Exploring Methodological Issues in Mental Practice for Upper-Extremity Function Following Stroke-Related Paralysis: A Scoping Review
Abstract
1. Introduction
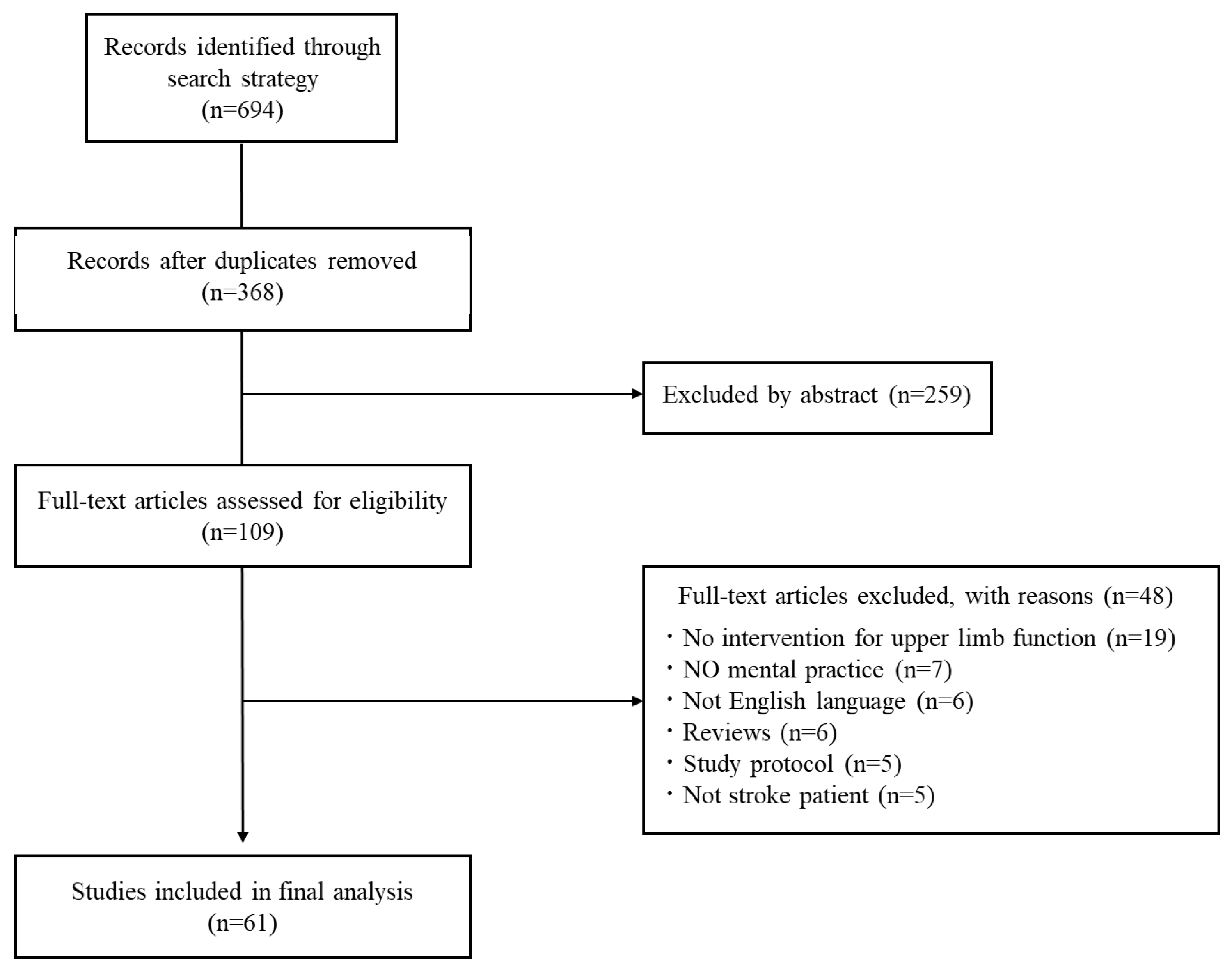
2. Materials and Methods
- Step 1: Identifying the research question
- Step 2: Identifying relevant studies
- Step 3: Study selection
- Step 4: Data extraction and analysis
3. Results
- (1)
- When is the most common time to start an MP intervention for post-stroke paralytic side upper-limb function after stroke?
- (2)
- What is the MP load (intervention time, number of intervention days, and intervention period)?
| No. | Author/Year | Paper Title | Evidence Level/ Study Design | Time Taken to Start Mental Practice Intervention after Stroke Onset | MP Combination | MP Intervention |
|---|---|---|---|---|---|---|
| 1 | Park et al. (2022) [24] | The effects of task-oriented mental practice on upper limb function and coordination in chronic stroke patients Randomized controlled trial design | 2B/RCT | 72.22 ± 20.37 months | Traditional rehabilitation | Time taken per intervention: 5 min Intervention frequency per week: 5/W Total intervention period: 3 weeks |
| 2 | Xiong et al. (2021) [26] | Motor imagery training reduces contralesional compensation in stroke patients with moderate to severe upper limb impairment | 3B/One group, nonrandomized | 112.08 ± 37.87 days | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 3 | Qian Hu et al. (2021) [34] | Motor imagery-based brain-computer interface combined with multimodal feedback to promote upper limb motor function after stroke: A preliminary study | 2B/RCT | 7.9 ± 6.5 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: None Total intervention period: performed only once |
| 4 | Liepert et al. (2020) [35] | Effects of a single mental chronometry training session in subacute stroke patients—a randomized controlled trial | 3B/One group, nonrandomized | 2.1 ± 1.1 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: None Total intervention period: performed only once |
| 5 | Page et al. (2021) [36] | Multimodal Mental Practice Versus Repetitive Task Practice Only to Treat Chronic Stroke: A Randomized Controlled Pilot Study | 2B/RCT | 1.9 ± 2.5 months | Traditional rehabilitation | Time taken per intervention: 45 min Intervention frequency per week: 3/W Total intervention period: 10 weeks |
| 6 | Kang et al. (2021) [23] | The effects of additional electrical stimulation combined with repetitive transcranial magnetic stimulation and motor imagery on upper extremity motor recovery in the subacute period after stroke | 2B/Tow group, nonrandomized | 24.13 ± 12.4 days | Traditional rehabilitation | Time taken per intervention: 20 min Intervention frequency per week: 5/W Total intervention period: 2 weeks |
| 7 | Ji et al. (2021) [14] | Graded motor imagery training as a home exercise program for upper limb motor function in patients with chronic stroke A randomized controlled trial | 2B/RCT | 46.29 ± 40.96 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 7/W Total intervention period: 8 weeks |
| 8 | Wang et al. (2020) [28] | Motor Imagery Training After Stroke Increases Slow-5 Oscillations and Functional Connectivity in the Ipsilesional Inferior Parietal Lobule. | 2B/RCT | 121.19 ± 37.33 days | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 9 | Nam et al. (2019) [37] | Effects of adjuvant mental practice using inverse video of the unaffected upper limb in subacute stroke: a pilot randomized controlled study. | 2B/RCT | 67.4 ± 43.7 months | Traditional rehabilitation | Time taken per intervention: 20 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 10 | Kim et al. (2018) [6] | The effects of mental practice combined with modified constraint-induced therapy on corticospinal excitability, movement quality, function, and activities of daily living in persons with stroke. | 2B/RCT | 41 months (range: 8–120) | Traditional rehabilitation | Time taken per intervention: 10 min Intervention frequency per week: 5/W Total intervention period: 2 weeks |
| 11 | Chowdhury et al. (2018) [38] | Active Physical Practice Followed by Mental Practice Using BCI-Driven Hand Exoskeleton: A Pilot Trial for Clinical Effectiveness and Usability. | 3B/One group, nonrandomized | 7 ± 1.1 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 2–3/WTotal intervention period: 6 weeks |
| 12 | Kawakami et al. (2018) [39] | Change in Reciprocal Inhibition of the Forearm with Motor Imagery among Patients with Chronic Stroke. | 3B/One group, nonrandomized | 30.5 months (range 9~180) | Traditional rehabilitation | Time taken per intervention: 45 min Intervention frequency per week: 5/W Total intervention period: 10 days |
| 13 | Fang et al. (2018) [31] | Motor imagery training induces changes in brain neural networks in stroke patient | 2B/RCT | 1.8 ± 0.7 months | Traditional rehabilitation | Time taken per intervention: 45 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 14 | Azad et al. (2018) [40] | Effect of motor imagery training with sensory feedback on sensory-motor function of the upper extremity in patients with chronic stroke | 2B/Tow group, nonrandomized | None | Traditional rehabilitation | Time taken per intervention: None Intervention frequency per week: None Total intervention period: None |
| 15 | Park et al. (2017) [27] | Effects of mental practice combined with electromyogram-triggered electrical stimulation for upper extremity function in stroke patients | 2B/Tow group, nonrandomized | None | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 16 | Iso at al. (2016) [41] | Effect of mental practice using inverse video of the unaffected upper limb in a subject with chronic hemiparesis after stroke | 4/Case study | 5 years | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 6 weeks |
| 17 | Park et al. (2016) [42] | Influence of mental practice on upper limb muscle activity and activities of daily living in chronic stroke patients | 4/Case series | 39.5 ± 3.5 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 2 weeks |
| 18 | Park et al. (2016) [43] | The effects of game-based virtual reality movement therapy plus mental practice on upper extremity function in chronic stroke patients with hemiparesis: A randomized controlled trial | 2B/RCT | More than 6 months | VR rehabilitation | Time taken per intervention: 5 min Intervention frequency per week: 5/W Total intervention period: 2 weeks |
| 19 | Oh et al. (2016) [44] | Effects of Adjuvant Mental Practice on Affected Upper Limb Function Following a Stroke: Results of Three-Dimensional Motion Analysis, Fugl-Meyer Assessment of the Upper Extremity and Motor Activity Log | 2B/Tow group, nonrandomized | 128.1 ± 26.05 days | Traditional rehabilitation | Time taken per intervention: 20 min Intervention frequency per week: 3/W Total intervention period: 3 weeks |
| 20 | Page et al. (2016) [45] | Retention of the spacing effect with mental practice in hemiparetic stroke. | 2B/RCT | 1041.5 ± 999.8 days | Traditional rehabilitation | Time taken per intervention: 60 min Intervention frequency per week: 3/W Total intervention period: 10 weeks |
| 21 | Cha et al. (2015) [46] | Effects of mental practice with action observation training on occupational performance after stroke. | 4/Case series | 25.3 ± 14 months | Traditional rehabilitation | Time taken per intervention: 4 min Intervention frequency per week: None Total intervention period: 20 times |
| 22 | Morone et al. (2015) [47] | Proof of principle of a brain-computer interface approach to support poststroke arm rehabilitation in hospitalized patients: design, acceptability, and usability. | 3B/One group, nonrandomized | 24.3 ± 21.1 days | MP only | Time taken per intervention: 30 min Intervention frequency per week: 3/W Total intervention period: 4 weeks |
| 23 | Page et al. (2015) [13] | Mental Practice–Triggered Electrical Stimulation in Chronic, Moderate, Upper-Extremity Hemiparesis After Stroke | 4/Case series | 56.5 ± 42.2 months | Electrical stimulation | Time taken per intervention: 60 min Intervention frequency per week: 7/W Total intervention period: 8 weeks |
| 24 | Park et al. (2015) [7] | Effects of mental practice on stroke patients’ upper extremity function and daily activity performance | 2B/RCT | 18 ± 11.7 months | Traditional rehabilitation | Time taken per intervention: 10 min Intervention frequency per week: 5/W Total intervention period: 2 weeks |
| 25 | Park et al. (2015) [48] | The effects of modified constraint-induced therapy combined with mental practice on patients with chronic stroke | 2B/RCT | 15.9 ± 5.8 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 6 weeks |
| 26 | Bajaj et al. (2015) [49] | Functional organization and restoration of the brain motor-execution network after stroke and rehabilitation | 2B/Tow group, nonrandomized | 10.1 ± 13.3 months | Traditional rehabilitation or MP only | Time taken per intervention: 240 min Intervention frequency per week: None Total intervention period: 3 weeks (3600 min) |
| 27 | Kim et al. (2015) [50] | Motor imagery training improves upper extremity performance in stroke patients | 2B/RCT | 8.1 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 3/W Total intervention period: 4 weeks |
| 28 | Hua et al. (2014) [32] | Changes in brain activation in stroke patients after mental practice and physical exercise a functional MRI study | 2B/Tow group, nonrandomized | 1.61 ± 0.8 months | Traditional rehabilitation | Time taken per intervention: 45 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 29 | Oliveira et al. (2014) [51] | Mental practice and mirror therapy associated with conventional physical therapy training on the hemiparetic upper limb in poststroke rehabilitation: a preliminary study. | 3B/One group, nonrandomized | 4.14 ± 1.9 months | Traditional rehabilitation | Time taken per intervention: 25 min Intervention frequency per week: 2/W Total intervention period: 8 weeks |
| 30 | de Assis et al. (2014) [52] | An augmented reality system for upper-limb post-stroke motor rehabilitation: a feasibility study. | 3B/One group, nonrandomized | None | None | Time taken per intervention: 60 min Intervention frequency per week: 1~2/W Total intervention period: 4 weeks |
| 31 | Ji et al. (2014) [53] | Effects of Mental Practice in Conjunction with Repetitive Transcranial Magnetic Stimulation on the Upper Limbs of Sub-acute Stroke Patients | 2B/RCT | 7.81 ± 2.4 months | Traditional rehabilitation | Time taken per intervention: 15 min Intervention frequency per week: 5/W Total intervention period: 6 weeks |
| 32 | Liu et al. (2014) [33] | Mental practice combined with physical practice to enhance hand recovery in stroke patients. | 2B/Tow group, nonrandomized | 1.83 ± 0.6 months | Traditional rehabilitation | Time taken per intervention: 45 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 33 | Sun et al. (2013) [29] | Cortical reorganization after motor imagery training in chronic stroke patients with severe motor impairment: a longitudinal fMRI study. | 2B/RCT | 132.1 ± 27.3 days | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 34 | Clarissa et al. (2013) [54] | The addition of functional task-oriented mental practice to conventional physical therapy improves motor skills in daily functions after stroke. | 4/Case series | 13 ± 6.5 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 3/W Total intervention period: 4 weeks |
| 35 | Mihara et al. (2013) [55] | Near-infrared spectroscopy-mediated neurofeedback enhances efficacy of motor imagery-based training in poststroke victims: a pilot study. | 2B/RCT | 135 ± 38.2 days | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 3/W Total intervention period: 2 weeks |
| 36 | Timmermans et al.(2013) [56] | Effect of mental practice on the improvement of function and daily activity performance of the upper extremity in patients with subacute stroke: a randomized clinical trial. | 2B/RCT | 36.1 ± 27.4 days | MP only | Time taken per intervention: 30 min Intervention frequency per week: 7/W Total intervention period: 6 weeks |
| 37 | Nilsen et al. (2012) [12] | Effect of imagery perspective on occupational performance after stroke: a randomized controlled trial. | 2B/RCT | 43.2 ± 15.4 months | Traditional rehabilitation | Time taken per intervention: 18 min Intervention frequency per week: 2/W Total intervention period: 6 weeks |
| 38 | Braun et al. (2012) [22] | A multicenter randomized controlled trial to compare subacute ‘treatment as usual’ with and without mental practice among persons with stroke in Dutch nursing homes. | 2B/RCT | 6.1 ± 2.7 months | Traditional rehabilitation | Time taken per intervention: None Intervention frequency per week: None Total intervention period: 6 weeks |
| 39 | Trobia et al. (2011) [57] | Combined use of music and virtual reality to support mental practice in stroke rehabilitation | 4/Case series | 24 months | MP only | Time taken per intervention: None Intervention frequency per week: 7/W Total intervention period: 4 weeks |
| 40 | Page et al. (2011) [58] | Retention of motor changes in chronic stroke survivors who were administered mental practice. | 2B/RCT | 58.7 months (range 13–129) | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 10 weeks |
| 41 | Page et al. (2011) [59] | Longer versus shorter mental practice sessions for affected upper extremity movement after stroke: a randomized controlled trial. | 2B/RCT | 36 months | Traditional rehabilitation | Time taken per intervention: 20 or 40 or 60 min Intervention frequency per week: 3/W Total intervention period: 10 weeks |
| 42 | Ietswaart et al. (2011) [21] | Mental practice with motor imagery in stroke recovery: randomized controlled trial of efficacy | 1B/RCT | 82 ± 55 days | MP only | Time taken per intervention: 45 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 43 | Wu et al. (2011) [60] | Improved function after combined physical and mental practice after stroke: a case of hemiparesis and apraxia. | 4/Case study | 7 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 6 weeks |
| 44 | Céline et al. (2010) [61] | Determining specificity of motor imagery training for upper limb improvement in chronic stroke patients: a training protocol and pilot results. | 3B/One group, nonrandomized | 16.5 ± 7.3 | MP only | Time taken per intervention: 15 min Intervention frequency per week: 4/W Total intervention period: 3 weeks |
| 45 | Riccio et al.(2010) [15] | Mental practice is effective in upper limb recovery after stroke: a randomized single-blind cross-over study. | 2B/RCT | 7.33 ± 2.38 week | Traditional rehabilitation | Time taken per intervention: 60 min Intervention frequency per week: 5/W Total intervention period: 3 weeks |
| 46 | Gaggioli et al. (2009) [62] | Computer-guided mental practice in neurorehabilitation. | 3B/One group, nonrandomized | 31 ± 25.3 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 2/W Total intervention period: 8 weeks |
| 47 | Prasad et al. (2009) [63] | Using Motor Imagery Based Brain-Computer Interface for Post-stroke Rehabilitation | 4/Case series | 28 ± 15.4 months | Traditional rehabilitation | Time taken per intervention: None Intervention frequency per week: 2/W Total intervention period: 6 weeks |
| 48 | Page et al. (2009) [16] | Cortical plasticity following motor skill learning during mental practice in stroke. | 3B/One group, nonrandomized | 36.7 ± 34 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 10 weeks |
| 49 | Page et al. (2009) [17] | Modified constraint-induced therapy combined with mental practice: thinking through better motor outcomes. | 2B/RCT | 28.5 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 3/W Total intervention period: 10 weeks |
| 50 | Simmons et al. (2008) [64] | Motor imagery to enhance recovery after subcortical stroke: who might benefit, daily dose, and potential effects. | 3B/One group, nonrandomized | 8.71 ± 10.4 months | MP only | Time taken per intervention: 60 min Intervention frequency per week: 5/W Total intervention period: 2 weeks |
| 51 | Hewett et al. (2007) [10] | Reaching kinematics to measure motor changes after mental practice in stroke. | 4/Case series | 51.2 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 2/W Total intervention period: 6 weeks |
| 52 | Page et al. (2007) [11] | Mental practice as a gateway to modified constraint-induced movement therapy: a promising combination to improve function. | 4/Case series | 32 ± 22 months | Traditional Rehabilitation | Time taken per intervention: None Intervention frequency per week: 2/W Total intervention period: 6 weeks |
| 53 | Page et al. (2007) [65] | Mental practice in chronic stroke: results of a randomized, placebo-controlled trial. | 1B/RCT | 38.8 ± 25.8 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 2/W Total intervention period: 6 weeks |
| 54 | Müller et al. (2007) [30] | Mental practice improves hand function after hemiparetic stroke. | 2B/RCT | 28.7 ± 21.2 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 5/W Total intervention period: 4 weeks |
| 55 | Butler et al. (2006) [25] | Mental practice with motor imagery: evidence for motor recovery and cortical reorganization after stroke. | 4/Case series | 9.2 ± 6.7 months | Traditional rehabilitation | Time taken per intervention: 180 min Intervention frequency per week: 7/W Total intervention period: 2 weeks |
| 56 | Gaggioli et al. (2005) [66] | A strategy for computer-assisted mental practice in stroke rehabilitation. | 4/Case study | 13 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 3/W Total intervention period: 12 weeks |
| 57 | Page et al. (2005) [67] | Effects of mental practice on affected limb use and function in chronic stroke. | 2B/RCT | 23.8 months | Traditional rehabilitation | Time taken per intervention: 30 min Intervention frequency per week: 2/W Total intervention period: 6 weeks |
| 58 | Dijkerman et al. (2004) [68] | Does motor imagery training improve hand function in chronic stroke patients? A pilot study. | 2B/RCT | 2 ± 0.8 months | MP only | Time taken per intervention: None Intervention frequency per week: 7/W Total intervention period: 4 weeks |
| 59 | Stevens et al. (2003) [8] | Using motor imagery in the rehabilitation of hemiparesis | 4/Case series | 44 ± 42.4 months | MP only | Time taken per intervention: 60 min Intervention frequency per week: 3/W Total intervention period: 4 weeks |
| 60 | Crosbie et al. (2003) [69] | The adjunctive role of mental practice in the rehabilitation of the upper limb after hemiplegic stroke: a pilot study. | 4/Case series | 39.4 ± 49.6 days | Traditional rehabilitation | Time taken per intervention: 45 min Intervention frequency per week: 5/W Total intervention period: 2 weeks |
| 61 | Page et al. (2001) [70] | Mental practice combined with physical practice for upper-limb motor deficit in subacute stroke. | 4/Case study | 5 months | Traditional rehabilitation | Time taken per intervention: 10 min Intervention frequency per week: 2/W Total intervention period: 6 weeks |
- (3)
- What are the most common methods of MI recall and MI tasks used during an MP intervention?
- (4)
- Is MP often used in conjunction with individual rehabilitation?
- (5)
- What are the upper-limb and cognitive function levels on the paralyzed side at the start of an MP intervention?
4. Discussion
- (1)
- When is an MP intervention most frequently employed after stroke onset?
- (2)
- What is the MP load (intervention time, number of intervention days, and intervention period)?
- (3)
- What are the most common methods of MI recall and MI tasks used during an MP intervention?
- (4)
- Is MP often used in conjunction with individual rehabilitation?
- (5)
- What are the upper-limb and cognitive function levels on the paralyzed side at the start of MP intervention?
5. Clinical Implications
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Langhorne, P.; Coupar, F.; Pollock, A. Motor recovery after stroke: A systematic review. Lancet Neurol. 2009, 8, 741–754. [Google Scholar] [CrossRef]
- Hatem, S.M.; Saussez, G.; Della Faille, M.; Prist, V.; Zhang, X.; Dispa, D.; Bleyenheuft, Y. Rehabilitation of motor function after stroke: A multiple systematic review focused on techniques to stimulate upper extremity recovery. Front. Hum. Neurosci. 2016, 10, 442. [Google Scholar] [CrossRef] [PubMed]
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef] [PubMed]
- Malouin, F.; Jackson, P.L.; Richards, C.L. Towards the integration of mental practice in rehabilitation programs. A critical review. Front. Hum. Neurosci. 2013, 7, 576. [Google Scholar] [CrossRef] [PubMed]
- Guerra, Z.F.; Lucchetti, A.L.G.; Lucchetti, G. Motor imagery training after stroke: A systematic review and meta-analysis of randomized controlled trials. J. Neurol. Phys. Ther. 2017, 41, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Yoo, E.Y.; Jung, M.Y.; Kim, J.; Park, J.H.; Kang, D.H. The effects of mental practice combined with modified constraint-induced therapy on corticospinal excitability, movement quality, function, and activities of daily living in persons with stroke. Disabil. Rehabil. 2018, 40, 2449–2457. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Lee, N.; Cho, M.; Kim, D.K.; Yang, Y. Effects of mental practice on stroke patients’ upper extremity function and daily activity performance. J. Phys. Ther. Sci. 2015, 27, 1075–1077. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.A.; Stoykov, M.E.P. Using motor imagery in the rehabilitation of hemiparesis. Arch. Phys. Med. Rehabil. 2003, 84, 1090–1092. [Google Scholar] [CrossRef] [PubMed]
- Page, S.J.; Hade, E.M.; Pang, J. Retention of distributed practice effect during mental practice in hemiparetic stroke. Arch. Phys. Med. Rehabil. 2015, 96, e57. [Google Scholar] [CrossRef]
- Hewett, T.E.; Ford, K.R.; Levine, P.; Page, S.J. Reaching kinematics to measure motor changes after mental practice in stroke. Top. Stroke Rehabil. 2007, 14, 23–29. [Google Scholar] [CrossRef]
- Page, S.J.; Levine, P.; Hill, V. Mental practice as a gateway to modified constraint-induced movement therapy: A promising combination to improve function. Am. J. Occup. Ther. 2007, 61, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, D.M.; Gillen, G.; DiRusso, T.; Gordon, A.M. Effect of imagery perspective on occupational performance after stroke: A randomized controlled trial. Am. J. Occup. Ther. 2012, 66, 320–329. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Page, S.J.; Levine, P.; Hill, V. Mental Practice–Triggered Electrical Stimulation in Chronic, Moderate, Upper-Extremity Hemiparesis After Stroke. Am. J. Occup. Ther. 2015, 69, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ji, E.K.; Wang, H.H.; Jung, S.J.; Lee, K.B.; Kim, J.S.; Jo, L.; Hong, B.Y.; Lim, S.H. Graded motor imagery training as a home exercise program for upper limb motor function in patients with chronic stroke: A randomized controlled trial. Medicine 2021, 100, e24351. [Google Scholar] [CrossRef] [PubMed]
- Riccio, I.; Iolascon, G.; Barillari, M.R.; Gimigliano, R.; Gimigliano, F. Mental practice is effective in upper limb recovery after stroke: A randomized single-blind cross-over study. Eur. J. Phys. Rehabil. Med. 2010, 46, 19–25. [Google Scholar]
- Page, S.J.; Szaflarski, J.P.; Eliassen, J.C.; Pan, H.; Cramer, S.C. Cortical plasticity following motor skill learning during mental practice in stroke. Neurorehabilit. Neural Repair 2009, 23, 382–388. [Google Scholar] [CrossRef]
- Page, S.J.; Levine, P.; Khoury, J.C. Modified constraint-induced therapy combined with mental practice: Thinking through better motor outcomes. Stroke 2009, 40, 551–554. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Ietswaart, M.; Johnston, M.; Dijkerman, H.C.; Joice, S.; Scott, C.L.; MacWalter, R.S.; Hamilton, S.J. Mental practice with motor imagery in stroke recovery: Randomized controlled trial of efficacy. Brain 2011, 134, 1373–1386. [Google Scholar] [CrossRef]
- Braun, S.M.; Beurskens, A.J.; Kleynen, M.; Oudelaar, B.; Schols, J.M.; Wade, D.T. A multicenter randomized controlled trial to compare subacute ‘treatment as usual’ with and without mental practice among persons with stroke in Dutch nursing homes. J. Am. Med. Dir. Assoc. 2012, 13, 85.e1–85.e857. [Google Scholar] [CrossRef]
- Kang, J.H.; Kim, M.W.; Park, K.H.; Choi, Y.A. The effects of additional electrical stimulation combined with repetitive transcranial magnetic stimulation and motor imagery on upper extremity motor recovery in the subacute period after stroke: A preliminary study. Medicine 2021, 100, e27170. [Google Scholar] [CrossRef]
- Park, J. The effects of task-oriented mental practice on upper limb function and coordination in chronic stroke patients—Randomized controlled trial design. Br. J. Occup. Ther. 2022, 85, 164–171. [Google Scholar] [CrossRef]
- Butler, A.J.; Page, S.J. Mental practice with motor imagery: Evidence for motor recovery and cortical reorganization after stroke. Arch. Phys. Med. Rehabil. 2006, 87 (Suppl. S2), S2–S11. [Google Scholar] [CrossRef]
- Xiong, X.; Wang, H.; Wang, X.; Sun, L.; Guo, X. Motor imagery training reduces contralesional compensation in stroke patients with moderate to severe upper limb impairment. In Proceedings of the 2021 10th International IEEE/EMBS Conference on Neural Engineering (NER), Virtual Event, 4–6 May 2021; pp. 876–879. [Google Scholar] [CrossRef]
- Park, J.S.; Choi, J.B.; An, D.H.; Chang, M.Y. Effects of mental practice combined with electromyogram-triggered electrical stimulation for upper extremity function in stroke patients. J. Phys. Ther. Sci. 2017, 29, 1819–1820. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, X.; Wang, H.; Xiong, X.; Sun, C.; Zhu, B.; Xu, Y.; Fan, M.; Tong, S.; Sun, L.; Guo, X. Motor imagery training after stroke increases slow-5 oscillations and functional connectivity in the ipsilesional inferior parietal lobule. Neurorehabilit. Neural Repair 2020, 34, 321–332. [Google Scholar] [CrossRef]
- Sun, L.; Yin, D.; Zhu, Y.; Fan, M.; Zang, L.; Wu, Y.; Jia, J.; Bai, Y.; Zhu, B.; Hu, Y. Cortical reorganization after motor imagery training in chronic stroke patients with severe motor impairment: A longitudinal fMRI study. Neuroradiology 2013, 55, 913–925. [Google Scholar] [CrossRef] [PubMed]
- Müller, K.; Bütefisch, C.M.; Seitz, R.J.; Hömberg, V. Mental practice improves hand function after hemiparetic stroke. Restor. Neurol. Neurosci. 2007, 25, 501–511. [Google Scholar] [PubMed]
- Li, F.; Zhang, T.; Li, B.J.; Zhang, W.; Zhao, J.; Song, L.P. Motor imagery training induces changes in brain neural networks in stroke patients. Neural Regen. Res. 2018, 13, 1771–1781. [Google Scholar] [CrossRef]
- Liu, H.; Song, L.; Zhang, T. Changes in brain activation in stroke patients after mental practice and physical exercise: A functional MRI study. Neural Regen. Res. 2014, 9, 1474–1484. [Google Scholar] [CrossRef]
- Liu, H.; Song, L.P.; Zhang, T. Mental practice combined with physical practice to enhance hand recovery in stroke patients. Behav. Neurol. 2014, 2014, 876416. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.Q.; Gao, T.H.; Li, J.; Tao, J.C.; Bai, Y.L.; Lu, R.R. Motor imagery-based brain-computer interface combined with multimodal feedback to promote upper limb motor function after stroke: A preliminary study. Evid. Based Complement. Altern. Med. 2021, 2021, 1116126. [Google Scholar] [CrossRef] [PubMed]
- Liepert, J.; Stürner, J.; Büsching, I.; Sehle, A.; Schoenfeld, M.A. Effects of a single mental chronometry training session in subacute stroke patients—A randomized controlled trial. BMC Sports Sci. Med. Rehabil. 2020, 12, 66. [Google Scholar] [CrossRef] [PubMed]
- Page, S.J.; Levine, P. Multimodal mental practice versus repetitive task practice only to treat chronic stroke: A randomized controlled pilot study. Am. J. Occup. Ther. 2021, 75, 7506205020. [Google Scholar] [CrossRef] [PubMed]
- Nam, J.S.; Yi, T.I.; Moon, H.I. Effects of adjuvant mental practice using inverse video of the unaffected upper limb in subacute stroke: A pilot randomized controlled study. Int. J. Rehabli. Res. 2019, 42, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, A.; Meena, Y.K.; Raza, H.; Bhushan, B.; Uttam, A.K.; Pandey, N.; Hashmi, A.A.; Bajpai, A.; Dutta, A.; Prasad, G. Active physical practice followed by mental practice using BCI-driven hand exoskeleton: A pilot trial for clinical effectiveness and usability. IEEE J. Biomed. Health Inform. 2018, 22, 1786–1795. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, M.; Okuyama, K.; Takahashi, Y.; Hiramoto, M.; Nishimura, A.; Ushiba, J.; Fujiwara, T.; Liu, M. Change in reciprocal inhibition of the forearm with motor imagery among patients with chronic stroke. Neural Plast. 2018, 2018, 3946367. [Google Scholar] [CrossRef]
- Azad, A.; Mahmoodi-Manbar, A.; Arani-Kashani, Z. Effect of motor imagery training with sensory feedback on sensory-motor function of the upper extremity in patients with chronic stroke. J. Babol Univ. Med. Sci. 2018, 20, 28–35. [Google Scholar]
- Iso, N.; Ooso, S.; Yamamoto, N.; Moriuchi, T.; Sagari, A.; Iso, F.; Tanaka, K.; Tabira, T.; Toshio, H. Effect of mental practice using inverse video of the unaffected upper limb in a subject with chronic hemiparesis after stroke. J. Phys. Ther. Sci. 2016, 28, 2984–2987. [Google Scholar] [CrossRef][Green Version]
- Park, J. Influence of mental practice on upper limb muscle activity and activities of daily living in chronic stroke patients. J. Phys. Ther. Sci. 2016, 28, 1061–1063. [Google Scholar] [CrossRef]
- Park, J.; Park, J. The effects of game-based virtual reality movement therapy plus mental practice on upper extremity function in chronic stroke patients with hemiparesis: A randomized controlled trial. J. Phys. Ther. Sci. 2016, 28, 811–815. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.S.; Kim, E.J.; Kim, D.Y.; Kim, S.J. Effects of Adjuvant Mental Practice on Affected Upper Limb Function Following a Stroke: Results of Three-Dimensional Motion Analysis, Fugl-Meyer Assessment of the Upper Extremity and Motor Activity Logs. Ann. Rehabil. Med. 2016, 40, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Page, S.J.; Hade, E.M.; Pang, J. Retention of the spacing effect with mental practice in hemiparetic stroke. Exp. Brain Res. 2016, 234, 2841–2847. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.J.; Yoo, E.Y.; Jung, M.Y.; Park, S.H.; Park, J.H.; Lee, J. Effects of mental practice with action observation training on occupational performance after stroke. J. Stroke Cerebrovasc. Dis. 2015, 24, 1405–1413. [Google Scholar] [CrossRef] [PubMed]
- Morone, G.; Pisotta, I.; Pichiorri, F.; Kleih, S.; Paolucci, S.; Molinari, M.; Cincotti, F.; Kübler, A.; Mattia, D. Proof of principle of a brain-computer interface approach to support poststroke arm rehabilitation in hospitalized patients: Design, acceptability, and usability. Arch. Phys. Med. Rehabil. 2015, 96, S71–S78. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H. The effects of modified constraint-induced therapy combined with mental practice on patients with chronic stroke. J. Phys. Ther. Sci. 2015, 27, 1585–1588. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, S.; Butler, A.J.; Drake, D.; Dhamala, M. Functional organization and restoration of the brain motor-execution network after stroke and rehabilitation. Front. Hum. Neurosci. 2015, 30, 173. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.S.; Lee, B.H. Motor imagery training improves upper extremity performance in stroke patients. J. Phys. Ther. Sci. 2015, 27, 2289–2291. [Google Scholar] [CrossRef]
- De Almeida Oliveira, R.; Cintia Dos Santos Vieira, P.; Fernanda Rodrigues Martinho Fernandes, L.; Patrizzi, L.; De Oliveira, S.F.; De Souza, L.A.P.S. Mental practice and mirror therapy associated with conventional physical therapy training on the hemiparetic upper limb in poststroke rehabilitation: A preliminary study. Top. Stroke Rehabil. 2014, 21, 484–494. [Google Scholar] [CrossRef]
- de Assis, G.A.; Corrêa, A.G.D.; Martins, M.B.R.; Pedrozo, W.G.; Lopes, R.D. An augmented reality system for upper-limb post-stroke motor rehabilitation: A feasibility study. Disabil. Rehabil. Assist. Technol. 2016, 11, 521–528. [Google Scholar] [CrossRef]
- Ji, S.G.; Kim, M.K.; Cha, H.G. Effects of mental practice in conjunction with repetitive transcranial magnetic stimulation on the upper limbs of sub-acute stroke patients. J. Magn. 2014, 19, 353–356. [Google Scholar] [CrossRef]
- Santos-Couto-Paz, C.C.; Teixeira-Salmela, L.F.; Tierra-Criollo, C.J. The addition of functional task-oriented mental practice to conventional physical therapy improves motor skills in daily functions after stroke. Braz. J. Phys. Ther. 2013, 17, 564–571. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mihara, M.; Hattori, N.; Hatakenaka, M.; Yagura, H.; Kawano, T.; Hino, T.; Miyai, I. Near-infrared spectroscopy-mediated neurofeedback enhances efficacy of motor imagery-based training in poststroke victims: A pilot study. Stroke 2013, 44, 1091–1098. [Google Scholar] [CrossRef]
- Timmermans, A.A.A.; Verbunt, J.A.; van Woerden, R.; Moennekens, M.; Pernot, D.H.; Seelen, H.A.M. Effect of mental practice on the improvement of function and daily activity performance of the upper extremity in patients with subacute stroke: A randomized clinical trial. Am. Med. Dir. Assoc. 2013, 14, 204–212. [Google Scholar] [CrossRef]
- Trobia, J.; Gaggioli, A.; Antonietti, A. Combined use of music and virtual reality to support mental practice in stroke rehabilitation. J. Cyber Ther. Rehabil. 2011, 4, 57–61. [Google Scholar]
- Page, S.J.; Murray, C.; Hermann, V.; Levine, P. Retention of motor changes in chronic stroke survivors who were administered mental practice. Arch. Phys. Med. Rehabil. 2011, 92, 1741–1745. [Google Scholar] [CrossRef]
- Page, S.J.; Dunning, K.; Hermann, V.; Leonard, A.; Levine, P. Longer versus shorter mental practice sessions for affected upper extremity movement after stroke: A randomized controlled trial. Clin. Rehabil. 2011, 25, 627–637. [Google Scholar] [CrossRef]
- Wu, A.J.; Radel, J.; Hanna-Pladdy, B. Improved function after combined physical and mental practice after stroke: A case of hemiparesis and apraxia. Am. J. Occup. Ther. 2011, 65, 161–168. [Google Scholar] [CrossRef]
- Crajé, C.; Van Der Graaf, C.; Lem, F.C.; Geurts, A.C.H.; Steenbergen, B. Determining specificity of motor imagery training for upper limb improvement in chronic stroke patients: A training protocol and pilot results. Int. J. Rehabil. Res. 2010, 33, 359–362. [Google Scholar] [CrossRef]
- Gaggioli, A.; Morganti, F.; Meneghini, A.; Pozzato, I.; Greggio, G.; Pigatto, M.; Riva, G. Computer-guided mental practice in neurorehabilitation. Stud. Health Technol. Inform. 2009, 145, 195–208. [Google Scholar]
- Prasad, G.; Herman, P.; Coyle, D.; McDonough, S.; Crosbie, J. Using motor imagery based brain-computer interface for post-stroke rehabilitation. In Proceedings of the 2009 4th International IEEE/EMBS Conference on Neural Engineering, Antalya, Turkey, 29 April–2 May 2009; pp. 258–262. [Google Scholar] [CrossRef]
- Simmons, L.; Sharma, N.; Baron, J.C.; Pomeroy, V.M. Motor imagery to enhance recovery after subcortical stroke: Who might benefit, daily dose, and potential effects. Neurorehabilit. Neural Repair 2008, 22, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Page, S.J.; Levine, P.; Leonard, A. Mental practice in chronic stroke: Results of a randomized, placebo-controlled trial. Stroke 2007, 38, 1293–1297. [Google Scholar] [CrossRef]
- Gaggioli, A.; Meneghini, A.; Morganti, F.; Alcaniz, M.; Riva, G. A strategy for computer-assisted mental practice in stroke rehabilitation. Neurorehabilit. Neural Repair 2006, 20, 503–507. [Google Scholar] [CrossRef]
- Page, S.J.; Levine, P.; Leonard, A.C. Effects of mental practice on affected limb use and function in chronic stroke. Arch. Phys. Med. Rehabil. 2005, 86, 399–402. [Google Scholar] [CrossRef]
- Dijkerman, H.C.; Ietswaart, M.; Johnston, M.; MacWalter, R.S. Does motor imagery training improve hand function in chronic stroke patients? A pilot study. Clin. Rehabil. 2004, 18, 538–549. [Google Scholar] [CrossRef]
- Crosbie, J.H.; McDonough, S.M.; Gilmore, D.H.; Wiggam, M.I. The adjunctive role of mental practice in the rehabilitation of the upper limb after hemiplegic stroke: A pilot study. Clin. Rehabil. 2004, 18, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Page, S.J.; Levine, P.; Sisto, S.A.; Johnston, M.V. Mental practice combined with physical practice for upper-limb motor deficit in subacute stroke. Phys. Ther. 2001, 81, 1455–1462. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097-269. [Google Scholar] [CrossRef]
- Teasell, R.; Bayona, N.A.; Bitensky, J. Plasticity and reoeganization of the brain post stroke. Top. Stroke Rehabil. 2005, 12, 11–26. [Google Scholar] [CrossRef]
- Graham, J.D.; Sonne, M.W.; Bray, S.R. It wears me out just imagining it! Mental imagery leads to muscle fatigue and diminished performance of isometric exercise. Biol. Psychol. 2014, 103, 1–6. [Google Scholar] [CrossRef]
- Rozand, V.; Lebon, F.; Papaxanthis, C.; Lepers, R. Does a mental training session induce neuromuscular fatigue? Med. Sci. Sports Exerc. 2014, 46, 1981–1989. [Google Scholar] [CrossRef]
- Rozand, V.; Lebon, F.; Stapley, P.J.; Papaxanthis, C.; Lepers, R. A prolonged motor imagery session alter imagined and actual movement durations: Potential implications for neurorehabilitation. Behav. Brain Res. 2016, 297, 67–75. [Google Scholar] [CrossRef]
- Nakashima, A.; Moriuchi, T.; Matsuda, D.; Hasegawa, T.; Nakamura, J.; Anan, K.; Satoh, K.; Suzuki, T.; Higashi, T.; Sugawara, K. Corticospinal excitability during motor imagery is diminished by continuous repetition-induced fatigue. Neural Regen. Res. 2021, 16, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, A.; Moriuchi, T.; Matsuda, D.; Nakamura, J.; Fujiwara, K.; Ikio, Y.; Hasegawa, T.; Mitunaga, W.; Higashi, T. Continuous repetition motor imagery training and physical practice training exert the growth of fatigue and its effect on performance. Brain Sci. 2022, 12, 1087. [Google Scholar] [CrossRef] [PubMed]
- Ruffino, C.; Papaxanthis, C.; Lebon, F. Neural plasticity during motor learning with motor imagery practice: Review and perspectives. Neuroscience 2017, 341, 61–78. [Google Scholar] [CrossRef] [PubMed]
- Ruffino, C.; Papaxanthis, C.; Lebon, F. The influence of imagery capacity in motor performance improvement. Exp. Brain Res. 2017, 235, 3049–3057. [Google Scholar] [CrossRef] [PubMed]
- Arya, K.N. Underlying neural mechanisms of mirror therapy: Implications for motor rehabilitation in stroke. Neurol. India 2016, 64, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Thieme, H.; Morkisch, N.; Mehrholz, J.; Pohl, M.; Behrens, J.; Borgetto, B.; Dohle, C. Mirror therapy for improving motor function after stroke. Cochrane Database Syst. Rev. 2018, 2018, CD008449. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Song, C. Postural difference between the interventions reflecting the concept of mirror therapy in healthy subjects. Brain Sci. 2021, 11, 1567. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Yi, J.; Song, C.H. Kinematic analysis of head, trunk, and pelvic motion during mirror therapy for stroke patients. J. Phys. Ther. Sci. 2017, 29, 1793–1799. [Google Scholar] [CrossRef][Green Version]
- Okamura, R.; Nakashima, A.; Moriuchi, T.; Fujiwara, K.; Ohno, K.; Higashi, T.; Tomori, K. Effects of a virtual reality-based mirror therapy system on upper extremity rehabilitation after stroke: A systematic review and meta-analysis of randomized controlled trials. Front. Neurol. 2024, 8, 1298291. [Google Scholar] [CrossRef] [PubMed]
- Abdullahi, A.; Wong, T.W.; Ng, S.S.M. Rehabilitation of severe impairment in motor function after stroke: Suggestions for harnessing the potentials of mirror neurons and the mentalizing systems to stimulate recovery. Brain Sci. 2022, 12, 1311. [Google Scholar] [CrossRef] [PubMed]
- Jeannerod, M. Mental Imagery in the Motor Context. Neuropsychologia 1995, 33, 1419–1432. [Google Scholar] [CrossRef] [PubMed]
- Decety, J. The Neurophysiological Basis of Motor Imagery. Behav. Brain Res. 1996, 77, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Mizuguchi, N.; Nakata, H.; Uchida, Y.; Kanosue, K. Motor imagery and sport performance. J. Phys. Fitness Sports Med. 2012, 1, 103–111. [Google Scholar] [CrossRef]
- Villa-Berges, E.; Laborda Soriano, A.A.; Lucha-López, O.; Tricas-Moreno, J.M.; Hernández-Secorún, M.; Gómez-Martínez, M.; Hidalgo-García, C. Motor Imagery and Mental Practice in the Subacute and Chronic Phases in Upper Limb Rehabilitation after Stroke: A Systematic Review. Occup. Ther. Int. 2023, 24, 3752889. [Google Scholar] [CrossRef] [PubMed]
- Stockley, R.C.; Jarvis, K.; Boland, P.; Clegg, A.J. Systematic Review and Meta-Analysis of the Effectiveness of Mental Practice for the Upper Limb after Stroke: Imagined or Real Benefit? Arch. Phys. Med. Rehabil. 2021, 102, 1011–1027. [Google Scholar] [CrossRef]
- Corbetta, D.; Sirtori, V.; Castellini, G.; Moja, L.; Gatti, R. Constraint-induced movement therapy for upper extremities in people with stroke. Cochrane Database Syst. Rev. 2015, 2015, CD004433. [Google Scholar] [CrossRef]
| Identifying the Research Questions | |
|---|---|
| Participants | Adult stroke patient |
| Concept | MP (time taken to start the intervention; MP load; MI recall and MI tasks performed during MP; association with individual rehabilitation; function level for the use of MP) |
| Context | Acute to chronic; Japan; Abroad |
| Inclusion Criteria | |
| · A study on MP for post-stroke paralytic lateral upper-limb function (Including all study types) · English Papers | |
| Database | Search Strategy |
|---|---|
| PubMed | (“cerebrovascular disorder”[Title/Abstract] OR (“stroke”[MeSH Terms] OR “stroke”[Title/Abstract] OR “strokes”[Title/Abstract] OR “stroke s”[Title/Abstract]) OR “Brain infarction”[Title/Abstract] OR “Brain Stem Infarctions”[Title/Abstract] OR “Cerebral Infarction”[Title/Abstract] OR (“lacunar”[Title/Abstract] OR “lacunars”[Title/Abstract]) OR “Brain injury”[Title/Abstract]) AND (“mental practice”[Title/Abstract] OR “motor imagery training”[Title/Abstract] OR “motor image”[Title/Abstract]) |
| Scopus | (TITLE-ABS-KEY (“cerebrovascular disorder” OR stroke OR “brain infarction” OR “brain stem infarctions” OR “cerebral infarction” OR lacunar OR “brain injury”)) AND (TITLE-ABS-KEY (“mental practice” OR “motor imagery training” OR “motor image”)) |
| Medline | title(“cerebrovascular disorder” OR stroke OR “Brain infarction” OR “Brain Stem Infarctions” OR “Cerebral Infarction” OR Lacunar OR “Brain injury”) AND title(“mental practice” OR “motor imagery training” OR “motor image”) abstract(“cerebrovascular disorder” OR stroke OR “Brain infarction” OR “Brain Stem Infarctions” OR “Cerebral Infarction” OR Lacunar OR “Brain injury”) AND abstract(“mental practice” OR “motor imagery training” OR “motor image”) |
| Cochrane Library | Cochrane Reviews matching “cerebrovascular disorder” OR stroke OR “Brain infarction” OR “Brain Stem Infarctions” OR “Cerebral Infarction” OR Lacunar OR “Brain injury” in Title Abstract Keyword AND “mental practice” OR “motor imagery training” OR “motor image” in Title Abstract Keyword |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakashima, A.; Okamura, R.; Moriuchi, T.; Fujiwara, K.; Higashi, T.; Tomori, K. Exploring Methodological Issues in Mental Practice for Upper-Extremity Function Following Stroke-Related Paralysis: A Scoping Review. Brain Sci. 2024, 14, 202. https://doi.org/10.3390/brainsci14030202
Nakashima A, Okamura R, Moriuchi T, Fujiwara K, Higashi T, Tomori K. Exploring Methodological Issues in Mental Practice for Upper-Extremity Function Following Stroke-Related Paralysis: A Scoping Review. Brain Sciences. 2024; 14(3):202. https://doi.org/10.3390/brainsci14030202
Chicago/Turabian StyleNakashima, Akira, Ryohei Okamura, Takefumi Moriuchi, Kengo Fujiwara, Toshio Higashi, and Kounosuke Tomori. 2024. "Exploring Methodological Issues in Mental Practice for Upper-Extremity Function Following Stroke-Related Paralysis: A Scoping Review" Brain Sciences 14, no. 3: 202. https://doi.org/10.3390/brainsci14030202
APA StyleNakashima, A., Okamura, R., Moriuchi, T., Fujiwara, K., Higashi, T., & Tomori, K. (2024). Exploring Methodological Issues in Mental Practice for Upper-Extremity Function Following Stroke-Related Paralysis: A Scoping Review. Brain Sciences, 14(3), 202. https://doi.org/10.3390/brainsci14030202






