Exploring Relationships between Recurrent Binge Eating and Illicit Substance Use in a Non-Clinical Sample of Women over Two Years
Abstract
:1. Introduction
1.1. Background
1.2. Co-Morbidity
1.3. Longitudinal Predictors
1.4. Aim and Hypotheses
2. Materials and Methods
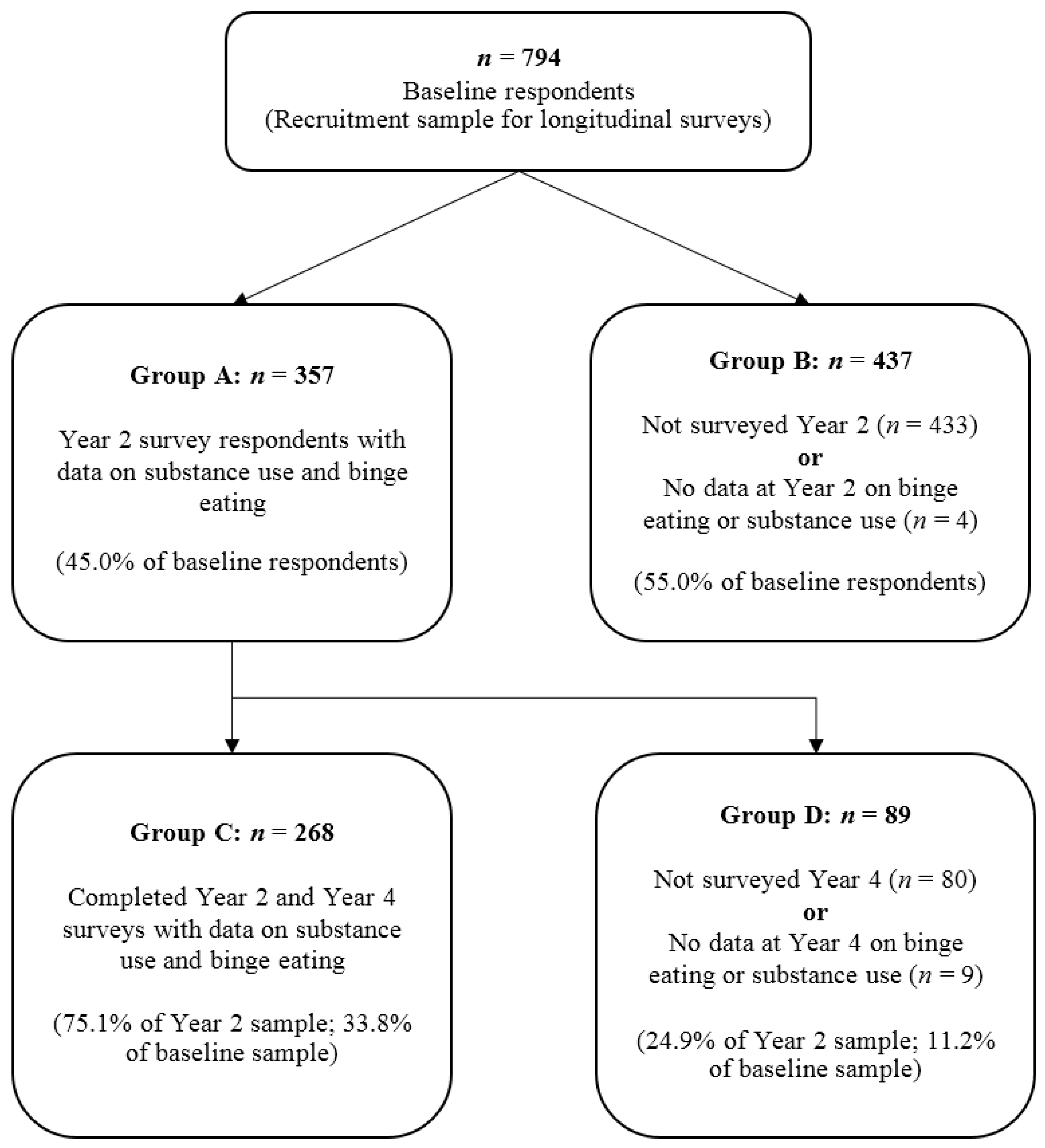
2.1. Participants
2.2. Procedures
2.3. Measures
2.3.1. Binge Eating
2.3.2. Illicit Substance Use (ISU)
2.3.3. Psychological Distress
2.3.4. Health-Related Quality of Life (HRQoL)
2.4. Statistical Methods
3. Results
3.1. Participant Features
3.2. Co-Morbid ISU and RBE in the T2 Cohort
3.3. Participant Trajectories from T2 to T4
4. Discussion
4.1. Comorbid Psychopathology
4.2. Participant Trajectories and Between-Group Associations
4.3. Strengths and Limitations
4.4. Clinical Implications
4.5. Future Directions
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Cassin, S.E.; von Ranson, K.M. Is binge eating experienced as an addiction? Appetite 2007, 49, 687–690. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; White, M.A.; Potenza, M.N. Binge eating disorder and food addiction. Curr. Drug Abuse Rev. 2011, 4, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, L.R.; Odlaug, B.L.; Grant, J.E. The overlap between binge eating disorder and substance use disorders: Diagnosis and neurobiology. J. Behav. Addict. 2013, 2, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.G.; Robbins, T.W. The neurobiological underpinnings of obesity and binge eating: A rationale for adopting the food addiction model. Biol. Psychiatry 2013, 73, 804–810. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Feeding and Eating Disorders. In Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Grant, J.E.; Potenza, M.N.; Weinstein, A.; Gorelick, D.A. Introduction to behavioral addictions. Am. J. Drug Alcohol. Abuse 2010, 36, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Ferriter, C.; Ray, L.A. Binge eating and binge drinking: An integrative review. Eat Behav. 2011, 12, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Schulte, E.M.; Grilo, C.M.; Gearhardt, A.N. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin. Psychol. Rev. 2016, 44, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Avena, N.M.; Rada, P.; Hoebel, B.G. Evidence for sugar addiction: Behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci. Biobehav. Rev. 2008, 32, 20–39. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.M.; Kenny, P.J. Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats. Nat. Neurosci. 2010, 13, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Avena, N.M.; Rada, P.; Hoebel, B.G. Sugar and fat bingeing have notable differences in addictive-like behavior. J. Nutr. 2009, 139, 623–628. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Feeding and Eating Disorders. In Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Harrop, E.N.; Marlatt, G.A. The comorbidity of substance use disorders and eating disorders in women: Prevalence, etiology, and treatment. Addict. Behav. 2010, 35, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Hudson, J.I.; Hiripi, E.; Pope, H.G., Jr.; Kessler, R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 2007, 61, 348–358. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Berglund, P.A.; Chiu, W.T.; Deitz, A.C.; Hudson, J.I.; Shahly, V.; Aguilar-Gaxiola, S.; Alonso, J.; Angermeyer, M.C.; Benjet, C.; et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol. Psychiatry 2013, 73, 904–914. [Google Scholar] [CrossRef] [PubMed]
- Gregorowski, C.; Seedat, S.; Jordaan, G.P. A clinical approach to the assessment and management of co-morbid eating disorders and substance use disorders. BMC Psychiatry 2013, 13, 289. [Google Scholar] [CrossRef] [PubMed]
- Calero-Elvira, A.; Krug, I.; Davis, K.; Lopez, C.; Fernandez-Aranda, F.; Treasure, J. Meta-analysis on drugs in people with eating disorders. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2009, 17, 243–259. [Google Scholar] [CrossRef] [PubMed]
- Root, T.L.; Pisetsky, E.M.; Thornton, L.; Lichtenstein, P.; Pedersen, N.L.; Bulik, C.M. Patterns of co-morbidity of eating disorders and substance use in Swedish females. Psychol. Med. 2010, 40, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Piran, N.; Robinson, S.R. Associations between disordered eating behaviors and licit and illicit substance use and abuse in a university sample. Addict. Behav. 2006, 31, 1761–1775. [Google Scholar] [CrossRef] [PubMed]
- Piran, N.; Robinson, S.R. Patterns of associations between eating disordered behaviors and substance use in two non-clinical samples: A university and a community based sample. J. Health Psychol. 2011, 16, 1027–1037. [Google Scholar] [CrossRef] [PubMed]
- Measelle, J.R.; Stice, E.; Hogansen, J.M. Developmental trajectories of co-occurring depressive, eating, antisocial, and substance abuse problems in female adolescents. J. Abnorm. Psychol. 2006, 115, 524–538. [Google Scholar] [CrossRef] [PubMed]
- Patton, G.C.; Coffey, C.; Carlin, J.B.; Sanci, L.; Sawyer, S. Prognosis of adolescent partial syndromes of eating disorder. Br. J. Psychiatry 2008, 192, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Sonneville, K.R.; Horton, N.J.; Micali, N.; Crosby, R.D.; Swanson, S.A.; Solmi, F.; Field, A.E. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: Does loss of control matter? JAMA Pediatr. 2013, 167, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Vogeltanz-Holm, N.D.; Wonderlich, S.A.; Lewis, B.A.; Wilsnack, S.C.; Harris, T.R.; Wilsnack, R.W.; Kristjanson, A.F. Longitudinal predictors of binge eating, intense dieting, and weight concerns in a national sample of women. Behav. Ther. 2000, 31, 221–235. [Google Scholar] [CrossRef]
- Konkoly Thege, B.; Woodin, E.M.; Hodgins, D.C.; Williams, R.J. Natural course of behavioral addictions: A 5-year longitudinal study. BMC Psychiatry 2015, 15, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, J.E.; Schreiber, L.R.; Odlaug, B.L. Phenomenology and treatment of behavioural addictions. Can J. Psychiatry 2013, 58, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Cowan, J.; Devine, C. Food, eating, and weight concerns of men in recovery from substance addiction. Appetite 2008, 50, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Long, C.G.; Blundell, J.E.; Finlayson, G. A Systematic Review of the Application And Correlates of YFAS-Diagnosed ‘Food Addiction’ in Humans: Are Eating-Related ‘Addictions’ a Cause for Concern or Empty Concepts? Obes. Facts 2015, 8, 386–401. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Beglin, S.J. Assessment of eating disorders: Interview or self-report questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar] [PubMed]
- Wilfley, D.E.; Schwartz, M.B.; Spurrell, E.B.; Fairburn, C.G. Assessing the specific psychopathology of binge eating disorder patients: Interview or self-report? Behav. Res. Ther. 1997, 35, 1151–1159. [Google Scholar] [CrossRef]
- Al-Adawi, S.; Bax, B.; Bryant-Waugh, R.; Claudino, A.M.; Hay, P.; Monteleone, P.; Norring, C.; Pike, K.M.; Pilon, D.J.; Herscovici, C.R.; et al. Revision of ICD—Status update on feeding and eating disorders. Adv. Eat. Disord. 2013, 1, 10–20. [Google Scholar] [CrossRef]
- Grilo, C.M.; White, M.A. A controlled evaluation of the distress criterion for binge eating disorder. J. Consult. Clin. Psychol. 2011, 79, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, B.E.; Baker, C.W.; Smith, A.T.; Kelly-Weeder, S. Validity and utility of the current definition of binge eating. Int. J. Eat. Disord. 2009, 42, 674–686. [Google Scholar] [CrossRef] [PubMed]
- Womens Health Australia. The Australian Longitudinal Study on Women’s Health: Data Book, 2nd ed.; Womens Health Australia: Newcastle, UK, 1997. [Google Scholar]
- Andrews, G.; Slade, T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust. N. Z. J. Public Health 2001, 25, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Vargas Terrez, B.E.; Villamil Salcedo, V.; Rodríguez Estrada, C.; Pérez Romero, J.; Cortés Sotres, J. Validación de la escala Kessler 10 (K-10) en la detección de depresión y ansiedad en el primer nivel de atención. Propiedades psicométricas. Salud Ment. 2011, 34, 323–331. [Google Scholar]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, K.; Andrews, G. The SF-12 in the Australian population: Cross-validation of item selection. Aust. N. Z. J. Public Health 2002, 26, 343–345. [Google Scholar] [CrossRef] [PubMed]
- Mond, J.M.; Hay, P.J.; Rodgers, B.; Owen, C.; Beumont, P.J. Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav. Res. Ther. 2004, 42, 551–567. [Google Scholar] [CrossRef]
- Davis, C.; Carter, J.C. Compulsive overeating as an addiction disorder. A review of theory and evidence. Appetite 2009, 53, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Killeen, T.; Brewerton, T.D.; Campbell, A.; Cohen, L.R.; Hien, D.A. Exploring the relationship between eating disorder symptoms and substance use severity in women with comorbid PTSD and substance use disorders. Am. J. Drug Alcohol. Abuse 2015, 41, 547–552. [Google Scholar] [PubMed]
- Grilo, C.M.; White, M.A.; Masheb, R.M. DSM-IV psychiatric disorder comorbidity and its correlates in binge eating disorder. Int. J. Eat. Disord. 2009, 42, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Edge, P.J.; Gold, M.S. Drug withdrawal and hyperphagia: Lessons from tobacco and other drugs. Curr. Pharm. Des. 2011, 17, 1173–1179. [Google Scholar] [CrossRef] [PubMed]
- Orsini, C.A.; Ginton, G.; Shimp, K.G.; Avena, N.M.; Gold, M.S.; Setlow, B. Food consumption and weight gain after cessation of chronic amphetamine administration. Appetite 2014, 78, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; McClair, V.L. Epidemiology of substance use disorders. Hum. Genet. 2012, 131, 779–789. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Substance-Related and Addictive Disorders. In Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
| n | Mean | Standard Deviation | Median | Interquartile Range | |
|---|---|---|---|---|---|
| Age/years at year 2 | 354 | 30.7 | 11.4 | 25 | 15 |
| Body Mass Index (kg/m2) | 342 | 24.8 | 5.5 | 23.5 | 5.3 |
| Eating Disorder Examination—Questionnaire | |||||
| Weight concern subscale | 353 | 2.04 | 1.54 | 1.80 | 2.60 |
| Eating concern subscale | 350 | 0.953 | 1.18 | 0.400 | 1.20 |
| Shape concern subscale | 346 | 2.37 | 1.58 | 2.13 | 2.63 |
| Restraint subscale | 352 | 1.57 | 1.43 | 1.20 | 2.00 |
| Global Score | 336 | 1.74 | 1.29 | 1.44 | 1.95 |
| Illicit substance use frequency 1 | 357 | 0.65 | 1.72 | 0 | 0 |
| Kessler 10 Psychological Distress Scale | 351 | 17.5 | 6 | 16 | 7 |
| Short Form-12 2 Physical Component Score | 348 | 52.1 | 8.2 | 54.5 | 8.3 |
| Short Form-12 Mental Component Score | 348 | 44.9 | 11.3 | 48.6 | 16.7 |
| Feature | Group A 1 | Group B 2 | Group C 3 | Group D 4 | ||
|---|---|---|---|---|---|---|
| Mean (SD) n | t, p | Mean (SD) n | t, p | |||
| Age | 28.7 (11.4) 354 | 26.5 (10.5) 426 | −2.85, 0.005 | 31.7 (12.02) 266 | 27.9 (8.54) 88 | −2.74, 0.006 |
| Body Mass Index (kg/m2) | 24.3 (5.23) 336 | 23.7 (5.52) 409 | −1.59, 0.11 | 24.91 (5.62) 254 | 24.5 (5.17) 88 | −6.1, 0.545 |
| Median (IQR) n | z, p | Median (IQR) n | z, p | |||
| OBE/month | 0 (0–1) 340 | 0 (0–0) 408 | −3.34, 0.001 | 0 (0–0) 268 | 0 (0–0) 89 | −0.62, 0.534 |
| SBE/month | 0 (0–2) 340 | 0 (0–0) 408 | −2.75, 0.01 | 0 (0–2) 267 | 0 (0–2) 89 | −0.09, 0.928 |
| ISU | n.a. (ISU not assessed at baseline) | 0 (0–0) 267 | 0 (0–1) 89 | −1.70, 0.089 | ||
| Level of Behaviour | Median, IQ Range, n | Mann–Whitney U Z, p | |
|---|---|---|---|
| n = 357 | RBE | No RBE | |
| ISU | 1, 0–6, 73 | 0, 0–2, 282 | −2.612, 0.009 |
| ISU | No. ISU | ||
| RBE | 0, 0–6, 76 | 0, 0–2, 281 | −2.234, 0.026 |
| Neither 1 | RBE 2 | ISU 3 | Both 4 | Post-Hoc Tests with p < 0.05 | ||
|---|---|---|---|---|---|---|
| Outcome | mean, SD, n | ANOVA F (df), p | Tukey test | |||
| EDE-Q Global | 1.56, 1.21, 210 | 2.62, 1.38, 59 | 2.12, 1.43, 49 | 3.16, 1.23, 21 | 18.19 (3), <0.001 | Neither ≠ Both, ISU, RBE; ISU ≠ Both |
| EDE-Q Restraint | 1.17, 1.20, 219 | 2.59, 1.44, 59 | 1.46, 1.41, 50 | 2.87, 1.43, 23 | 27.33 (3), <0.001 | Neither ≠ Both, RBE; ISU ≠ Both, RBE |
| EDE-Q Eating Concern | 0.52, 0.74, 216 | 2.11, 1.29, 59 | 0.69, 0.73, 51 | 2.46,1.43, 23 | 70.62 (3), <0.001 | Neither ≠ Both, RBE; ISU ≠ Both, RBE |
| EDE-Q Shape concern | 1.86, 1.32, 210 | 3.82, 1.36, 59 | 2.01, 1.36, 53 | 3.89, 1.44, 23 | 44.24 (3), <0.001 | Neither ≠ Both, RBE; ISU ≠ Both, RBE |
| EDE-Q Weight Concern | 1.56, 1.28, 218 | 3.41, 1.42, 58 | 1.71, 1.24, 53 | 3.66, 1.43, 23 | 43.65 (3), <0.001 | Neither ≠ Both, RBE; ISU ≠ Both, RBE |
| SF-12 MCS | 45.94, 10.77, 219 | 43.04, 11.71, 59 | 44.31, 1.60, 52 | 41.09, 11.79, 23 | 2.13 (3), 0.096 | n.a. |
| SF-12 PCS | 52.61, 7.32, 291 | 51.24, 9.05, 59 | 53.15, 6.61, 52 | 51.20, 7.35, 23 | 0.89 (3), 0.45 | n.a. |
| K-10 score | 17.50, 6.23, 218 | 21.07, 7.65, 60 | 19.12, 7.8, 52 | 22.09, 7.99, 23 | 6.54 (3), <0.001 | Neither ≠ RBE, Both |
| median, IQ range, n | Kruskal–Wallis Χ2 (df), p | Mann–Whitney U Z, p | ||||
| Body Mass Index (kg/m2) | 23.6, 21.5–26.4 211 | 23.2, 20.8–29.2 57 | 23.5, 20.9–25.0 50 | 23.1, 20.2–25.0 23 | 1.924 (3), 0.588 | n.a. |
| Year 4 Participants | ||||
|---|---|---|---|---|
| n (%) | ||||
| Year 2 Participants | Neither | Both | ISU | RBE |
| Neither 1 | 139 (82.2) | 2 (1.2) | 7 (4.1) | 21 (12.4) |
| Both 2 | 2 (15.4) | 6 (46.2) | 3 (23.1) | 2 (15.4) |
| ISU 3 | 9 (23.1) | 7 (17.9) | 18 (46.2) | 5 (12.8) |
| RBE 4 | 26 (57.8) | 1 (2.2) | 1 (2.2) | 17 (37.8) |
| Year 4 Outcome Estimated Marginal Probability with 95% Confidence Interval | ||||
|---|---|---|---|---|
| Neither RBE nor ISU | Both RBE & ISU | RBE Only | ISU Only | |
| Year 2 Status | ||||
| Neither RBE nor ISU | 0.825 a (0.764, 0.886) | 0.009 (−0.005, 0.024) | 0.120 a (0.068, 0.172) | 0.045 b (0.012, 0.078) |
| Both RBE & ISU | 0.213 (−0.556, 0.481) | 0.334 c (0.009, 0.659) | 0.139 (−0.052, 0.331) | 0.314 c (0.007, 0.621) |
| RBE Only | 0.587 a (0.432, 0.741) | 0.012 (−0.013, 0.036) | 0.363 a (0.211, 0.515) | 0.038 (−0.016, 0.095) |
| ISU Only | 0.270 b (0.116, 0.425) | 0.137 c (0.012, 0.263) | 0.116 c (0.014, 0.217) | 0.477 a (0.299, 0.654) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, H.K.; Mannan, H.; Hay, P. Exploring Relationships between Recurrent Binge Eating and Illicit Substance Use in a Non-Clinical Sample of Women over Two Years. Behav. Sci. 2017, 7, 46. https://doi.org/10.3390/bs7030046
Lu HK, Mannan H, Hay P. Exploring Relationships between Recurrent Binge Eating and Illicit Substance Use in a Non-Clinical Sample of Women over Two Years. Behavioral Sciences. 2017; 7(3):46. https://doi.org/10.3390/bs7030046
Chicago/Turabian StyleLu, Henry Kewen, Haider Mannan, and Phillipa Hay. 2017. "Exploring Relationships between Recurrent Binge Eating and Illicit Substance Use in a Non-Clinical Sample of Women over Two Years" Behavioral Sciences 7, no. 3: 46. https://doi.org/10.3390/bs7030046




