A Novel Computer Oculomotor Rehabilitation (COR) Program for Mild Traumatic Brain Injury (mTBI)
Abstract
:1. Introduction
2. General Program Concepts
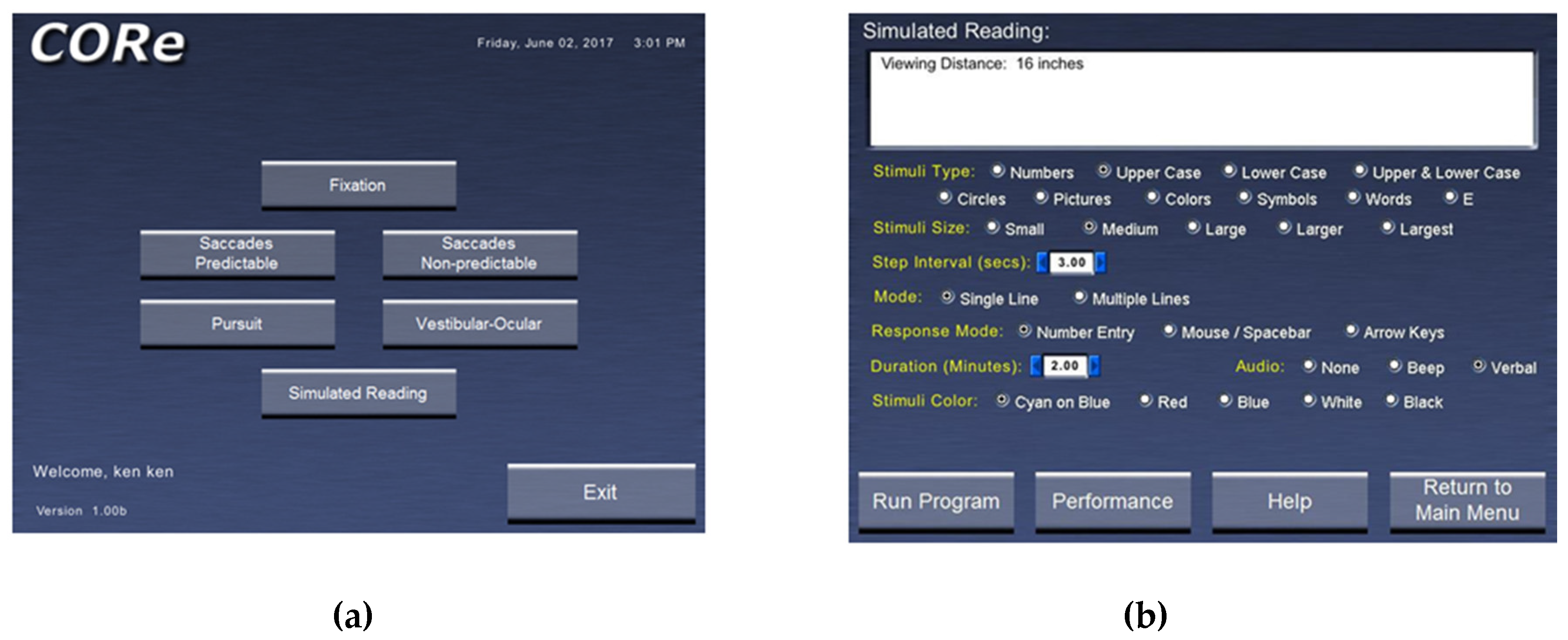
- A window displaying the possible categories of eye movement training. These currently include fixation in different positions of gaze (central, horizontal, and vertical); predictable saccades (horizontal and vertical); non-predictable saccades (horizontal and vertical); smooth pursuit (horizontal and vertical): vestibulo-ocular reflex in different positions of gaze (central, horizontal, vertical, and oblique); and simulated reading (Figure 1a). Figure 1b shows the specific template for training reading eye movements.
- Related to #1, there is the ability to vary the stimulus parameters for each category of eye movement trained. For example, for smooth pursuit training, direction (horizontal or vertical), amplitude (5 or 10 degrees), target velocity (0.5–10.0 degrees per second), and size (in five increments ranging from very small to very large), as well as other parameters (e.g., color), can be varied to maintain attention and/or gradually increase the level of task difficulty (i.e., task loading).
- Related to #1 and 2, the concept of rapid serial visual presentation (RSVP) is employed [27]. RSVP represents an experimental approach to assess temporal aspects of general/visual attention. RSVP involves the use of a “targeted” stimulus presented immediately prior to the training trial, as well as various, random “distractor” stimuli that are presented along with the “targeted” stimulus during a trial run. For example, as the patient trains fixation on the midline for 30 s, either the targeted or distractor stimulus is presented multiple times. The task is to perform the oculomotor training while concurrently counting how many times the “targeted” stimulus was presented with respect to the total number of stimulus changes that occurred (e.g., four times out of 12). The RSVP paradigm forces an additional attentional aspect to the training task. RSVP is incorporated into all of the training programs.
- The ability to add a visual and/or auditory distractor during training is possible. The visual distractor is comprised of a white, rectangular bar that is spatially and temporally presented at random, concurrently with the training stimulus during a trial, if so desired. Similarly, the audio distractor is comprised of “white noise” that is present throughout the trial, if so desired. This feature introduces increased “task-loading” to the training, which adds an additional layer of difficulty, once the patient begins to perform better. It is also possible to have neither distractor, if so desired, especially at the early training sessions when the patient’s performance is less than optimal.
- There is basic monitoring of progress for each category of training over time. This feature provides the number of “targeted” stimuli and the number of errors for each training trial, and then for all trials performed at a particular session, as well as across sessions on different days/weeks/months.
- Lastly, one can manually introduce plus or minus spherical lenses to alter the accommodative (eye focusing) near demand, as well as either base-out or base-in prisms to alter the horizontal vergence near demand, or both. Base-up and base-down prisms can also be introduced to train the vertical vergence system. Thus, all three basic oculomotor control systems can be activated during a training session, namely, vergence, accommodation, and version.
Specific Program Concepts
- Stimulus type: There are 10 possible choices—a number, upper case letter, lower case letter, upper and lower case letters combined, colored balls, symbols, short words, and a Snellen E.
- Stimulus size: There are five possible choices—small, medium, large, larger, and largest (2–20 mm in dimension).
- Duration per position: 0.25–5.0 min.
- Response mode: number entry, mouse/spacebar entry, or arrow key entry for the patient to indicate the number of targeted stimuli they believed to be present during a trial run.
- Stimulus color: cyan on blue, blue, red, white on black, and black on white.
- Distractor: none, visual, audio, or both.
- Audio performance indicator: none, beep, or computer-based human spoken word to indicate if the number of RSVP targeted changes entered was correct.
- Rapid serial visual presentation (RSVP).
- Fixation:
- presentation time on (0.1–4 s)
- presentation time off (0–4.0 s, with zero indicating no time gap between stimulus presentation)
- stimulus placement—all five possible positions, namely either center, or right, left, top, or down (all 10 degrees from center)
- Predictable saccades:
- step interval change (1–10 s)
- stimulus amplitude (5 or 10 degrees centered on the midline)
- direction of stimulus movement (horizontal or vertical)
- Non-predictable saccades
- does not have 2a and 2b above
- trial duration (0.25–5.0 min)
- direction of stimulus movement (horizontal or vertical centered on the midline)
- Smooth Pursuit
- velocity (0.5–10 degs/s)
- direction of stimulus movement (horizontal or vertical centered on the midline)
- Vestibulo-ocular reflex (VOR)
- stimulus placement—either center, or left, right, up, down, upper left, upper right, lower left, and lower right (all 10 degrees from center)
- metronome beat frequency—0.25–4.0 beats/s—indicates head movement frequency per cycle while fixating and maintaining stability of the target; up to 6 Hz if possible.
3. Examples of Training Benefits
4. Program Areas for Future Development
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Silver, J.M.; McAllister, T.W.; Yudofsky, S.C. (Eds.) Textbook of Traumatic Brain Injury; American Psychiatric Publishing Inc.: Washington, DC, USA, 2005. [Google Scholar]
- Zasler, N.D.; Katz, D.I.; Zafonte, R.D. (Eds.) Brain Injury Medicine: Principles and Practice; Demos Medical Publishing: New York, NY, USA, 2007. [Google Scholar]
- Suchoff, I.B.; Ciuffreda, K.J.; Kapoor, N. (Eds.) Visual and Vestibular Consequences of Acquired Brain Injury; Optometric Extension Program Foundation: Santa Ana, CA, USA, 2001. [Google Scholar]
- Suter, P.S.; Harvey, L.H. Vision Rehabilitation; CRC Press: Boca Raton, FL, USA, 2011. [Google Scholar]
- Ciuffreda, K.J. Compendium of Works on Vision Rehabilitation; Optometric Extension Program Foundation: Timonium, MD, USA, 2016; Volume 1. [Google Scholar]
- Ciuffreda, K.J. Compendium of Works on Vision Rehabilitation; Optometric Extension Program Foundation: Timonium, MD, USA, 2017; Volume 2. [Google Scholar]
- Kapoor, N.; Ciuffreda, K.J. Vision disturbances following traumatic brain injury. Curr. Treat. Options Neurol. 2002, 4, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, N.; Ciuffreda, K.J.; Han, Y. Oculomotor rehabilitation in acquired brain injury. Arch. Phys. Med. Rehabil. 2004, 85, 1667–1678. [Google Scholar] [CrossRef] [PubMed]
- Ciuffreda, K.J.; Han, Y.; Kapoor, N.; Ficarra, A.P. Oculomotor rehabilitation for reading in acquired brain injury. NeuroRehabilitation 2006, 21, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Ciuffreda, K.J.; Kapoor, N.; Rutner, D.; Suchoff, I.B.; Han, M.E.; Craig, S. Occurrence of oculomotor dysfunctions in acquired brain injury. Optometry 2007, 78, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Ciuffreda, K.J.; Rutner, D.; Kapoor, N.; Suchoff, I.B.; Craig, S.; Han, M.E. Vision therapy for oculomotor dysfunctions in acquired brain injury: A retrospective analysis. Optometry 2008, 79, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Green, W.; Ciuffreda, K.J.; Thiagarajan, P.; Szymanowicz, D.; Ludlam, D.P.; Kapoor, N. Accommodation in mild traumatic brain injury. J. Rehabil. Res. Dev. 2010, 47, 183–199. [Google Scholar] [CrossRef] [PubMed]
- Szymanowicz, D.; Ciuffreda, K.J.; Thiagarajan, P.; Ludlam, D.P.; Green, W.; Kapoor, N. Vergence in mild traumatic brain injury: A pilot study. J. Rehabil. Res. Dev. 2012, 49, 1083–1100. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajan, P.; Ciuffreda, K.J. Effect of oculomotor rehabilitation on vergence reponsivity in mild traumatic brain injury. J. Rehabil. Res. Dev. 2013, 50, 1223–1240. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajan, P.; Ciuffreda, K.J.; Capo-Aponte, J.E.; Ludlam, D.P.; Kapoor, N. Oculomotor rehabilitation for reading in mild traumatic brain injury: An integrative approach. NeuroRehabilitation 2014, 34, 129–146. [Google Scholar] [PubMed]
- Thiagarajan, P.; Ciuffreda, K.J. Effect of oculomotor rehabilitation on accommodative responsivity in mild traumatic brain injury. J. Rehabil. Res. Dev. 2014, 51, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajan, P.; Ciuffreda, K.J. Versional tracking in mild traumatic brain injury (mTBI): Effects of oculomotor training (OMT). Brain Inj. 2014, 28, 930–943. [Google Scholar] [CrossRef] [PubMed]
- Yadav, N.K.; Thiagarajan, P; Ciuffreda, K.J. Effect of oculomotor vision rehabilitation on the visual-evoked potential and visual attention in mild trauamatic brain injury. Brain Inj. 2014, 28, 922–929. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajan, P.; Ciuffreda, K.J. Accommodative and vergence dysfunctions in mTBI: Treatment effects and system correlations. Optom. Vis. Perf. 2014, 2, 280–288. [Google Scholar]
- Thiagarajan, P.; Ciuffreda, K.J. Short-term persistence of oculomotor rehabilitative changes in mild traumatic brain injury (mTBI): A pilot study. Brain Inj. 2015, 29, 1475–1479. [Google Scholar] [CrossRef] [PubMed]
- Leigh, R.J.; Zee, D.S. The Neurology of Eye Movements; Davis, F.A., Ed.; Oxford University Press: Philadelphia, PA, USA, 1991. [Google Scholar]
- Ciuffreda, K.J.; Tannen, B. Eye Movement Basics for the Clinician; Mosby-Year Book: St. Louis, MO, USA, 1995. [Google Scholar]
- Stark, L.; Bahill, A.T.; Ciuffreda, K.J.; Kenyon, R.V.; Phillips, S. Neuro-optometry: An evolving specialty clinic. Optom. Physiol. Opt. 1977, 54, 85–96. [Google Scholar] [CrossRef]
- Taylor, E.A. The Fundamental Reading Skill; Charles C. Thomas: Springfield, IL, USA, 1966. [Google Scholar]
- Han, Y.; Ciuffreda, K.J.; Kapoor, N. Reading-related oculomotor testing and training protocols for acquired brain injury in humans. Brain Res. Protocols. 2004, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajan, P. Oculomotor Rehabilitation for Reading in Mild Traumatic Brain Injury. Ph.D. Thesis, SUNY College of Optometry, New York, NY, USA, 2012. Available online: https://dspace.sunyconnect.suny.edu/handle/1951/60654 (1 April 2017).
- Potter, M.C. Short-term conceptual memory for pictures. J. Exper. Psychol. Human Learn. Mem. 1976, 2, 509–522. [Google Scholar] [CrossRef]
- Ron, S.; Najenson, T.; Hary, D.; Prywork, W. Eye movements in brain injured patients. Scand. J. Rehabil. Med. 1978, 10, 39–44. [Google Scholar] [PubMed]
- Ciuffreda, K.J. The scientific basis and efficacy of optometric vision therapy in non-strabismic accommodative and vergence disorders. Optometry 2002, 73, 735–762. [Google Scholar] [PubMed]
- Ciuffreda, K.J.; Tannen, B.; Rutner, D. Multi-sensory feedback therapy for oculomotor dysfunction. In Models of the Visual System; Hung, G.K., Ciuffreda, K.J., Eds.; Kluwer Academic/Plenum Publishers: New York, NY, USA, 2002; pp. 741–769. [Google Scholar]


| (a) | |||
| Stimulus | Stimulus Parameter | Training Period Duration (s) | Total Training Duration (s) |
| Fixation | Central (midline) | 60 | 300 |
| Left (10 degrees) | 60 | ||
| Right (10 degrees) | 60 | ||
| Up (10 degrees) | 60 | ||
| Down (10 degrees) | 60 | ||
| Predictable Saccades | Horizontal (±5 degrees) | 75 | 300 |
| Horizontal (±10 degrees) | 75 | ||
| Vertical (±5 degrees) | 75 | ||
| Vertical (±10 degrees) | 75 | ||
| Simulated Reading (repeated twice) | Full-screen | 75 | 300 |
| Single-line | 75 | ||
| Full-screen | 75 | ||
| Single-line | 75 | ||
| (b) | |||
| Stimulus | Stimulus Parameter | Training Period Duration (min) | Total Training Duration (min) |
| Vergence | Step amplitude (BO/BI *) | 7 | 15 |
| Step facility (BO/BI *) | 5 | ||
| Ramp | 3 | ||
| Accommodation | Step amplitude right eye lenses | 5 | 15 |
| Step amplitude left eye lenses | 5 | ||
| Step facility | 5 | ||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciuffreda, K.J.; Yadav, N.K.; Thiagarajan, P.; Ludlam, D.P. A Novel Computer Oculomotor Rehabilitation (COR) Program for Mild Traumatic Brain Injury (mTBI). Brain Sci. 2017, 7, 99. https://doi.org/10.3390/brainsci7080099
Ciuffreda KJ, Yadav NK, Thiagarajan P, Ludlam DP. A Novel Computer Oculomotor Rehabilitation (COR) Program for Mild Traumatic Brain Injury (mTBI). Brain Sciences. 2017; 7(8):99. https://doi.org/10.3390/brainsci7080099
Chicago/Turabian StyleCiuffreda, Kenneth J., Naveen K. Yadav, Preethi Thiagarajan, and Diana P. Ludlam. 2017. "A Novel Computer Oculomotor Rehabilitation (COR) Program for Mild Traumatic Brain Injury (mTBI)" Brain Sciences 7, no. 8: 99. https://doi.org/10.3390/brainsci7080099




