Bridging Perspectives: Exploring the Convergence of Clinimetrics and Network Theory in Mental Health Assessment and Conceptualization
Abstract
:1. Introduction
2. Materials and Methods
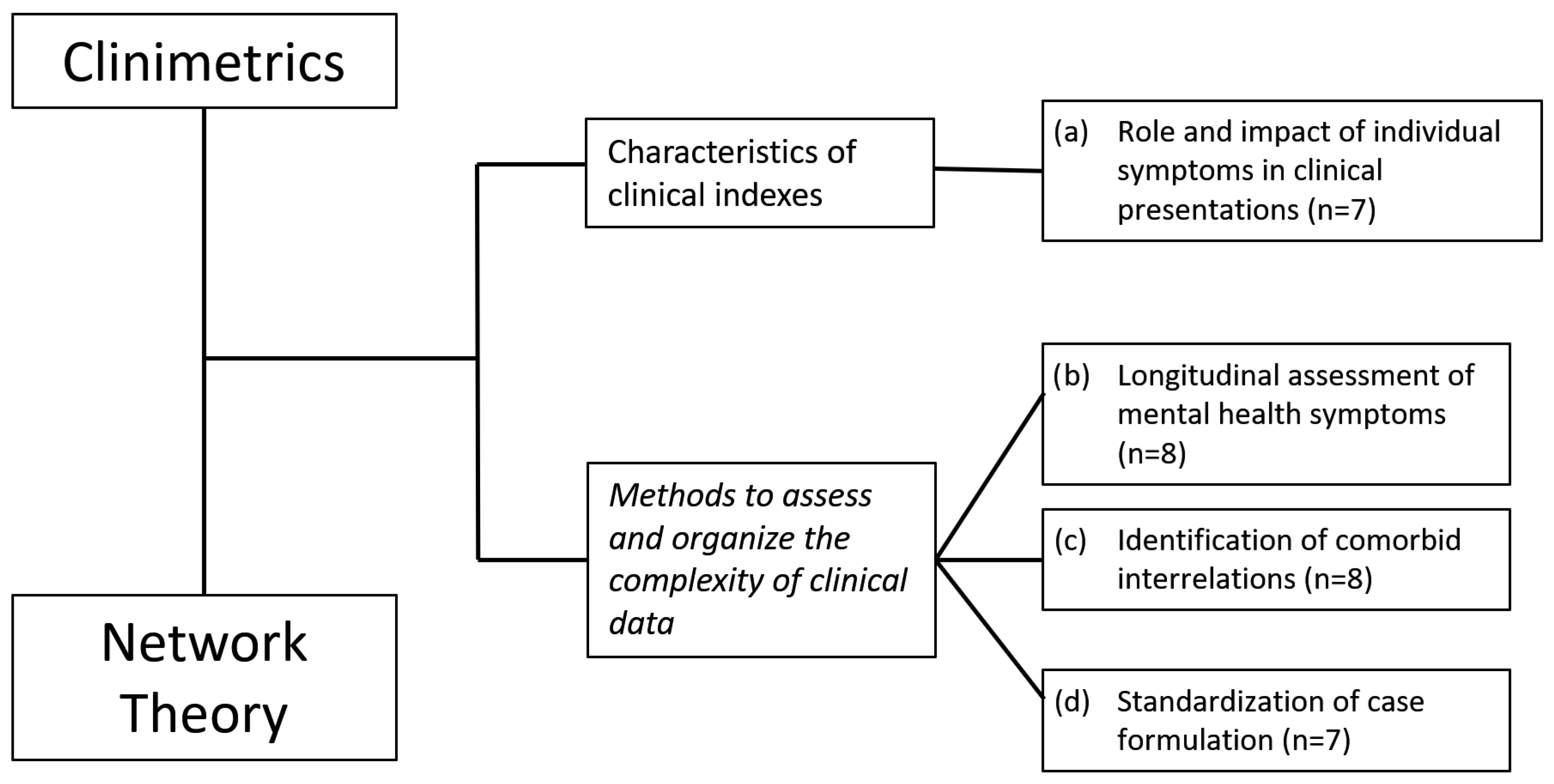
3. Results
3.1. Characteristics of Clinical Indexes
(a) Role and Impact of Individual Symptoms in Clinical Presentations
3.2. Methods to Assess and Organize Complex Clinical Information
3.2.1. (b) Longitudinal Assessment of Mental Health Symptoms
3.2.2. (c) Identification of Comorbid Interrelations
3.2.3. (d) Standardization of Case Formulation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kirkpatrick, R.H.; Munoz, D.P.; Khalid-Khan, S.; Booij, L. Methodological and clinical challenges associated with biomarkers for psychiatric disease: A scoping review. J. Psychiatr. Res. 2021, 143, 572–579. [Google Scholar] [CrossRef]
- García-Gutiérrez, M.S.; Navarrete, F.; Sala, F.; Gasparyan, A.; Austrich-Olivares, A.; Manzanares, J. Biomarkers in Psychiatry: Concept, Definition, Types and Relevance to the Clinical Reality. Front. Psychiatry 2020, 11, 432. [Google Scholar] [CrossRef] [PubMed]
- Cattell, J.M. Early psychological laboratories. Science 1928, 67, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Bollen, K.A. Latent Variables in Psychology and the Social Sciences. Annu. Rev. Psychol. 2002, 53, 605–634. [Google Scholar] [CrossRef] [PubMed]
- Fava, G.A. Forty Years of Clinimetrics. Psychother. Psychosom. 2022, 91, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Fava, G.A.; Ruini, C.; Rafanelli, C. Psychometric Theory Is an Obstacle to the Progress of Clinical Research. Psychother. Psychosom. 2004, 73, 145–148. [Google Scholar] [CrossRef] [PubMed]
- Faravelli, C. Assessment of psychopathology. Psychother. Psychosom. 2004, 73, 139–141. [Google Scholar] [CrossRef] [PubMed]
- Feinstein, A.R. The pre-therapeutic classification of co-morbidity in chronic diseases. J. Chronic Dis. 1970, 23, 455–468. [Google Scholar] [CrossRef]
- Fava, G.A.; Tomba, E.; Sonino, N. Clinimetrics: The science of clinical measurements. Int. J. Clin. Pract. 2012, 66, 11–15. [Google Scholar] [CrossRef]
- Feinstein, A.R. An additional basic science for clinical medicine: IV. The development of clinimetrics. Ann. Intern. Med. 1983, 99, 843–848. [Google Scholar] [CrossRef]
- Feinstein, A.R. Clinimetrics; Yale University Press: New Haven, CT, USA, 1987. [Google Scholar]
- Fava, G.A.; Rafanelli, C.; Tomba, E. The clinical process in psychiatry: A clinimetric approach. J. Clin. Psychiatry 2012, 73, 177–184. [Google Scholar] [CrossRef]
- Tomba, E.; Bech, P. Clinimetrics and clinical psychometrics: Macro- and micro-analysis. Psychother. Psychosom. 2012, 81, 333–343. [Google Scholar] [CrossRef]
- Feinstein, A.R.T. Duckett Jones Memorial Lecture. The Jones criteria and the challenges of clinimetrics. Circulation 1982, 66, 1–5. [Google Scholar] [CrossRef]
- The Criteria Committee of the New York Heart Association. Diseases of the Heart and Blood Vessels. In Nomenclature and Criteria for Diagnosis, 6th ed.; Little, Brown, and Co.: Boston, MA, USA, 1964. [Google Scholar]
- Feinstein, A.R. Multi-item “instruments” vs. Virginia Apgar’s principles of clinimetrics. Arch. Intern. Med. 1999, 159, 125–128. [Google Scholar] [CrossRef]
- Bech, P. Clinical Psychometrics; Wiley-Blackwell: Oxford, UK, 2012. [Google Scholar]
- Emmelkamp, P.M. The additional value of clinimetrics needs to be established rather than assumed. Psychother. Psychosom. 2004, 73, 142–144. [Google Scholar] [CrossRef]
- Tomba, E.; Fava, G.A. The emerging role of Clinimetrics in Psychological Assessment. In Psychological Tests and Testing Research; Lange, M.A., Ed.; Nova Science Publishers: New York, NY, USA, 2007; pp. 129–143. [Google Scholar]
- Streiner, D.L. Clinimetrics vs. psychometrics: An unnecessary distinction. J. Clin. Epidemiol. 2003, 56, 1142–1145, discussion 6–9. [Google Scholar] [CrossRef]
- Streiner, D.L. Test development: Two-sided coin or one-sided Möbius strip? J. Clin. Epidemiol. 2003, 56, 1148–1149. [Google Scholar] [CrossRef]
- Fried, E.I. Problematic assumptions have slowed down depression research: Why symptoms, not syndromes are the way forward. Front. Psychol. 2015, 6, 309. [Google Scholar] [CrossRef]
- Borsboom, D. Psychometric perspectives on diagnostic systems. J. Clin. Psychol. 2008, 64, 1089–1108. [Google Scholar] [CrossRef]
- Cramer, A.O.; Waldorp, L.J.; van der Maas, H.L.; Borsboom, D. Comorbidity: A network perspective. Behav. Brain Sci. 2010, 33, 137–150, discussion 50–93. [Google Scholar] [CrossRef]
- Schmittmann, V.D.; Cramer, A.O.J.; Waldorp, L.J.; Epskamp, S.; Kievit, R.A.; Borsboom, D. Deconstructing the construct: A network perspective on psychological phenomena. New Ideas Psychol. 2013, 31, 43–53. [Google Scholar] [CrossRef]
- Borsboom, D. A network theory of mental disorders. World Psychiatry 2017, 16, 5–13. [Google Scholar] [CrossRef]
- van Bork, R.; van Borkulo, C.D.; Waldorp, L.J.; Cramer, A.O.J.; Borsboom, D. Network Models for Clinical Psychology. In Stevens’ Handbook of Experimental Psychology and Cognitive Neuroscience; John Wiley & Sons: Hoboken, NJ, USA, 2018; pp. 1–35. [Google Scholar]
- Borsboom, D.; Deserno, M.K.; Rhemtulla, M.; Epskamp, S.; Fried, E.I.; McNally, R.J.; Robinaugh, D.J.; Perugini, M.; Dalege, J.; Costantini, G.; et al. Network analysis of multivariate data in psychological science. Nat. Rev. Methods Primers 2021, 1, 58. [Google Scholar] [CrossRef]
- Hyland, M.E. The Origins of Health and Disease; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]
- Robinaugh, D.J.; Hoekstra, R.H.A.; Toner, E.R.; Borsboom, D. The network approach to psychopathology: A review of the literature 2008–2018 and an agenda for future research. Psychol. Med. 2020, 50, 353–366. [Google Scholar] [CrossRef]
- Tomei, G.; Pieroni, M.F.; Tomba, E. Network analysis studies in patients with eating disorders: A systematic review and methodological quality assessment. Int. J. Eat. Disord. 2022, 55, 1641–1669. [Google Scholar] [CrossRef]
- Burger, J.; Isvoranu, A.M.; Lunansky, G.; Haslbeck, J.M.B.; Epskamp, S.; Hoekstra, R.H.A.; Fried, E.I.; Borsboom, D.; Blanken, T.F. Reporting standards for psychological network analyses in cross-sectional data. Psychol. Methods 2022, 28, 806–824. [Google Scholar] [CrossRef]
- Fonseca-Pedrero, E. Network analysis: A new way of understanding psychopathology? Rev. Psiquiatr. Salud. Ment. 2017, 10, 206–215. [Google Scholar] [CrossRef]
- Malgaroli, M.; Calderon, A.; Bonanno, G.A. Networks of major depressive disorder: A systematic review. Clin. Psychol. Rev. 2021, 85, 102000. [Google Scholar] [CrossRef]
- Contreras, A.; Nieto, I.; Valiente, C.; Espinosa, R.; Vazquez, C. The Study of Psychopathology from the Network Analysis Perspective: A Systematic Review. Psychother. Psychosom. 2019, 88, 71–83. [Google Scholar] [CrossRef]
- Monteleone, A.M.; Cascino, G. A systematic review of network analysis studies in eating disorders: Is time to broaden the core psychopathology to non specific symptoms. Eur. Eat. Disord. Rev. 2021, 29, 531–547. [Google Scholar] [CrossRef]
- Lo Buglio, G.; Pontillo, M.; Cerasti, E.; Polari, A.; Schiano Lomoriello, A.; Vicari, S.; Lingiardi, V.; Boldrini, T.; Solmi, M. A network analysis of anxiety, depressive, and psychotic symptoms and functioning in children and adolescents at clinical high risk for psychosis. Front. Psychiatry 2022, 13, 1016154. [Google Scholar] [CrossRef]
- Griffiths, S.L.; Leighton, S.P.; Mallikarjun, P.K.; Blake, G.; Everard, L.; Jones, P.B.; Fowler, D.; Hodgekins, J.; Amos, T.; Freemantle, N.; et al. Structure and stability of symptoms in first episode psychosis: A longitudinal network approach. Transl. Psychiatry 2021, 11, 567. [Google Scholar] [CrossRef]
- Isvoranu, A.-M.; Boyette, L.-L.; Guloksuz, S.; Borsboom, D. Symptom network models of psychosis. In Psychotic Disorders: Comprehensive Conceptualization and Treatments; Oxford University Press: New York, NY, USA, 2021; pp. 70–78. [Google Scholar]
- Segal, A.; Wald, I.; Lubin, G.; Fruchter, E.; Ginat, K.; Ben Yehuda, A.; Pine, D.S.; Bar-Haim, Y. Changes in the dynamic network structure of PTSD symptoms pre-to-post combat. Psychol. Med. 2020, 50, 746–753. [Google Scholar] [CrossRef]
- Liebman, R.E.; Becker, K.R.; Smith, K.E.; Cao, L.; Keshishian, A.C.; Crosby, R.D.; Eddy, K.T.; Thomas, J.J. Network Analysis of Posttraumatic Stress and Eating Disorder Symptoms in a Community Sample of Adults Exposed to Childhood Abuse. J. Trauma. Stress 2021, 34, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Birkeland, M.S.; Greene, T.; Spiller, T.R. The network approach to posttraumatic stress disorder: A systematic review. Eur. J. Psychotraumatol. 2020, 11, 1700614. [Google Scholar] [CrossRef] [PubMed]
- Gernigon, C.; Den Hartigh, R.J.R.; Vallacher, R.R.; van Geert, P.L.C. How the Complexity of Psychological Processes Reframes the Issue of Reproducibility in Psychological Science. Perspect. Psychol. Sci. 2023, 17456916231187324. [Google Scholar] [CrossRef] [PubMed]
- Paré, G.; Trudel, M.-C.; Jaana, M.; Kitsiou, S. Synthesizing information systems knowledge: A typology of literature reviews. Inf. Manag. 2015, 52, 183–199. [Google Scholar] [CrossRef]
- Fava, G.A.; Kellner, R. Staging: A neglected dimension in psychiatric classification. Acta Psychiatr. Scand. 1993, 87, 225–230. [Google Scholar] [CrossRef]
- Fava, G.A.; Belaise, C. A discussion on the role of clinimetrics and the misleading effects of psychometric theory. J. Clin. Epidemiol. 2005, 58, 753–756. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef]
- Bringmann, L.F.; Pe, M.L.; Vissers, N.; Ceulemans, E.; Borsboom, D.; Vanpaemel, W.; Tuerlinckx, F.; Kuppens, P. Assessing Temporal Emotion Dynamics Using Networks. Assessment 2016, 23, 425–435. [Google Scholar] [CrossRef]
- von Klipstein, L.; Riese, H.; van der Veen, D.C.; Servaas, M.N.; Schoevers, R.A. Using person-specific networks in psychotherapy: Challenges, limitations, and how we could use them anyway. BMC Med. 2020, 18, 345. [Google Scholar] [CrossRef]
- Bringmann, L.F.; Elmer, T.; Epskamp, S.; Krause, R.W.; Schoch, D.; Wichers, M.; Wigman, J.T.W.; Snippe, E. What do centrality measures measure in psychological networks? J. Abnorm. Psychol. 2019, 128, 892–903. [Google Scholar] [CrossRef] [PubMed]
- Flake, J.K.; Fried, E.I. Measurement Schmeasurement: Questionable Measurement Practices and How to Avoid Them. Adv. Methods Pract. Psychol. Sci. 2020, 3, 456–465. [Google Scholar] [CrossRef]
- Feinstein, A.R. An analysis of diagnostic reasoning. I. The domains and disorders of clinical macrobiology. Yale J. Biol. Med. 1973, 46, 212–232. [Google Scholar] [PubMed]
- Guidi, J.; Tomba, E.; Cosci, F.; Park, S.K.; Fava, G.A. The Role of Staging in Planning Psychotherapeutic Interventions in Depression. J. Clin. Psychiatry 2017, 78, 456–463. [Google Scholar] [CrossRef]
- Cosci, F.; Fava, G.A. Staging of mental disorders: Systematic review. Psychother. Psychosom. 2013, 82, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Jordan, D.G.; Winer, E.S.; Salem, T. The current status of temporal network analysis for clinical science: Considerations as the paradigm shifts? J. Clin. Psychol. 2020, 76, 1591–1612. [Google Scholar] [CrossRef]
- Fava, G.A.; Tomba, E.; Grandi, S. The road to recovery from depression-don’t drive today with yesterday’s map. Psychother. Psychosom. 2007, 76, 260–265. [Google Scholar] [CrossRef]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Bogenschutz, M.P.; Nurnberg, H.G. Theoretical and methodological issues in psychiatric comorbidity. Harv. Rev. Psychiatry 2000, 8, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Fava, G.A.; Tossani, E.; Bech, P.; Berrocal, C.; Chouinard, G.; Csillag, C.; Wittchen, H.; Rief, W. Emerging clinical trends and perspectives on comorbid patterns of mental disorders in research. Int. J. Methods Psychiatr. Res. 2014, 23 (Suppl. S1), 92–101. [Google Scholar] [CrossRef] [PubMed]
- Mansueto, A.C.; Wiers, R.W.; van Weert, J.C.M.; Schouten, B.C.; Epskamp, S. Investigating the feasibility of idiographic network models. Psychol. Methods 2022, 28, 1052–1068. [Google Scholar] [CrossRef] [PubMed]
- Fried, E.I.; Cramer, A.O.J. Moving Forward: Challenges and Directions for Psychopathological Network Theory and Methodology. Perspect. Psychol. Sci. 2017, 12, 999–1020. [Google Scholar] [CrossRef]
- Fried, E.I.; van Borkulo, C.D.; Cramer, A.O.; Boschloo, L.; Schoevers, R.A.; Borsboom, D. Mental disorders as networks of problems: A review of recent insights. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 1–10. [Google Scholar] [CrossRef]
- van Loo, H.M.; Romeijn, J.W. Psychiatric comorbidity: Fact or artifact? Theor. Med. Bioeth. 2015, 36, 41–60. [Google Scholar] [CrossRef]
- Ridley, C.R.; Jeffrey, C.E. The Conceptual Framework of Thematic Mapping in Case Conceptualization. J. Clin. Psychol. 2017, 73, 376–392. [Google Scholar] [CrossRef]
- Roefs, A.; Fried, E.I.; Kindt, M.; Martijn, C.; Elzinga, B.; Evers, A.W.M.; Wiers, R.W.; Borsboom, D.; Jansen, A. A new science of mental disorders: Using personalised, transdiagnostic, dynamical systems to understand, model, diagnose and treat psychopathology. Behav. Res. Ther. 2022, 153, 104096. [Google Scholar] [CrossRef]
- Cosci, F. Clinimetric Perspectives in Clinical Psychology and Psychiatry. Psychother. Psychosom. 2021, 90, 217–221. [Google Scholar] [CrossRef]
- von Klipstein, L.; Borsboom, D.; Arntz, A. The exploratory value of cross-sectional partial correlation networks: Predicting relationships between change trajectories in borderline personality disorder. PLoS ONE 2021, 16, e0254496. [Google Scholar] [CrossRef] [PubMed]
- Boyle, G.J. Does item homogeneity indicate internal consistency or item redundancy in psychometric scales? Personal. Individ. Differ. 1991, 12, 291–294. [Google Scholar] [CrossRef]
- Cattel, R.B. The Scientific Use of Factor Analysis in Behavioral and Life Sciences; Springer: New York, NY, USA, 1978. [Google Scholar]
- Fried, E.I.; van Borkulo, C.D.; Epskamp, S. On the Importance of Estimating Parameter Uncertainty in Network Psychometrics: A Response to Forbes et al. (2019). Multivar. Behav. Res. 2021, 56, 243–248. [Google Scholar] [CrossRef]
- Fava, G.A.; Tomba, E. New modalities of assessment and treatment planning in depression: The sequential approach. CNS Drugs 2010, 24, 453–465. [Google Scholar] [CrossRef] [PubMed]
- Persons, J.B.; Mooney, K.A.; Padesky, C.A. Interrater relability of cognitive-behavioral case formulations. Cogn. Ther. Res. 1995, 19, 21–34. [Google Scholar] [CrossRef]
- Beutler, L.E.; Mohr, D.C. The integrative clinical interview. In Integrative Assessment of Adult Personality, 2nd ed.; Beutler, L.E., Groth-Marnat, G., Eds.; Guilford: New York, NY, USA, 2010. [Google Scholar]
- van de Leemput, I.A.; Wichers, M.; Cramer, A.O.; Borsboom, D.; Tuerlinckx, F.; Kuppens, P.; van Nes, E.H.; Viechtbauer, W.; Giltay, E.J.; Aggen, S.H.; et al. Critical slowing down as early warning for the onset and termination of depression. Proc. Natl. Acad. Sci. USA 2014, 111, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Tomba, E.; Tecuta, L.; Crocetti, E.; Squarcio, F.; Tomei, G. Residual eating disorder symptoms and clinical features in remitted and recovered eating disorder patients: A systematic review with meta-analysis. Int. J. Eat. Disord. 2019, 52, 759–776. [Google Scholar] [CrossRef]
- Maj, M. “Psychiatric comorbidity”: An artefact of current diagnostic systems? Br. J. Psychiatry 2005, 186, 182–184. [Google Scholar] [CrossRef]
- Vella, G.; Aragona, M.; Alliani, D. The complexity of psychiatric comorbidity: A conceptual and methodological discussion. Psychopathology 2000, 33, 25–30. [Google Scholar] [CrossRef]
- Jones, P.J.; Ma, R.; McNally, R.J. Bridge Centrality: A Network Approach to Understanding Comorbidity. Multivar. Behav. Res. 2021, 56, 353–367. [Google Scholar] [CrossRef]
- McNally, R.J. Can network analysis transform psychopathology? Behav. Res. Ther. 2016, 86, 95–104. [Google Scholar] [CrossRef]
- Padesky, C.A.; Mooney, K.A. Presenting the cognitive model to clients. Int. Cogn. Ther. Newsl. 1990, 6, 13–14. [Google Scholar]
- Kuyken, W.; Fothergill, C.D.; Musa, M.; Chadwick, P. The reliability and quality of cognitive case formulation. Behav. Res. Ther. 2005, 43, 1187–1201. [Google Scholar] [CrossRef] [PubMed]
- Kuyken, W.; Padesky, C.A.; Dudley, R. The Science and Practice of Case Conceptualization. Behav. Cogn. Psychother. 2008, 36, 757–768. [Google Scholar] [CrossRef]
| True Comorbidity | A true relationship between two discrete disorders. Can be either the result of two disorders sharing common etiologic factors or a common diathesis, while remaining two distinct entities, or when one disorder causes (or increases the probability of) the other. |
| Spurious comorbidity | An apparent relationship between two diagnoses that does not reflect the true relationship between the two disorders or diseases. It can be the result of different phenotypic expressions of the same disease, leading to apparent comorbidity, or when one disorder is, in fact, a prodrome or an attenuated form of the other disorder, or again when a disorder might be a subcategory nested within the more general category defining another disorder. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomba, E.; Tomei, G. Bridging Perspectives: Exploring the Convergence of Clinimetrics and Network Theory in Mental Health Assessment and Conceptualization. J. Clin. Med. 2024, 13, 1814. https://doi.org/10.3390/jcm13061814
Tomba E, Tomei G. Bridging Perspectives: Exploring the Convergence of Clinimetrics and Network Theory in Mental Health Assessment and Conceptualization. Journal of Clinical Medicine. 2024; 13(6):1814. https://doi.org/10.3390/jcm13061814
Chicago/Turabian StyleTomba, Elena, and Giuliano Tomei. 2024. "Bridging Perspectives: Exploring the Convergence of Clinimetrics and Network Theory in Mental Health Assessment and Conceptualization" Journal of Clinical Medicine 13, no. 6: 1814. https://doi.org/10.3390/jcm13061814




