Does Age Influence the Outcome of Lower Limb Non-Union Treatment? A Matched Pair Analysis
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Design
2.2. Matching of Patients
- Study group: patients receiving surgical treatment based on the “diamond concept” older than 60 years
- Control group: patients receiving surgical treatment based on the “diamond concept” younger than 60 years
2.3. Surgical Technique
2.4. Follow-Up
2.5. Analysis of Radiological and Clinical Outcome
2.6. Statistics
3. Results
3.1. Analysis of Non-Union Therapy Outcome
3.2. Analysis of Risk Factors’ Influence on Outcome
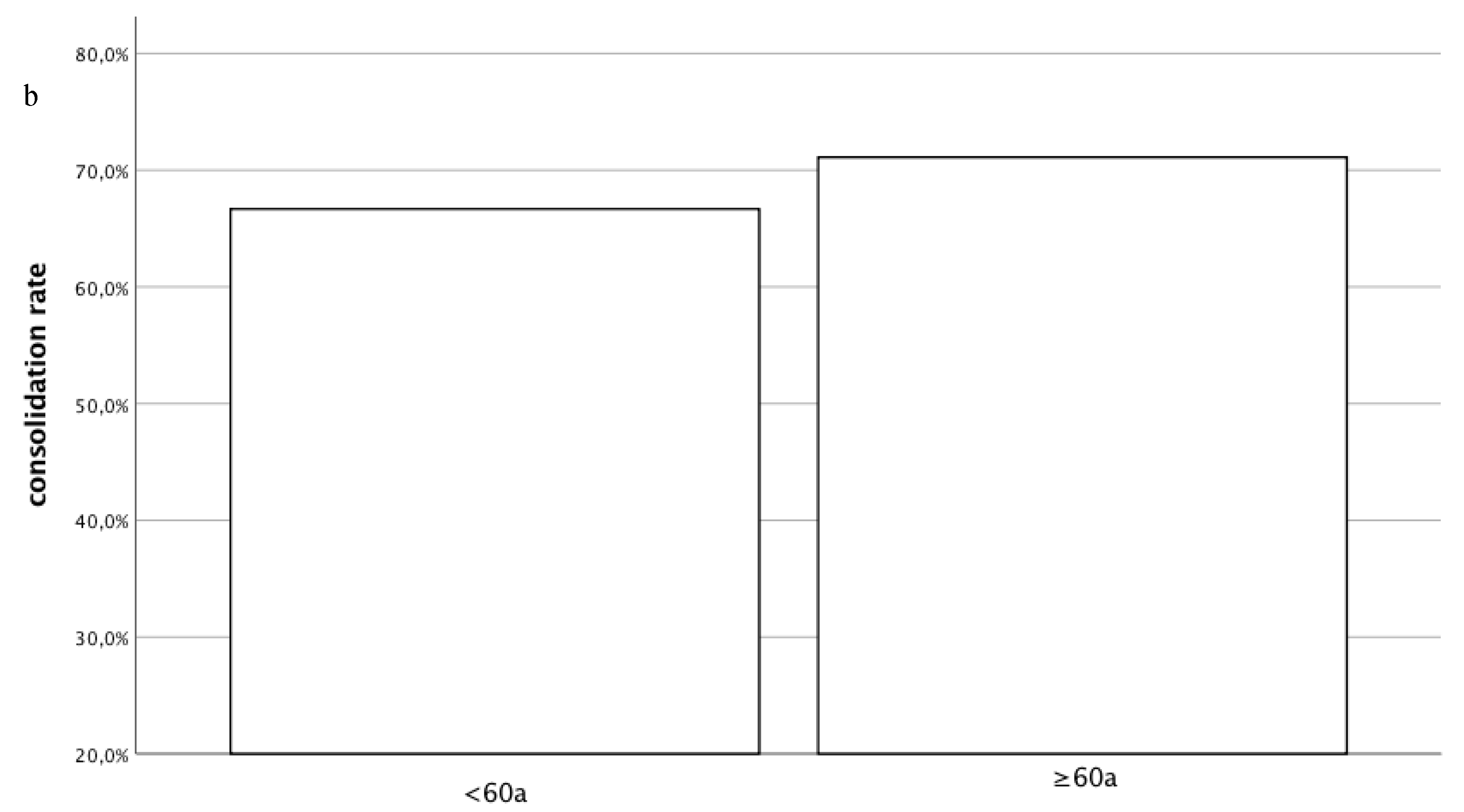
3.2.1. Radiological Outcome
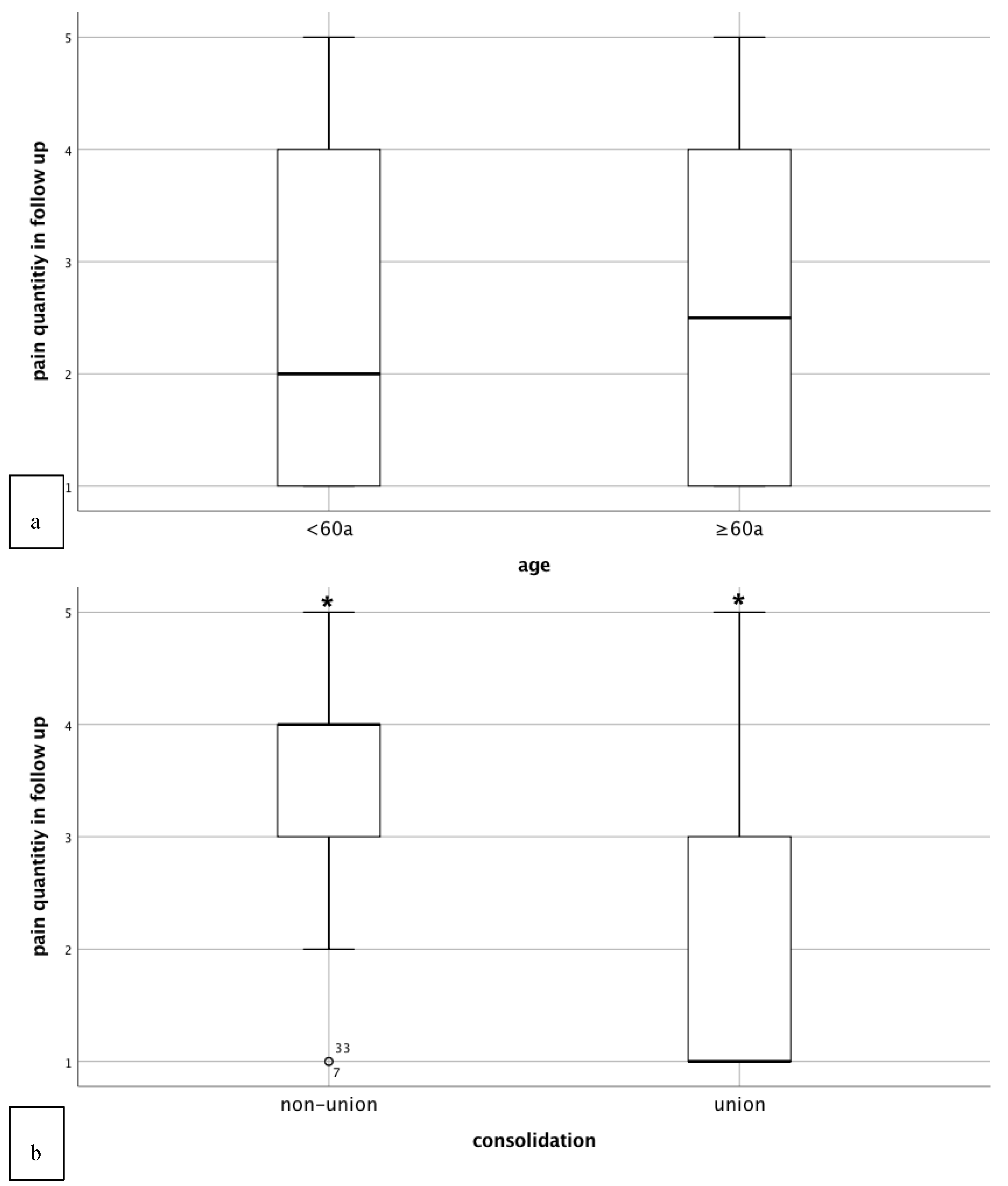
3.2.2. Clinical Outcome
4. Discussion
4.1. Influence of Age on Radiological Outcome of Non-Union Therapy
4.2. Influence of Age on Clinical Outcome of Non-Union Therapy
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Nguyen, N.D.; Ahlborg, H.G.; Center, J.R.; Eisman, J.A.; Nguyen, T.V. Residual lifetime risk of fractures in women and men. J. Bone Miner. Res. 2007, 22, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Lems, W.F.; Raterman, H.G. Critical issues and current challenges in osteoporosis and fracture prevention. An overview of unmet needs. Ther. Adv. Musculoskelet. Dis. 2017, 9, 299–316. [Google Scholar] [CrossRef] [PubMed]
- McGuigan, F.E.; Bartosch, P.; Akesson, K.E. Musculoskeletal health and frailty. Best Pract. Res. Clin. Rheumatol. 2017, 31, 145–159. [Google Scholar] [CrossRef] [PubMed]
- Tarantino, U.; Saturnino, L.; Scialdoni, A.; Feola, M.; Liuni, F.M.; Tempesta, V.; Pistillo, P. Fracture healing in elderly patients: New challenges for antiosteoporotic drugs. Aging Clin. Exp. Res. 2013, 25 (Suppl. 1), S105–S108. [Google Scholar] [CrossRef] [PubMed]
- Mills, L.A.; Aitken, S.A.; Simpson, A. The risk of non-union per fracture: Current myths and revised figures from a population of over 4 million adults. Acta Orthop. 2017, 88, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Dalle Carbonare, L.; Valenti, M.T.; Zanatta, M.; Donatelli, L.; Lo Cascio, V. Circulating mesenchymal stem cells with abnormal osteogenic differentiation in patients with osteoporosis. Arthritis Rheumatol. 2009, 60, 3356–3365. [Google Scholar] [CrossRef] [PubMed]
- Moghaddam, A.; Zimmermann, G.; Hammer, K.; Bruckner, T.; Grützner, P.A.; von Recum, J. Cigarette smoking influences the clinical and occupational outcome of patients with tibial shaft fractures. Injury 2011, 42, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Miclau, T.; Hu, D.; Hansen, E.; Tsui, K.; Puttlitz, C.; Marcucio, R.S. Cellular basis for age-related changes in fracture repair. J. Orthop. Res. 2005, 23, 1300–1307. [Google Scholar] [CrossRef]
- Egol, K.A.; Koval, K.J.; Zuckerman, J.D. Functional recovery following hip fracture in the elderly. J. Orthop. Trauma 1997, 11, 594–599. [Google Scholar] [CrossRef]
- Karger, C.; Kishi, T.; Schneider, L.; Fitoussi, F.; Masquelet, A.C. Treatment of posttraumatic bone defects by the induced membrane technique. Orthop. Traumatol. Surg. Res. 2012, 98, 97–102. [Google Scholar] [CrossRef]
- Foulke, B.A.; Kendal, A.R.; Murray, D.W.; Pandit, H. Fracture healing in the elderly: A review. Maturitas 2016, 92, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Moghaddam, A.; Zietzschmann, S.; Bruckner, T.; Schmidmaier, G. Treatment of atrophic tibia non-unions according to ‘diamond concept’: Results of one- and two-step treatment. Injury 2015, 46 (Suppl. 4), S39–S50. [Google Scholar] [CrossRef]
- Schmidmaier, G.; Moghaddam, A. Long Bone Nonunion. Z Orthop. Unf. 2015, 153, 659–674. [Google Scholar]
- Miska, M.; Findeisen, S.; Tanner, M.; Biglari, B.; Studier-Fischer, S.; Grützner, P.A.; Schmidmaier, G.; Moghaddam, A. Treatment of nonunions in fractures of the humeral shaft according to the Diamond Concept. Bone Jt. J. 2016, 98-B, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Moghaddam, A.; Thaler, B.; Bruckner, T.; Tanner, M.; Schmidmaier, G. Treatment of atrophic femoral non-unions according to the diamond concept: Results of one- and two-step surgical procedure. J. Orthop. 2017, 14, 123–133. [Google Scholar] [CrossRef]
- Andrzejowski, P.; Giannoudis, P.V. The ‘diamond concept’ for long bone non-union management. J. Orthop. Traumatol. 2019, 20, 21. [Google Scholar] [CrossRef]
- Masquelet, A.C.; Obert, L. Induced membrane technique for bone defects in the hand and wrist. Chir. Main 2010, 29 (Suppl. 1), S221–S224. [Google Scholar] [CrossRef]
- Haubruck, P.; Kammerer, A.; Korff, S.; Apitz, P.; Xiao, K.; Büchler, A.; Biglari, B.; Zimmermann, G.; Daniel, V.; Schmidmaier, G.; et al. The treatment of nonunions with application of BMP-7 increases the expression pattern for angiogenic and inflammable cytokines: A matched pair analysis. J. Inflamm. Res. 2016, 9, 155–165. [Google Scholar] [CrossRef]
- Masquelet, A.C.; Begue, T. The concept of induced membrane for reconstruction of long bone defects. Orthop. Clin. N. Am. 2010, 41, 27–37. [Google Scholar] [CrossRef]
- Moghaddam-Alvandi, A.; Zimmermann, G.; Büchler, A.; Elleser, C.; Biglari, B.; Grützner, P.A.; Wölfl, C.G. Results of nonunion treatment with bone morphogenetic protein 7 (BMP-7). Unfallchirurg 2012, 115, 518–526. [Google Scholar] [CrossRef]
- Pelissier, P.; Masquelet, A.C.; Bareille, R.; Pelissier, S.M.; Amedee, J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J. Orthop. Res. 2004, 22, 73–79. [Google Scholar] [CrossRef]
- Helbig, L.; Bechberger, M.; Aldeeri, R.; Ivanova, A.; Haubruck, P.; Miska, M.; Schmidmaier, G.; Omlor, G.W. Initial peri- and postoperative antibiotic treatment of infected nonunions: Results from 212 consecutive patients after mean follow-up of 34 months. Ther. Clin. Risk Manag. 2018, 14, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Dapunt, U.; Spranger, O.; Gantz, S.; Burckhardt, I.; Zimmermann, S.; Schmidmaier, G.; Moghaddam, A. Are atrophic long-bone nonunions associated with low-grade infections? Ther. Clin. Risk Manag. 2015, 11, 1843–1852. [Google Scholar] [CrossRef] [PubMed]
- Gruber, R.; Koch, H.; Doll, B.A.; Tegtmeier, F.; Einhorn, T.A.; Hollinger, J.O. Fracture healing in the elderly patient. Exp. Gerontol. 2006, 41, 1080–1093. [Google Scholar] [CrossRef] [PubMed]
- Zura, R.; Braid-Forbes, M.J.; Jeray, K.; Mehta, S.; Einhorn, T.A.; Watson, J.T.; della Rocca, G.J.; Forbes, K.; Steen, R.G. Bone fracture nonunion rate decreases with increasing age: A prospective inception cohort study. Bone 2017, 95, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, R.K.; Do, T.P.; Critchlow, C.W.; Dent, R.E.; Jick, S.S. Patient-related risk factors for fracture-healing complications in the United Kingdom General Practice Research Database. Acta Orthop. 2012, 83, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Taormina, D.P.; Shulman, B.S.; Karia, R.; Spitzer, A.B.; Konda, S.R.; Egol, K.A. Older age does not affect healing time and functional outcomes after fracture nonunion surgery. Geriatr. Orthop. Surg. Rehabil. 2014, 5, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Gortler, H.; Rusyn, J.; Godbout, C.; Chahal, J.; Schemitsch, E.H.; Nauth, A. Diabetes and Healing Outcomes in Lower Extremity Fractures: A Systematic Review. Injury 2018, 49, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, N.; Humphers, J.M.; Fluhman, B.L.; Jupiter, D.C. Factors associated with nonunion, delayed union, and malunion in foot and ankle surgery in diabetic patients. J. Foot Ankle Surg. 2013, 52, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Brinker, M.R.; O’Connor, D.P. Outcomes of tibial nonunion in older adults following treatment using the Ilizarov method. J. Orthop. Trauma 2007, 21, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Murena, L.; Canton, G.; Vulcano, E.; Surace, M.F.; Cherubino, P. Treatment of humeral shaft aseptic nonunions in elderly patients with opposite structural allograft, BMP-7, and mesenchymal stem cells. Orthopedics 2014, 37, e201–e206. [Google Scholar] [CrossRef] [PubMed]
- Bishop, J.A.; Palanca, A.A.; Bellino, M.J.; Lowenberg, D.W. Assessment of compromised fracture healing. J. Am. Acad. Orthop. Surg. 2012, 20, 273–282. [Google Scholar] [CrossRef] [PubMed]



| Characteristic | Group | |
|---|---|---|
| <60a (n = 45) | ≥60a (n = 45) | |
| Age (years) | 43 ± 11 | 67 ± 5 |
| Sex | ||
| Male | 28 (62%) | 28 (62%) |
| Female | 17 (38%) | 17 (38%) |
| Affected long bone | ||
| Tibia | 22 (49%) | 22 (49%) |
| Femur | 23 (51%) | 23 (51%) |
| Non-union treatment | ||
| One-Step | 17 (38%) | 17 (38%) |
| Two-Step | 28 (62%) | 28 (62%) |
| Smoking status | ||
| yes | 8 (18%) | 8 (18%) |
| no | 33 (73%) | 33 (73%) |
| former | 4 (9%) | 4 (9%) |
| Infection | ||
| yes | 16 (36%) | 16 (36%) |
| no | 29 (65%) | 29 (65%) |
| Bone Morphogenetic Protein used | ||
| rhBMP-2 | 5 (11%) | 9 (20%) |
| rhBMP-7 | 31 (69%) | 31 (69%) |
| none | 9 (20%) | 5 (11%) |
| Diabetes | ||
| yes | 3 (7%) | 7 (16%) |
| no | 42 (93%) | 38 (84%) |
| Method of osteosynthesis | ||
| External fixator | 0 (0%) | 1 (4%) |
| Nail | 24 (53%) | 19 (42%) |
| Plate | 21 (47%) | 25 (54%) |
| Type of non-union | ||
| hypertrophic | 10 (22%) | 3 (7%) |
| atrophic | 35 (78%) | 42 (93%) |
| Consolidation | ||
| yes | 30 (67%) | 32 (71%) |
| no | 15 (33%) | 13 (29%) |
| Characteristic | Group | ||
|---|---|---|---|
| <60a (n = 15) | ≥60a (n = 13) | Total (n = 28) | |
| Age (years) | 45 ± 8 | 71 ± 7 | 55 ± 13 |
| Sex | |||
| Male | 7 (47%) | 7 (54%) | 14 (50%) |
| Female | 8 (53%) | 6 (46%) | 14 (50%) |
| Affected long bone | |||
| Tibia | 4 (27%) | 6 (46%) | 10 (36%) |
| Femur | 11 (73%) | 7 (54%) | 18 (64%) |
| Non-union treatment | |||
| One-Step | 3 (20%) | 5 (38%) | 8 (29%) |
| Two-Step | 12 (80%) | 8 (62%) | 20 (71%) |
| Smoking status | |||
| yes | 3 (20%) | 4 (31%) | 7 (25%) |
| no | 11 (73%) | 7 (54%) | 18 (64%) |
| former | 1 (7%) | 2 (15%) | 3 (11%) |
| Infection | |||
| yes | 9 (60%) | 5 (38%) | 14 (50%) |
| no | 6 (40%) | 8 (62%) | 14 (50%) |
| rhBMP | |||
| rhBMP-2 | 0 (0%) | 1 (8%) | 1 (4%) |
| rhBMP-7 | 13 (87%) | 12 (92%) | 25 (89%) |
| none | 2 (13%) | 0 (0%) | 2 (7%) |
| Diabetes | |||
| yes | 3 (20%) | 3 (23%) | 6 (21%) |
| no | 12 (80%) | 10 (77%) | 22 (79%) |
| Method of osteosynthesis | |||
| External fixator | 0 (0%) | 0 (0%) | 0 (0%) |
| Nail | 8 (53%) | 4 (31%) | 12 (43%) |
| Plate | 7 (47%) | 9 (69%) | 16 (57%) |
| Type of non-union | |||
| hypertrophic | 3 (20%) | 1 (8%) | 4 (14%) |
| atrophic | 12 (80%) | 12 (92%) | 24 (86%) |
| Group | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| <60a (n = 38) | 21 (47%) | 3 (7%) | 8 (18%) | 10 (22%) | 2 (4%) |
| ≥60a (n = 38) | 17 (38%) | 4 (9%) | 7 (16%) | 12 (27%) | 2 (4%) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanner, M.; Vlachopoulos, W.; Findeisen, S.; Miska, M.; Ober, J.; Hagelskamp, S.; Schmidmaier, G.; Haubruck, P. Does Age Influence the Outcome of Lower Limb Non-Union Treatment? A Matched Pair Analysis. J. Clin. Med. 2019, 8, 1276. https://doi.org/10.3390/jcm8091276
Tanner M, Vlachopoulos W, Findeisen S, Miska M, Ober J, Hagelskamp S, Schmidmaier G, Haubruck P. Does Age Influence the Outcome of Lower Limb Non-Union Treatment? A Matched Pair Analysis. Journal of Clinical Medicine. 2019; 8(9):1276. https://doi.org/10.3390/jcm8091276
Chicago/Turabian StyleTanner, Michael, Wasilios Vlachopoulos, Sebastian Findeisen, Matthias Miska, Julian Ober, Saskia Hagelskamp, Gerhard Schmidmaier, and Patrick Haubruck. 2019. "Does Age Influence the Outcome of Lower Limb Non-Union Treatment? A Matched Pair Analysis" Journal of Clinical Medicine 8, no. 9: 1276. https://doi.org/10.3390/jcm8091276
APA StyleTanner, M., Vlachopoulos, W., Findeisen, S., Miska, M., Ober, J., Hagelskamp, S., Schmidmaier, G., & Haubruck, P. (2019). Does Age Influence the Outcome of Lower Limb Non-Union Treatment? A Matched Pair Analysis. Journal of Clinical Medicine, 8(9), 1276. https://doi.org/10.3390/jcm8091276





