Implementation of Machine Learning Software on the Radiology Worklist Decreases Scan View Delay for the Detection of Intracranial Hemorrhage on CT
Abstract
1. Introduction
2. Materials and Methods
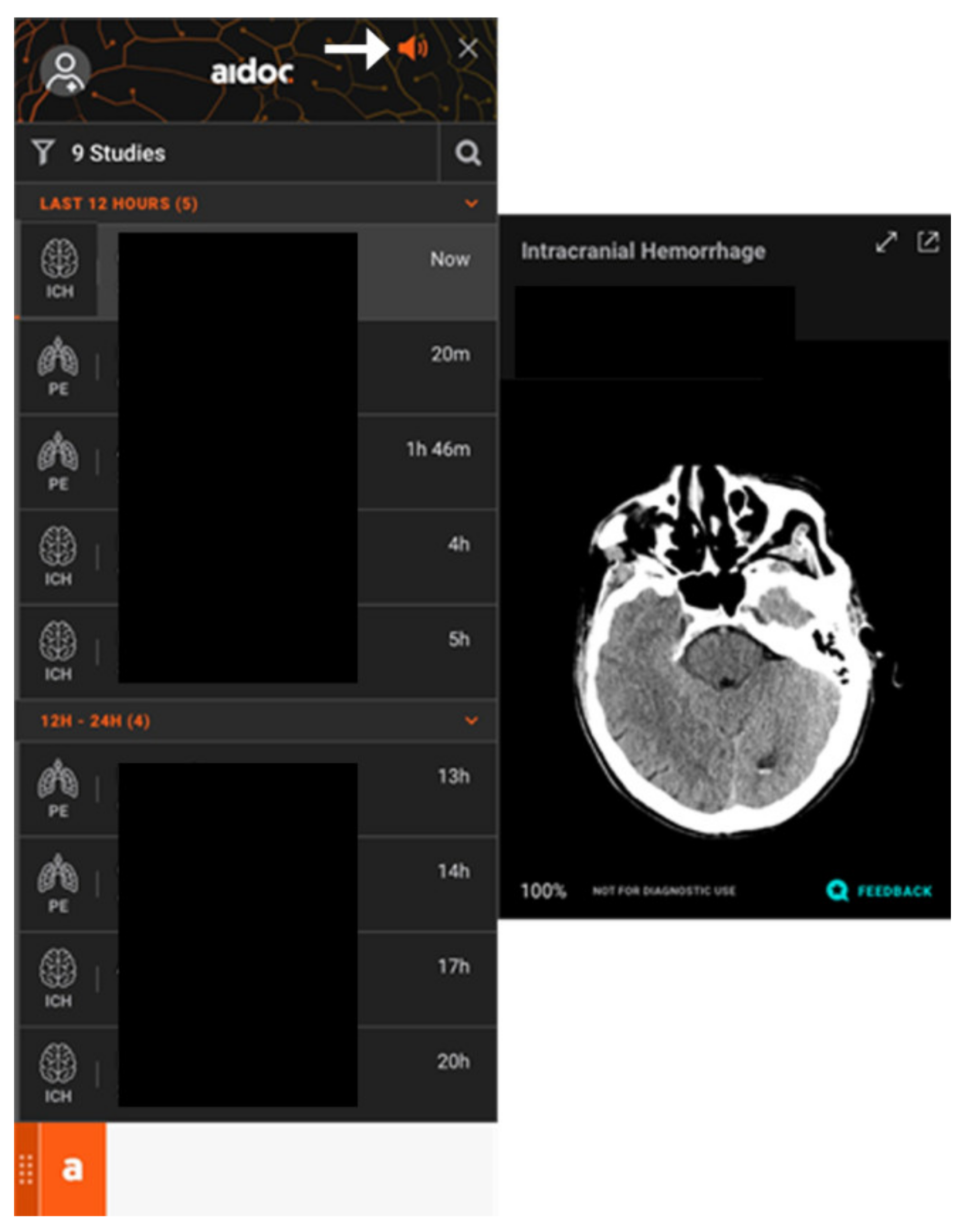
2.1. Artificial Intelligence System
2.2. Software Integration and Deployment
2.3. Dataset
2.4. Analysis
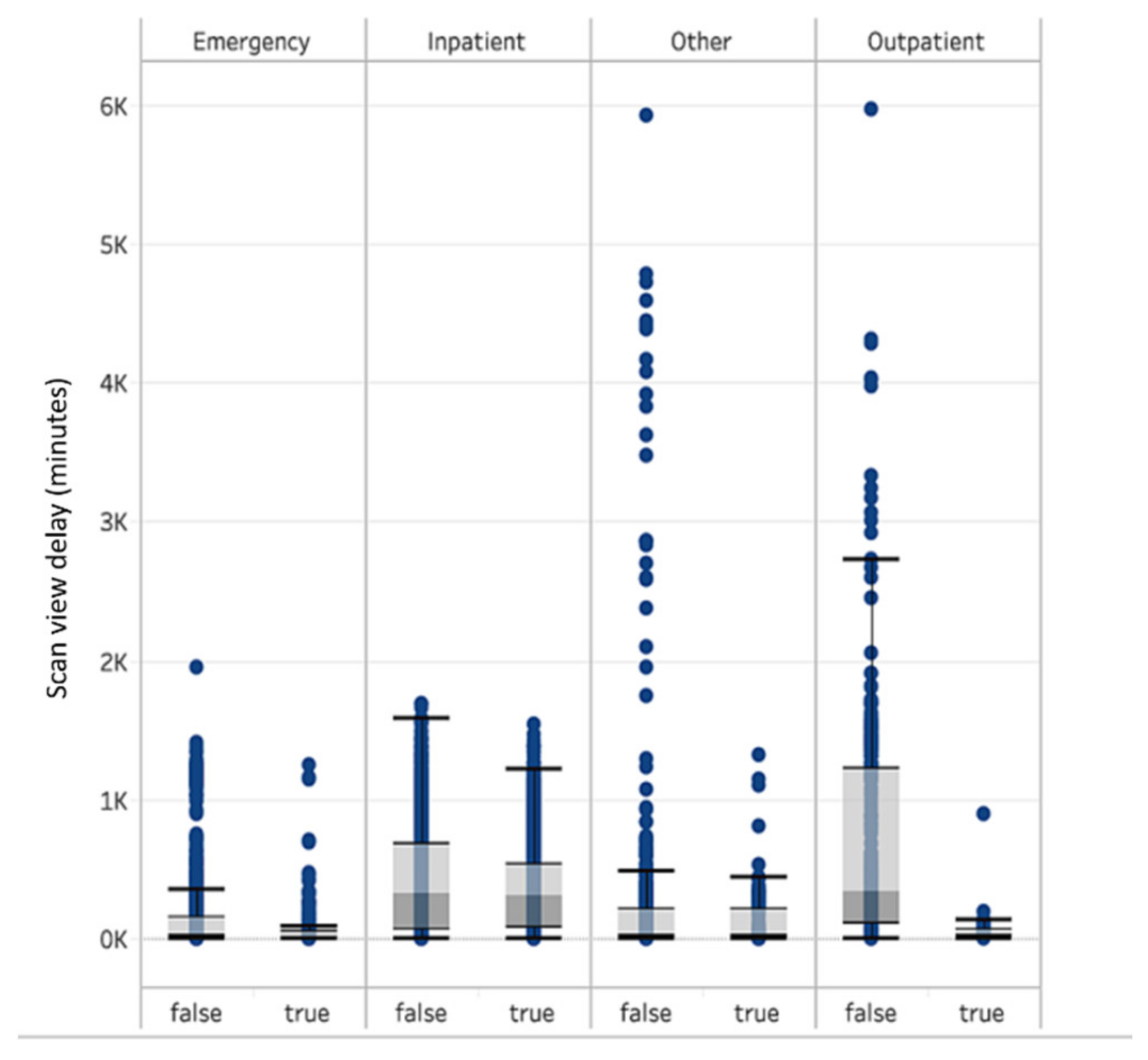
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Carter, J.A.; Curry, W. Intracerebral Hemorrhage: Pathophysiology and Management for Generalists. Hosp. Med. Clin. 2017, 6, 95–111. [Google Scholar] [CrossRef][Green Version]
- Elliott, J.; Smith, M. The Acute Management of Intracerebral Hemorrhage: A Clinical Review. Anesth. Analg. 2010, 110, 1419–1427. [Google Scholar] [CrossRef] [PubMed]
- Fujitsu, K.; Muramoto, M.; Ikeda, Y.; Inada, Y.; Kim, I.; Kuwabara, T. Indications for surgical treatment of putaminal hemorrhage. J. Neurosurg. 1990, 73, 518–525. [Google Scholar] [CrossRef] [PubMed]
- McDonald, R.J.; Schwartz, K.M.; Eckel, L.J.; Diehn, F.E.; Hunt, C.H.; Bartholmai, B.J.; Erickson, B.J.; Kallmes, D.F. The Effects of Changes in Utilization and Technological Advancements of Cross-Sectional Imaging on Radiologist Workload. Acad. Radiol. 2015, 22, 1191–1198. [Google Scholar] [CrossRef] [PubMed]
- Sasank Chilamkurthy, B.; Rohit Ghosh, B.; Swetha Tanamala, M.; Mustafa Biviji, D.N.B.; Campeau, N.G.; Venugopal, V.K.; Mahajan, V.; Rao, P.; Warier, P. Deep learning algorithms for detection of critical findings in head CT scans: A retrospective study. Lancet 2018, 392, 2388–2396. [Google Scholar] [CrossRef]
- Ojeda, P.; Zawaideh, M.; Mossa-Basha, M.; Haynor, D. The Utility of Deep Learning: Evaluation of a Convolutional Neural Network for Detection of Intracranial Bleeds on Non-Contrast Head Computed Tomography Studies. SPIE Medical Imaging. In Proceedings of the Medical Imaging 2019: Image Processing, San Diego, CA, USA, 16–21 February 2019; Volume 10949, p. 109493J. [Google Scholar]
- Ginat, D.T. Analysis of head CT scans flagged by deep learning software for acute intracranial hemorrhage. Neuroradiology 2020, 62, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Arbabshirani, M.R.; Fornwalt, B.K.; Mongelluzzo, G.J.; Suever, J.D.; Geise, B.D.; Patel, A.A.; Moore, G.J. Advanced machine learning in action: Identification of intracranial hemorrhage on computed tomography scans of the head with clinical workflow integration. NPJ Digit. Med. 2018, 1, 9. [Google Scholar] [CrossRef] [PubMed]
- Buls, N.; Watté, N.; Nieboer, K.; Ilsen, B.; de Mey, J. Performance of an artificial intelligence tool with real-time clinical workflow in-tegration—Detection of intracranial hemorrhage and pulmonary embolism. Phys. Med. 2021, 83, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Titano, J.J.; Badgeley, M.; Schefflein, J.; Pain, M.; Su, A.; Cai, M.; Swinburne, N.; Zech, J.; Kim, J.; Bederson, J.; et al. Automated deep-neural-network surveillance of cranial images for acute neurologic events. Nat. Med. 2018, 24, 1337–1341. [Google Scholar] [CrossRef] [PubMed]
- Rao, B.; Zohrabian, V.; Cedeno, P.; Saha, A.; Pahade, J.; Davis, M.A. Utility of Artificial Intelligence Tool as a Prospective Radiology Peer Reviewer—Detection of Unreported Intracranial Hemorrhage. Acad. Radiol. 2021, 28, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.A.; Rao, B.; Cedeno, P.A.; Saha, A.; Zohrabian, V.M. Machine Learning and Improved Quality Metrics in Acute Intracranial Hemorrhage by Noncontrast Computed Tomography. Curr. Probl. Diagn. Radiol. 2020, S0363-0188(20)30208-5. [Google Scholar]
- Rathnayake, S.; Nautsch, F.; Goodman, T.R.; Forman, H.P.; Gunabushanam, G. Effect of Radiology Study Flow on Report Turna-round Time. AJR Am. J. Roentgenol. 2017, 209, 1308–1311. [Google Scholar] [CrossRef] [PubMed]
- Stern, C.; Boehm, T.; Seifert, B.; Kawel-Boehm, N. Subspecialized Radiological Reporting Expedites Turnaround Time of Radiology Reports and Increases Productivity. Subspezialisierte Befundung beschleunigt die Befunddurchlaufzeit radiologischer Berich-te und steigert die Produktivität. Rofo 2018, 190, 623–629. [Google Scholar] [PubMed]
- Glover, M., 4th; Almeida, R.R.; Schaefer, P.W.; Lev, M.H.; Mehan, W.A., Jr. Quantifying the Impact of Noninterpretive Tasks on Radiology Report Turn-Around Times. J. Am. Coll. Radiol. 2017, 14, 1498–1503. [Google Scholar] [CrossRef] [PubMed]
| Emergency | Inpatient | Other | Outpatient | |||||
|---|---|---|---|---|---|---|---|---|
| Negative | Positive | Negative | Positive | Negative | Positive | Negative | Positive | |
| Number of scans | 3398 | 201 | 2130 | 1457 | 987 | 132 | 379 | 39 |
| Median scan view time delay (minutes) | 16 | 14 | 298 | 298 | 14 | 18 | 326 | 35 |
| Average scan view time delay (minutes) | 85 | 72 | 390 | 352 | 167 | 109 | 674 | 70 |
| Standard deviation (minutes) | 194 | 177 | 368 | 315 | 572 | 217 | 825 | 141 |
| Sensitivity | 88.4% (95% confidence interval: 87.88% to 89.82%) |
| Specificity | 96.1% (95% confidence interval: 95.65% to 96.52%) |
| Positive Predictive Value | 85.9% (95% confidence interval: 84.36% to 87.34%) |
| Negative Predictive Value | 96.3% (95% confidence interval: 95.86% to 96.71%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ginat, D. Implementation of Machine Learning Software on the Radiology Worklist Decreases Scan View Delay for the Detection of Intracranial Hemorrhage on CT. Brain Sci. 2021, 11, 832. https://doi.org/10.3390/brainsci11070832
Ginat D. Implementation of Machine Learning Software on the Radiology Worklist Decreases Scan View Delay for the Detection of Intracranial Hemorrhage on CT. Brain Sciences. 2021; 11(7):832. https://doi.org/10.3390/brainsci11070832
Chicago/Turabian StyleGinat, Daniel. 2021. "Implementation of Machine Learning Software on the Radiology Worklist Decreases Scan View Delay for the Detection of Intracranial Hemorrhage on CT" Brain Sciences 11, no. 7: 832. https://doi.org/10.3390/brainsci11070832
APA StyleGinat, D. (2021). Implementation of Machine Learning Software on the Radiology Worklist Decreases Scan View Delay for the Detection of Intracranial Hemorrhage on CT. Brain Sciences, 11(7), 832. https://doi.org/10.3390/brainsci11070832





