Smartphone Addiction and Related Factors among Athletes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Study Sample
2.3. Procedure
2.4. Variables
2.5. Statistical Analysis
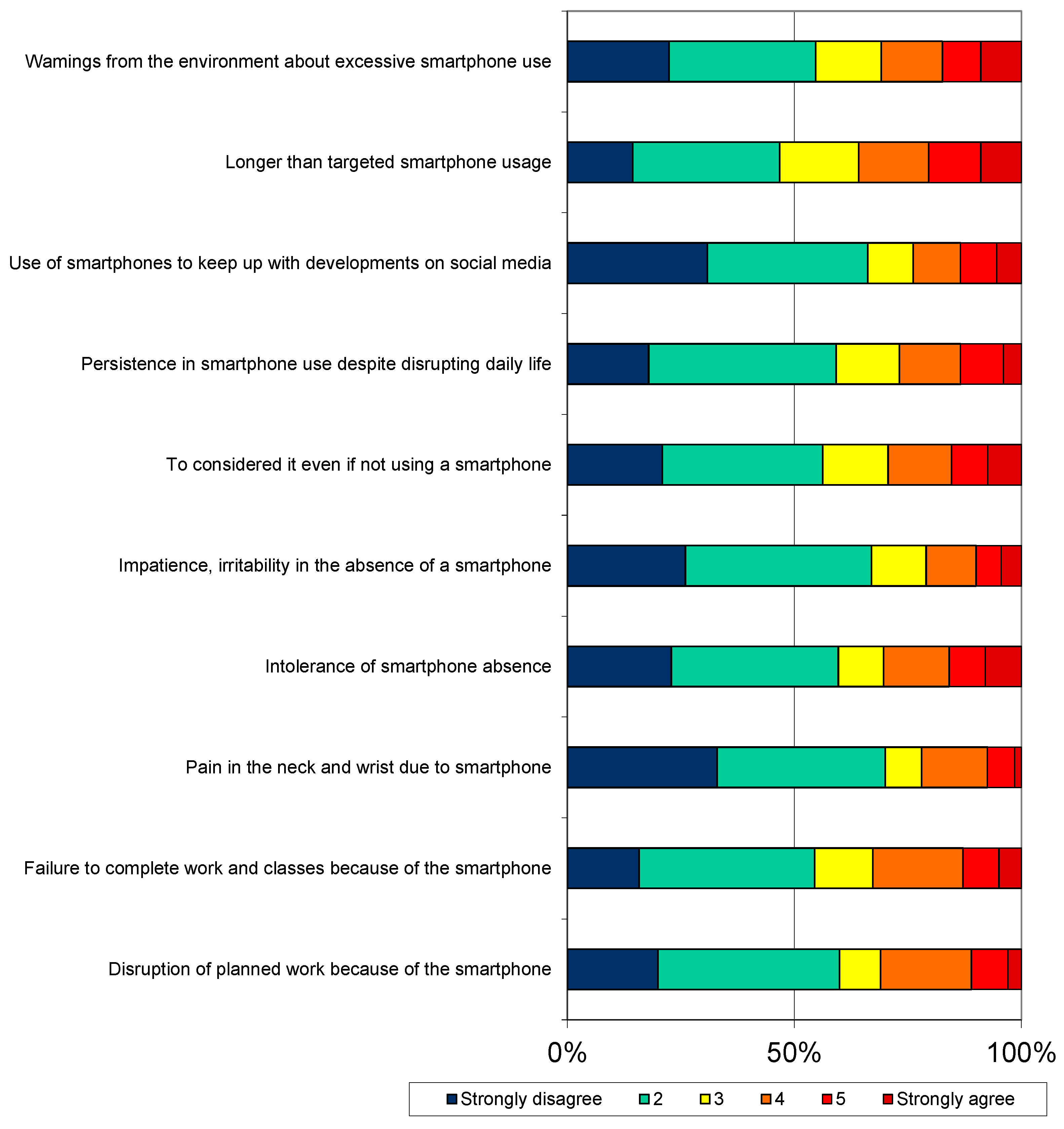
3. Results
4. Discussion
4.1. Strengths and Limitations
4.2. Comparison of the Results with the Literature
4.2.1. Socio-Demographic Variables and Prevalence of Smartphone Addiction
4.2.2. Alcohol Use and Smartphone Addiction
4.2.3. Eating Behavior and Smartphone Addiction
4.2.4. Body Perception and Smartphone Addiction
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abidoye Tiamiyu, K.; Bolanle Abdulkareem, B.; Olabis Popola, B. Internet Addiction among University Students: Causes, Consequences, and the Role of Cyber Counseling. INJIISCOM 2024, 5, 114–131. [Google Scholar]
- Kakul, F.; Javed, S. Internet Gaming Disorder: An Interplay of Cognitive Psychopathology. Asian J. Soc. Health Behav. 2023, 6, 36–45. [Google Scholar]
- Kamolthip, R.; Chirawat, P.; Ghavifekr, S.; Gan, W.Y.; Tung, S.E.H.; Nurmala, I.; Nadhiroh, S.R.; Pramukti, I.; Lin, C.-Y. Problematic Internet Use (PIU) in Youth: A Brief Literature Review of Selected Topics. Curr. Opin. Behav. Sci. 2022, 46, 101150. [Google Scholar]
- Noyan, C.O.; Enez Darcin, A.; Nurmedov, S.; Yilmaz, O.; Dilbaz, N. Akilli telefon bagimliliği olceginin kisa formunun universite ogrencilerinde Turkce gecerlilik ve guvenilirlik calismasi. Anadolu Psikiyatr. Derg. 2015, 16, 71–83. [Google Scholar] [CrossRef]
- Tateno, M.; Teo, A.R.; Ukai, W.; Kanazawa, J.; Katsuki, R.; Kubo, H.; Kato, T.A. Internet Addiction, Smartphone Addiction, and Hikikomori Trait in Japanese Young Adult: Social Isolation and Social Network. Front. Psychiatry 2019, 10, 455. [Google Scholar] [CrossRef] [PubMed]
- Olson, J.A.; Sandra, D.A.; Colucci, É.S.; Al Bikaii, A.; Chmoulevitch, D.; Nahas, J.; Raz, A.; Veissière, S.P.L. Smartphone addiction is increasing across the world: A meta-analysis of 24 countries. Comput. Hum. Behav. 2022, 129, 107138. [Google Scholar] [CrossRef]
- Blum, K.; Bowirrat, A.; Braverman, E.R.; Baron, D.; Cadet, J.L.; Kazmi, S.; Elman, I.; Thanos, P.K.; Badgaiyan, R.D.; Downs, W.B.; et al. Reward Deficiency Syndrome (RDS): A Cytoarchitectural Common Neurobiological Trait of All Addictions. Int. J. Environ. Res. Public Health 2021, 18, 11529. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, L.M.S.; Rabelo, P.C.R.; Moraes, M.M.; Coimbra, C.C. Physical exercise-induced fatigue: The role of serotonergic and dopaminergic systems. Braz. J. Med. Biol. Res. 2017, 50, e6432. [Google Scholar] [CrossRef] [PubMed]
- Rodan, S.C.; Bryant, E.; Le, A.; Maloney, D.; Touyz, S.; McGregor, I.S.; Maguire, S. National Eating Disorder Research Consortium. Pharmacotherapy, alternative and adjunctive therapies for eating disorders: Findings from a rapid review. J. Eat. Disord. 2023, 11, 112. [Google Scholar] [CrossRef]
- Barakat, S.; Mclean, S.A.; Bryant, E.; Le, A.; Marks, P.; Eating, N. Risk factors for eating disorders: Findings from a rapid review. J. Eat. Disord. 2023, 11, 8. [Google Scholar] [CrossRef]
- Thompson, A.; Petrie, T.; Anderson, C. Journal of Science and Medicine in Sport Eating disorders and weight control behaviors change over a collegiate sport season. J. Sci. Med. Sport 2017, 20, 808–813. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Padilla, I.C.; Portela-Pino, I.; Martínez-Patiño, M.J. The Risk of Eating Disorders in Adolescent Athletes: How We Might Address This Phenomenon? Sports 2024, 12, 77. [Google Scholar] [CrossRef] [PubMed]
- Flores, M.R.; Mon-l, D.; Gil-ares, J. Training Conditions and Psychological Health: Eating Behavior Disorders in Spanish High-Performance Women’s Olympic Wrestling Athletes—A Qualitative Study. Int. J. Environ. Res. Public Health 2023, 20, 2441. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, M.B.; Johansen, K.K.; Runge, E.; Hansen, M.B.; Holmberg, T.T.; Tarp, K. Behind the athletic body: A clinical interview study of identification of eating disorder symptoms and diagnoses in elite athletes. BMJ Open Sport Exerc. Med. 2022, 8, e001265. [Google Scholar] [CrossRef] [PubMed]
- Toselli, S.; Zaccagni, L.; Rinaldo, N.; Mauro, M.; Grigoletto, A.; Maietta Latessa, P.; Marini, S. Body Image Perception in High School Students: The Relationship with Gender, Weight Status, and Physical Activity. Children 2023, 10, 137. [Google Scholar] [CrossRef] [PubMed]
- Boursier, V.; Griffiths, G. Do selfie-expectancies and social appearance anxiety predict adolescents’ problematic social media use? Comput. Hum. Behav. 2023, 110, 106395. [Google Scholar] [CrossRef]
- Yilmaz, R.; Sulak, S.; Griffiths, M.D.; Yilmaz, F.G.K. An Exploratory Examination of the Relationship Between Internet Gaming Disorder, Smartphone Addiction, Social Appearance Anxiety and Aggression Among Undergraduate Students. J. Affect. Disord. Rep. 2023, 11, 100483. [Google Scholar] [CrossRef]
- Kwon, S.; Kim, R.; Lee, J.T.; Kim, J.; Song, S.; Kim, S.; Oh, H. Association of Smartphone Use with Body Image Distortion and Weight Loss Behaviors in Korean Adolescents. JAMA Netw. Open 2022, 5, E2213237. [Google Scholar] [CrossRef] [PubMed]
- Jochimek, M.; Krokosz, D.; Lipowski, M. Physical activity and sport as a protective factor against health- -threatening experiments with adulthood. Balt. J. Health Phys. Act. 2017, 9, 112–124. [Google Scholar] [CrossRef]
- Xu, P.; Chen, J.-S.; Chang, Y.-L.; Wang, X.; Jiang, X.; Griffiths, M.D.; Pakpour, A.H.; Lin, C.-Y. Gender differences in the associations between physical activity, smartphone use, and weight stigma. Front. Public Health 2022, 10, 862829. [Google Scholar] [CrossRef]
- Ong, N.C.H.; Kee, Y.H.; Pillai, J.S.; Lim, H.B.T.; Chua, J.H.E. Problematic mobile phone use among youth athletes: A topic modelling approach. Int. J. Sport Exerc. Psychol. 2023, 21, 616–637. [Google Scholar] [CrossRef]
- Buke, M.; Egesoy, H.; Unver, F. The effect of smartphone addiction on physical activity level in sports science undergraduates. J. Bodyw. Mov. Ther. 2021, 28, 530–534. [Google Scholar] [CrossRef] [PubMed]
- Gezgin, D.M.; Mihci, C. Smartphone addiction in undergraduate athletes: Reasons and effects of using Instagram intensively. Int. J. Technol. Educ. Sci. (IJTES) 2020, 4, 188–202. [Google Scholar] [CrossRef]
- Karnincic, H.; Cavala, M.; Rogulj, N. The Relationship between Handball Players and Alcohol and Smoking Habits. J. Hum. Kinet. 2018, 63, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.-C.; Latner, J.D.; O’Brien, K.S.; Chang, Y.-L.; Hung, C.-H.; Chen, J.-S.; Lee, K.-H.; Lin, C.-Y. Associations between social media addiction, psychological distress, and food addiction among Taiwanese university students. J. Eat. Disord. 2023, 11, 43. [Google Scholar] [CrossRef] [PubMed]
- Protzner, A.; Szmodis, M.; Udvardy, A.; Bosnyák, E.; Trájer, E.; Komka, Z.; Györe, I.; Tóth, M. Correction: Hormonal Neuroendocrine and Vasoconstrictor Peptide Responses of Ball Game and Cyclic Sport Elite Athletes by Treadmill Test. PLoS ONE 2016, 11, e0153905. [Google Scholar] [CrossRef] [PubMed]
- Kwon, M.; Kim, D.J.; Cho, H.; Yang, S. The Smartphone Addiction Scale: Development and Validation of a Short Version for Adolescents. PLoS ONE 2013, 8, e83558. [Google Scholar] [CrossRef] [PubMed]
- Stunkard, A.J.; Messick, S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J. Psychosom. Res. 1985, 29, 71–83. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, J.; Persson, L.O.; Sjöström, L.; Sullivan, M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int. J. Obes. 2000, 24, 1715–1725. [Google Scholar] [CrossRef]
- Kirac, D.; Kaspar, E.; Avcilar, T.; Cakir, O.; Ulucan, K.; Kurtel, H.; Deyneli, O.; Guney, A. A New Method for Investigating Eating Behaviours Related with Obesity “ Three-Factor Eating Questionnaire. J. Marmara Univ. Inst. Health Sci. 2015, 5, 162–169. [Google Scholar] [CrossRef]
- Secord, P.F.; Jourard, S.M. The appraisal of body-cathexis: Body-cathexis and the self. J. Consult. Psychol. 1953, 17, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Hovardaoglu, S. Vücut Algısı Olçegi. Psikiyatri, Psikoloji, Psikofarmakoloji Dergisi (3P). Test. Ozel. Eki. 1992, 1, 26–27. [Google Scholar]
- Hamurcu, P.; Telatar, B.; Yesildag, S. Obezitenin benlik saygisi ve beden algisi üzerine etkisi. The impact of obesity on self-esteem and body image. Türk. Aile Hek. Derg. 2015, 19, 122–128. [Google Scholar] [CrossRef]
- Lee, D.K. Alternatives to P value: Confidence interval and effect size. Korean J. Anesthesiol. 2016, 69, 555–562. [Google Scholar] [CrossRef]
- Tayfur, S.N.; Evrensel, A. Investigation of the relationships between eating attitudes, bergbody image and depression among Turkish university students. Riv. Psichiatr. 2020, 55, 90–97. [Google Scholar] [CrossRef]
- Cappelleri, J.C.; Bushmakin, A.G.; Gerber, R.A.; Leidy, N.K.; Sexton, C.C.; Karlsson, J.; Lowe, M.R. Evaluating the Power of Food Scale in obese subjects and a general sample of individuals: Development and measurement properties. Int. J. Obes. 2009, 33, 913–922. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Lotfi, A.; Lin, C.-Y.; Griffiths, M.D.; Pakpour, A.H. Estimation of behavioral addiction prevalence during COVID-19 pandemic: A systematic review and meta-analysis. Curr. Addict. Rep. 2022, 9, 486–517. [Google Scholar] [CrossRef]
- Gjoneska, B.; Potenza, M.N.; Jones, J.; Corazza, O.; Hall, N.; Sales, C.M.D.; Grünblatt, E.; Martinotti, G.; Burkauskas, J.; Werling, A.M.; et al. Problematic use of the internet during the COVID-19 pandemic: Good practices and mental health recommendations. Compr. Psychiatry 2022, 112, 152279. [Google Scholar] [CrossRef] [PubMed]
- Baloglu, M.; Sahin, R.; Arpaci, I. A review of recent research in problematic internet use: Gender and cultural differences. Curr. Opin. Psychol. 2020, 36, 124–129. [Google Scholar] [CrossRef]
- Buctot, D.B.; Kim, N.; Kim, S.H. Comparing the Mediating Effect of Adolescent Lifestyle Profiles on the Relationship between Smartphone Addiction and Health-Related Quality of Life Among Male and Female Senior High School Students in the Philippines. Int. J. Ment. Health Addict. 2021, 21, 511–528. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, K.Z.K.; Gong, X.; Zhao, S.J.; Lee, M.K.O.; Liang, L. Examining the effects of motives and gender differences on smartphone addiction. Comput. Hum. Behav. 2017, 75, 891–902. [Google Scholar] [CrossRef]
- Choo, Y.-K.; Bae, W.-S.; Kim, H.-I. Analysis of Major Factors Related to Smartphone Addiction According to Gender Differences in Health College Students. J. Korean Soc. Integr. Med. 2022, 10, 135–143. [Google Scholar] [CrossRef]
- Koob, G.F. Addiction is a reward deficit and stress surfeit disorder. Front. Psychiatry 2013, 4, 72. [Google Scholar] [CrossRef] [PubMed]
- Cha, S.S.; Seo, B.K. Smartphone use and smartphone addiction in middle school students in Korea: Prevalence, social networking service, and game use. Health Psychol. Open 2018, 5, 2055102918755046. [Google Scholar] [CrossRef] [PubMed]
- Akbulut Zencirci, S.; Aygar, H.; Goktas, S.; Onsuz, M.F.; Alaiye, M.; Metintas, S. Evaluation of smartphone addiction and related factors among university students. Int. J. Res. Med. Sci. 2018, 6, 2210. [Google Scholar] [CrossRef]
- Alotaibi, M.S.; Fox, M.; Coman, R.; Ratan, Z.A.; Hosseinzadeh, H. Smartphone Addiction Prevalence and Its Association on Academic Performance, Physical Health, and Mental Well-Being among University Students in Umm Al-Qura University (UQU), Saudi Arabia. Int. J. Environ. Res. Public Health 2022, 19, 3710. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.W.; Kim, D.J.; Choi, J.S.; Ahn, H.; Choi, E.J.; Song, W.Y.; Kim, S.; Youn, H. Comparison of risk and protective factors associated with smartphone addiction and Internet addiction. J. Behav. Addict. 2015, 4, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, J.D.S.; de Fonseca, F.R.; Rubio, G. Cell-phone addiction: A review. Front. Psychiatry 2016, 7, 175. [Google Scholar] [CrossRef]
- Lopez-Fernandez, O. Emerging health and education issues related to internet technologies and addictive problems. Int. J. Environ. Res. Public Health 2021, 18, 321. [Google Scholar] [CrossRef]
- De-Sola, J.; Talledo, H.; Rubio, G.; de Fonseca, F.R. Psychological Factors and Alcohol Use in Problematic Mobile Phone Use in the Spanish Population. Front. Psychiatry 2017, 8, 11. [Google Scholar] [CrossRef]
- Sohi, I.; Chrystoja, B.R.; Rehm, J.; Wells, S.; Monteiro, M.; Ali, S.; Shield, K.D. Changes in alcohol use during the COVID-19 pandemic and previous pandemics: A systematic review. Alcohol. Clin. Exp. Res. 2022, 46, 498–513. [Google Scholar] [CrossRef] [PubMed]
- Serra, G.; Lo Scalzo, L.; Giuffrè, M.; Ferrara, P.; Corsello, G. Smartphone use and addiction during the coronavirus disease 2019 (COVID-19) pandemic: Cohort study on 184 Italian children and adolescents. Ital. J. Pediatr. 2021, 47, 150. [Google Scholar] [CrossRef] [PubMed]
- Leasure, J.L.; Neighbors, C.; Henderson, C.E.; Young, C.M. Exercise and Alcohol Consumption: What We Know, What We Need to Know, and Why It Is Important. Front. Psychiatry 2015, 6, 156. [Google Scholar] [CrossRef] [PubMed]
- Hahn, T.; Notebaert, K.H.; Dresler, T.; Kowarsch, L.; Reif, A.; Fallgatter, A.J. Linking online gaming and addictive behavior: Converging evidence for a general reward deficiency in frequent online gamers. Front. Behav. Neurosci. 2014, 8, 385. [Google Scholar] [CrossRef] [PubMed]
- Flack, K.; Pankey, C.; Ufholz, K.; Johnson, L.; Roemmich, J.N. Genetic variations in the dopamine reward system influence exercise reinforcement and tolerance for exercise intensity. Behav. Brain Res. 2019, 375, 112148. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Xu, X.; Lin, X.; Chen, Y.; Zheng, F.; Bei, Y.; Zhang, L.; Zhang, B. Association of mobile phone overuse with sleep disorder and unhealthy eating behaviors in college students of a medical university in Guangzhou. J. South. Med. Univ. 2019, 39, 1500–1505. [Google Scholar] [CrossRef]
- Singh, N.A. Comparative study of eating behaviour among the team sports. Int. J. Phys. Educ. Sports Health 2018, 5, 85–87. [Google Scholar]
- Hebebrand, J.; Albayrak, O.; Adan, R.; Antel, J.; Dieguez, C.; De Jong, J.; Leng, G.; Menzies, J.; Mercer, J.G.; Murphy, M.; et al. Neuroscience and Biobehavioral Reviews “Eating addiction”, rather than “food addiction ”, better captures addictive-like eating behavior. Neurosci. Biobehav. Rev. 2014, 47, 295–306. [Google Scholar] [CrossRef]
- Avena, N.M.; Simkus, J.; Lewandowski, A.; Gold, M.S.; Potenza, M.N. Substance Use Disorders and Behavioral Addictions During the COVID-19 Pandemic and COVID-19-Related Restrictions. Front. Psychiatry 2021, 12, 653674. [Google Scholar] [CrossRef]
- Langbein, R.K.; Martin, D.; Allen-collinson, J.; Crust, L.; Jackman, P.C.; Langbein, R.K.; Martin, D.; Allen-collinson, J.; Crust, L.; Martin, D.; et al. “I’d got self-destruction down to a fine art”: A qualitative exploration of relative energy deficiency in sport (RED-S) in endurance athletes energy deficiency in sport (RED-S) in endurance athletes ABSTRACT. J. Sports Sci. 2021, 39, 1555–1564. [Google Scholar] [CrossRef]
- Ayran, G.; Suleyman, Z.; Avci, U. The effect of Internet addiction on eating attitude and body image in university students. J. Child Adolesc. Psychiatr. Nurs. 2021, 34, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y. Smartphone addiction: Psychological and social factors predict the use and abuse of a social mobile application, Information. Commun. Soc. 2020, 23, 454–467. [Google Scholar] [CrossRef]
- Liu, Q.; Sun, J.; Li, Q.; Zhou, Z. Body dissatisfaction and smartphone addiction among Chinese adolescents: A moderated mediation model. Child. Youth Serv. Rev. 2019, 108, 104613. [Google Scholar] [CrossRef]
- Goicochea, E.A.; Coloma-Naldos, B.; Moya-Salazar, J.; Rojas-Zumaran, V.; Moya-Espinoza, J.G.; Contreras-Pulache, H. Physical Activity and Body Image Perceived by University Students during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 16498. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic and Economic Characteristics | Addicted to Smartphones | Not Addicted to Smartphones | Total ** | Effect Size | p | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||||
| Age | 23 years and under | 48 | 28.2 | 122 | 71.8 | 170 | 84.1 | 0.026 | 0.708 |
| 24 years and older | 8 | 25.0 | 24 | 75.0 | 32 | 15.9 | |||
| Sex | Female | 43 | 33.9 | 84 | 66.1 | 127 | 62.9 | 0.178 | 0.011 * |
| Male | 13 | 17.3 | 62 | 82.7 | 75 | 37.1 | |||
| Education Status | Middle school–high school | 38 | 27.7 | 99 | 72.3 | 137 | 67.8 | 0.000 | 0.995 |
| University and above | 18 | 27.7 | 47 | 72.3 | 65 | 32.2 | |||
| Monthly Average Income | Low | 10 | 17.2 | 48 | 82.8 | 58 | 28.7 | 0.149 | 0.035 * |
| High | 46 | 31.9 | 98 | 68.1 | 144 | 71.3 | |||
| Active Training/Sports | Yes | 50 | 26.2 | 141 | 73.8 | 191 | 94.6 | 0.144 | 0.041 * |
| No | 6 | 54.5 | 5 | 45.5 | 11 | 5.4 | |||
| Diagnosed Disease | Yes | 7 | 31.8 | 15 | 68.2 | 22 | 10.9 | 0.032 | 0.649 |
| No | 49 | 27.2 | 131 | 72.8 | 180 | 89.1 | |||
| BMI Groups | 17.00–18.49 | 1 | 20.0 | 4 | 80.0 | 5 | 2.5 | 0.034 | 0.887 |
| 18.50–24.90 | 44 | 27.5 | 116 | 72.5 | 160 | 79.2 | |||
| 25.00 and above | 11 | 29.7 | 26 | 70.3 | 37 | 18.3 | |||
| Cigarette Use | I don’t smoke | 43 | 25.9 | 123 | 74.1 | 166 | 82.2 | 0.087 | 0.215 |
| Smoking | 13 | 36.1 | 23 | 63.9 | 36 | 17.8 | |||
| Alcohol Usage | Yes | 25 | 38.5 | 40 | 61.5 | 65 | 32.2 | 0.165 | 0.019 * |
| No | 31 | 22.6 | 106 | 77,4 | 137 | 67.8 | |||
| Nutrition Specifications | Addicted to Smartphone | Not Addicted to Smartphone | Total ** | Effect Size | p | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Body perception score | 48–134 points | 48 | 25.5 | 140 | 74.5 | 188 | 93.6 | 0.179 | 0.025 * |
| 135–192 points | 8 | 57.1 | 6 | 42.9 | 14 | 6.4 | |||
| Three-factor nutrition score | 20–29 | 3 | 10.0 | 27 | 90.0 | 30 | 14.8 | 0.244 | 0.017 * |
| 30–39 | 11 | 20.0 | 44 | 80.0 | 55 | 27.1 | |||
| 40–49 | 28 | 38.4 | 45 | 61.6 | 73 | 36.1 | |||
| 50–59 | 7 | 25.9 | 20 | 74.1 | 27 | 13.4 | |||
| 60–69 | 7 | 41.2 | 10 | 58.8 | 17 | 8.4 | |||
| Uncontrolled eating factor | 5–9 points | 7 | 12.1 | 51 | 87.9 | 58 | 28.7 | 0.244 | 0.002 * |
| 10–14 points | 29 | 30.2 | 67 | 69.8 | 96 | 47.5 | |||
| 15+ points | 20 | 41.7 | 28 | 58.3 | 48 | 23.8 | |||
| Emotional eating factor | 3–6 points | 17 | 15.7 | 91 | 84.3 | 108 | 53.5 | 0.290 | <0.001 * |
| 7–10 points | 27 | 39.7 | 41 | 60.3 | 68 | 33.7 | |||
| 11 + points | 12 | 46.2 | 14 | 53.9 | 26 | 12.8 | |||
| Inability to constrain factor | 4–7 points | 11 | 24.4 | 34 | 75.6 | 45 | 22.3 | 0.075 | 0.567 |
| 8–11 points | 30 | 31.3 | 66 | 68.8 | 96 | 47.5 | |||
| 12+ points | 15 | 24.6 | 46 | 75.4 | 61 | 30.2 | |||
| Hunger factor | 4–7 points | 16 | 18.4 | 71 | 81.6 | 87 | 43.0 | 0.184 | 0.033 * |
| 8–11 points | 23 | 33.3 | 46 | 66.7 | 69 | 34.2 | |||
| 12+ points | 17 | 37.0 | 29 | 63.0 | 46 | 22.8 | |||
| Variables | OR | (%95 GA) | p | |
|---|---|---|---|---|
| Sex | Ref: Male | 1 | ||
| Female | 2.49 | GA: 1.17–5.31 | 0.018 * | |
| Alcohol use | Ref: No alcohol consumption | 1 | ||
| Alcohol consumption | 2.01 | GA: 1.01–4.06 | 0.048 * | |
| Active training/sports | Ref: Regular sports are practiced | 1 | ||
| Lack of regular exercise | 2.04 | GA: 0.50–8.39 | 0.320 | |
| Three-factor nutrition score | Ref: Low-scale score | 1 | ||
| High scale score | 2.17 | GA: 1.04–4.58 | 0.042 * | |
| Income | Ref: Low income | 1 | ||
| High income level | 2.65 | GA: 1.15–6.10 | 0.022 * | |
| Body perception score | Ref: Low scale score | 1 | ||
| High scale score | 2.66 | GA: 1.07–6.64 | 0.036 * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sahin Koybulan, S.; Altin, D.; Yararbas, G.; Hassoy, H. Smartphone Addiction and Related Factors among Athletes. Behav. Sci. 2024, 14, 341. https://doi.org/10.3390/bs14040341
Sahin Koybulan S, Altin D, Yararbas G, Hassoy H. Smartphone Addiction and Related Factors among Athletes. Behavioral Sciences. 2024; 14(4):341. https://doi.org/10.3390/bs14040341
Chicago/Turabian StyleSahin Koybulan, Sultan, Duygu Altin, Gorkem Yararbas, and Hur Hassoy. 2024. "Smartphone Addiction and Related Factors among Athletes" Behavioral Sciences 14, no. 4: 341. https://doi.org/10.3390/bs14040341







