A Cognitive—Behavioral Intervention for Postpartum Anxiety and Depression: Individual Phone vs. Group Format
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure
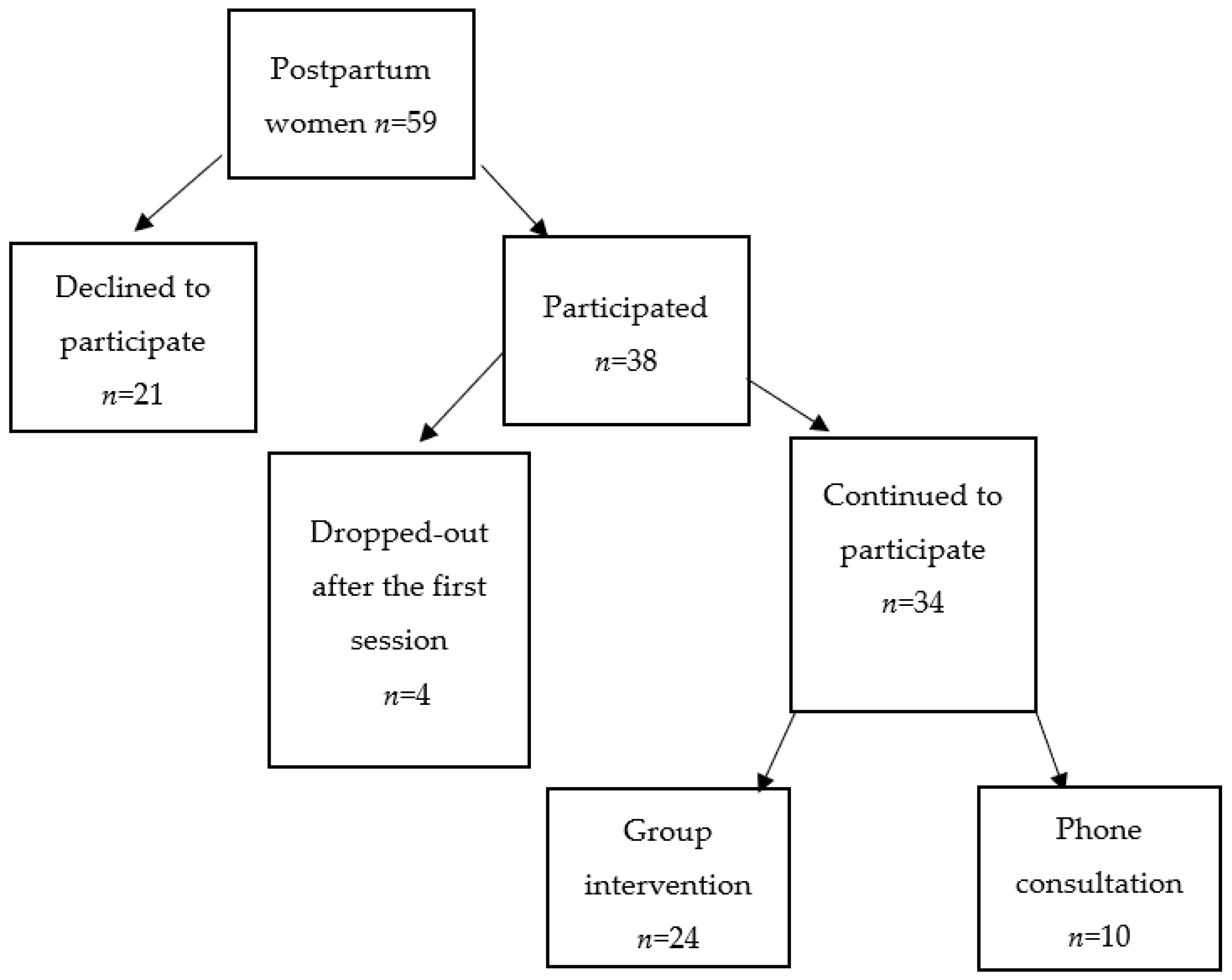
2.2. Sample
2.3. Research Instruments
2.4. The WAWA Protocol
2.5. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Glasser, S.; Barell, V.; Boyko, V.; Ziv, A.; Lusky, A.; Shoham, A.; Hart, S. Postpartum depression in an Israeli cohort: Demographic, psychosocial and medical risk if actors. J. Psychosom. Obstet. Gynecol. 2000, 21, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, J.; Holt, C.J.; Gemmill, A.W.; Ericksen, J.; Leigh, B.; Buist, A.; Schembri, C. Treating postnatal depressive symptoms in primary care: A randomised controlled trial of GP management, with and without adjunctive counselling. BMC Psychiatry 2011, 11, 95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, L.; Arteche, A.; Fearon, R.; Halligan, S.; Goodyer, I.; Cooper, P. Maternal Postnatal Depression and the Development of Depression in Offspring Up to 16 Years of Age. J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 460–470. [Google Scholar] [CrossRef] [PubMed]
- Rowe, H.J.; Calcagni, S.C.; Galgut, S.; Michelmore, J.; Fisher, J.R. Self-management of mild to moderate anxiety in women who have recently given birth: Development and acceptability of a theoretically sound complex intervention. Int. J. Ment. Health Promot. 2014, 16, 308–319. [Google Scholar] [CrossRef]
- Sarid, O.; Cwikel, J.; Czamanski-Cohen, J.; Huss, E. Treating women with perinatal mood and anxiety disorders (PMADs) with a hybrid cognitive behavioural and art therapy treatment (CB-ART). Arch. Women’s Ment. Health 2017, 20, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Sockol, L.E. A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. J. Affect. Disord. 2015, 177, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Simhi, M.; Cwikel, J.; Sarid, O. Treatment Preferences for Postpartum Depression Among New Israeli Mothers: The Contribution of Health Beliefs and Social Support. J. Am. Psychiatr. Nurses Assoc. 2021. [Google Scholar] [CrossRef]
- Simhi, M.; Sarid, O.; Cwikel, J. Preferences for mental health treatment for post-partum depression among new mothers. Isr. J. Health Policy Res. 2019, 8, 84. [Google Scholar] [CrossRef] [Green Version]
- Dennis, C.L.; Dowswell, T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst. Rev. 2013, 2. [Google Scholar] [CrossRef]
- Bledsoe, S.E.; Grote, N.K. Treating depression during pregnancy and the postpartum: A preliminary meta-analysis. Res. Soc. Work. Pract. 2006, 16, 109–120. [Google Scholar] [CrossRef]
- Clark, R.; Tluczek, A.; Brown, R. A mother-infant therapy group model for postpartum depression. Child Adolesc. Soc. Work. J. 2008, 29, 514–536. [Google Scholar] [CrossRef]
- Dennis, C.L.; Chung-Lee, L. Group treatment for postpartum depression: A systematic review. Arch. Womens Ment. Health. 2011, 14, 277–293. [Google Scholar]
- Ugarriza, D.N. Group therapy and its barriers for women suffering from postpartum depression. Arch. Psychiatr. Nurs. 2004, 18, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Scope, A.; Leaviss, J.; Kaltenthaler, E.; Parry, G.; Sutcliffe, P.; Bradburn, M.; Cantrell, A. Is group cognitive behaviour therapy for postnatal depression evidence-based practice? A systematic review. BMC Psychiatry 2013, 13, 321. [Google Scholar] [CrossRef] [Green Version]
- Bastien, C.H.; Morin, C.M.; Ouellet, M.-C.; Blais, F.C.; Bouchard, S. Cognitive-Behavioral Therapy for Insomnia: Comparison of Individual Therapy, Group Therapy, and Telephone Consultations. J. Consult. Clin. Psychol. 2004, 72, 653–659. [Google Scholar] [CrossRef] [PubMed]
- Goodman, J.H. Women’s Attitudes, Preferences, and Perceived Barriers to Treatment for Perinatal Depression. Birth 2009, 36, 60–69. [Google Scholar] [CrossRef]
- Huang, L.; Zhao, Y.; Qiang, C.; Fan, B. Is cognitive behavioral therapy a better choice for women with postnatal depression? A systematic review and meta-analysis. PLoS ONE 2018, 13, e0205243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ngai, F.W.; Wong, P.W.-C.; Chung, K.F.; Leung, K.Y. The effect of telephone-based cognitive-behavioural therapy on parenting stress: A randomised controlled trial. J. Psychosom. Res. 2016, 86, 34–38. [Google Scholar] [CrossRef]
- Brenes, G.A.; Ingram, C.W.; Danhauer, S.C. Benefits and challenges of conducting psychotherapy by telephone. Prof. Psychol. Res. Pract. 2011, 42, 543. [Google Scholar] [CrossRef] [Green Version]
- Cuijpers, P.; Noma, H.; Karyotaki, E.; Cipriani, A.; Furukawa, T.A. Effectiveness and acceptability of cognitive behavior therapy delivery formats in adults with depression: A network meta-analysis. JAMA Psychiatry 2019, 76, 700–707. [Google Scholar] [CrossRef]
- Letourneau, N.; Secco, L.; Colpitts, J.; Aldous, S.; Stewart, M.; Dennis, C.-L. Quasi-experimental evaluation of a telephone-based peer support intervention for maternal depression. J. Adv. Nurs. 2015, 71, 1587–1599. [Google Scholar] [CrossRef]
- Mureşan-Madar, A.; Băban, A. The development and piloting of a CBT group program for postpartum depression. J. Evid.-Based Psychother. 2015, 15, 51. [Google Scholar]
- Shulman, B.; Dueck, R.; Ryan, D.; Breau, G.; Sadowski, I.; Misri, S. Feasibility of a mindfulness-based cognitive therapy group intervention as an adjunctive treatment for postpartum depression and anxiety. J. Affect. Disord. 2018, 235, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression anxiety stress scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Cox, J.; Holden, J. Perinatal Mental Health: A Guide to the Edinburgh Postnatal Depression Scale (EPDS); Royal College of Psychiatrists: London, UK, 2003. [Google Scholar]
- Bina, R. Seeking Help for Postpartum Depression in the Israeli Jewish Orthodox Community: Factors Associated with Use of Professional and Informal Help. Women Health 2014, 54, 455–473. [Google Scholar] [CrossRef]
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed. e-Health 2020, 26, 377–379. [Google Scholar] [CrossRef] [Green Version]
- O’Mahen, H.A.; Woodford, J.; McGinley, J.; Warren, F.C.; Richards, D.; Lynch, T.; Taylor, R.S. Internet-based behavioral activation—Treatment for postnatal depression (Netmums): A randomized controlled trial. J. Affect. Disord. 2013, 150, 814–822. [Google Scholar] [CrossRef] [PubMed]
- Pugh, N.E.; Hadjistavropoulos, H.D.; Dirkse, D. A Randomised Controlled Trial of Therapist-Assisted, Internet-Delivered Cognitive Behavior Therapy for Women with Maternal Depression. PLoS ONE 2016, 11, e0149186. [Google Scholar] [CrossRef]
| Variables | n = 34 (%) | Individual n (%) | Group n (%) |
|---|---|---|---|
| Family status (n = 32) | |||
| Married | 31 (97) | 9 (28) | 22 (69) |
| Divorced | 1 (3) | 0 | 1 (3) |
| Children (n = 33) | |||
| First child | 6 (18) | 2 (6) | 4 (12) |
| <Second child | 27 (82) | 8 (24) | 19 (58) |
| Religious status (n = 33) | |||
| Secular | 1 (3) | 0 | 1 (3) |
| Traditional | 2 (6) | 1 (3) | 1 (3) |
| Religious | 26 (79) | 6 (18) | 20 (61) |
| Ultra-Orthodox | 4 (12) | 2 (6) | 2 (6) |
| Country of origin (n = 34) | |||
| Immigrant | 2 (6) | 0 | 2 (6) |
| Native born | 32 (94) | 10 (29) | 22 (65) |
| Employed (n = 34) | |||
| Yes | 31 (91) | 9 | 22 |
| No | 3 (9) | 1 | 2 |
| Spouse employment (n = 34) | |||
| Unemployed | 2 (6) | 1 (3) | 1 (3) |
| Employed | 32 (94) | 9 (26) | 23 (68) |
| Economic status (n = 34) | |||
| Some difficulty | 15 (45) | 7 (21) | 8 (24) |
| No difficulty | 19 (55) | 3 (8) | 16 (47) |
| Session Number | Topics Discussed | Homework Assigned |
|---|---|---|
| Initial introductory meeting | Introduction to the intervention principles presented in the workbook. Participants signing informed consent forms received a personal workbook. | |
| Session 1 | Background information on how symptoms of anxiety, depression, and distress present in the post-partum period. The links between thoughts, feelings, and behaviors are presented. | Identify thoughts that preceded distressing feelings and behaviors and write them down. |
| Session 2 | Participants were taught to discern maladaptive thought patterns such as dichotomized thinking (e.g., good–bad), catastrophizing, ‘should or must’ self-talk, etc. Participants learned to reframe maladaptive thoughts, in general, and in relation to mothering their infant, into more realistic, flexible patterns, and were encouraged to remember when things have gone well. Relaxation techniques to reduce stress were taught. | Identify and write down thoughts concerning infant’s feeding, crying, and other disturbing situations. Reframe thoughts into more flexible and adaptive patterns. Practice breathing and relaxation. |
| Session 3 | Using examples from daily life, mothers learned to manage inconsistent information regarding infant health and safety and deal with feelings of anxiety when they leave the infant with another person. Mindfulness and breathing skills were taught and practiced. | Identification of thoughts regarding infant behaviors and mother’s responses that were learned in the session. Reframing thoughts and assessing the feelings and behaviors derived from more adaptive ways of thinking. Practice mindfulness and breathing. |
| Session 4 | Mothers shared their personal experiences. Cognitive patterns of comparing oneself with others and how ‘I used to be’ were discussed and addressed with cognitive restructuring techniques. Skills attained over the intervention were highlighted and reinforced. | Mothers were encouraged to keep practicing relaxation techniques and to use their more adaptive modes of thinking and behaving after the intervention. |
| Dependent Variables | Mean | (SD) | t (df = 33) | Cohen’s d Effect Size |
|---|---|---|---|---|
| EPDST1 | 5.88 | (4.43) | 3.28 ** | 0.56 |
| EPDST2 | 3.67 | (3.06) | ||
| GADT1 | 5.97 | (3.66) | 2.53 ** | 0.45 |
| GADT2 | 4.34 | (3.18) | ||
| DASS Stress T1 | 4.94 | (4.05) | 2.204 * | 0.40 |
| DASS Stress T2 | 3.52 | (2.70) | ||
| DASS Anxiety T1 | 1.44 | (2.03) | 2.050 * | 0.35 |
| DASS Anxiety T2 | 0.79 | (1.20) | ||
| DASS Depression T1 | 3.06 | (2.75) | 2.651 ** | 0.45 |
| DASS Depression T2 | 1.88 | (1.99) |
| Dependent Variables | Format of Intervention | n | Mean | (SD) | t (df = 33) |
|---|---|---|---|---|---|
| Delta EPDS | telephone | 10 | 4.80 | (5.09) | 2.72 * |
| group | 24 | 1.12 | (2.78) | ||
| Delta GAD | telephone | 10 | 0.80 | (5.37) | −0.86 (ns) |
| group | 22 | 2.00 | (2.58) | ||
| Delta DASS stress | telephone | 9 | 3.33 | (4.44) | 2.00 * |
| group | 22 | 0.63 | (2.93) | ||
| Delta DASS anxiety | telephone | 10 | 1.20 | (2.14) | 1.03 (ns) |
| group | 24 | 0.41 | (1.69) | ||
| Delta DASS depression | telephone | 10 | 1.30 | (3.33) | 0.15 (ns) |
| group | 24 | 1.12 | (2.29) |
| T1 n (% of the Sample) | T2 n (% Reduction among Those with Concern at T1 *, % of the Sample) | |
|---|---|---|
| My baby’s safety and health | 18 (55) | 15 (17,45) |
| Comparing myself to others | 16 (49) | 10 (37,30) |
| Comparing myself to who I was before | 15 (45) | 12 (20,36) |
| Leaving my baby to be cared for by others | 12 (36) | 4 (67,12) |
| Leaving home/going out with baby Feeding my baby | 8 (24) 7 (21) | 5(37,15) 5 (29,15) |
| Dealing with inconsistent information | 6 (18) | 4 (33,12) |
| Maladaptive Cognitive Patterns | ||
| “Should” and “must” statements | 26 (76) | 16 (39,47) |
| Catastrophizing | 17 (50) | 16 (6,47) |
| Overgeneralizing | 17 (50) | 15 (12,44) |
| Jumping to conclusions | 12 (35) | 7 (42,21) |
| Personalization | 10 (29) | 7 (30,21) |
| Mind reading | 10 (29) | 9 (10,26) |
| Overstating the danger | 8 (24) | 3 (62,8) |
| Underestimating one’s coping ability | 8 (24) | 6(25,18) |
| Filtering | 7 (21) | 6 (14,18) |
| Dichotomous thinking | 7 (21) | 5 (29,15) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simhi, M.; Sarid, O.; Rowe, H.; Fisher, J.; Cwikel, J. A Cognitive—Behavioral Intervention for Postpartum Anxiety and Depression: Individual Phone vs. Group Format. J. Clin. Med. 2021, 10, 5952. https://doi.org/10.3390/jcm10245952
Simhi M, Sarid O, Rowe H, Fisher J, Cwikel J. A Cognitive—Behavioral Intervention for Postpartum Anxiety and Depression: Individual Phone vs. Group Format. Journal of Clinical Medicine. 2021; 10(24):5952. https://doi.org/10.3390/jcm10245952
Chicago/Turabian StyleSimhi, Meital, Orly Sarid, Heather Rowe, Jane Fisher, and Julie Cwikel. 2021. "A Cognitive—Behavioral Intervention for Postpartum Anxiety and Depression: Individual Phone vs. Group Format" Journal of Clinical Medicine 10, no. 24: 5952. https://doi.org/10.3390/jcm10245952
APA StyleSimhi, M., Sarid, O., Rowe, H., Fisher, J., & Cwikel, J. (2021). A Cognitive—Behavioral Intervention for Postpartum Anxiety and Depression: Individual Phone vs. Group Format. Journal of Clinical Medicine, 10(24), 5952. https://doi.org/10.3390/jcm10245952






