Down to Earth: Planetary Health and Biophilosophy in the Symbiocene Epoch
Abstract
:1. Introduction
1.1. Scales of Health Promotion
“Ideas determine the nature, characteristics, and behavior of a metabiological cell—an individual—or the metabiological organism, the society…the time has arrived in which we have to realize that we are all parts of a single organism and develop some new kinds of responses and relationships”.—Jonas E. Salk, 1983 [1]
1.2. Roadmap to the Current Review
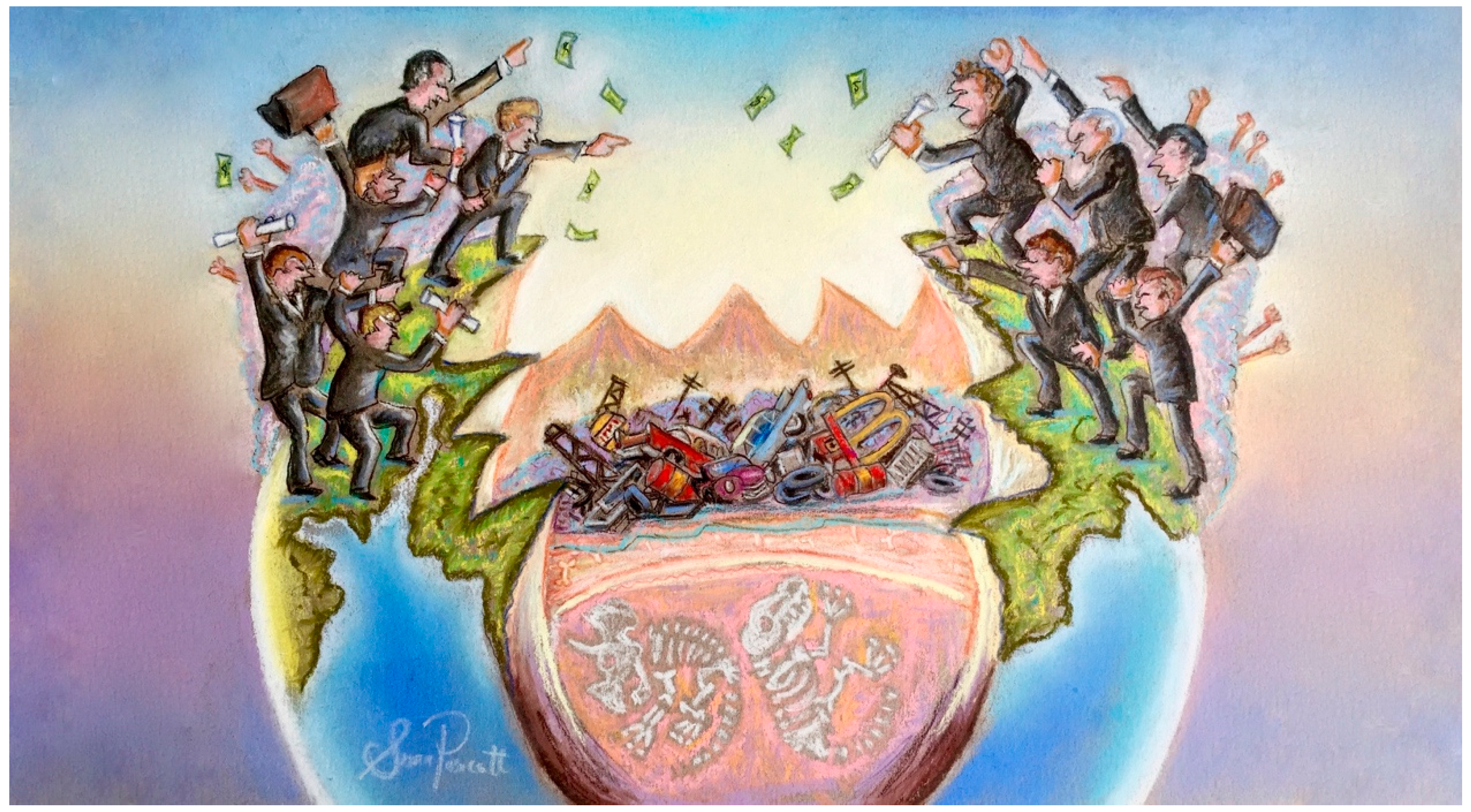
1.3. Anthropocene Syndrome
1.4. Mars Colonies and Intellectual Escapism
“Today, the investment devoted to developing preventatives or cures for human disease and to maintain health from conception to the end of life is a pitifully small fraction of the cost of the material of war or the race into space”.—Jonas Salk, 1966 [45]
“The technology cannot cure the intellectual dishonesty that burdens its channels today. Even more dangerous and more universal is intellectual escapism, the attempt to escape the real problems around us…we organize meetings about it in all sorts of pleasant places to talk about this [biomedicine], and that saves us the responsibility of walking across the street, where 100,000 children are being poisoned every day by lead in paint...something can be done immediately about this problem, but it is not being done because it is not of sufficient interest or as exciting intellectually as talking about changing the genetic nature of man”.[50]
“It is crucial that increased knowledge and understanding of brain anatomy and function, the mind and consciousness, have absolute priority if we are to find ways to ameliorate extremes of human aggression, mental sickness, and brain aging and pathologies…claims of immediate, economic and human side benefits from space research, for jobs, inventions and curiosity, apply no less to the life sciences. Cosmic issues fade before urgent exploration of the human brain. Mars can surely wait 30–50 years”.[63]
1.5. Biophilosophy
“What might happen if biologists and other scholars so oriented were to combine talents even more than they do now, not simply to develop further their own special interests individually…[they]…are realizing more and more, their responsibility to society as well as to themselves”.—Jonas E. Salk, 1962 [70]
1.6. Microbiome: Metaphor for a Broken System
1.7. Dysbiosis and the Mental Environment
1.8. The Symbiocene
“The Symbiocene will be that period in the Earth’s history where humans symbiotically reintegrate themselves, psychologically and technologically, into nature and natural systems”.—Glenn Albrecht, 2014 [108]
2. Conclusions
“The creation of the institute is more important and more significant. Here, we are working for the excellence of human health. Individual subject matters are studied for their relevance to the problems of humankind from the scientific and philosophical points of view. Hopefully, this institute will choose the more important problems to address. We are laying the foundation to understand more about ourselves and nature”.[154]
Author Contributions
Conflicts of Interest
References
- Stoler, P. A conversation with Jonas Salk. Psychol. Today 1983, 17, 50–56. [Google Scholar]
- Allen, L.N.; Feigl, A.B. What’s in a name? A call to reframe non-communicable diseases. Lancet Glob. Health 2017, 5, e129–e130. [Google Scholar] [CrossRef]
- Prescott, S.L.; Logan, A.C. Transforming life: A broad view of the developmental origins of health and disease concept from an ecological justice perspective. Int. J. Environ. Res. Public Health 2016, 13, 1075. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Mental Health: Strengthening Our Response; WHO Fact Sheet No. 220; World Health Organization: Genava, Switzerland, 2014. [Google Scholar]
- Orpana, H.; Vachon, J.; Dykxhoorn, J.; McRae, L.; Jayaraman, G. Monitoring positive mental health and its determinants in Canada: The development of the positive mental health surveillance indicator framework. Health Promot. Chronic Dis. Prev. Can. 2016, 36, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Havinga, P.J.; Boschloo, L.; Bloemen, A.J.; Nauta, M.H.; de Vries, S.O.; Penninx, B.W.; Schoevers, R.A.; Hartman, C.A. Doomed for disorder? High incidence of mood and anxiety disorders in offspring of depressed and anxious patients: A prospective cohort study. J. Clin. Psychiatry 2017, 78, e8–e17. [Google Scholar] [CrossRef] [PubMed]
- Baird, J.; Jacob, C.; Barker, M.; Fall, C.H.; Hanson, M.; Harvey, N.C.; Inskip, H.M.; Kumaran, K.; Cooper, C. Developmental origins of health and disease: A lifecourse approach to the prevention of non-communicable diseases. Healthcare 2017, 5, 14. [Google Scholar] [CrossRef] [PubMed]
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.G.; de Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.; Head, P.; et al. Safeguarding human health in the anthropocene epoch: Report of the rockefeller foundation-lancet commission on planetary health. Lancet 2015, 386, 1973–2028. [Google Scholar] [CrossRef]
- Craig, J.M.; Prescott, S.L. Planning ahead: The mental health value of natural environments. Lancet Planet Health 2017, 1, e128–e129. [Google Scholar] [CrossRef]
- Ruokolainen, L.; Lehtimäki, J.; Karkman, A.; Haahtela, T.; von Hertzen, L.; Fyhrquist, N. Holistic view on health: Two protective layers of biodiversity. Ann. Zool. Fenn. 2017, 54, 39–49. [Google Scholar] [CrossRef]
- Monge, G.; Jimenez-Espejo, F.J.; Garcia-Alix, A.; Martinez-Ruiz, F.; Mattielli, N.; Finlayson, C.; Ohkouchi, N.; Sanchez, M.C.; de Castro, J.M.; Blasco, R.; et al. Earliest evidence of pollution by heavy metals in archaeological sites. Sci. Rep. 2015, 5, 14252. [Google Scholar] [CrossRef] [PubMed]
- Waters, C.N.; Zalasiewicz, J.; Summerhayes, C.; Barnosky, A.D.; Poirier, C.; Galuszka, A.; Cearreta, A.; Edgeworth, M.; Ellis, E.C.; Ellis, M.; et al. The anthropocene is functionally and stratigraphically distinct from the holocene. Science 2016, 351, aad2622. [Google Scholar] [CrossRef] [PubMed]
- Voosen, P. Anthropocene pinned to postwar period. Science 2016, 353, 852–853. [Google Scholar] [CrossRef] [PubMed]
- Carey, J. Core concept: Are we in the “anthropocene”? Proc. Natl. Acad. Sci. USA 2016, 113, 3908–3909. [Google Scholar] [CrossRef] [PubMed]
- Allen, L. Are we facing a noncommunicable disease pandemic? J. Epidemiol. Glob. Health 2017, 7, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Logan, A.C.; Katzman, M.A.; Balanza-Martinez, V. Natural environments, ancestral diets, and microbial ecology: Is there a modern “paleo-deficit disorder”? Part II. J. Physiol. Anthropol. 2015, 34, 9. [Google Scholar] [CrossRef] [PubMed]
- Whalen, K.A.; Judd, S.; McCullough, M.L.; Flanders, W.D.; Hartman, T.J.; Bostick, R.M. Paleolithic and mediterranean diet pattern scores are inversely associated with all-cause and cause-specific mortality in adults. J. Nutr. 2017, 147, 612–620. [Google Scholar] [CrossRef] [PubMed]
- James, P.; Seward, M.W.; James O’Malley, A.; Subramanian, S.V.; Block, J.P. Changes in the food environment over time: Examining 40 years of data in the framingham heart study. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 84. [Google Scholar] [CrossRef] [PubMed]
- Zenk, S.N.; Tarlov, E.; Powell, L.M. Weight and veterans’ environments study (waves) I and II. Am. J. Health Promot. 2017. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, L.; Xue, H.; Qu, W. A review of the growth of the fast food industry in China and its potential impact on obesity. Int. J. Environ. Res. Public Health 2016, 13, 1112. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Moubarac, J.C.; Levy, R.B.; Canella, D.S.; Louzada, M.; Cannon, G. Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr. 2017, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Martinez Steele, E.; Popkin, B.M.; Swinburn, B.; Monteiro, C.A. The share of ultra-processed foods and the overall nutritional quality of diets in the U.S.: Evidence from a nationally representative cross-sectional study. Popul. Health Metr. 2017, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Moubarac, J.C.; Batal, M.; Louzada, M.L.; Martinez Steele, E.; Monteiro, C.A. Consumption of ultra-processed foods predicts diet quality in Canada. Appetite 2017, 108, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Stuart, H. Reducing the stigma of mental illness. Glob. Ment. Health 2016, 3, e17. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M.; Honeycutt, N.; Prislin, R.; Sherman, R.A. More polarized but more independent: Political party identification and ideological self-categorization among U.S. Adults, college students, and late adolescents, 1970–2015. Pers. Soc. Psychol. Bull. 2016, 42, 1364–1383. [Google Scholar] [CrossRef] [PubMed]
- Cosma, A.; Whitehead, R.; Neville, F.; Currie, D.; Inchley, J. Trends in bullying victimization in Scottish adolescents 1994–2014: Changing associations with mental well-being. Int. J. Public Health 2017, 62, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Rosen, C.C.; Koopman, J.; Gabriel, A.S.; Johnson, R.E. Who strikes back? A daily investigation of when and why incivility begets incivility. J. Appl. Psychol. 2016, 101, 1620–1634. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M. Overwhelming evidence for generation ME. Emerg. Adulthood 2013, 1, 21–26. [Google Scholar] [CrossRef]
- Twenge, J.M.; Campbell, W.K. Birth cohort differences in the monitoring the future dataset and elsewhere: Further evidence for generation me-commentary on Trzesniewski & Donnellan (2010). Perspect. Psychol. Sci. 2010, 5, 81–88. [Google Scholar] [PubMed]
- Bockler, A.; Sharifi, M.; Kanske, P.; Dziobek, I.; Singer, T. Social decision making in narcissism: Reduced generosity and increased retaliation are driven by alterations in perspective-taking and anger. Personal. Individ. Differ. 2017, 104, 1–7. [Google Scholar] [CrossRef]
- Campbell, W.K.; Bush, C.P.; Brunell, A.B.; Shelton, J. Understanding the social costs of narcissism: The case of the tragedy of the commons. Pers. Soc. Psychol. Bull. 2005, 31, 1358–1368. [Google Scholar] [CrossRef] [PubMed]
- Blinkhorn, V.; Lyons, M.; Almond, L. Drop the bad attitude! Narcissism predicts acceptance of violent behaviour. Personal. Individ. Differ. 2016, 98, 157–161. [Google Scholar] [CrossRef]
- Twenge, J.M.; Campbell, W.K.; Carter, N.T. Declines in trust in others and confidence in institutions among American adults and late adolescents, 1972–2012. Psychol. Sci. 2014, 25, 1914–1923. [Google Scholar] [CrossRef] [PubMed]
- Hampton, K.M. Why is helping behavior declining in the United States but not in Canada?: Ethnic diversity, new technologies, and other explanations. City Community 2016, 15, 380–399. [Google Scholar] [CrossRef]
- Stuckler, D. The dispossessed: A public health response to the rise of the far-right in Europe and North America. Eur. J. Public Health 2017, 27, 5–6. [Google Scholar] [CrossRef] [PubMed]
- McKee, M. Health professionals must uphold truth and human rights. Eur. J. Public Health 2017, 27, 6–7. [Google Scholar] [CrossRef] [PubMed]
- Baxter, A.J.; Scott, K.M.; Ferrari, A.J.; Norman, R.E.; Vos, T.; Whiteford, H.A. Challenging the Myth of an “epidemic” of common mental disorders: Trends in the global prevalence of anxiety and depression between 1990 and 2010. Depression Anxiety 2014, 31, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Janicki-Deverts, D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J. Appl. Soc. Psychol. 2012, 42, 1320–1334. [Google Scholar] [CrossRef]
- Boak, A.; Hamilton, H.A.; Adlaf, E.M.; Henderson, J.L.; Mann, R.E. The Mental Well-Being of Ontario Students, 1991–2015; CAMH Research Document No. 43; The Centre for Addiction and Mental Health: Toronto, ON, Canada, 2016. [Google Scholar]
- Rowlands, I.J.; Dobson, A.J.; Mishra, G.D. Physical health of young, Australian women: A comparison of two national cohorts surveyed 17 years apart. PLoS ONE 2015, 10, e0142088. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M. Time period and birth cohort differences in depressive symptoms in the U.S., 1982–2013. Soc. Indic. Res. 2015, 121, 437. [Google Scholar] [CrossRef]
- Glasgow, S.; Schrecker, T. The double burden of neoliberalism? Noncommunicable disease policies and the global political economy of risk. Health Place 2016, 39, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Brijnath, B.; Antoniades, J. “I’m running my depression:” Self-management of depression in neoliberal Australia. Soc. Sci. Med. 2016, 152, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Davies, J. Political pills: Psychopharmaceuticals and neoliberalism as mutually supporting. In The Sedated Society, lst ed.; Springer International: Gewerbestrasse, Switzerland, 2017; pp. 189–225. [Google Scholar]
- Salk, J. Research fund for human welfare. Daily Press 1966, 71, 34. [Google Scholar]
- Stassinopoulos, A. Dr Jonas Salk’s formula for the future. Courage. Love. Forgiveness. Parade Magazine, 4 Norvember 1984. [Google Scholar]
- Davidson, K. Jonas Salk tackles the meaning of life. Los Angeles Times, 6 July 1983; Section II: 1,5. [Google Scholar]
- Dubos, R. The human landscape. Bull. At. Sci. 1970, 26, 31–37. [Google Scholar] [CrossRef]
- Dubos, R. Priorities debated. Moon or earth? Index Journal, 28 July 1969; 4. [Google Scholar]
- Dubos, R. The genius of design. The Rest of Our Lives. In Proceedings of the International Design Conference, Aspen, CO, USA, 15–20 June 1969; pp. 57–63. [Google Scholar]
- Corburn, J. Concepts for studying urban environmental justice. Curr. Environ. Health Rep. 2017, 4, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Smith, K. Trillion-dollar brain drain. Nature 2011, 478, 15. [Google Scholar] [CrossRef] [PubMed]
- Bouchery, E.E.; Harwood, H.J.; Sacks, J.J.; Simon, C.J.; Brewer, R.D. Economic costs of excessive alcohol consumption in the U.S., 2006. Am. J. Prev. Med. 2011, 41, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Hansen, R.N.; Oster, G.; Edelsberg, J.; Woody, G.E.; Sullivan, S.D. Economic costs of nonmedical use of prescription opioids. Clin. J. Pain 2011, 27, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Al-Rousan, T.; Rubenstein, L.; Sieleni, B.; Deol, H.; Wallace, R.B. Inside the nation’s largest mental health institution: A prevalence study in a state prison system. BMC Public Health 2017, 17, 342. [Google Scholar] [CrossRef] [PubMed]
- Kiss, D.; Ambeskovic, M.; Montina, T.; Metz, G.A. Stress transgenerationally programs metabolic pathways linked to altered mental health. Cell. Mol. Life Sci. 2016, 73, 4547–4557. [Google Scholar] [CrossRef] [PubMed]
- Baams, L.; Talmage, C.A.; Russell, S.T. Economic costs of bias-based bullying. Sch. Psychol. Q. 2017. [Google Scholar] [CrossRef] [PubMed]
- Zurbrugg, L.; Miner, K.N. Gender, sexual orientation, and workplace incivility: Who is most targeted and who is most harmed? Front. Psychol. 2016, 7, 565. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.A. The cost of war on public health: An exploratory method for understanding the impact of conflict on public health in Sri Lanka. PLoS ONE 2017, 12, e0166674. [Google Scholar] [CrossRef] [PubMed]
- Thomas, H.J.; Connor, J.P.; Lawrence, D.M.; Hafekost, J.M.; Zubrick, S.R.; Scott, J.G. Prevalence and correlates of bullying victimisation and perpetration in a nationally representative sample of Australian youth. Aust. N. Z. J. Psychiatry 2017. [Google Scholar] [CrossRef] [PubMed]
- Wallace, L.N.; Menard, K.S. Friendships lost: The social consequences of violent victimization. J. Aggress. Maltreat. Trauma 2017, 26, 116–136. [Google Scholar] [CrossRef] [PubMed]
- Czarna, A.Z.; Leifeld, P.; Smieja, M.; Dufner, M.; Salovey, P. Do narcissism and emotional intelligence win us friends? Modeling dynamics of peer popularity using inferential network analysis. Pers. Soc. Psychol. Bull. 2016, 42, 1588–1599. [Google Scholar] [CrossRef] [PubMed]
- Goodman, G.; Gershwin, M.E.; Bercovich, D. Mars can wait: Facing the challenges of our civilization. Isr. Med. Assoc. J. 2014, 16, 744–747. [Google Scholar] [PubMed]
- U.S. House of Science, Space, and Technology. 115th Congress (2017–2018). National Aeronautics and Space Administration Transition Authorization Act of 2017. Available online: https://www.congress.gov/bill/115th-congress/senate-bill/442/text (accessed on 30 July 2017).
- National Institutes of Health (NIH). HHS FY 2017 Budget in Brief. Available online: https://www.hhs.gov/about/budget/fy2017/budget-in-brief/nih/index.html (accessed on 22 July 2017).
- Hiltzik, M. Trump’s Call for Human Space Exploration is Hugely Wasteful and Pointless. Available online: http://www.latimes.com/business/hiltzik/la-fi-hiltzik-trump-space-20170228-story.html (accessed on 30 August 2017).
- Vietnam War U.S. Casualties in 1969. Available online: http://www.vietnamwarcasualties.org/index.php?page=directory&dd=1969 (accessed on 30 July 2017).
- World Health Organization. Mental Health Atlas 2011. Available online: http://apps.who.int/iris/bitstream/10665/44697/1/9799241564359_eng.pdf (accessed on 12 July 2017).
- Locke, R. All the problems of man are not going to be solved in a laboratory. Advocate Newark 1984, 164, 1B. [Google Scholar]
- Salk, J.E. Biology in the future. Perspect. Biol. Med. 1962, 5, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Scarr, L. Dr. Salk: Book deals with man’s relation, not medicine. Courier-Post 1972, 97, 61. [Google Scholar]
- Salk, J.E. Biological basis of disease and behaviour. Perspect. Biol. Med. 1962, 5, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Dighton, R. Polio conqueror jonas salk readies new attack against disease. Prog. Index 1964, 100, 6. [Google Scholar]
- McEwen, B.S. Brain on stress: How the social environment gets under the skin. Proc. Natl. Acad. Sci. USA 2012, 109, 17180–17185. [Google Scholar] [CrossRef] [PubMed]
- Renz, H.; Holt, P.G.; Inouye, M.; Logan, A.C.; Prescott, S.L.; Sly, P.D. An exposome perspective: Early-life events and immune development in a changing world. J. Allergy Clin. Immunol. 2017, 140, 24–40. [Google Scholar] [CrossRef] [PubMed]
- Franco, F.G.M.; Laurinavicius, A.G.; Lotufo, P.A.; Conceicao, R.D.; Morita, F.; Katz, M.; Wajngarten, M.; Carvalho, J.A.M.; Bosworth, H.B.; Santos, R.D. Persistent depressive symptoms are independent predictors of low-grade inflammation onset among healthy individuals. Arq. Bras. Cardiol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.Y.; Wagner, J.T.; Glaus, J.; Vandeleur, C.L.; Castelao, E.; Strippoli, M.P.; Vollenweider, P.; Preisig, M.; von Kanel, R. Evidence for chronic low-grade systemic inflammation in individuals with agoraphobia from a population-based prospective study. PLoS ONE 2015, 10, e0123757. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Messay, B.; Lim, A.; Marsland, A.L. Current understanding of the bi-directional relationship of major depression with inflammation. Biol. Mood Anxiety Disord. 2012, 2, 4. [Google Scholar] [CrossRef] [PubMed]
- Ligthart, S.; Marzi, C.; Aslibekyan, S.; Mendelson, M.M.; Conneely, K.N.; Tanaka, T.; Colicino, E.; Waite, L.L.; Joehanes, R.; Guan, W.; et al. DNA methylation signatures of chronic low-grade inflammation are associated with complex diseases. Genome Biol. 2016, 17, 255. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; Pounis, G.; De Curtis, A.; Costanzo, S.; Persichillo, M.; Cerletti, C.; Donati, M.B.; de Gaetano, G.; Iacoviello, L.; et al. A score of low-grade inflammation and risk of mortality: Prospective findings from the moli-sani study. Haematologica 2016, 101, 1434–1441. [Google Scholar] [CrossRef] [PubMed]
- Chehoud, C.; Rafail, S.; Tyldsley, A.S.; Seykora, J.T.; Lambris, J.D.; Grice, E.A. Complement modulates the cutaneous microbiome and inflammatory milieu. Proc. Natl. Acad. Sci. USA 2013, 110, 15061–15066. [Google Scholar] [CrossRef] [PubMed]
- Zeng, M.Y.; Inohara, N.; Nunez, G. Mechanisms of inflammation-driven bacterial dysbiosis in the gut. Mucosal Immunol. 2017, 10, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Sender, R.; Fuchs, S.; Milo, R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016, 14, e1002533. [Google Scholar] [CrossRef] [PubMed]
- Human Microbiome Project Consortium. A framework for human microbiome research. Nature 2012, 486, 215–221. [Google Scholar] [Green Version]
- Prescott, S.L. History of medicine: Origin of the term microbiome and why it matters. Hum. Microbiome J. 2017, 4, 24–25. [Google Scholar] [CrossRef]
- Gupta, V.K.; Paul, S.; Dutta, C. Geography, ethnicity or subsistence-specific variations in human microbiome composition and diversity. Front. Microbiol. 2017, 8, 1162. [Google Scholar] [CrossRef] [PubMed]
- Segata, N. Gut microbiome: Westernization and the disappearance of intestinal diversity. Curr. Biol. 2015, 25, R611–R613. [Google Scholar] [CrossRef] [PubMed]
- Sonnenburg, E.D.; Smits, S.A.; Tikhonov, M.; Higginbottom, S.K.; Wingreen, N.S.; Sonnenburg, J.L. Diet-induced extinctions in the gut microbiota compound over generations. Nature 2016, 529, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Petersen, C.; Round, J.L. Defining dysbiosis and its influence on host immunity and disease. Cell. Microbiol. 2014, 16, 1024–1033. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.J.; Li, S.; Gan, R.Y.; Zhou, T.; Xu, D.P.; Li, H.B. Impacts of gut bacteria on human health and diseases. Int. J. Mol. Sci. 2015, 16, 7493–7519. [Google Scholar] [CrossRef] [PubMed]
- Logan, A.C. Dysbiotic drift: Mental health, environmental grey space, and microbiota. J. Physiol. Anthropol. 2015, 34, 23. [Google Scholar] [CrossRef] [PubMed]
- Corburn, J. Confronting the challenges in reconnecting urban planning and public health. Am. J. Public Health 2004, 94, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Cheon, B.K.; Hong, Y.Y. Mere experience of low subjective socioeconomic status stimulates appetite and food intake. Proc. Natl. Acad. Sci. USA 2017, 114, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Bratanova, B.; Loughnan, S.; Klein, O.; Claassen, A.; Wood, R. Poverty, inequality, and increased consumption of high calorie food: Experimental evidence for a causal link. Appetite 2016, 100, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Cardel, M.I.; Johnson, S.L.; Beck, J.; Dhurandhar, E.; Keita, A.D.; Tomczik, A.C.; Pavela, G.; Huo, T.; Janicke, D.M.; Muller, K.; et al. The effects of experimentally manipulated social status on acute eating behavior: A randomized, crossover pilot study. Physiol. Behav. 2016, 162, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Laxer, R.E.; Janssen, I. The proportion of excessive fast-food consumption attributable to the neighbourhood food environment among youth living within 1 km of their school. Appl. Physiol. Nutr. Metab. 2014, 39, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Lucan, S.C.; Maroko, A.R.; Sanon, O.C.; Schechter, C.B. Unhealthful food-and-beverage advertising in subway stations: Targeted marketing, vulnerable groups, dietary intake, and poor health. J. Urban Health Bull. N. Y. Acad. Med. 2017, 94, 220–232. [Google Scholar] [CrossRef] [PubMed]
- Arredondo, E.; Castaneda, D.; Elder, J.P.; Slymen, D.; Dozier, D. Brand name logo recognition of fast food and healthy food among children. J. Community Health 2009, 34, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Zenk, S.N.; Powell, L.M.; Rimkus, L.; Isgor, Z.; Barker, D.C.; Ohri-Vachaspati, P.; Chaloupka, F. Relative and absolute availability of healthier food and beverage alternatives across communities in the United States. Am. J. Public Health 2014, 104, 2170–2178. [Google Scholar] [CrossRef] [PubMed]
- Rimkus, L.; Isgor, Z.; Ohri-Vachaspati, P.; Zenk, S.N.; Powell, L.M.; Barker, D.C.; Chaloupka, F.J. Disparities in the availability and price of low-fat and higher-fat milk in U.S. food stores by community characteristics. J. Acad. Nutr. Diet. 2015, 115, 1975–1985. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.J.; Thornton, L.E.; McNaughton, S.A.; Crawford, D. Variation in supermarket exposure to energy-dense snack foods by socio-economic position. Public Health Nutr. 2013, 16, 1178–1185. [Google Scholar] [CrossRef] [PubMed]
- Rose, D.; Hutchinson, P.L.; Bodor, J.N.; Swalm, C.M.; Farley, T.A.; Cohen, D.A.; Rice, J.C. Neighborhood food environments and body mass index: The importance of in-store contents. Am. J. Prev. Med. 2009, 37, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Farley, T.A.; Rice, J.; Bodor, J.N.; Cohen, D.A.; Bluthenthal, R.N.; Rose, D. Measuring the food environment: Shelf space of fruits, vegetables, and snack foods in stores. J. Urban Health Bull. N. Y. Acad. Med. 2009, 86, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Burgoine, T.; Forouhi, N.G.; Griffin, S.J.; Brage, S.; Wareham, N.J.; Monsivais, P. Does neighborhood fast-food outlet exposure amplify inequalities in diet and obesity? A cross-sectional study. Am. J. Clin. Nutr. 2016, 103, 1540–1547. [Google Scholar] [CrossRef] [PubMed]
- Kahr, M.K.; Suter, M.A.; Ballas, J.; Ramin, S.M.; Monga, M.; Lee, W.; Hu, M.; Shope, C.D.; Chesnokova, A.; Krannich, L.; et al. Geospatial analysis of food environment demonstrates associations with gestational diabetes. Am. J. Obstet. Gynecol. 2016, 214, 110.e1–110.e9. [Google Scholar] [CrossRef] [PubMed]
- Turi, K.N.; Grigsby-Toussaint, D.S. Spatial spillover and the socio-ecological determinants of diabetes-related mortality across us counties. Appl. Geogr. 2017, 85, 62–72. [Google Scholar] [CrossRef]
- Moodie, R.; Stuckler, D.; Monteiro, C.; Sheron, N.; Neal, B.; Thamarangsi, T.; Lincoln, P.; Casswell, S.; Lancet, N.C.D.A.G. Profits and pandemics: Prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013, 381, 670–679. [Google Scholar] [CrossRef]
- Albrecht, G. Ecopsychology in the symbiocene. Ecopsychology 2014, 6, 58–59. [Google Scholar] [CrossRef]
- Manzoni, C.; Kia, D.A.; Vandrovcova, J.; Hardy, J.; Wood, N.W.; Lewis, P.A.; Ferrari, R. Genome, transcriptome and proteome: The rise of omics data and their integration in biomedical sciences. Brief. Bioinform. 2016. [Google Scholar] [CrossRef]
- Ceballos, G.; Ehrlich, P.R.; Dirzo, R. Biological annihilation via the ongoing sixth mass extinction signaled by vertebrate population losses and declines. Proc. Natl. Acad. Sci. USA 2017, 114, E6089–E6096. [Google Scholar] [CrossRef] [PubMed]
- Weintraub, P. The new epoch: Jonas Salk. In The Omni Interviews; Weintraub, P., Ed.; Ticknor and fields: Boston, MA, USA, 1984; pp. 94–115. [Google Scholar]
- Salk, J. The Survival of the Wisest; Harper and Row: San Francisco, CA, USA, 1973. [Google Scholar]
- Huff, C. The growth of holistic health. Philadelphia Inquirer, 3 November 1977; 52. [Google Scholar]
- Newsmakers: The challenge of science, Jonas Salk speaks. Philadelphia Inquirer, 11 October 1992; 3.
- Albrecht, G.A. Exiting the anthropocene and entering the symbiocene. Minding Nat. 2016, 9, 12–16. [Google Scholar]
- Christian, N.; Herre, E.A.; Mejia, L.C.; Clay, K. Exposure to the leaf litter microbiome of healthy adults protects seedlings from pathogen damage. Proc. Biol. Sci. 2017, 284, 20170641. [Google Scholar] [CrossRef] [PubMed]
- Soga, M.; Gaston, K.J.; Yamaura, Y.; Kurisu, K.; Hanaki, K. Both direct and vicarious experiences of nature affect children’s willingness to conserve biodiversity. Int. J. Environ. Res. Public Health 2016, 13, 529. [Google Scholar] [CrossRef] [PubMed]
- Watt, K.; Abbott, P.; Reath, J. Developing cultural competence in general practitioners: An integrative review of the literature. BMC Fam. Pract. 2016, 17, 158. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Integrative medicine: Breaking down silos of knowledge and practice an epigenetic approach. Metab. Clin. Exp. 2017, 69S, S21–S29. [Google Scholar] [CrossRef] [PubMed]
- Gray, B. How should we respond to non-dominant healing practices, the example of homeopathy. J. Bioeth. Inq. 2017, 14, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Cloud, R. No Funds for Homeless Vets. Program Eliminated in King. Available online: http://www.waupacanow.com/2017/07/17/no-funds-for-homeless-vets/ (accessed on 30 July 2017).
- Halpern, L.W. Analysis finds about 20 veterans died daily from suicide between 2001 and 2014. Am. J. Nurs. 2016, 116, 17. [Google Scholar] [CrossRef] [PubMed]
- McKee, M.; Stuckler, D.; Zeegers Paget, D.; Dorner, T. The Vienna declaration on public health. Eur. J. Public Health 2016, 26, 897–898. [Google Scholar] [CrossRef] [PubMed]
- Shelton, D.L. Problems in environmental protection and human rights: A human right to the environment. GL Law Scholarly Commons 2011. [Google Scholar] [CrossRef]
- United Nations General Assembly. Convention on the Rights of the Child; United Nations Treaty Series; United Nations General Assembly: New York, NY, USA, 1989. [Google Scholar]
- Craig, J.M.; Logan, A.C.; Prescott, S.L. Natural environments, nature relatedness and the ecological theater: Connecting satellites and sequencing to Shinrin-Yoku. J. Physiol. Anthropol. 2016, 35, 1. [Google Scholar] [CrossRef] [PubMed]
- Metz, A.L. Back to nature: The relationship between nature relatedness on empathy and narcissism in the millennial generation. Vistas Online 2017, 11, 1–14. [Google Scholar]
- Martyn, P.; Brymer, E. The relationship between nature relatedness and anxiety. J. Health Psychol. 2016, 21, 1436–1445. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Geng, L.; Xiang, P.; Zhang, J.; Zhu, L. Nature connectedness: It’s concept, measurement, function and intervention. Adv. Psychol. Sci. 2017, 25, 1360–1374. [Google Scholar]
- Asah, S.T.; Bengston, D.N.; Westphal, L.M.; Gowan, C.H. Mechanisms of children’s exposure to nature: Predicting adulthood environmental citizenship and commitment to nature-based activities. Environ. Behav. 2017. [Google Scholar] [CrossRef]
- Allemand, M.; Steiger, A.E.; Fend, H.A. Empathy development in adolescence predicts social competencies in adulthood. J. Pers. 2015, 83, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Alvarez, N.; Extremera, N.; Fernandez-Berrocal, P. The relation between emotional intelligence and subjective well-being: A meta-analytic investigation. J. Posit. Psychol. 2016, 11, 276–285. [Google Scholar] [CrossRef]
- Schutte, N.S.; Malouff, J.M.; Thorsteinsson, E.B.; Bhullar, N.; Rooke, S.E. A meta-analytic investigation of the relationship between emotional intelligence and health. Pers. Indiv. Differ. 2007, 42, 921–933. [Google Scholar] [CrossRef]
- Zeidner, M.; Matthews, G.; Roberts, R.D. The emotional intelligence, health, and well-being nexus: What have we learned and what have we missed? Appl. Psychol. Health Well Being 2012, 4, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Extremera, N.; Rey, L. Ability emotional intelligence and life satisfaction: Positive and negative affect as mediators. Person.l Indiv. Diff. 2016, 102, 98–101. [Google Scholar] [CrossRef]
- Abdollahi, A.; Abu Talib, M.; Motalebi, S.A. Emotional intelligence and depressive symptoms as predictors of happiness among adolescents. Iran J. Psychiatry Behav. Sci. 2015, 9, e2268. [Google Scholar] [CrossRef] [PubMed]
- Killgore, W.D.; Kahn-Greene, E.T.; Lipizzi, E.L.; Newman, R.A.; Kamimori, G.H.; Balkin, T.J. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Med. 2008, 9, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Mavroveli, S.; Sanchez-Ruiz, M.J. Trait emotional intelligence influences on academic achievement and school behaviour. Br. J. Educ. Psychol. 2011, 81, 112–134. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.; Faria, L. The impact of emotional intelligence on academic achievement: A longitudinal study in Portuguese secondary school. Learn Individ. Differ. 2015, 37, 38–47. [Google Scholar] [CrossRef]
- Curci, A.; Lanciano, T.; Soleti, E. Emotions in the classroom: The role of teachers’ emotional intelligence ability in predicting students’ achievement. Am. J. Psychol. 2014, 127, 431–445. [Google Scholar] [CrossRef] [PubMed]
- Aminabadi, N.A.; Pourkazemi, M.; Babapour, J.; Oskouei, S.G. The impact of maternal emotional intelligence and parenting style on child anxiety and behavior in the dental setting. Med. Oral Patol. Oral 2012, 17, E1089–E1095. [Google Scholar] [CrossRef]
- Ulutas, I.; Omeroglu, E. Maternal attitudes, emotional intelligence and home environment and their relations with emotional intelligence of sixth years old children, emotional intelligence. In New Perspectives and Applications; di fabio, A., Ed.; Intech: Rijeka, Croatia, 2012. [Google Scholar]
- Slaski, M.; Cartwright, S. Emotional intelligence training and its implications for stress, health and performance. Stress Health 2003, 19, 233–239. [Google Scholar] [CrossRef]
- Nyklicek, I.; Schalken, P.; Meertens, S. The role of emotional intelligence in symptom reduction after psychotherapy in a heterogeneous psychiatric sample. Compr. Psychiat. 2015, 57, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Castillo, R.; Salguero, J.M.; Fernandez-Berrocal, P.; Balluerka, N. Effects of an emotional intelligence intervention on aggression and empathy among adolescents. J. Adolescence 2013, 36, 883–892. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; De Curtis, A.; Costanzo, S.; Bracone, F.; Persichillo, M.; Donati, M.B.; de Gaetano, G.; Iacoviello, L.; Moli-sani Project, I. Nut consumption is inversely associated with both cancer and total mortality in a mediterranean population: Prospective results from the Moli-Sani study. Br. J. Nutr. 2015, 114, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Dubos, R. Symbiosis between the earth and humankind. Science 1976, 193, 459–462. [Google Scholar] [CrossRef] [PubMed]
- Azeredo, C.M.; Santos, I.S.; Barros, A.J.D.; Barros, F.C.; Matijasevich, A. Maternal depression and bullying victimization among adolescents: Results from the 2004 pelotas cohort study. Depress Anxiety 2017. [Google Scholar] [CrossRef] [PubMed]
- Horton, R.; Beaglehole, R.; Bonita, R.; Raeburn, J.; McKee, M.; Wall, S. From public to planetary health: A manifesto. Lancet 2014, 383, 847. [Google Scholar] [CrossRef]
- Wang, Y.; Jing, X.; Lv, K.; Wu, B.; Bai, Y.; Luo, Y.; Chen, S.; Li, Y. During the long way to mars: Effects of 520 days of confinement (mars500) on the assessment of affective stimuli and stage alteration in mood and plasma hormone levels. PLoS ONE 2014, 9, e87087. [Google Scholar] [CrossRef] [PubMed]
- Schuster, H.; Peck, S.L. Mars ain’t the kind of place to raise your kid: Ethical implications of pregnancy on missions to colonize other planets. Life Sci. Soc. Policy 2016, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Smollar, D. 30 years after 1st vaccine, dr jonas salk still strives to eradicate polio. Los Angeles Times, 7 April 1985; Part II. 9. [Google Scholar]
- Heuck, D. Institute a blueprint for a new way of thinking. Pittsburgh-Post Gazette, 28 November 1994; a1–a6. [Google Scholar]
- Houseman, M.P. Salk believes institute most important creation. Ottawa J. 1980, 12, 32. [Google Scholar]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prescott, S.L.; Logan, A.C. Down to Earth: Planetary Health and Biophilosophy in the Symbiocene Epoch. Challenges 2017, 8, 19. https://doi.org/10.3390/challe8020019
Prescott SL, Logan AC. Down to Earth: Planetary Health and Biophilosophy in the Symbiocene Epoch. Challenges. 2017; 8(2):19. https://doi.org/10.3390/challe8020019
Chicago/Turabian StylePrescott, Susan L., and Alan C. Logan. 2017. "Down to Earth: Planetary Health and Biophilosophy in the Symbiocene Epoch" Challenges 8, no. 2: 19. https://doi.org/10.3390/challe8020019




