Investigating the Effects of Seizures on Procedural Memory Performance in Patients with Epilepsy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
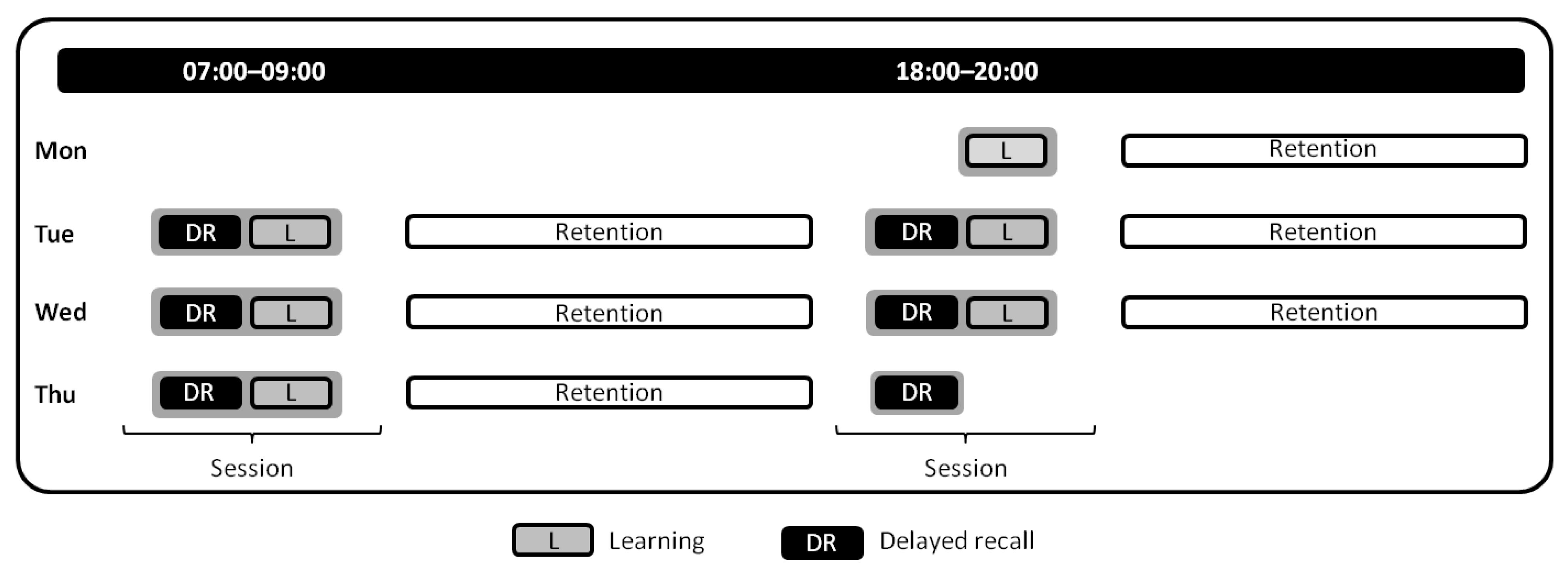
2.2. Study Protocol
2.3. Instruments
2.3.1. Epilepsy Monitoring
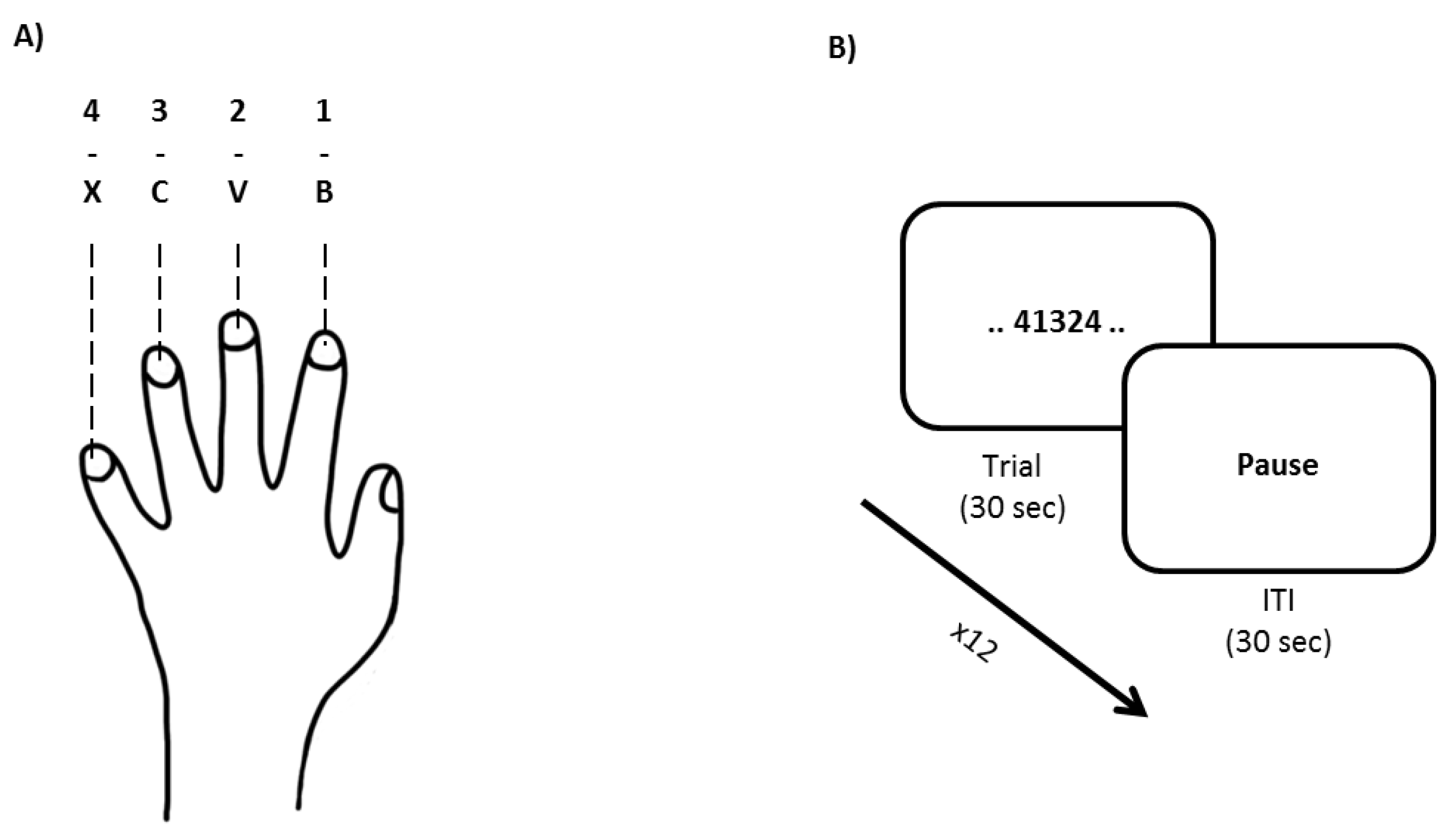
2.3.2. Procedural Memory-Motor Sequence Learning Task
2.4. Analyses
3. Results
3.1. Patient Demographics and Baseline Descriptive
3.2. Confounding Factors
3.3. Seizure Occurrence
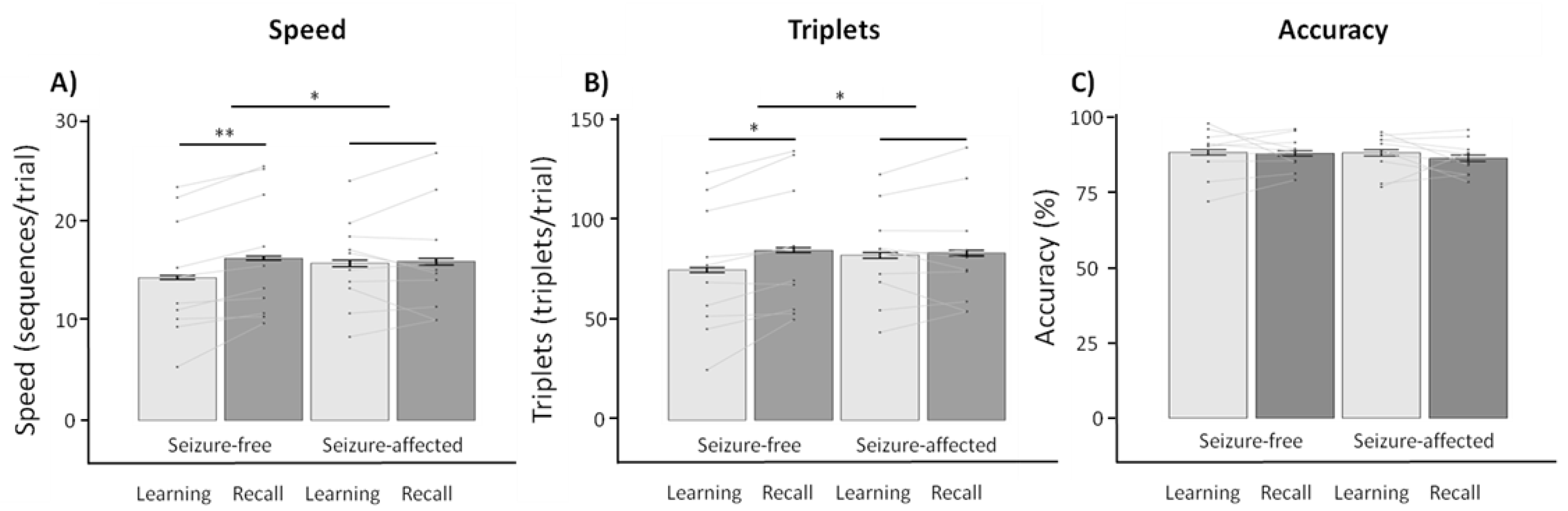
3.4. Behavioral Within-Subject Contrasts
3.4.1. Seizure-Free vs. Seizure-Affected Retention Periods
3.4.2. Seizure-Free Day vs. Seizure-Free Night
3.5. Exploratory Within-Subject Contrasts in Patients with Temporal Lobe Epilepsy
3.6. Between-Subjects Contrasts
4. Discussion
4.1. General Discussion
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tramoni-Negre, E.; Lambert, I.; Bartolomei, F.; Felician, O. Long-term memory deficits in temporal lobe epilepsy. Rev. Neurol. 2017, 173, 490–497. [Google Scholar] [CrossRef] [PubMed]
- McAuley, J.W.; Elliott, J.O.; Patankar, S.; Hart, S.; Long, L.; Moore, J.L.; Shneker, B.F. Comparing patients’ and practitioners’ views on epilepsy concerns: A call to address memory concerns. Epilepsy Behav. 2010, 19, 580–583. [Google Scholar] [CrossRef]
- Giovagnoli, A.R.; Avanzini, G. Quality of life and memory performance in patients with temporal lobe epilepsy. Acta Neurol. Scand. 2000, 101, 295–300. [Google Scholar] [CrossRef]
- Langfitt, J.T.; Westerveld, M.; Hamberger, M.J.; Walczak, T.S.; Cicchetti, D.V.; Berg, A.T.; Vickrey, B.G.; Barr, W.B.; Sperling, M.R.; Masur, D.; et al. Worsening of quality of life after epilepsy surgery: Effect of seizures and memory decline. Neurology 2007, 68, 1988–1994. [Google Scholar] [CrossRef]
- Fitzgerald, Z.; Thayer, Z.; Mohamed, A.; Miller, L.A. Examining factors related to accelerated long-term forgetting in epilepsy using ambulatory EEG monitoring. Epilepsia 2013, 54, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, H.; Holdstock, J.S.; Baker, G.; Herbert, A.; Clague, F.; Downes, J.J. Long-term accelerated forgetting of verbal and non-verbal information in temporal lobe epilepsy. Cortex 2012, 48, 317–332. [Google Scholar] [CrossRef]
- Mameniskiene, R.; Jatuzis, D.; Kaubrys, G.; Budrys, V. The decay of memory between delayed and long-term recall in patients with temporal lobe epilepsy. Epilepsy Behav. 2006, 8, 278–288. [Google Scholar] [CrossRef] [PubMed]
- Butler, C.R.; Zeman, A.Z. Recent insights into the impairment of memory in epilepsy: Transient epileptic amnesia, accelerated long-term forgetting and remote memory impairment. Brain 2008, 131 (Pt 9), 2243–2263. [Google Scholar] [CrossRef] [Green Version]
- Delaney, R.C.; Rosen, A.J.; Mattson, R.H.; Novelly, R.A. Memory function in focal epilepsy: A comparison of non-surgical, unilateral temporal lobe and frontal lobe samples. Cortex 1980, 16, 103–117. [Google Scholar] [CrossRef]
- Muhlert, N.; Grunewald, R.A.; Hunkin, N.M.; Reuber, M.; Howell, S.; Reynders, H.; Isaac, C.L. Accelerated long-term forgetting in temporal lobe but not idiopathic generalised epilepsy. Neuropsychologia 2011, 49, 2417–2426. [Google Scholar] [CrossRef]
- Scoville, W.B.; Milner, B. Loss of Recent Memory after Bilateral Hippocampal Lesions. J. Neurol. Neurosurg. Psychiatry 1957, 20, 11–21. [Google Scholar] [CrossRef] [Green Version]
- Milner, B. Disorders of learning and memory after temporal lobe lesions in man. Clin. Neurosurg. 1972, 19, 421–446. [Google Scholar] [CrossRef] [PubMed]
- Squire, L.R. Declarative and nondeclarative memory: Multiple brain systems supporting learning and memory. J. Cogn. Neurosci. 1992, 4, 232–243. [Google Scholar] [CrossRef] [PubMed]
- Albouy, G.; Sterpenich, V.; Balteau, E.; Vandewalle, G.; Desseilles, M.; Dang-Vu, T.; Darsaud, A.; Ruby, P.; Luppi, P.H.; Degueldre, C.; et al. Both the hippocampus and striatum are involved in consolidation of motor sequence memory. Neuron 2008, 58, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Albouy, G.; King, B.R.; Maquet, P.; Doyon, J. Hippocampus and striatum: Dynamics and interaction during acquisition and sleep-related motor sequence memory consolidation. Hippocampus 2013, 23, 985–1004. [Google Scholar] [CrossRef]
- King, B.R.; Hoedlmoser, K.; Hirschauer, F.; Dolfen, N.; Albouy, G. Sleeping on the motor engram: The multifaceted nature of sleep-related motor memory consolidation. Neurosci. Biobehav. Rev. 2017, 80, 1–22. [Google Scholar] [CrossRef]
- Doyon, J.; Gabitov, E.; Vahdat, S.; Lungu, O.; Boutin, A. Current issues related to motor sequence learning in humans. Curr. Opin. Behav. Sci. 2018, 20, 89–97. [Google Scholar] [CrossRef]
- Schapiro, A.C.; Reid, A.G.; Morgan, A.; Manoach, D.S.; Verfaellie, M.; Stickgold, R. The hippocampus is necessary for the consolidation of a task that does not require the hippocampus for initial learning. Hippocampus 2019, 29, 1091–1100. [Google Scholar] [CrossRef]
- Albouy, G.; Fogel, S.; King, B.R.; Laventure, S.; Benali, H.; Karni, A.; Carrier, J.; Robertson, E.M.; Doyon, J. Maintaining vs. enhancing motor sequence memories: Respective roles of striatal and hippocampal systems. Neuroimage 2015, 108, 423–434. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Ruiz, A.; Oliva, A.; Fermino de Oliveira, E.; Rocha-Almeida, F.; Tingley, D.; Buzsaki, G. Long-duration hippocampal sharp wave ripples improve memory. Science 2019, 364, 1082–1086. [Google Scholar] [CrossRef] [PubMed]
- Gelinas, J. Ripples for memory retrieval in humans. Science 2019, 363, 927–928. [Google Scholar] [CrossRef] [PubMed]
- Gelinas, J.N.; Khodagholy, D.; Thesen, T.; Devinsky, O.; Buzsaki, G. Interictal epileptiform discharges induce hippocampal-cortical coupling in temporal lobe epilepsy. Nat. Med. 2016, 22, 641–648. [Google Scholar] [CrossRef] [Green Version]
- Girardeau, G.; Benchenane, K.; Wiener, S.I.; Buzsaki, G.; Zugaro, M.B. Selective suppression of hippocampal ripples impairs spatial memory. Nat. Neurosci. 2009, 12, 1222–1223. [Google Scholar] [CrossRef] [PubMed]
- Halász, P.; Bódizs, R.; Ujma, P.P.; Fabo, D.; Szucs, A. Strong relationship between NREM sleep, epilepsy and plastic functions—A conceptual review on the neurophysiology background. Epilepsy Res. 2019, 150, 95–105. [Google Scholar] [CrossRef]
- Halász, P.; Ujma, P.P.; Fabo, D.; Bódizs, R.; Szucs, A. Epilepsy as a derailment of sleep plastic functions may cause chronic cognitive impairment—A theoretical review. Sleep Med. Rev. 2019, 45, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Helmstaedter, C. Effects of chronic epilepsy on declarative memory systems. Prog. Brain Res. 2002, 135, 439–453. [Google Scholar] [CrossRef]
- Ricci, M.; Mohamed, A.; Savage, G.; Boserio, J.; Miller, L.A. The impact of epileptiform abnormalities and hippocampal lesions on retention of recent autobiographical experiences: Adding insult to injury? Neuropsychologia 2015, 66, 259–266. [Google Scholar] [CrossRef]
- Jokeit, H.; Daamen, M.; Zang, H.; Janszky, J.; Ebner, A. Seizures accelerate forgetting in patients with left-sided temporal lobe epilepsy. Neurology 2001, 57, 125–126. [Google Scholar] [CrossRef] [PubMed]
- Horak, P.C.; Meisenhelter, S.; Song, Y.; Testorf, M.E.; Kahana, M.J.; Viles, W.D.; Bujarski, K.A.; Connolly, A.C.; Robbins, A.A.; Sperling, M.R.; et al. Interictal epileptiform discharges impair word recall in multiple brain areas. Epilepsia 2017, 58, 373–380. [Google Scholar] [CrossRef] [Green Version]
- Ricci, M.; Mohamed, A.; Savage, G.; Miller, L.A. Disruption of learning and long-term retention of prose passages in patients with focal epilepsy. Epilepsy Behav. 2015, 51, 104–111. [Google Scholar] [CrossRef]
- van Schalkwijk, F.J.; Ricci, M.; Nikpour, A.; Miller, L.A. The impact of sleep characteristics and epilepsy variables on memory performance in patients with focal seizures. Epilepsy Behav. 2018, 87, 152–158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Long, J.; Feng, Y.; Liao, H.; Zhou, Q.; Urbin, M.A. Motor Sequence Learning Is Associated With Hippocampal Subfield Volume in Humans With Medial Temporal Lobe Epilepsy. Front. Hum. Neurosci. 2018, 12, 367. [Google Scholar] [CrossRef] [Green Version]
- Höller, Y.; Höhn, C.; Schwimmbeck, F.; Plancher, G.; Trinka, E. Effects of Antiepileptic Drug Tapering on Episodic Memory as Measured by Virtual Reality Tests. Front. Neurol. 2020, 11, 93. [Google Scholar] [CrossRef] [PubMed]
- Höller, Y.; Höhn, C.; Schwimmbeck, F.; Plancher, G.; Trinka, E. A virtual reality paradigm to assess episodic memory: Validation-dataset for six parallel versions and a structured behavioral assessment. Data Brief 2020, 29, 105279. [Google Scholar] [CrossRef]
- Walker, M.P.; Brakefield, T.; Morgan, A.; Hobson, J.A.; Stickgold, R. Practice with sleep makes perfect: Sleep-dependent motor skill learning. Neuron 2002, 35, 205–211. [Google Scholar] [CrossRef] [Green Version]
- Friedrich, S.; Konietschke, F.; Pauly, M. MANOVA.RM: Resampling-Based Analysis of Multivariate Data and Repeated Measures Designs; R-Package Version 0.4.2. 2020. Available online: https://github.com/smn74/MANOVA.RM (accessed on 1 February 2021).
- Torchiano, M. Efficient Effect Size Computation; R-Package Version 0.8.0. 2017. Available online: https://github.com/mtorchiano/effsize/ (accessed on 8 September 2020).
- Ung, H.; Cazares, C.; Nanivadekar, A.; Kini, L.; Wagenaar, J.; Becker, D.; Krieger, A.; Lucas, T.; Litt, B.; Davis, K.A. Interictal epileptiform activity outside the seizure onset zone impacts cognition. Brain 2017, 140, 2157–2168. [Google Scholar] [CrossRef] [Green Version]
- Deak, M.C.; Stickgold, R.; Pietras, A.C.; Nelson, A.P.; Bubrick, E.J. The role of sleep in forgetting in temporal lobe epilepsy: A pilot study. Epilepsy Behav. 2011, 21, 462–466. [Google Scholar] [CrossRef] [Green Version]
- Moroni, F.; Nobili, L.; Curcio, G.; De Carli, F.; Tempesta, D.; Marzano, C.; De Gennaro, L.; Mai, R.; Francione, S.; Lo Russo, G.; et al. Procedural learning and sleep hippocampal low frequencies in humans. Neuroimage 2008, 42, 911–918. [Google Scholar] [CrossRef]
- Nishida, M.; Walker, M.P. Daytime naps, motor memory consolidation and regionally specific sleep spindles. PLoS ONE 2007, 2, e341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doyon, J.; Korman, M.; Morin, A.; Dostie, V.; Hadj Tahar, A.; Benali, H.; Karni, A.; Ungerleider, L.G.; Carrier, J. Contribution of night and day sleep vs. simple passage of time to the consolidation of motor sequence and visuomotor adaptation learning. Exp. Brain Res. 2009, 195, 15–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motamedi, G.K.; Meador, K.J. Antiepileptic drugs and memory. Epilepsy Behav. 2004, 5, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Dinkelacker, V.; Xin, X.; Baulac, M.; Samson, S.; Dupont, S. Interictal epileptic discharge correlates with global and frontal cognitive dysfunction in temporal lobe epilepsy. Epilepsy Behav. 2016, 62, 197–203. [Google Scholar] [CrossRef]
- Faught, E.; Karakis, I.; Drane, D.L. The Impact of Interictal Discharges on Performance. Curr. Neurol. Neurosci. Rep. 2018, 18, 88. [Google Scholar] [CrossRef]
- Brown, R.M.; Robertson, E.M. Inducing motor skill improvements with a declarative task. Nat. Neurosci. 2007, 10, 148–149. [Google Scholar] [CrossRef] [Green Version]
- Bazil, C.W.; Castro, L.H.; Walczak, T.S. Reduction of rapid eye movement sleep by diurnal and nocturnal seizures in temporal lobe epilepsy. Arch. Neurol. 2000, 57, 363–368. [Google Scholar] [CrossRef]
- Maganti, R.; Sheth, R.D.; Hermann, B.P.; Weber, S.; Gidal, B.E.; Fine, J. Sleep architecture in children with idiopathic generalized epilepsy. Epilepsia 2005, 46, 104–109. [Google Scholar] [CrossRef]
- Bazil, C.W. Nocturnal seizures and the effects of anticonvulsants on sleep. Curr. Neurol. Neurosci. Rep. 2008, 8, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Clemens, B.; Menes, A. Sleep spindle asymmetry in epileptic patients. Clin. Neurophysiol. 2000, 111, 2155–2159. [Google Scholar] [CrossRef]
- Höller, Y.; Trinka, E. Is There a Relation between EEG-Slow Waves and Memory Dysfunction in Epilepsy? A Critical Appraisal. Front. Hum. Neurosci. 2015, 9, 341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lambert, I.; Tramoni-Negre, E.; Lagarde, S.; Roehri, N.; Giusiano, B.; Trebuchon-Da Fonseca, A.; Carron, R.; Benar, C.G.; Felician, O.; Bartolomei, F. Hippocampal Interictal Spikes during Sleep Impact Long-Term Memory Consolidation. Ann. Neurol. 2020, 87, 976–987. [Google Scholar] [CrossRef]

| Demographics | |
|---|---|
| Age (M ± SD) | 32.92 ± 13.80 |
| Gender (M/F) | 23/30 |
| Epilepsy characteristics | |
| Epilepsy Type | |
| Focal | 43 |
| Generalized | 10 |
| Location | |
| Frontal | 8 |
| Temporal | 14 |
| Occipital | 2 |
| Bifrontal | 2 |
| Fronto-central | 1 |
| Fronto-temporal | 5 |
| Fronto-centro-parietal | 1 |
| Temporo-mesial | 3 |
| Parieto-occipital | 1 |
| Unclear | 16 |
| Lateralization | |
| Left | 20 |
| Right | 12 |
| Bilateral | 8 |
| Unclear | 13 |
| Learning | Recall | ||||
|---|---|---|---|---|---|
| Speed | M ± SD | M ± SD | Z | p | |
| Seizure-free retention | 14.61 ± 5.14 | 16.10 ± 5.43 | −2.897 | 0.048 * | |
| Seizure-affected retention | 15.65 ± 3.84 | 16.66 ± 5.29 | −0.816 | 1.000 | |
| Z | −1.619 | −1.108 | |||
| p | 0.954 | 1.000 | |||
| Triplets | |||||
| Seizure-free retention | 76.66 ± 27.38 | 84.78 ± 28.17 | −2.811 | 0.055 + | |
| Seizure-affected retention | 82.42 ± 20.36 | 87.48 ± 26.36 | −0.909 | 1.000 | |
| Z | −1.675 | −1.221 | |||
| p | 0.940 | 1.000 | |||
| Accuracy | |||||
| Seizure-free retention | 88.21 ± 7.14 | 87.16 ± 6.56 | −0.426 | 1.000 | |
| Seizure-affected retention | 87.35 ± 6.28 | 87.44 ± 5.22 | −0.085 | 1.000 | |
| Z | −0.628 | −0.199 | |||
| p | 1.000 | 1.000 |
| Learning | Recall | ||||
|---|---|---|---|---|---|
| Speed | M ± SD | M ± SD | Z | p | |
| Seizure-free retention | 13.18 ± 4.77 | 14.03 ± 5.50 | −2.093 | 0.324 | |
| Seizure-affected retention | 13.77 ± 4.55 | 14.58 ± 5.67 | −2.732 | 0.066 + | |
| Z | −1.663 | −1.309 | |||
| p | 0.672 | 0.905 | |||
| Triplets | |||||
| Seizure-free retention | 69.35 ± 24.10 | 74.53 ± 28.20 | −2.651 | 0.080 + | |
| Seizure-affected retention | 71.75 ± 23.23 | 76.75 ± 28.03 | −3.282 | 0.012 * | |
| Z | −1.200 | −1.575 | |||
| p | 0.905 | 0.690 | |||
| Accuracy | |||||
| Seizure-free retention | 85.47 ± 7.96 | 84.42 ± 9.95 | −0.313 | 1.000 | |
| Seizure-affected retention | 86.86 ± 8.12 | 85.50 ± 11.77 | −0.025 | 1.000 | |
| Z | −1.901 | −1.338 | |||
| p | 0.456 | 0.905 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Schalkwijk, F.J.; Gruber, W.R.; Miller, L.A.; Trinka, E.; Höller, Y. Investigating the Effects of Seizures on Procedural Memory Performance in Patients with Epilepsy. Brain Sci. 2021, 11, 261. https://doi.org/10.3390/brainsci11020261
van Schalkwijk FJ, Gruber WR, Miller LA, Trinka E, Höller Y. Investigating the Effects of Seizures on Procedural Memory Performance in Patients with Epilepsy. Brain Sciences. 2021; 11(2):261. https://doi.org/10.3390/brainsci11020261
Chicago/Turabian Stylevan Schalkwijk, Frank J., Walter R. Gruber, Laurie A. Miller, Eugen Trinka, and Yvonne Höller. 2021. "Investigating the Effects of Seizures on Procedural Memory Performance in Patients with Epilepsy" Brain Sciences 11, no. 2: 261. https://doi.org/10.3390/brainsci11020261






