Seasonal Variation in Physical Activity among Preoperative Patients with Lung Cancer Determined Using a Wearable Device
Abstract
:1. Introduction
2. Methods
2.1. Subjects and Data Sources
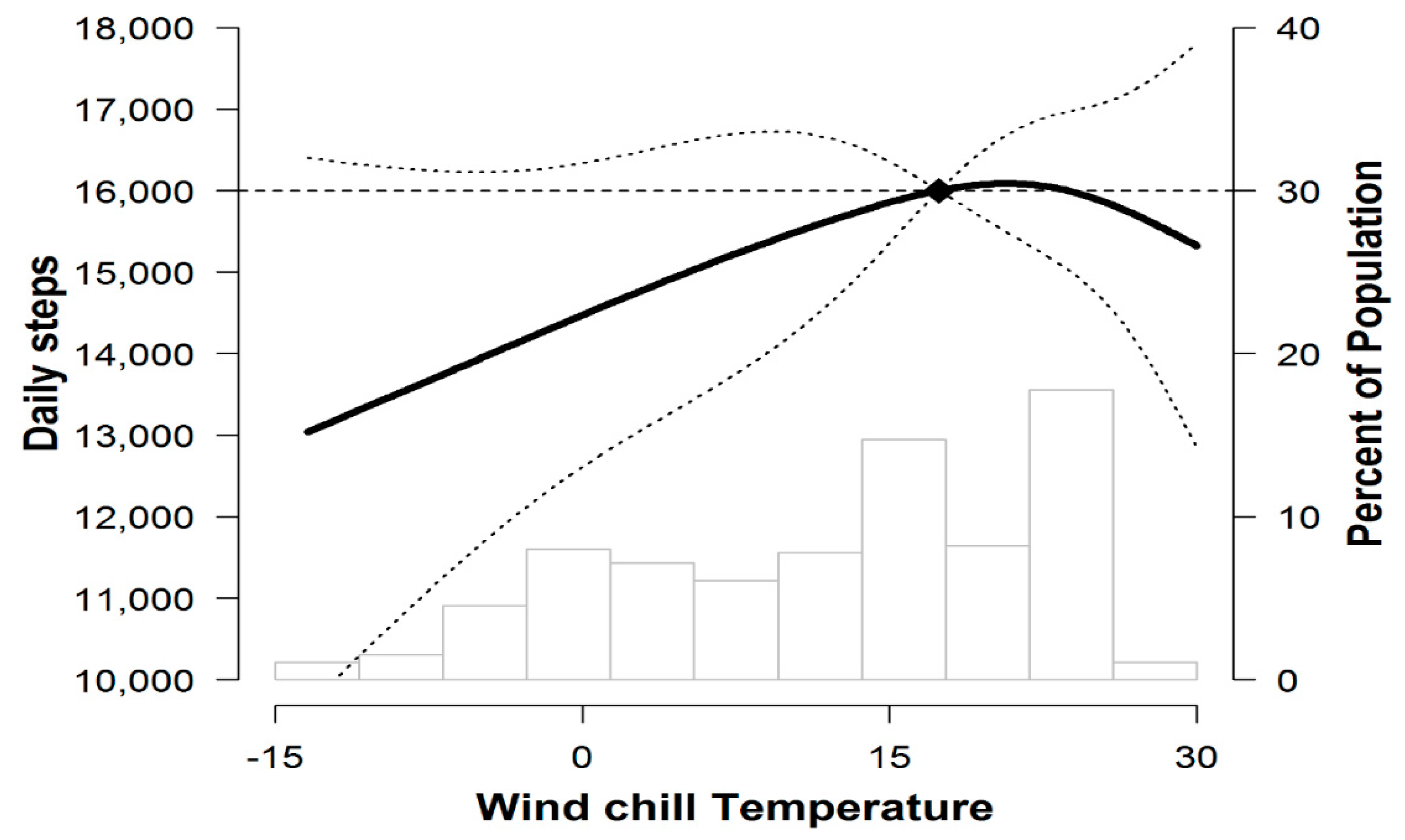
2.2. Grouping and Weather Data Collection
2.3. Physical Activity and other Variable
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fitzmaurice, C.; Allen, C.; Barber, R.M.; Barregard, L.; Bhutta, Z.A.; Brenner, H.; Dicker, D.J.; Chimed-Orchir, O.; Dandona, R.; Dandona, L.; et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017, 3, 524–548. [Google Scholar] [PubMed]
- Sebio Garcia, R.; Yanez Brage, M.I.; Gimenez Moolhuyzen, E.; Granger, C.L.; Denehy, L. Functional and postoperative outcomes after preoperative exercise training in patients with lung cancer: A systematic review and meta-analysis. Interact. Cardiovasc. Thorac. Surg. 2016, 23, 486–497. [Google Scholar] [CrossRef] [PubMed]
- Bade, B.C.; Thomas, D.D.; Scott, J.B.; Silvestri, G.A. Increasing physical activity and exercise in lung cancer: Reviewing safety, benefits, and application. J. Thorac. Oncol. 2015, 10, 861–871. [Google Scholar] [CrossRef] [Green Version]
- Vainshelboim, B.; Muller, J.; Lima, R.M.; Nead, K.T.; Chester, C.; Chan, K.; Kokkinos, P.; Myers, J. Cardiorespiratory fitness, physical activity and cancer mortality in men. Prev. Med. 2017, 100, 89–94. [Google Scholar] [CrossRef]
- Kehler, D.S.; Stammers, A.N.; Tangri, N.; Hiebert, B.; Fransoo, R.; Schultz, A.S.H.; Macdonald, K.; Giacomontonio, N.; Hassan, A.; Legare, J.F.; et al. Systematic review of preoperative physical activity and its impact on postcardiac surgical outcomes. BMJ Open 2017, 7, e015712. [Google Scholar] [CrossRef]
- Steffens, D.; Beckenkamp, P.R.; Hancock, M.; Solomon, M.; Young, J. Preoperative exercise halves the postoperative complication rate in patients with lung cancer: A systematic review of the effect of exercise on complications, length of stay and quality of life in patients with cancer. Br. J. Sports Med. 2018, 52, 344. [Google Scholar] [CrossRef]
- Chen, Y.M. Perceived barriers to physical activity among older adults residing in long-term care institutions. J. Clin. Nurs. 2010, 19, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Tucker, P.; Gilliland, J. The effect of season and weather on physical activity: A systematic review. Public Health 2007, 121, 909–922. [Google Scholar] [CrossRef] [PubMed]
- Ridgers, N.D.; Salmon, J.; Timperio, A. Seasonal changes in physical activity during school recess and lunchtime among Australian children. J. Sports Sci. 2018, 36, 1508–1514. [Google Scholar] [CrossRef] [Green Version]
- Wu, Y.T.; Luben, R.; Wareham, N.; Griffin, S.; Jones, A.P. Weather, day length and physical activity in older adults: Cross-sectional results from the European Prospective Investigation into Cancer and Nutrition (EPIC) Norfolk Cohort. PLoS ONE 2017, 12, e0177767. [Google Scholar] [CrossRef] [Green Version]
- Novoa, N.M.; Varela, G.; Jimenez, M.F.; Ramos, J. Value of the average basal daily walked distance measured using a pedometer to predict maximum oxygen consumption per minute in patients undergoing lung resection. Eur J Cardiothorac Surg. 2011, 39, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Novoa, N.; Varela, G.; Jimenez, M.F.; Aranda, J.L. Influence of major pulmonary resection on postoperative daily ambulatory activity of the patients. Interact. Cardiovasc. Thorac. Surg. 2009, 9, 934–938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granger, C.L.; McDonald, C.F.; Irving, L.; Clark, R.A.; Gough, K.; Murnane, A.; Mileshkin, L.; Krishnasamy, M.; Denehy, L. Low physical activity levels and functional decline in individuals with lung cancer. Lung Cancer 2014, 83, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Sushames, A.; Edwards, A.; Thompson, F.; McDermott, R.; Gebel, K. Validity and Reliability of Fitbit Flex for Step Count, Moderate to Vigorous Physical Activity and Activity Energy Expenditure. PLoS ONE 2016, 11, e0161224. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Thompson, P.J.; Berman, L.B.; Sullivan, M.J.; Townsend, M.; Jones, N.L.; Pugsley, S.O. How should we measure function in patients with chronic heart and lung disease? J. Chronic Dis. 1985, 38, 517–524. [Google Scholar] [CrossRef]
- Celli, B.; Tetzlaff, K.; Criner, G.; Polkey, M.I.; Sciurba, F.; Casaburi, R.; Tal-Singer, R.; Kawata, A.; Merrill, D.; Rennard, S. The 6-Minute-Walk Distance Test as a Chronic Obstructive Pulmonary Disease Stratification Tool. Insights from the COPD Biomarker Qualification Consortium. Am. J. Respir. Crit. Care Med. 2016, 194, 1483–1493. [Google Scholar] [CrossRef] [Green Version]
- Miller, M. ATS/ERS task force: Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef] [Green Version]
- American Thoracic Society. Single-breath carbon monoxide diffusing capacity (transfer factor). Recommendations for a standard technique—1995 update. Am. J. Respir. Crit. Care Med. 1995, 152, 2185–2198. [Google Scholar] [CrossRef]
- Choi, J.K.; Paek, D.; Lee, J.O. Normal predictive values of spirometry in Korean population. Tuberc. Respir. Dis. 2005, 58, 230–242. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Choi, I.; Park, K. Normal predicted standards of single breath carbon monoxide diffusing capacity of lung in healthy nonsmoking adults. J. Korean J. Intern. Med. 1985, 28, 176–183. [Google Scholar]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; De Bourdeaudhuij, I.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Lutes, L.D.; et al. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tudor-Locke, C.; Jones, R.; Myers, A.M.; Paterson, D.H.; Ecclestone, N.A. Contribution of structured exercise class participation and informal walking for exercise to daily physical activity in community-dwelling older adults. Res. Q. Exerc. Sport 2002, 73, 350–356. [Google Scholar] [CrossRef] [PubMed]
- American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med. Sci. Sports Exerc. 1998, 30, 975–991. [Google Scholar]
- World Health Organization (WHO). Definition of an Older or Elderly Person. World Health Organization. 2016. Available online: http://www.who.int/healthinfo/survey/ageingdefnolder/en/ (accessed on 3 August 2017).
- Marjanski, T.; Wnuk, D.; Bosakowski, D.; Szmuda, T.; Sawicka, W.; Rzyman, W. Patients who do not reach a distance of 500 m during the 6-min walk test have an increased risk of postoperative complications and prolonged hospital stay after lobectomy. Eur. J. Cardiothorac. Surg. 2015, 47, e213–e219. [Google Scholar] [CrossRef] [Green Version]
- Alahmari, A.D.; Mackay, A.J.; Patel, A.R.; Kowlessar, B.S.; Singh, R.; Brill, S.E.; Allinson, J.P.; Wedzicha, J.A.; Donaldson, G.C. Influence of weather and atmospheric pollution on physical activity in patients with COPD. Respir. Res. 2015, 16, 71. [Google Scholar] [CrossRef] [Green Version]
- Merchant, A.T.; Dehghan, M.; Akhtar-Danesh, N. Seasonal variation in leisure-time physical activity among Canadians. Can. J. Public Health 2007, 98, 203–208. [Google Scholar] [CrossRef]
- Klenk, J.; Buchele, G.; Rapp, K.; Franke, S.; Peter, R. Walking on sunshine: Effect of weather conditions on physical activity in older people. J. Epidemiol. Community Health 2012, 66, 474–476. [Google Scholar] [CrossRef]
- Shoemaker, M.J.; Roper, S.E.; Calkins, T.N. Seasonal variation of daily physical activity in individuals with heart failure. Heart Int. 2016, 11, e25–e31. [Google Scholar] [CrossRef]
- Elliot, A.J.; Cross, K.W.; Fleming, D.M. Acute respiratory infections and winter pressures on hospital admissions in England and Wales 1990–2005. J. Public Health 2008, 30, 91–98. [Google Scholar] [CrossRef] [Green Version]
- Hasegawa, J.; Suzuki, H.; Yamauchi, T. Impact of season on the association between muscle strength/volume and physical activity among community-dwelling elderly people living in snowy-cold regions. J. Physiol. Anthr. 2018, 37, 25. [Google Scholar] [CrossRef] [PubMed]
- Stefanelli, F.; Meoli, I.; Cobuccio, R.; Curcio, C.; Amore, D.; Casazza, D.; Tracey, M.; Rocco, G. High-intensity training and cardiopulmonary exercise testing in patients with chronic obstructive pulmonary disease and non-small-cell lung cancer undergoing lobectomy. Eur. J. Cardiothorac. Surg. 2013, 44, e260–e265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hattori, K.; Matsuda, T.; Takagi, Y.; Nagaya, M.; Inoue, T.; Nishida, Y.; Hasegawa, Y.; Kawaguchi, K.; Fukui, T.; Ozeki, N.; et al. Preoperative six-minute walk distance is associated with pneumonia after lung resection. Interact. Cardiovasc. Thorac. Surg. 2018, 26, 277–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lai, Y.; Huang, J.; Yang, M.; Su, J.; Liu, J.; Che, G. Seven-day intensive preoperative rehabilitation for elderly patients with lung cancer: A randomized controlled trial. J. Surg. Res. 2017, 209, 30–36. [Google Scholar] [CrossRef]
- Aspvik, N.P.; Viken, H.; Ingebrigtsen, J.E.; Zisko, N.; Mehus, I.; Wisloff, U.; Stensvold, D. Do weather changes influence physical activity level among older adults?—The Generation 100 study. PLoS ONE 2018, 13, e0199463. [Google Scholar] [CrossRef]
- Chan, C.B.; Ryan, D.A.; Tudor-Locke, C. Relationship between objective measures of physical activity and weather: A longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 21. [Google Scholar] [CrossRef] [Green Version]
- Kimura, T.; Kobayashi, H.; Nakayama, E.; Kakihana, W. Seasonality in physical activity and walking of healthy older adults. J. Physiol. Anthr. 2015, 34, 33. [Google Scholar] [CrossRef] [Green Version]
- Togo, F.; Watanabe, E.; Park, H.; Shephard, R.J.; Aoyagi, Y. Meteorology and the physical activity of the elderly: The Nakanojo Study. Int. J. Biometeorol. 2005, 50, 83–89. [Google Scholar] [CrossRef]
- Bluestein, M. An evaluation of the wind chill factor: Its development and applicability. J. Biomech. Eng. 1998, 120, 255–258. [Google Scholar] [CrossRef]

| Characteristics | Spring (n = 171) | Summer (n = 178) | Autumn (n = 99) | Winter (n = 107) | p |
|---|---|---|---|---|---|
| Mean age | 60.6 (8.9) | 62.6 (8.3) | 60.6 (9.0) | 59.9 (9.4) | 0.05 |
| Age categories | 0.04 | ||||
| <65 | 118 (69.0) | 104 (58.4) | 66 (66.7) | 79 (73.8) | |
| ≥65 | 53 (31.0) | 74 (41.6) | 33 (33.3) | 28 (26.2) | |
| Sex, male | 97 (56.7) | 101 (56.7) | 57 (57.6) | 57 (53.3) | 0.92 |
| Body mass index, kg/m2 | 24.1 (2.9) | 24.3 (2.7) | 24.1 (2.7) | 24.5 (3.2) | 0.67 |
| Smoking status | 0.32 | ||||
| Never-smoker | 78 (45.6) | 89 (50.0) | 48 (48.5) | 57 (53.3) | |
| Ex-smoker | 59 (34.5) | 34 (19.1) | 27 (27.3) | 16 (15.0) | |
| Current smoker | 34 (19.9) | 55 (30.9) | 24 (24.2) | 34 (31.8) | |
| Marital status | 0.64 | ||||
| Married | 151 (88.3) | 159 (89.3) | 91 (91.9) | 91 (85.1) | |
| Single/divorced/widowed | 19 (11.1) | 19 (10.7) | 7 (7.1) | 15 (14.0) | |
| Unknown | 1 (0.6) | 0 | 1 (1.0) | 1 (0.9) | |
| Employment status | 0.46 | ||||
| Current work | 98 (57.3) | 81 (45.5) | 49 (49.5) | 58 (54.2) | |
| No work | 72 (42.1) | 96 (53.9) | 49 (49.5) | 48 (44.9) | |
| Unknown | 1 (0.6) | 1 (0.6) | 1 (1.0) | 1 (0.9) | |
| Monthly family income | 0.19 | ||||
| <$3.000 | 54 (31.6) | 51 (28.7) | 23 (23.2) | 31 (29.0) | |
| ≥$3.000 | 87 (50.9) | 93 (52.3) | 54 (54.6) | 66 (61.7) | |
| Unknown | 30 (17.5) | 34 (19.1) | 22 (22.2) | 10 (9.4) | |
| Comorbidities | |||||
| Pulmonary comorbidities | |||||
| COPD | 40 (23.4) | 43 (24.2) | 26 (26.3) | 19 (17.8) | 0.49 |
| Asthma | 3 (1.8) | 8 (4.5) | 1 (1.0) | 3 (2.8) | 0.34 |
| ILD | 1 (0.6) | 2 (1.1) | 1 (1.0) | 2 (1.9) | 0.86 |
| Extra-pulmonary comorbidities | |||||
| Hypertension | 52 (30.4) | 72 (40.5) | 28 (28.3) | 35 (32.7) | 0.12 |
| Diabetes mellitus | 22 (12.9) | 27 (15.2) | 11 (11.1) | 7 (6.5) | 0.18 |
| Cardiovascular disease | 12 (7.0) | 20 (11.2) | 9 (9.1) | 9 (8.4) | 0.58 |
| Pathologic stage | 0.81 | ||||
| I | 128 (74.9) | 130 (73.0) | 75 (75.8) | 75 (70.1) | |
| II | 25 (14.6) | 31 (17.4) | 13 (13.1) | 16 (15.0) | |
| III | 18 (10.5) | 17 (9.6) | 11 (11.1) | 16 (15.0) | |
| Pulmonary function test | |||||
| FVC, L | 3.6 (0.9) | 3.4 (0.8) | 3.7 (0.9) | 3.7 (0.8) | 0.02 |
| FVC, % predicted | 93.4 (11.5) | 89.8 (12.9) | 94.3 (12.7) | 96.4 (12.1) | < 0.01 |
| FEV1, L | 2.7 (0.7) | 2.5 (0.6) | 2.7 (0.6) | 2.8 (0.6) | < 0.01 |
| FEV1, % predicted | 90.0 (13.2) | 87.5 (15.5) | 90.2 (14.9) | 95.0 (13.5) | < 0.01 |
| FEV1/FVC | 73.8 (8.2) | 73.6 (8.6) | 72.6 (8.6) | 75.1 (8.3) | 0.21 |
| DLco, % | 91.6 (16.0) | 89.2 (17.3) | 89.7 (15.2) | 91.3 (13.7) | 0.47 |
| Cardiorespiratory fitness | |||||
| 6 min walk distance (m) | 520.1(85.7) | 506.9(89.1) | 515.0(66.8) | 508.1(80.7) | 0.46 |
| 6 min walk distance | 0.69 | ||||
| Short distance (<500 m) | 68 (39.9) | 77 (43.3) | 37 (37.4) | 49 (45.8) | |
| Long distance (≥500 m) | 102 (59.7) | 97 (54.5) | 60 (60.1) | 56 (52.3) | |
| Unknown | 1 (0.6) | 4 (2.3) | 2 (2.1) | 2 (1.9) |
| Spring | Summer | Autumn | Winter | |
|---|---|---|---|---|
| Difference in steps per day (%) | ||||
| Overall | Reference | −0.86 (−12.38, 12.18) | −6.24 (−18.86, 8.33) | −27.04 (−36.68, −15.93) |
| Age | ||||
| <65 years | Reference | −8.08 (−21.25, 7.30) | −10.27 (−24.74, 6.98) | −25.21 (−36.65, −11.70) |
| ≥65 years | Reference | 11.91 (−9.08, 37.74) | 2.36 (−20.65, 32.02) | −32.16 (−48.31, −10.97) |
| p for interaction | 0.14 | 0.40 | 0.55 | |
| Cardiorespiratory fitness (6MWD) | ||||
| <500 m | Reference | −1.21 (−18.1, 19.18) | 7.07 (−14.97, 34.83) | −27.63 (−41.48, −10.50) |
| ≥500 m | Reference | −0.75 (−15.53, 16.62) | −12.95 (−27.52, 4.55) | −20.97 (−34.54, −4.59) |
| p for interaction | 0.97 | 0.17 | 0.54 | |
| Difference in MVPA minutes per day (%) | ||||
| Overall | Reference | 5.06 (−14.6, 29.24) | −2.11(−23.13, 24.67) | −35.22 (−49.18, −17.43) |
| Age | ||||
| <65 years | Reference | 5.13 (−19.26, 36.89) | −1.43 (−26.71, 32.57) | −33.03 (−49.63, −10.95) |
| ≥65 years | Reference | 4.05 (−26.37, 47.04) | −3.75 (−37.24, 47.60) | −40.72 (−62.76, −5.62) |
| p for interaction | 0.96 | 0.93 | 0.66 | |
| Cardiorespiratory fitness (6MWD) | ||||
| <500 m | Reference | −4.25 (−30.56, 32.04) | 20.57 (−18.5, 78.39) | −38.65 (−57.62, −11.18) |
| ≥500 m | Reference | 11.12 (−15.17, 45.55) | −10.57 (−34.3, 21.73) | −26.01 (−46.46, 2.25) |
| p for interaction | 0.48 | 0.24 | 0.03 | |
| Spring | Summer | Autumn | Winter | |
|---|---|---|---|---|
| Steps ≥8000/day | ||||
| Overall | Reference | 1.11 (0.69, 1.79) | 0.98 (0.57, 1.70) | 0.46 (0.28, 0.77) |
| Age | ||||
| <65 years | Reference | 0.79 (0.43, 1.44) | 0.73 (0.37, 1.45) | 0.38 (0.20, 0.71) |
| ≥65 years | Reference | 2.00 (0.93, 4.31) | 1.75 (0.67, 4.56) | 0.67 (0.26, 1.74) |
| p for interaction | 0.06 | 0.15 | 0.32 | |
| Cardiorespiratory fitness (6MWD) | ||||
| <500 m | Reference | 0.94 (0.48, 1.82) | 1.75 (0.73, 4.20) | 0.45 (0.21, 0.96) |
| ≥500 m | Reference | 1.35 (0.67, 2.74) | 0.74 (0.36, 1.55) | 0.58 (0.28, 1.22) |
| p for interaction | 0.46 | 0.14 | 0.63 | |
| MVPA ≥60 min/day | ||||
| Overall | Reference | 1.73 (1.10, 2.71) | 1.07 (0.62, 1.83) | 0.52 (0.29, 0.94) |
| Age | ||||
| <65 years | Reference | 1.59 (0.91, 2.79) | 1.19 (0.62, 2.27) | 0.59 (0.30, 1.15) |
| ≥65 years | Reference | 2.11 (0.96, 4.61) | 0.92 (0.34, 2.50) | 0.29 (0.07, 1.13) |
| P for interaction | 0.50 | 0.72 | 0.42 | |
| Cardiorespiratory fitness (6MWD) | ||||
| <500 m | Reference | 1.26 (0.61, 2.58) | 1.24 (0.52, 2.98) | 0.30 (0.10, 0.87) |
| ≥500 m | Reference | 1.97 (1.10, 3.55) | 1.03 (0.52, 2.05) | 0.77 (0.37, 1.61) |
| p for interaction | 0.34 | 0.75 | 0.15 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kong, S.; Park, H.Y.; Kang, D.; Lee, J.K.; Lee, G.; Kwon, O.J.; Shim, Y.M.; Zo, J.I.; Cho, J. Seasonal Variation in Physical Activity among Preoperative Patients with Lung Cancer Determined Using a Wearable Device. J. Clin. Med. 2020, 9, 349. https://doi.org/10.3390/jcm9020349
Kong S, Park HY, Kang D, Lee JK, Lee G, Kwon OJ, Shim YM, Zo JI, Cho J. Seasonal Variation in Physical Activity among Preoperative Patients with Lung Cancer Determined Using a Wearable Device. Journal of Clinical Medicine. 2020; 9(2):349. https://doi.org/10.3390/jcm9020349
Chicago/Turabian StyleKong, Sunga, Hye Yun Park, Danbee Kang, Jae Kyung Lee, Genehee Lee, O Jung Kwon, Young Mog Shim, Jae Ill Zo, and Juhee Cho. 2020. "Seasonal Variation in Physical Activity among Preoperative Patients with Lung Cancer Determined Using a Wearable Device" Journal of Clinical Medicine 9, no. 2: 349. https://doi.org/10.3390/jcm9020349





