Comparison of Oncologic Outcomes in Laparoscopic versus Open Surgery for Non-Metastatic Colorectal Cancer: Personal Experience in a Single Institution
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Study Population
2.3. Pre-Operative Staging Work-Up
2.4. Surgical Techniques
2.5. Post-Operative Management
2.6. Post-Operative Follow-Up
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Patients
3.2. Surgical Outcomes
3.3. Cancer-Free Survival Rates and Tumor Recurrence Incidence
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Guo, D.Y.; Eteuati, J.; Nguyen, M.H.; Lloyd, D.; Ragg, J.L. Laparoscopic assisted colectomy: Experience from a rural centre. ANZ J. Surg. 2007, 77, 283–286. [Google Scholar] [CrossRef] [PubMed]
- Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N. Engl. J. Med. 2004, 350, 2050–2059. [Google Scholar] [CrossRef] [PubMed]
- Leung, K.L.; Kwok, S.P.; Lam, S.C.; Lee, J.F.; Yiu, R.Y.; Ng, S.S.; Lai, P.B.; Lau, W.Y. Laparoscopic resection of rectosigmoid carcinoma: Prospective randomised trial. Lancet 2004, 363, 1187–1192. [Google Scholar] [CrossRef]
- Guillou, P.J.; Quirke, P.; Thorpe, H.; Walker, J.; Jayne, D.G.; Smith, A.M.; Heath, R.M.; Brown, J.M.; MRC CLASICC Trial Group. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): Multicentre, randomised controlled trial. Lancet 2005, 365, 1718–1726. [Google Scholar] [CrossRef]
- Liang, J.T.; Huang, K.C.; Lai, H.S.; Lee, P.H.; Jeng, Y.M. Oncologic results of laparoscopic versus conventional open surgery for stage II or III left-sided colon cancers: A randomized controlled trial. Ann. Surg. Oncol. 2007, 14, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Veldkamp, R.; Kuhry, E.; Hop, W.C.; Jeekel, J.; Kazemier, G.; Bonjer, H.J.; Haglind, E.; Påhlman, L.; Cuesta, M.A.; Msika, S.; et al. Laparoscopic surgery versus open surgery for colon cancer: Short-term outcomes of a randomised trial. Lancet Oncol. 2005, 6, 477–484. [Google Scholar] [PubMed]
- Jayne, D.G.; Guillou, P.J.; Thorpe, H.; Quirke, P.; Copeland, J.; Smith, A.M.; Heath, R.M.; Brown, J.M.; UK MRC CLASICC Trial Group. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J. Clin. Oncol. 2007, 25, 3061–3068. [Google Scholar] [CrossRef]
- Colon Cancer Laparoscopic or Open Resection Study Group; Buunen, M.; Veldkamp, R.; Hop, W.C.; Kuhry, E.; Jeekel, J.; Haglind, E.; Påhlman, L.; Cuesta, M.A.; Msika, S.; et al. Survival after laparoscopic surgery versus open surgery for colon cancer: Long-term outcome of a randomised clinical trial. Lancet Oncol. 2009, 10, 44–52. [Google Scholar]
- Hemandas, A.K.; Abdelrahman, T.; Flashman, K.G.; Skull, A.J.; Senapati, A.; O’Leary, D.P.; Parvaiz, A. Laparoscopic colorectal surgery produces better outcomes for high risk cancer patients compared to open surgery. Ann. Surg. 2010, 252, 84–89. [Google Scholar] [CrossRef]
- Bagshaw, P.F.; Allardyce, R.A.; Frampton, C.M.; Frizelle, F.A.; Hewett, P.J.; McMurrick, P.J.; Rieger, N.A.; Smith, J.S.; Solomon, M.J.; Stevenson, A.R.; et al. Long-term outcomes of the australasian randomized clinical trial comparing laparoscopic and conventional open surgical treatments for colon cancer: The Australasian Laparoscopic Colon Cancer Study trial. Ann. Surg. 2012, 256, 915–919. [Google Scholar] [CrossRef]
- Cummings, L.C.; Delaney, C.P.; Cooper, G.S. Laparoscopic versus open colectomy for colon cancer in an older population: A cohort study. World J. Surg. Oncol. 2012, 10, 31. [Google Scholar] [CrossRef] [PubMed]
- Hinoi, T.; Kawaguchi, Y.; Hattori, M.; Okajima, M.; Ohdan, H.; Yamamoto, S.; Hasegawa, H.; Horie, H.; Murata, K.; Yamaguchi, S.; et al. Laparoscopic versus open surgery for colorectal cancer in elderly patients: A multicenter matched case-control study. Ann. Surg. Oncol. 2015, 22, 2040–2050. [Google Scholar] [CrossRef] [PubMed]
- Hutter, M.M.; Randall, S.; Khuri, S.F.; Henderson, W.G.; Abbott, W.M.; Warshaw, A.L. Laparoscopic versus open gastric bypass for morbid obesity: A multicenter, prospective, risk-adjusted analysis from the National Surgical Quality Improvement Program. Ann. Surg. 2006, 243, 657–662. [Google Scholar] [CrossRef] [PubMed]
- Weeks, J.C.; Nelson, H.; Gelber, S.; Sargent, D.; Schroeder, G.; Clinical Outcomes of Surgical Therapy (COST) Study Group. Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: A randomized trial. JAMA 2002, 287, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Tong, D.K.; Law, W.L. Laparoscopic versus open right hemicolectomy for carcinoma of the colon. JSLS 2007, 11, 76–80. [Google Scholar] [PubMed]
- Steele, S.R.; Brown, T.A.; Rush, R.M.; Martin, M.J. Laparoscopic vs open colectomy for colon cancer: Results from a large nationwide population-based analysis. J. Gastrointest. Surg. 2008, 12, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, G.D.; Heise, C.; Rajamanickam, V.; Harms, B.; Foley, E.F. Laparoscopy decreases postoperative complication rates after abdominal colectomy: Results from the national surgical quality improvement program. Ann. Surg. 2009, 249, 596–601. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Li, G.; Chen, P.; Yu, J. Laparoscopic versus open colorectal resection for cancer: A meta-analysis of results of randomized controlled trials on recurrence. Eur. J. Surg. Oncol. 2008, 34, 1217–1224. [Google Scholar] [CrossRef]
- Cianchi, F.; Trallori, G.; Mallardi, B.; Macrì, G.; Biagini, M.R.; Lami, G.; Indennitate, G.; Bagnoli, S.; Bonanomi, A.; Messerini, L.; et al. Survival after laparoscopic and open surgery for colon cancer: A comparative, single-institution study. BMC Surg. 2015, 15, 33. [Google Scholar] [CrossRef]
- Neudecker, J.; Klein, F.; Bittner, R.; Carus, T.; Stroux, A.; Schwenk, W.; LAPKON II Trialists. Short-term outcomes from a prospective randomized trial comparing laparoscopic and open surgery for colorectal cancer. Br. J. Surg. 2009, 96, 1458–1467. [Google Scholar] [CrossRef]
- Biondi, A.; Grosso, G.; Mistretta, A.; Marventano, S.; Toscano, C.; Gruttadauria, S.; Basile, F. Laparoscopic-assisted versus open surgery for colorectal cancer: Short- and long-term outcomes comparison. J. Laparoendosc. Adv. Surg. Tech. A 2013, 23, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Małczak, P.; Mizera, M.; Torbicz, G.; Witowski, J.; Major, P.; Pisarska, M.; Wysocki, M.; Strzałka, M.; Budzyński, A.; Pędziwiatr, M. Is the laparoscopic approach for rectal cancer superior to open surgery? A systematic review and meta-analysis on short-term surgical outcomes. Wideochir. Inne Tech. Maloinwazyjne 2018, 13, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Tjandra, J.J.; Chan, M.K. Systematic review on the short-term outcome of laparoscopic resection for colon and rectosigmoid cancer. Colorectal. Dis. 2006, 8, 375–388. [Google Scholar] [CrossRef] [PubMed]
- Senagore, A.J.; Stulberg, J.J.; Byrnes, J.; Delaney, C.P. A national comparison of laparoscopic vs. open colectomy using the National Surgical Quality Improvement Project data. Dis. Colon Rectum 2009, 52, 183–186. [Google Scholar] [CrossRef]
- Law, W.L.; Poon, J.T.; Fan, J.K.; Lo, S.H. Comparison of outcome of open and laparoscopic resection for stage II and stage III rectal cancer. Ann. Surg. Oncol. 2009, 16, 1488–1493. [Google Scholar] [CrossRef] [PubMed]
- Lacy, A.M.; Delgado, S.; Castells, A.; Prins, H.A.; Arroyo, V.; Ibarzabal, A.; Pique, J.M. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann. Surg. 2008, 248, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Capussotti, L.; Massucco, P.; Muratore, A.; Amisano, M.; Bima, C.; Zorzi, D. Laparoscopy as a prognostic factor in curative resection for node positive colorectal cancer: Results for a single-institution nonrandomized prospective trial. Surg. Endosc. 2004, 18, 1130–1135. [Google Scholar] [CrossRef]
- Law, W.L.; Poon, J.T.; Fan, J.K.; Lo, O.S. Survival following laparoscopic versus open resection for colorectal cancer. Int. J. Colorectal. Dis. 2012, 27, 1077–1085. [Google Scholar] [CrossRef]
- Li, J.; Guo, H.; Guan, X.D.; Cai, C.N.; Yang, L.K.; Li, Y.C.; Zhu, Y.H.; Li, P.P.; Liu, X.L.; Yang, D.J. The impact of laparoscopic converted to open colectomy on short-term and oncologic outcomes for colon cancer. J. Gastrointest. Surg. 2015, 19, 335–343. [Google Scholar] [CrossRef]
- Patankar, S.K.; Larach, S.W.; Ferrara, A.; Williamson, P.R.; Gallagher, J.T.; DeJesus, S.; Narayanan, S. Prospective comparison of laparoscopic vs. open resections for colorectal adenocarcinoma over a ten-year period. Dis. Colon Rectum 2003, 46, 601–611. [Google Scholar] [CrossRef]
- Lujan, H.J.; Plasencia, G.; Jacobs, M.; Viamonte, M., III; Hartmann, R.F. Long-term survival after laparoscopic colon resection for cancer: Complete five-year follow-up. Dis. Colon Rectum 2002, 45, 491–501. [Google Scholar] [CrossRef] [PubMed]
- Edge, S.B.; Compton, C.C. The American Joint Committee on Cancer: The 7th edition of the AJCC cancer staging manual and the future of TNM. Ann. Surg. Oncol. 2010, 17, 1471–1474. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.B.; Zhang, L.Y.; Li, Y.F.; Zhou, Z.W.; Keshari, R.P.; Xu, R.H. Ratio of metastatic to resected lymph nodes enhances to predict survival in patients with stage III colorectal cancer. Ann. Surg. Oncol. 2011, 18, 1568–1574. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.W.; Kim, Y.J.; Kim, H.R. Ratio of metastatic to resected lymph nodes as a prognostic factor in node-positive colorectal cancer. Ann. Surg. Oncol. 2010, 17, 2640–2646. [Google Scholar] [CrossRef]
- Wang, J.; Hassett, J.M.; Dayton, M.T.; Kulaylat, M.N. Lymph node ratio: Role in the staging of node-positive colon cancer. Ann. Surg. Oncol. 2008, 15, 1600–1608. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, R.; Itah, R.; Ghinea, R.; Sacham-Shmueli, E.; Inbar, R.; Avital, S. Metastatic lymph node ratio (LNR) as a prognostic variable in colorectal cancer patients undergoing laparoscopic resection. Tech. Coloproctol. 2011, 15, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Li Destri, G.; Di Carlo, I.; Scilletta, R.; Scilletta, B.; Puleo, S. Colorectal cancer and lymph nodes: The obsession with the number 12. World J. Gastroenterol. 2014, 20, 1951–1960. [Google Scholar]
- Novitsky, Y.W.; Litwin, D.E.; Callery, M.P. The net immunologic advantage of laparoscopic surgery. Surg. Endosc. 2004, 18, 1411–1419. [Google Scholar] [CrossRef]
- Lacy, A.M.; García-Valdecasas, J.C.; Delgado, S.; Castells, A.; Taurá, P.; Piqué, J.M.; Visa, J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: A randomised trial. Lancet 2002, 359, 2224–2229. [Google Scholar] [CrossRef]
- Laurent, C.; Leblanc, F.; Wütrich, P.; Scheffler, M.; Rullier, E. Laparoscopic versus open surgery for rectal cancer: Long-term oncologic results. Ann. Surg. 2009, 250, 54–61. [Google Scholar] [CrossRef]
- Whelan, R.L.; Franklin, M.; Holubar, S.D.; Donahue, J.; Fowler, R.; Munger, C.; Doorman, J.; Balli, J.E.; Glass, J.; Gonzalez, J.J.; et al. Postoperative cell mediated immune response is better preserved after laparoscopic vs open colorectal resection in humans. Surg. Endosc. 2003, 17, 972–978. [Google Scholar] [CrossRef] [PubMed]
- Wichmann, M.W.; Hüttl, T.P.; Winter, H.; Spelsberg, F.; Angele, M.K.; Heiss, M.M.; Jauch, K.W. Immunological effects of laparoscopic vs open colorectal surgery: A prospective clinical study. Arch. Surg. 2005, 140, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Bessa, X.; Castells, A.; Lacy, A.M.; Elizalde, J.I.; Delgado, S.; Boix, L.; Piñol, V.; Pellisé, M.; García-Valdecasas, J.C.; Piqué, J.M. Laparoscopic-assisted vs. open colectomy for colorectal cancer: Influence on neoplastic cell mobilization. J. Gastrointest. Surg. 2001, 5, 66–73. [Google Scholar] [CrossRef]
- Hsu, T.C. Feasibility of colectomy with mini-incision. Am. J. Surg. 2005, 190, 48–50. [Google Scholar] [CrossRef] [PubMed]
- Hoyuela, C.; Juvany, M.; Carvajal, F. Single-incision laparoscopy versus standard laparoscopy for colorectal surgery: A systematic review and meta-analysis. Am. J. Surg. 2017, 214, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Acuna, S.A.; Elmi, M.; Shah, P.S.; Coburn, N.G.; Quereshy, F.A. Preoperative localization of colorectal cancer: A systematic review and meta-analysis. Surg. Endosc. 2017, 31, 2366–2379. [Google Scholar] [CrossRef] [PubMed]
- Nishigori, N.; Koyama, F.; Nakagawa, T.; Nakamura, S.; Ueda, T.; Inoue, T.; Kawasaki, K.; Obara, S.; Nakamoto, T.; Fujii, H.; et al. Visualization of Lymph/Blood Flow in Laparoscopic Colorectal Cancer Surgery by ICG Fluorescence Imaging (Lap-IGFI). Ann. Surg. Oncol. 2016, 23, S266–S274. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.C.; Ng, D.C.; Tsang, W.W.; Tang, W.L.; Yau, K.K.; Cheung, H.Y.; Wong, J.C.; Li, M.K. Hand-assisted laparoscopic versus open right colectomy: A randomized controlled trial. Ann. Surg. 2007, 246, 728–733. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Watanabe, M. Present laparoscopic surgery for colorectal cancer in Japan. World J. Clin. Oncol. 2016, 7, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Tekkis, P.P.; Senagore, A.J.; Delaney, C.P.; Fazio, V.W. Evaluation of the learning curve in laparoscopic colorectal surgery: Comparison of right-sided and left-sided resections. Ann. Surg. 2005, 242, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Morneau, M.; Boulanger, J.; Charlebois, P.; Latulippe, J.F.; Lougnarath, R.; Thibault, C.; Gervais, N.; Comité de l’Évolution des Pratiques en Oncologie. Laparoscopic versus open surgery for the treatment of colorectal cancer: A literature review and recommendations from the Comité de l’évolution des pratiques en oncologie. Can. J. Surg. 2013, 56, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Fleshman, J.; Sargent, D.J.; Green, E.; Anvari, M.; Stryker, S.J.; Beart, R.W., Jr.; Hellinger, M.; Flanagan, R., Jr.; Peters, W.; Nelson, H.; et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann. Surg. 2007, 246, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Hyman, N.; Manchester, T.L.; Osler, T.; Burns, B.; Cataldo, P.A. Anastomotic leaks after intestinal anastomosis: it’s later than you think. Ann. Surg. 2007, 245, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Pickleman, J.; Watson, W.; Cunningham, J.; Fisher, S.G.; Gamelli, R. The failed gastrointestinal anastomosis: An inevitable catastrophe? J. Am. Coll. Surg. 1999, 188, 473–482. [Google Scholar] [CrossRef]
- Bruce, J.; Krukowski, Z.H.; Al-Khairy, G.; Russell, E.M.; Park, K.G. Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br. J. Surg. 2001, 88, 1157–1168. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, Z.; Li, J. The current status of treatment for colorectal cancer in China: A systematic review. Medicine 2017, 96, e8242. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Ren, L. China Guideline for Diagnosis and Comprehensive Treatment of Colorectal Liver Metastases (Version 2018). Zhonghua Wei Chang Wai Ke Za Zhi 2018, 21, 601–626. [Google Scholar] [PubMed]
- Athanasakis, E.; Xenaki, S.; Venianaki, M.; Chalkiadakis, G.; Chrysos, E. Newly recognized extratumoral features of colorectal cancer challenge the current tumor-node-metastasis staging system. Ann. Gastroenterol. 2018, 31, 525–534. [Google Scholar] [CrossRef]
- Quirke, P.; Williams, G.T.; Ectors, N.; Ensari, A.; Piard, F.; Nagtegaal, I. The future of the TNM staging system in colorectal cancer: Time for a debate? Lancet Oncol. 2007, 8, 651–657. [Google Scholar] [CrossRef]
- Maguire, A.; Sheahan, K. Controversies in the pathological assessment of colorectal cancer. World J. Gastroenterol. 2014, 20, 9850–9861. [Google Scholar] [CrossRef]
- Puppa, G.; Sonzogni, A.; Colombari, R.; Pelosi, G. TNM staging system of colorectal carcinoma: A critical appraisal of challenging issues. Arch. Pathol. Lab. Med. 2010, 134, 837–852. [Google Scholar] [PubMed]
- Lennon, A.M.; Mulcahy, H.E.; Hyland, J.M.; Lowry, C.; White, A.; Fennelly, D.; Murphy, J.J.; O’Donoghue, D.P.; Sheahan, K. Peritoneal involvement in stage II colon cancer. Am. J. Clin. Pathol. 2003, 119, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Kojima, M.; Nakajima, K.; Ishii, G.; Saito, N.; Ochiai, A. Peritoneal elastic laminal invasion of colorectal cancer: The diagnostic utility and clinicopathologic relationship. Am. J. Surg. Pathol. 2010, 34, 1351–1360. [Google Scholar] [CrossRef] [PubMed]
- Burdy, G.; Panis, Y.; Alves, A.; Nemeth, J.; Lavergne-Slove, A.; Valleur, P. Identifying patients with T3-T4 node-negative colon cancer at high risk of recurrence. Dis. Colon Rectum 2001, 44, 1682–1688. [Google Scholar] [CrossRef] [PubMed]
- Merkel, S.; Wein, A.; Günther, K.; Papadopoulos, T.; Hohenberger, W.; Hermanek, P. High-risk groups of patients with stage II colon carcinoma. Cancer 2001, 92, 1435–1443. [Google Scholar] [CrossRef]
- Morris, M.; Platell, C.; de Boer, B.; McCaul, K.; Iacopetta, B. Population-based study of prognostic factors in stage II colonic cancer. Br. J. Surg. 2006, 93, 866–871. [Google Scholar] [CrossRef] [PubMed]
- Newland, R.C.; Dent, O.F.; Chapuis, P.H.; Bokey, L. Survival after curative resection of lymph node negative colorectal carcinoma. A prospective study of 910 patients. Cancer 1995, 76, 564–571. [Google Scholar] [CrossRef]
- Petersen, V.C.; Baxter, K.J.; Love, S.B.; Shepherd, N.A. Identification of objective pathological prognostic determinants and models of prognosis in Dukes’ B colon cancer. Gut 2002, 51, 65–69. [Google Scholar] [CrossRef]
- Grin, A.; Messenger, D.E.; Cook, M.; O’Connor, B.I.; Hafezi, S.; El-Zimaity, H.; Kirsch, R. Peritoneal elastic lamina invasion: Limitations in its use as a prognostic marker in stage II colorectal cancer. Hum. Pathol. 2013, 44, 2696–2705. [Google Scholar] [CrossRef]
- Grizzi, F.; Celesti, G.; Basso, G.; Laghi, L. Tumor budding as a potential histopathological biomarker in colorectal cancer: Hype or hope? World J. Gastroenterol. 2012, 18, 6532–6536. [Google Scholar] [CrossRef]
- Elfaedy, O.; Owens, P.; Aakif, M.; Mansour, E. Discrepancy in Colorectal Cancer Staging: A Single Center Experience. Available online: http://www.surgeryresearchjournal.com/full-text/wjssr-v1-id1054.php (accessed on 1 March 2019).
- Gong, Y.; Peng, P.; Bao, P.; Zhong, W.; Shi, Y.; Gu, K.; Zheng, Y.; Wu, C.; Cai, S.; Xu, Y.; et al. The Implementation and First-Round Results of a Community-Based Colorectal Cancer Screening Program in Shanghai, China. Oncologist 2018, 23, 928–935. [Google Scholar] [CrossRef] [PubMed]



| Items | LR (n = 188) | OR (n = 163) | p-Value |
|---|---|---|---|
| Gender | 0.435 | ||
| Male | 102 | 87 | |
| Female | 86 | 76 | |
| Age (mean ± SD) | 68.6 ± 12.7 | 71.5 ± 12.1 | 0.23 |
| ASA class | 0.698 | ||
| I | 113 | 92 | |
| II | 75 | 71 | |
| TNM stage (clinical/radiologic) | 0.345 | ||
| 0 | 3 | 0 | |
| I | 70 | 55 | |
| II | 26 | 26 | |
| III | 89 | 82 | |
| TNM stage (pathologic) | 0.344 | ||
| 0 | 3 | 0 | |
| I | 68 | 53 | |
| II | 30 | 29 | |
| III | 87 | 81 | |
| Histopathology | 0.624 | ||
| Well differentiated | 92 | 79 | |
| Moderate differentiated | 71 | 65 | |
| Poorly differentiated | 25 | 19 | |
| Tumor location | 0.431 | ||
| Cecum | 29 | 20 | |
| Ascending colon | 41 | 36 | |
| Transverse colon | 12 | 15 | |
| Descending colon | 21 | 18 | |
| Sigmoid colon | 52 | 45 | |
| Rectum | 33 | 29 | |
| Intervention | 0.720 | ||
| Right hemicolectomy | 65 | 56 | |
| Left hemicolectomy | 24 | 21 | |
| Transverse colectomy | 14 | 10 | |
| Sigmoid colectomy | 50 | 44 | |
| Protectomy | 32 | 27 | |
| Abdominal perineal resection | 3 | 5 | |
| Protective diversional stoma | 13 | 15 | |
| Pre-surgery | 1.000 | ||
| serum CEA level | |||
| <5 | 24 | 13 | |
| ≥5 | 164 | 150 |
| Items | LR (n = 188) | OR (n = 163) | p-Value |
|---|---|---|---|
| Tumor recurrence | 17 (9.0%) | 22 (13.5%) | 0.186 |
| Lymph nodes removed | 16.0 ± 9.2 | 19.2 ± 13.7 | 0.07 |
| Hospitalization (days) | 13.2 ± 4.2 | 18.8 ± 9 | <0.001 ** |
| Blood loss (mL) | 23.5 ± 14.6 | 162.2 ± 63.4 | <0.001 ** |
| Operation time (min) | 191.4 ± 71.1 | 150.8 ± 46.3 | <0.001 ** |
| Postoperative complications | |||
| Total | 8 | 25 | |
| Ileus | 3 | 5 | 0.273 |
| Urinary tract infection | 1 | 5 | <0.001 ** |
| Wound infection | 2 | 7 | <0.001 ** |
| Pneumonia | 2 | 6 | 0.048 * |
| Anastomosis leakage | 0 | 2 | 0.140 |
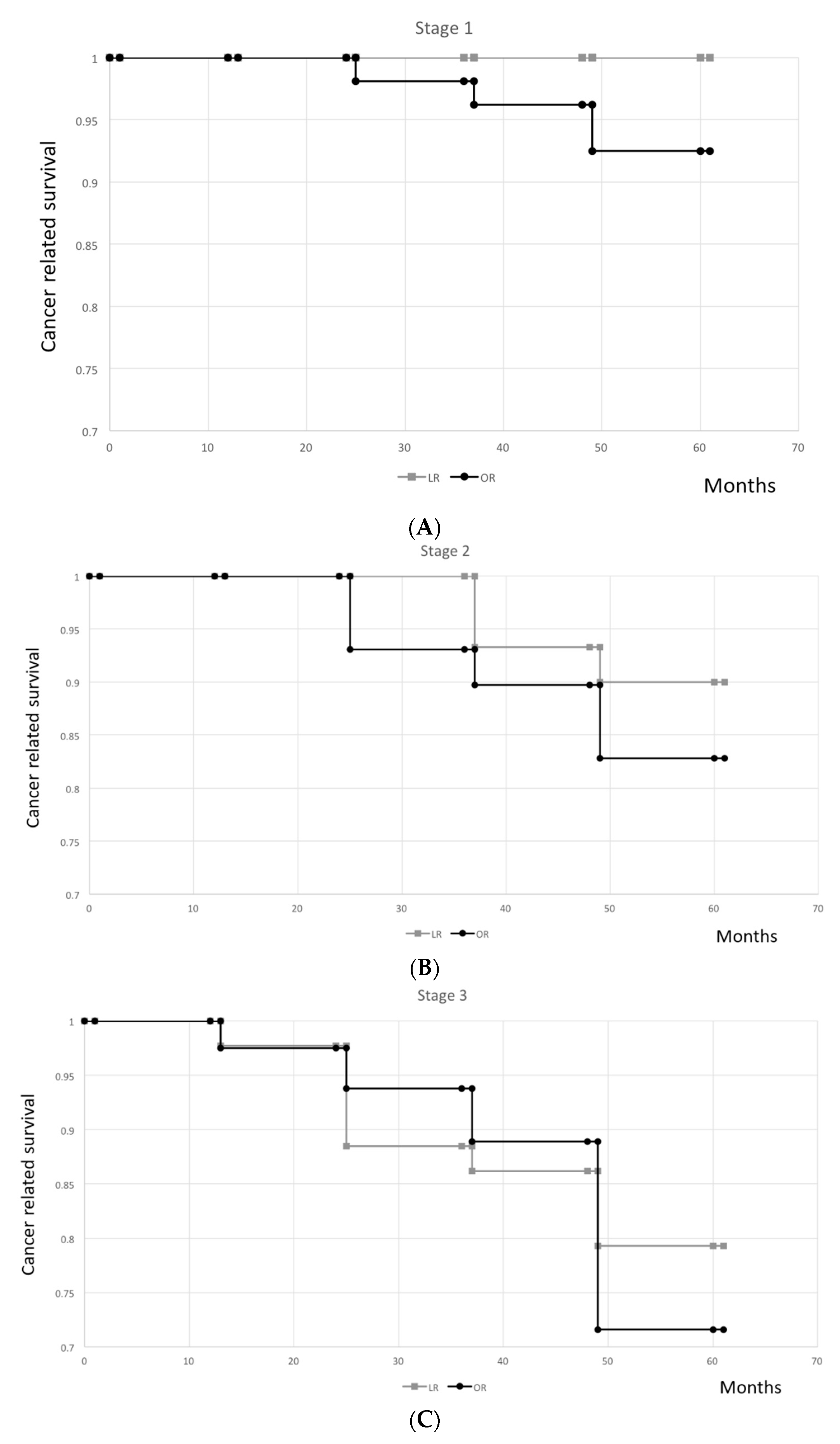
| Stage | Group | n | Death | Survival | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1st Year | 2nd Year | 3rd Year | 4th Year | 5th Year | p-Value | |||||
| n | % | % (n) | % (n) | % (n) | % (n) | % (n) | ||||
| 0 | LR | 3 | 0 | 0 | 100 (3) | 100 (3) | 100 (3) | 100 (3) | 100 (3) | - |
| OR | 0 | - | - | - | - | - | - | - | ||
| I | LR | 68 | 0 | 0 | 100 (68) | 100 (68) | 100 (68) | 100 (68) | 100 (68) | 0.206 |
| OR | 53 | 4 | 7.5 | 100 (53) | 100 (53) | 98.1 (52) | 96.2 (51) | 92.5 (49) | ||
| II | LR | 30 | 3 | 10.0 | 100 (30) | 100 (30) | 100 (30) | 93.3 (28) | 90.0 (27) | 0.713 |
| OR | 29 | 5 | 17.2 | 100 (29) | 93.1 (27) | 93.1 (27) | 89.7 (26) | 82.8 (24) | ||
| III | LR | 87 | 18 | 20.7 | 100 (87) | 97.7 (85) | 88.5 (77) | 86.2 (75) | 79.3 (69) | 0.426 |
| OR | 81 | 23 | 28.4 | 97.5 (79) | 93.8 (76) | 88.9 (72) | 82.7 (67) | 71.6 (58) | ||
| Total | LR | 188 | 21 | 11.2 | 100 (188) | 98.9 (186) | 94.7 (178) | 92.6 (174) | 88.8 (167) | 0.328 |
| OR | 163 | 32 | 19.6 | 98.8 (161) | 95.7 (156) | 92.6 (151) | 88.3 (144) | 80.3 (131) | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiu, C.-C.; Lin, W.-L.; Shi, H.-Y.; Huang, C.-C.; Chen, J.-J.; Su, S.-B.; Lai, C.-C.; Chao, C.-M.; Tsao, C.-J.; Chen, S.-H.; et al. Comparison of Oncologic Outcomes in Laparoscopic versus Open Surgery for Non-Metastatic Colorectal Cancer: Personal Experience in a Single Institution. J. Clin. Med. 2019, 8, 875. https://doi.org/10.3390/jcm8060875
Chiu C-C, Lin W-L, Shi H-Y, Huang C-C, Chen J-J, Su S-B, Lai C-C, Chao C-M, Tsao C-J, Chen S-H, et al. Comparison of Oncologic Outcomes in Laparoscopic versus Open Surgery for Non-Metastatic Colorectal Cancer: Personal Experience in a Single Institution. Journal of Clinical Medicine. 2019; 8(6):875. https://doi.org/10.3390/jcm8060875
Chicago/Turabian StyleChiu, Chong-Chi, Wen-Li Lin, Hon-Yi Shi, Chien-Cheng Huang, Jyh-Jou Chen, Shih-Bin Su, Chih-Cheng Lai, Chien-Ming Chao, Chao-Jung Tsao, Shang-Hung Chen, and et al. 2019. "Comparison of Oncologic Outcomes in Laparoscopic versus Open Surgery for Non-Metastatic Colorectal Cancer: Personal Experience in a Single Institution" Journal of Clinical Medicine 8, no. 6: 875. https://doi.org/10.3390/jcm8060875
APA StyleChiu, C.-C., Lin, W.-L., Shi, H.-Y., Huang, C.-C., Chen, J.-J., Su, S.-B., Lai, C.-C., Chao, C.-M., Tsao, C.-J., Chen, S.-H., & Wang, J.-J. (2019). Comparison of Oncologic Outcomes in Laparoscopic versus Open Surgery for Non-Metastatic Colorectal Cancer: Personal Experience in a Single Institution. Journal of Clinical Medicine, 8(6), 875. https://doi.org/10.3390/jcm8060875








