 | 39.1 ± 0.2 | 39.2 ± 0.2 |
| Fever (≥40 °C)/total pigs | 5/5 | 4/4 | 5/5 | 5/5 |
| Period, dpi | 3–23 | 10–24 | 4–27 | 5–21 |
| Duration, days | 10–18 | 1–15 | 6–18 | 2–11 |
| Mean values, °C (0–28 dpi) | 40.1 ± 0.8 | 39.5 ± 0.6 | 39.9 ± 0.7 | 39.6 ± 0.7 |
| Maximum values, °C (0–28 dpi) | 40.9–42.0 | 40.0–41.4 | 41.1–41.6 | 40.0–41.8 |
| Survival rate after administration of ASFV-PSA-1NH | ||||
| Survived/total pigs | 4/5 | 4/4 | 3/5 | 4/5 |
| Clinical signs (scores) | ||||
| Manifestation (≥6 scores)/total | 5/5 | 2/4 | 5/5 | 4/5 |
| Period, dpi | 7–25 | 13–17 | 6–24 | 10–21 |
| Duration, days | 6–18 | 0–5 | 6–17 | 0–10 |
| Scores, M ± m | 6.3 ± 6.1 | 1.6 ± 1.4 | 6.4 ± 5.3 | 3.6 ± 4.5 |
| Maximum scores | 10–21 | 3–6 | 13–15 | 3–11 |
| Real-Time PCR | ||||
| Manifestation (Ct < 40)/total) | 5/5 | 3/4 | 5/5 | 5/5 |
| Period, dpi | 7–28 | 7–28 | 3–28 | 7–28 |
| Duration, days | 5–22 | 0–19 | 26 | 22 |
| Ct values, M ± m | 39.6 ± 4.9 | >40.0 | 36.6 ± 4.5 | 37.9 ± 4.8 |
| Minimum Ct values | 30.1–35.3 | 30.4–>40.0 | 26.9–36.3 | 25.4–36.6 |
| Viremia | ||||
| Manifestation (>2.0 TCID50/mL)/total | 5/5 | 3/4 | 5/5 | 5/5 |
| Period, dpi | 10–28 | 10–21 | 3–28 | 7–28 |
| Duration, days | 5–19 | 0–12 | 18–26 | 4–15 |
| TCID50/mL, M ± m | 101.24 ± 101.45 | 100.55 ± 101.09 | 101.88 ± 101.49 | 101.02 ± 101.29 |
| Maximum values, TCID50/mL | 102.75–104.00 | 102.75–103.75 | 103.00–103.75 | 102.25–104.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vlasov, M.; Sindryakova, I.; Kudryashov, D.; Morgunov, S.; Kolbasova, O.; Lyska, V.; Zhivoderov, S.; Pivova, E.; Balyshev, V.; Namsrayn, S.; et al. Administration Routes and Doses of the Attenuated African Swine Fever Virus Strain PSA-1NH Influence Cross-Protection of Pigs against Heterologous Challenge. Animals 2024, 14, 1277. https://doi.org/10.3390/ani14091277
Vlasov M, Sindryakova I, Kudryashov D, Morgunov S, Kolbasova O, Lyska V, Zhivoderov S, Pivova E, Balyshev V, Namsrayn S, et al. Administration Routes and Doses of the Attenuated African Swine Fever Virus Strain PSA-1NH Influence Cross-Protection of Pigs against Heterologous Challenge. Animals. 2024; 14(9):1277. https://doi.org/10.3390/ani14091277
Chicago/Turabian StyleVlasov, Mikhail, Irina Sindryakova, Dmitriy Kudryashov, Sergey Morgunov, Olga Kolbasova, Valentina Lyska, Sergey Zhivoderov, Elena Pivova, Vladimir Balyshev, Sanzhi Namsrayn, and et al. 2024. "Administration Routes and Doses of the Attenuated African Swine Fever Virus Strain PSA-1NH Influence Cross-Protection of Pigs against Heterologous Challenge" Animals 14, no. 9: 1277. https://doi.org/10.3390/ani14091277






