Strategic Design and Fabrication of Engineered Scaffolds for Articular Cartilage Repair
Abstract
:1. Introduction
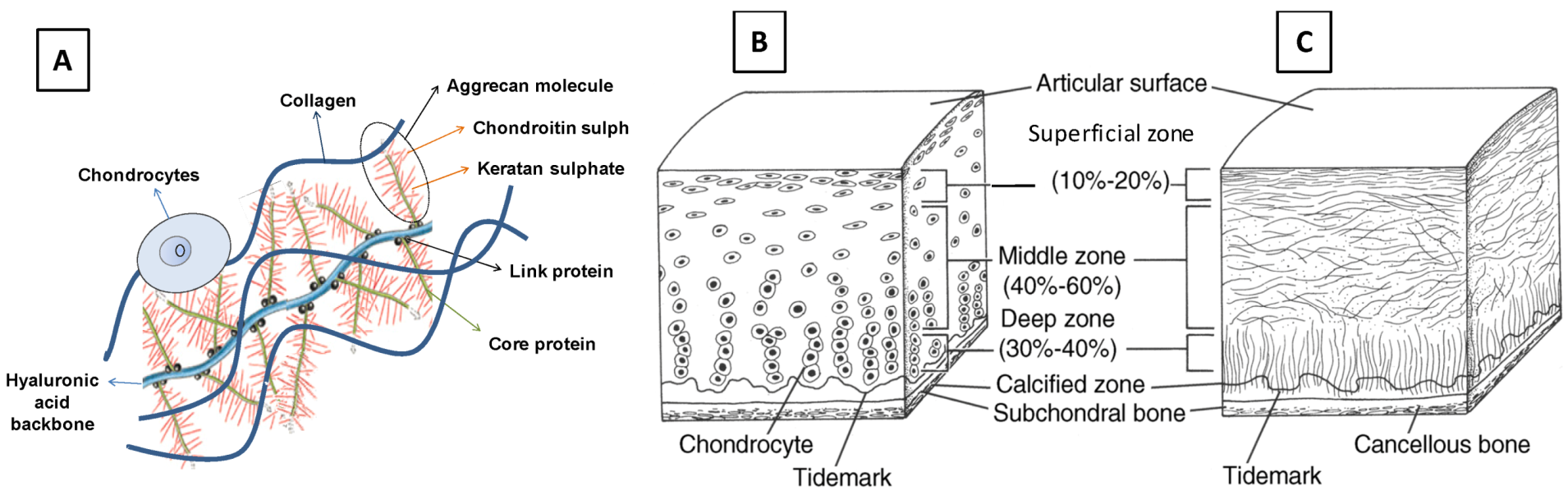
1.1. Structure and Organization of Natural Articular Cartilage
1.2. Cartilage Injuries, Osteoarthritis (OA), and Traditional Cartilage Repair Strategies
2. Scaffold Design for Cartilage Tissue Engineering
2.1. Scaffold Backbone Materials
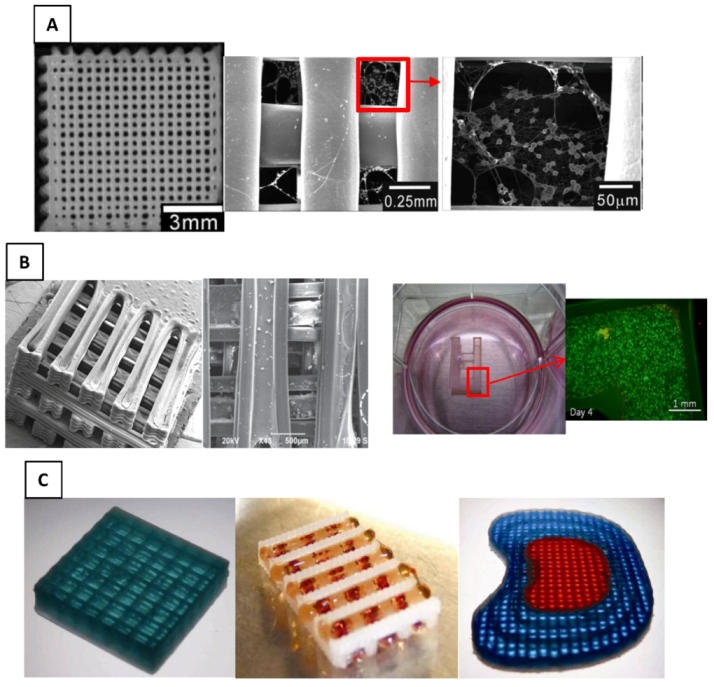
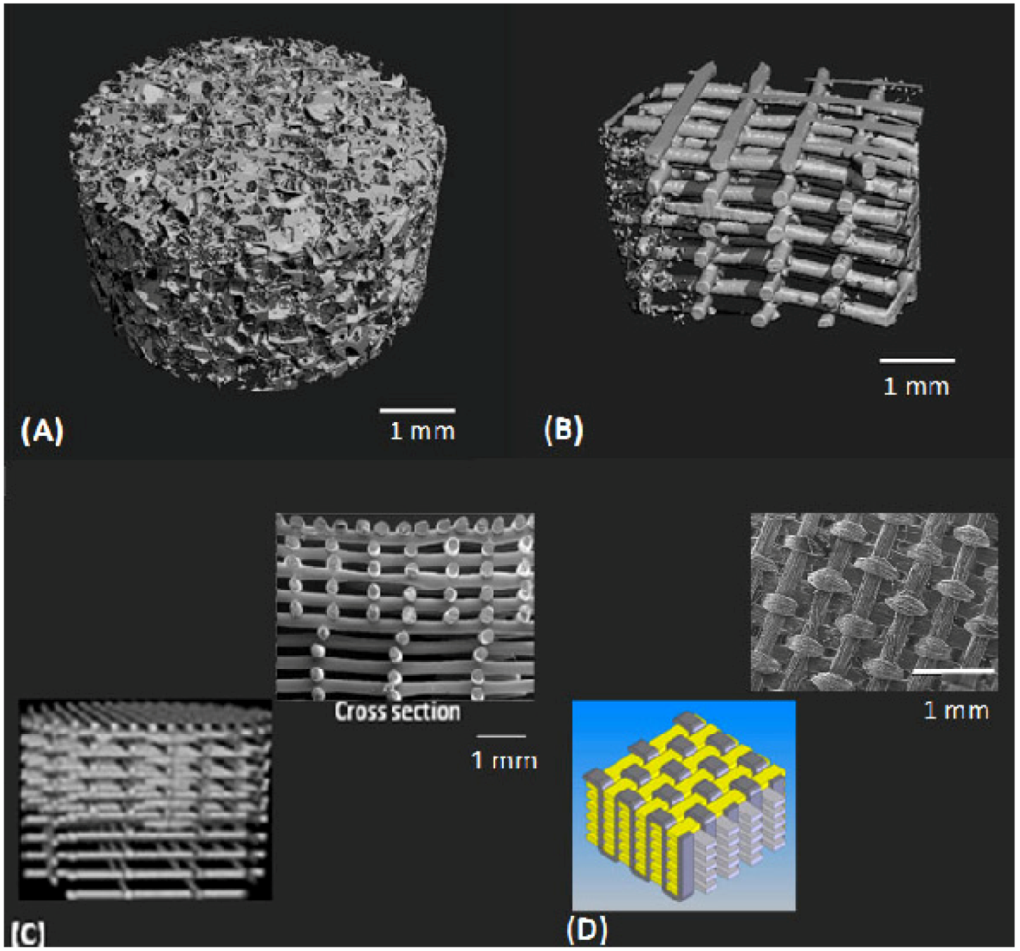
2.2. Scaffold Physical Architecture
| Scaffold | Avg. Pore size (µm) | Porosity | Surface area (mm2/mm3) | Interconnectivity | Fiber size | References |
|---|---|---|---|---|---|---|
| Sponge | 50–500 | 48%–95% | 55.6 | <100% | -- | [37,98,99,100,101,102] |
| (low cut off value*) | ||||||
| Fibrous | 100–1650 | 48%–87% | 16.5 | 100% (high cut off value) | 30–250 µm | [21,34,61,70,85,103,104,105,106] |
| Macro fibers | ||||||
| 20–80 | 84%–90% | -- | -- | 60–100 µm | ||
| Micro/nano fibers |
2.3. Mechanical Properties
| Mechanical properties | Healthy human articular cartilage | References | Cartilage TE construct | References |
|---|---|---|---|---|
| Tensile Young’s modulus (MPa) | 5–25 | [134,135,136] | 0.089–400 | [34,46,137,138] |
| Ultimate tensile stress (MPa) | 15–35 | [139,140] | 5.27–85 | [34,46,137] |
| Compression Young’s modulus (MPa) | 0.24–0.85 | [141,142,143] | 0.005–5.9 | [46,70,123] |
| Complex shear modulus (MPa) | 0.2–2.0 | [144] | 0.023–0.11 | [46,145] |
2.4. Degradation Properties
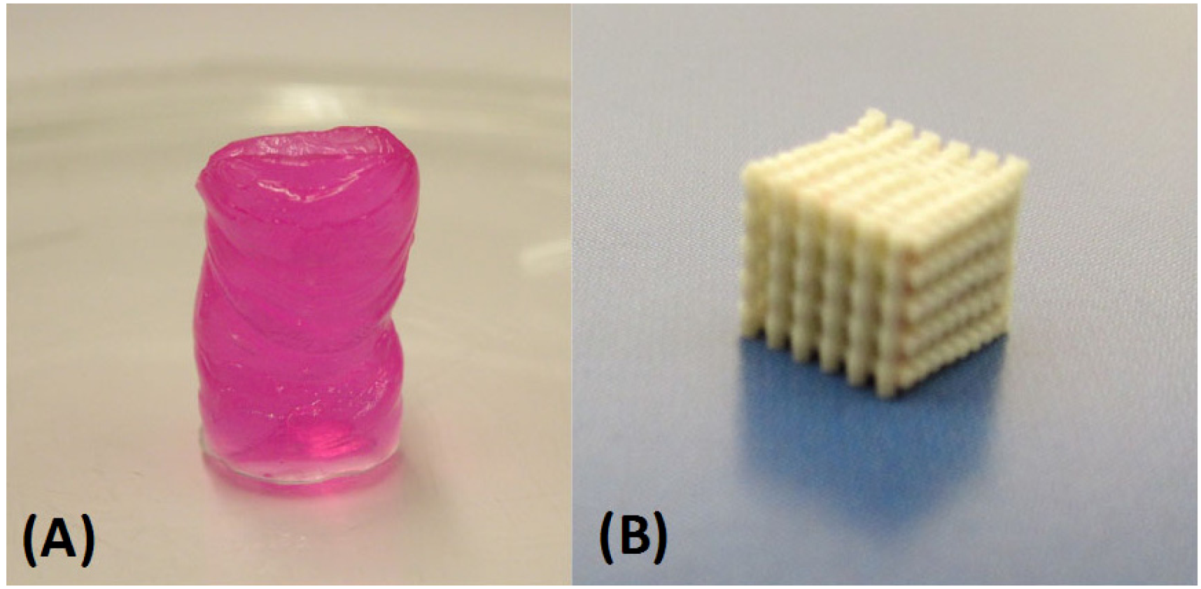
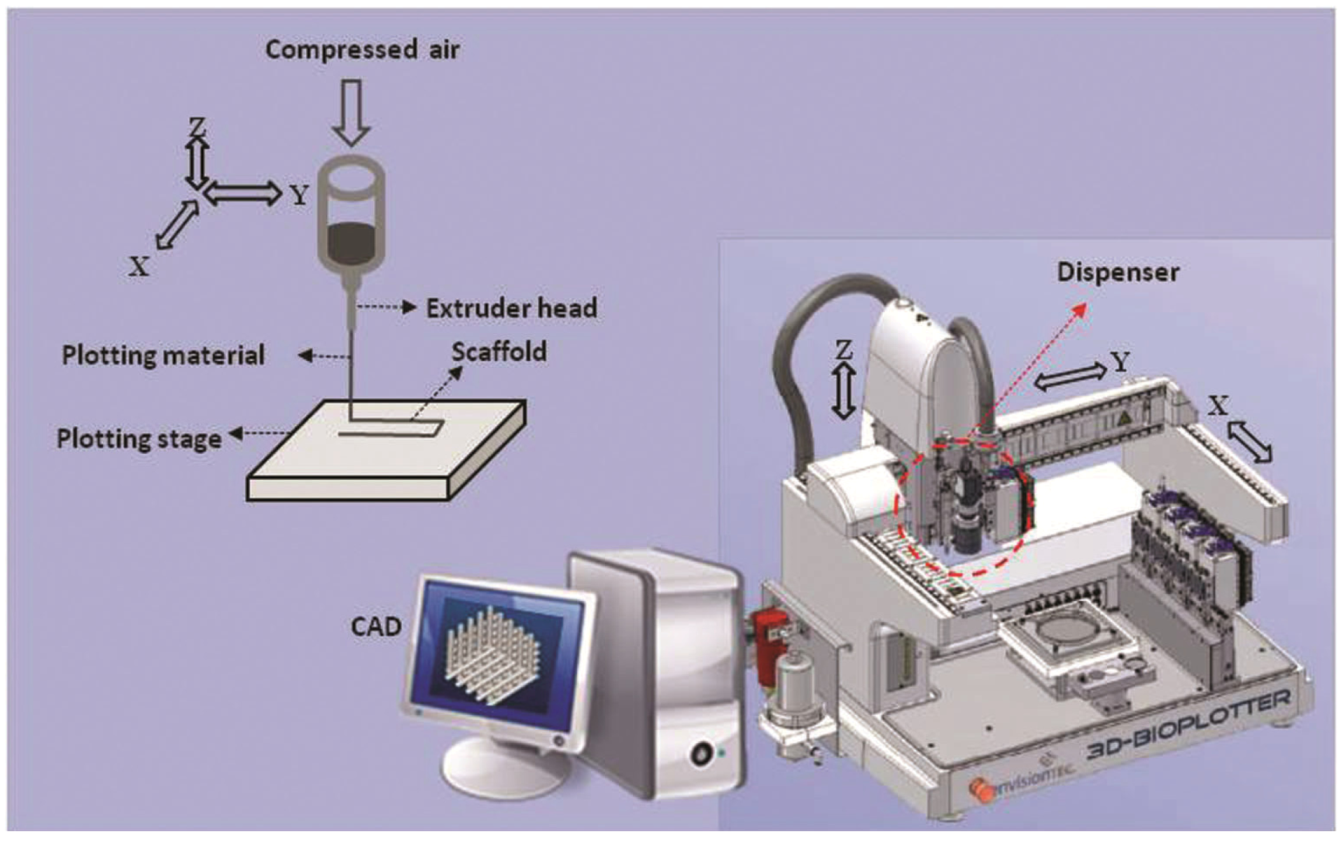
3. Fabrication of Designed Scaffolds
| Merits and demerits | Electrospinning | Bioplotter-additive manufacturing |
|---|---|---|
| Merits |
| |
| Demerits |
|
4. Strategic Scaffold Designs for Cartilage Tissue Engineering
4.1. Hybrid Scaffolds
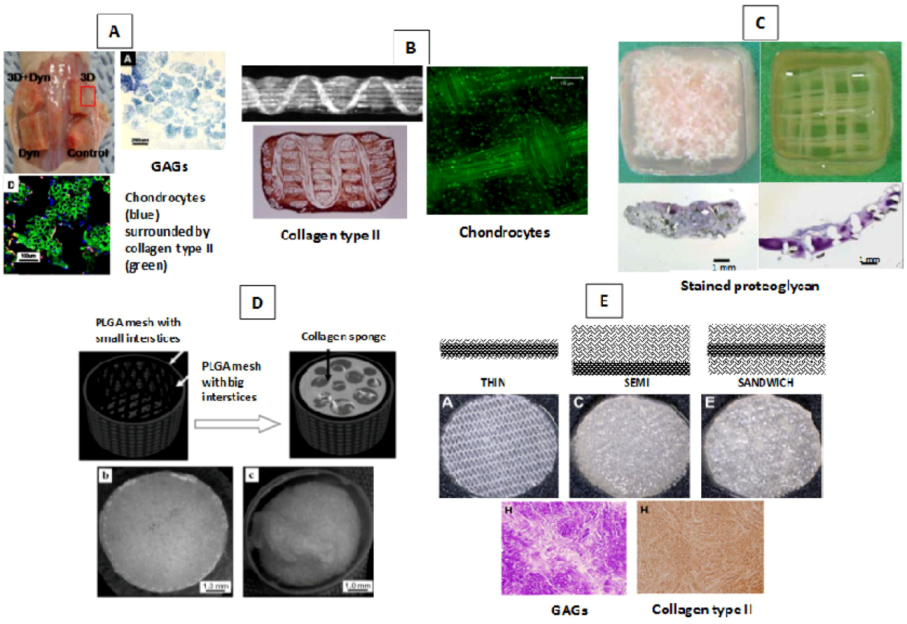
4.2. Zonal Scaffolds
5. Conclusions and Recommendations for Future Research
Conflict of Interest
Acknowledgments
References
- Moutos, F.T.; Guilak, F. Composite scaffolds for cartilage tissue engineering. J. Biorheol. 2008, 45, 501–512. [Google Scholar]
- Mow, V.C.; Ratcliffe, A.; Poole, A.R. Cartilage and diarthrodial joints as paradigms for hierarchical materials and structures. Biomaterials 1992, 13, 67–97. [Google Scholar] [CrossRef]
- Haleem, A.M.; Chu, C.R. Advances in tissue engineering techniques for articular cartilage repair. Oper. Tech. Orthop. 2010, 20, 76–89. [Google Scholar] [CrossRef]
- Gillogly, S.D.; Voightm, M.; Blackburn, T. Treatment of articular cartilage defects of the knee with autologous chondrocyte implantation. J. Orthop. Sports Phys. Ther. 1998, 28, 241–251. [Google Scholar]
- Athanasiou, K.A.; Darling, E.M.; Hu, J.C. Articular cartilage tissue engineering. In Synthesis Lectures on Tissue Engineering, 1st; Athanasiou K.A. Leach, J.K., Ed.; Morgan & Claypool: San Rafael, CA, USA, 2009; pp. 1–182. [Google Scholar]
- Alford, J.W.; Cole, B.J. Cartilage restoration, Part 2: Techniques, outcomes, and future directions. Am. J. Sports Med. 2005, 33, 443–460. [Google Scholar] [CrossRef]
- Lavik, E.; Langer, R. Tissue engineering: Current state and perspectives. Appl. Microbiol. Biotechnol. 2004, 65, 1–8. [Google Scholar]
- Mikos, A.G.; Herring, S.W.; Ochareon, P.; Elisseeff, J.; Lu, H.H.; Kandel, R.; Schoen, F.J.; Toner, M.; Mooney, D.; Atala, A.; Van Dyke, M.E.; Kaplan, D.; Vunjak-Novakovic, G. Engineering complex tissues. Tissue Eng. 2006, 12, 3307–3339. [Google Scholar] [CrossRef]
- Niklason, L.E.; Langer, R. Prospects for organ and tissue replacement. JAMA 2001, 285, 573–576. [Google Scholar] [CrossRef]
- Goldberg, M.; Langer, R.; Jia, X. Nanostructured materials for applications in drug delivery and tissue engineering. J. Biomater. Sci. Polym. Ed. 2007, 18, 241–268. [Google Scholar] [CrossRef]
- Athanasiou, K.A.; Niederauer, G.G.; Agrawal, C.M. Sterilization, toxicity, biocompatibility and clinical applications of polylactic Acid/Polyglycolic acid copolymers. Biomaterials 1996, 17, 93–102. [Google Scholar]
- Cima, L.G.; Vacanti, J.P.; Vacanti, C.; Ingber, D.; Mooney, D.; Langer, R. Tissue engineering by cell transplantation using degradable polymer substrates. J. Biomech. Eng. 1991, 113, 143–151. [Google Scholar]
- Freed, L.E.; Vunjak-Novakovic, G.; Biron, R.J.; Eagles, D.B.; Lesnoy, D.C.; Barlow, S.K.; Langer, R. Biodegradable polymer scaffolds for tissue engineering. Biotechnology 1994, 12, 689–693. [Google Scholar]
- Mikos, A.G.; Bao, Y.; Cima, L.G.; Ingber, D.E.; Vacanti, J.P.; Langer, R. Preparation of poly(glycolic acid) bonded fiber structures for cell attachment and transplantation. J Biomed. Mater. Res. 1993, 27, 183–189. [Google Scholar] [CrossRef]
- Buckwalter, J.A.; Mankin, H.J.; Grodzinsky, A.J. Articular cartilage and osteoarthritis. Instr. Course Lect. 2005, 54, 465–480. [Google Scholar]
- Ateshian, G.A.; Lai, W.M.; Zhu, W.B.; Mow, V.C. An asymptotic solution for the contact of two biphasic cartilage layers. J. Biomech. 1994, 27, 1347–1360. [Google Scholar] [CrossRef]
- Buckwalter, J.A.; Mow, V.C.; Ratcliffe, A. Restoration of injured or degenerated articular cartilage. J. Am. Acad. Orthop. Surg. 1994, 2, 192–201. [Google Scholar]
- Buckwalter, J.A.; Hunziker, E.B.; Rosenberg, L.C.; Coutts, R.D.; Adams, M.E.; Eyre, D.R. Articular cartilage. Composition and structure. In Injury and Repair of the Musculoskeletal Soft Tissues; Woo, S.L.-Y., Buckwalter, J.A., Eds.; The American Academy of Orthopaedic Surgeons: Park Ridge, IL, USA, 1988; pp. 405–425. [Google Scholar]
- Meachim, G.; Sheffield, S.R. Surface ultrastructure of mature adult human articular cartilage. J. Bone Joint. Surg. Br. 1969, 51, 529–539. [Google Scholar]
- Muir, H.; Bullough, P.; Maroudas, A. The distribution of collagen in human articular cartilage with some of its physiological implications. J. Bone Joint. Surg. Br. 1970, 52, 554–563. [Google Scholar]
- Klein, T.J.; Malda, J.; Sah, R.L.; Hutmacher, D.W. Tissue engineering of articular cartilage with biomimetic zones. Tissue Eng. Part B 2009, 15, 143–157. [Google Scholar] [CrossRef]
- Huang, C.Y.; Stankiewicz, A.; Ateshian, G.A.; Mow, V.C. Anisotropy, inhomogeneity, and tension-compression nonlinearity of human glenohumeral cartilage in finite deformation. J. Biomech. 2005, 38, 799–809. [Google Scholar]
- Venn, M.; Maroudas, A. Chemical composition and swelling of normal and osteoarthrotic femoral head cartilage. I. Chemical composition. Ann. Rheum. Dis. 1977, 36, 121–129. [Google Scholar]
- Eggli, P.S.; Hunziker, E.B.; Schenk, R.K. Quantitation of structural features characterizing weight- and less- weight-bearing regions in articular cartilage: A stereological analysis of medial femoral condyles in young adult rabbits. Anat. Rec. 1988, 222, 217–227. [Google Scholar] [CrossRef]
- Radin, E.L.; Ehrlich, M.G.; Chernack, R.; Abernethy, P.; Paul, I.L.; Rose, R.M. Effect of repetitive impulsive loading on the knee joints of rabbits. Clin. Orthop. Relat. Res. 1978, 131, 288–293. [Google Scholar]
- Brittberg, M.; Lindahl, A.; Nilsson, A.; Ohlsson, C.; Isaksson, O.; Peterson, L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N. Engl. J. Med. 1994, 331, 889–995. [Google Scholar]
- Bi, X.; Li, G.; Doty, S.B.; Camacho, N.P. A novel method for determination of collagen orientation in cartilage by fourier transform infrared imaging spectroscopy (FT-IRIS). Osteoarth. Cart. 2005, 13, 1050–1058. [Google Scholar]
- Chang, C.H.; Lin, F.H; Kuo, T.F.; Liu, H.C. Cartilage tissue engineering. Biomed. Eng. Appl. Basis Comm. 2005, 17, 1–11. [Google Scholar] [CrossRef]
- Horas, U.; Pelinkovic, D.; Herr, G.; Aigner, T.; Schnettler, R. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint: A prospective, comparative trial. J. Bone Joint Surg. Am. 2003, 85, 185–192. [Google Scholar]
- Roberts, S.; Menage, J.; Sandell, L.J.; Evans, E.H.; Richardson, J.B. Immunohistochemical study of collagen types I and II and procollagen IIa in human cartilage repair tissue following autologous chondrocyte implantation. Knee 2009, 16, 398–404. [Google Scholar] [CrossRef]
- Osteotomy of the knee. AAOS (American Academy of Orthopaedic Surgeons) Website. Available online: http://orthoinfo.aaos.org/topic.cfm?topic=A00591 (accessed on 26 October 2012).
- Hutmacher, D.; Woodfield, T.; Dalton, P.D.; Lewis, J.A. Scaffold design and fabrication. In Tissue Engineering; van Blitterswijk, C., Thomsen, P., Hubbell, J., Cancedda, R., de Bruijn, J., Lindahl, A., Sohier, J., Williams, D.F., Eds.; Elsevier Academic Press: London, UK, 2008; pp. 403–454. [Google Scholar]
- Stoop, R. Smart biomaterials for tissue engineering of cartilage injury. Int. J. Care Injured 2008, 39, 77–87. [Google Scholar]
- Li, W.J.; Laurencin, C.T.; Caterson, E.J.; Tuan, R.S.; Ko, F.K. Electrospun nanofibrous structure: a novel scaffold for tissue engineering. J. Biomed. Mater. Res. 2002, 60, 613–621. [Google Scholar] [CrossRef]
- Sechriest, V.; Miao, Y.; Niyibizi, C.; Westerhausen-Larson, A.; Matthew, H.; Evans, C.H.; Fu, F.H.; Suh, J.K. GAG-augmented polysaccharide hydrogel: A novel biocompatible and biodegradable material to support chondrogenesis. J. Biomed. Mater. Res. 2000, 49, 534–541. [Google Scholar] [CrossRef]
- Gibas, I.; Janik, H. Review: Synthetic polymer hydrogels for biomedical applications. Chem. Chem. Technol. 2010, 4, 297–304. [Google Scholar]
- Lin, Y.J.; Yen, C.N.; Hu, Y.C.; Wu, Y.C.; Liao, C.J.; Chu, I.M. Chondrocytes culture in three-dimensional porous alginate scaffolds enhanced cell proliferation, matrix synthesis and gene expression. J. Biomed. Mater. Res.Part A 2009, 88, 23–33. [Google Scholar]
- Perka, C.; Schultz, O.; Spitzer, R.; Lindenhayn, K. The influence of transforming growth factor beta1 on mesenchymal cell repair of full-thickness cartilage defects. J. Biomed. Mater. Res. 2000, 52, 543–552. [Google Scholar] [CrossRef]
- Mouw, J.K.; Case, N.D.; Guldberg, R.E.; Plaas, A.H.; Levenston, M.E. Variations in matrix composition and gag fine structure among scaffolds for cartilage tissue engineering. Osteoarth. Cart. 2005, 13, 828–836. [Google Scholar] [CrossRef]
- Rahfoth, B.; Weisser, J.; Sternkopf, F.; Aigner, T.; von der Mark, K.; Brauer, R. Transplantation of allograft chondrocytes embedded in agarose gel into cartilage defects of rabbits. Osteoarth. Cart. 1996, 6, 50–65. [Google Scholar]
- Reddy, N.; Yang, Y. Potential of plant proteins for medical applications. Trends Biotechnol. 2011, 29, 490–498. [Google Scholar] [CrossRef]
- Lee, K.Y.; Rowley, J.; Moy, E.; Bouhadir, K.H.; Mooney, D.J. Controlling mechanical and swelling properties of alginate hydrogels independently by cross-linker type and cross-linking density. Macromolecules 2000, 33, 4291–4294. [Google Scholar]
- Buschmann, M.D.; Gluzband, Y.A.; Grodzinsky, A.J.; Hunziker, E.B. Mechanical compression modulates matrix biosynthesis in chondrocyte/agarose culture. J. Cell Sci. 1995, 108, 1497–1508. [Google Scholar]
- Bryant, S.J.; Anseth, K.S. Hydrogel properties influence ECM production by chondrocytes PHotoencapsulated in poly (ethylene glycol) hydrogels. J. Biomed. Mater. Res. 2002, 59, 63–72. [Google Scholar] [CrossRef]
- Balakrishnan, B.; Banerjee, R. Biopolymer-based hydrogels for cartilage tissue engineering. Chem. Rev. 2011, 111, 4453–4474. [Google Scholar] [CrossRef]
- Moutos, F.T. Biomimetic Composite Scaffold for the Functional Tissue Engineering of Articular Cartilage. Ph.D. thesis, Duke University, Durham, NC, USA, 2009. [Google Scholar]
- Kemppainen, J.M.; Hollister, S.J. Tailoring the mechanical properties of 3D-designed poly(glycerol sebacate) scaffolds for cartilage applications. J. Biomed. Mater. Res. A 2010, 94, 9–18. [Google Scholar]
- Hutmacher, D.W. Scaffolds in tissue engineering bone and cartilage. Biomaterials 2000, 21, 2529–2543. [Google Scholar] [CrossRef]
- Yang, Z.; Wu, Y.; Li, C.; Zhang, T.; Zou, Y.; Hui, J.H.; Ge, Z.; Lee, E.H. Improved mesenchymal stem cells attachment and in vitro cartilage tissue formation on chitosan-modified poly(L-lactide-co-epsilon-caprolactone) scaffold. Tissue Eng. Part A. 2012, 18, 242–251. [Google Scholar]
- Ma, Z.; Gao, C.; Gong, Y.; Shen, J. Cartilage tissue engineering PLLA scaffold with surface immobilized collagen and basic fibroblast growth factor. Biomaterials 2005, 26, 1253–1259. [Google Scholar] [CrossRef]
- Bhati, R.S.; Mukherjee, D.P.; McCarthy, K.J.; Rogers, H.S.; Smith, D.F.; Shalaby, S.W. The growth of chondrocytes into a fibronectin-coated biodegradable scaffold. J. Biomed. Mater. Res. 2001, 56, 74–82. [Google Scholar] [CrossRef]
- Solchaga, L.A.; Gao, J.; Dennis, J.E.; Awadallah, A.; Lundberg, M.; Caplan, A.I.; Goldberg, V.M. Treatment of osteochondral defects with autologous bone marrow in a hyaluronan-based delivery vehicle. Tissue Eng. 2002, 8, 333–347. [Google Scholar] [CrossRef]
- Puppi, D.; Chiellini, F.; Piras, A.M.; Chiellini, E. Polymeric materials for bone and cartilage repair. Prog. Polym. Sci. 2010, 35, 403–440. [Google Scholar] [CrossRef]
- Yang, Q.; Peng, J.; Guo, Q.; Huang, J.; Zhang, L.; Yao, J.; Yang, F.; Wang, S.; Xu, W.; Wang, A.; Lu, S. A cartilage ECM-derived 3-D porous acellular matrix scaffold for in vivo cartilage tissue engineering with PKH26-labeled chondrogenic bone marrow-derived mesenchymal stem cells. Biomaterials 2008, 29, 2378–2387. [Google Scholar] [CrossRef]
- Yang, Z.; Shi, Y.; Wei, X.; He, J.; Yang, S.; Dickson, G.; Tang, J.; Xiang, J.; Song, C.; Li, G. Fabrication and repair of cartilage defects with a novel acellular cartilage matrix scaffold. Tissue Eng. Part C 2010, 16, 865–876. [Google Scholar] [CrossRef]
- Elder, B.D.; Eleswarapu, S.V.; Athanasiou, K.A. Extraction Techniques for the decellularization of tissue engineered articular cartilage constructs. Biomaterials 2009, 30, 3749–3756. [Google Scholar] [CrossRef]
- Malda, J.; Woodfield, T.B.F.; van der Vloodta, F.; Wilsond, C.; Martensc, D.E.; Tramperc, J.; van Blitterswijk, C.A.; Rieslea, J. The effect of PEGT/PBT scaffold architecture on the composition of tissue engineered cartilage. Biomaterials 2005, 26, 63–72. [Google Scholar] [CrossRef]
- Hwang, N.S.; Kim, M.S.; Sampattavanich, S.; Baek, J.H.; Zhang, Z.; Elisseeff, J. Effects of three-dimensional culture and growth factors on the chondrogenic differentiation of murine embryonic stem cells. Stem Cells 2006, 24, 284–291. [Google Scholar]
- Liu, H.; Lin, J.; Roy, K. Effect of 3D scaffold and dynamic culture condition on the global gene expression profile of mouse embryonic stem cells. Biomaterials 2006, 27, 5978–5989. [Google Scholar] [CrossRef]
- Putnam, A.J.; Mooney, D.J. Tissue Engineering using synthetic extracellular matrices. Nat. Med. 1996, 2, 824–826. [Google Scholar] [CrossRef]
- Woodfield, T.B.F.; van Blitterswijk, C.A.; de Wijn, J.; Sims, T.J.; Hollander, A.P.; Riesle, J. Polymer scaffold fabricated with pore-size gradient as a model for studying the zonal organization within tissue-engineered cartilage constructs. Tissue Eng. 2005, 11, 1297–1311. [Google Scholar] [CrossRef]
- Woodfield, T.B.F.; Bezemer, J.M.; Pieper, J.S.; van Blitterswijk, C.A.; Riesle, J. Scaffolds for tissue engineering of cartilage. Crit. Rev. Euk. Gene Exp. 2002, 12, 207–235. [Google Scholar]
- Zein, I.; Hutmacher, D.W.; Tan, K.C.; Teoh, S.H. Fused deposition modeling of novel scaffold architectures for tissue engineering applications. Biomaterials 2002, 23, 1169–1185. [Google Scholar] [CrossRef]
- Murphy, W.L.; Dennis, R.G.; Kileny, J.L.; Mooney, D.J. Salt fusion: An approach to improve pore interconnectivity within tissue engineering scaffolds. Tissue Eng. 2002, 8, 43–52. [Google Scholar] [CrossRef]
- Nehrer, S.; Breinan, H.A.; Ramappa, A.; Young, G.; Shortkroff, S.; Louie, L.K.; Sledge, C.B.; Yannas, I.V.; Spector, M. Matrix collagen type and pore size influence behaviour of seeded canine chondrocytes. Biomaterials 1997, 18, 769–776. [Google Scholar]
- LiVecchi, A.B.; Tombes, R.M.; LaBerge, M. In vitro chondrocyte collagen deposition within porous HDPE: Substrate microstructure and wettability effects. J. Biomed. Mater. Res. 1994, 28, 839–850. [Google Scholar]
- Bhardwaj, T.; Pilliar, R.M.; Grynpas, M.D.; Kandel, R.A. Effect of material geometry on cartilagenous tissue formation in vitro. J. Biomed. Mater. Res. 2001, 57, 190–199. [Google Scholar] [CrossRef]
- Silva, M.M.; Cyster, L.A.; Barry, J.J.; Yang, X.B.; Oreffo, R.O.; Grant, D.M.; Scotchford, C.A.; Howdle, S.M.; Shakesheff, K.M.; Rose, F.R. The effect of anisotropic architecture on cell and tissue infiltration into tissue engineering scaffolds. Biomaterials 2006, 27, 5909–5917. [Google Scholar] [CrossRef]
- El-Ayoubi, R.; Degrandpre, C.; Diraddo, R.; Yousef, A.M. design and dynamic culture of 3D-scaffolds for cartilage tissue engineering. J. Biomater. Appl. 2011, 25, 429–444. [Google Scholar] [CrossRef]
- Yamane, S.; Iwasaki, N.; Kasahara, Y.; Harada, K.; Majima, T.; Monde, K.; Nishimura, S.; Minami, A. effect of pore size on in vitro cartilage formation using chitosan-based hyaluronic acid hybrid polymer fibers. J. Biomed. Mater. Res. Part A 2007, 81A, 586–593. [Google Scholar]
- Lien, S.M.; Ko, L.Y.; Huang, T.J. Effect of pore size on ecm secretion and cell growth in gelatin scaffold for articular cartilage tissue engineering. Acta Biomater. 2009, 5, 670–679. [Google Scholar] [CrossRef]
- Grad, S.; Zhou, L.; Gogolewski, S.; Alini, M. Chondrocytes seeded onto poly (L/DL-Lactide) 80%/20% porous scaffolds: A biochemical evaluation. J. Biomed. Mater. Res. Part A 2003, 66, 571–579. [Google Scholar]
- Lefebvre, V.; Peeters-Joris, C.; Vaes, G. Production of collagens, collagenase and collagenase inhibitor during the dedifferentiation of articular chondrocytes by serial subcultures. Biochem. Biophys. Acta 1990, 1051, 266–275. [Google Scholar] [CrossRef]
- Rodriguez, A.M.; Vacanti, C.A. Tissue engineering of cartilage. In Frontiers in Tissue Engineering; Patrick, J.C.W., Mikos, A.G., McIntire, L.V., Eds.; Elsevier Scienc: New York, NY, USA, 1998; pp. 400–411. [Google Scholar]
- Li, W.J.; Jiang, Y.J.; Tuan, R.S. Chondrocyte phenotype in engineered fibrous matrix is regulated by fiber size. Tissue Eng. 2006, 12, 1775–1785. [Google Scholar]
- Spiteri, C.G.; Pilliar, R.M.; Kandel, R.A. Substrate porosity enhances chondrocyte attachment, spreading, and cartilage tissue formation in vitro. J. Biomed. Mater. Res. Part A 2006, 78, 677–683. [Google Scholar]
- Gerecht, S.; Townsend, S.A.; Pressler, H.; Zhu, H.; Nijst, C.L.; Bruggeman, J.P.; Nichol, J.W.; Langer, R. A porous photocurable elastomer for cell encapsulation and culture. Biomaterials 2007, 28, 4826–4835. [Google Scholar] [CrossRef]
- El-Ayoubi, R.; Eliopoulus, N.; Diraddo, R.; Galipeau, J.; Yousefi, A.M. Design and fabrication of 3D porous scaffolds to facilitate cell-based gene therapy. Tissue Eng. Part A 2008, 14, 1037–1048. [Google Scholar] [CrossRef]
- Moutos, F.T.; Estes, B.T.; Guilak, F. Multifunctional hybrid three-dimensionally woven scaffolds for cartilage tissue engineering. Macromol. Biosci. 2010, 10, 1355–1364. [Google Scholar] [CrossRef]
- Sahoo, S.; Cho-Hong, J.G.; Siew-Lok, T. Development of hybrid polymer scaffolds for potential applications in ligament and tendon tissue engineering. Biomed Mater. 2007, 2, 169–173. [Google Scholar]
- Cheng, Z.; Teoh, S.H. Surface modification of ultra thin poly (epsilon-caprolactone) films using acrylic acid and collagen. Biomaterials 2004, 25, 1991–2001. [Google Scholar] [CrossRef]
- Miot, S.; Woodfield, T.B.F.; Daniels, A.U.; Suetterlin, R.; Peterschmitt, I.; Heberer, M.; van Blitterswijk, C.A.; Riesle, J.; Martin, I. Effects of scaffold composition and architecture on human nasal chondrocyte redifferentiation and cartilaginous matrix deposition. Biomaterials 2005, 26, 2479–2489. [Google Scholar] [CrossRef]
- Freed, L.E.; Hollander, A.P.; Martin, I.; Barry, J.R.; Langer, R.; Vunjak-Novakovic, G. Chondrogenesis in a cell–polymer–bioreactor system. Exp. Cell Res. 1998, 240, 58–65. [Google Scholar] [CrossRef]
- Obradovic, B.; Meldon, J.H.; Freed, L.E.; Vunjak-Novakovic, G. Glycosaminoglycan deposition in engineered cartilage: Experiments and mathematical model. AIChE J 2000, 46, 1860–1871. [Google Scholar]
- Woodfield, T.B.F.; Malda, J.; de Wijn, J.; Peters, F.; Riesle, J.; van Blitterswijk, C.A. Design of porous scaffolds for cartilage tissue engineering using a three-dimensional fiber-deposition technique. Biomaterials 2004, 25, 4149–4161. [Google Scholar]
- Lin, A.S.; Barrows, T.H.; Cartmella, S.H.; Guldberg, R.E. Microarchitectural and mechanical characterization of oriented porous polymer scaffolds. Biomaterials 2003, 24, 481–489. [Google Scholar] [CrossRef]
- Slivka, M.A.; Leatherbury, N.C.; Kieswetter, K.; Niederauer, G.G. Porous, resorbable, fiber-reinforced scaffolds tailored for articular cartilage repair. Tissue Eng. 2001, 7, 767–780. [Google Scholar] [CrossRef]
- Fedorovich, N.E.; Schuurman, W.; Wijnberg, H.M.; Prins, H.J.; van Weeren, P.R.; Malda, J.; Alblas, J.; Dhert, W.J. Biofabrication of osteochondral tissue equivalents by printing topologically defined, cell-laden hydrogel scaffolds. Tissue Eng. Part C 2012, 18, 33–44. [Google Scholar]
- Guillotin, B.; Souquet, A.; Catros, S.; Duocastella, M.; Pippenger, B.; Bellance, S.; Bareille, R.; Rémy, M.; Bordenave, L.; Amédée, J.; et al. Laser assisted bioprinting of engineered tissue with high cell density and microscale organization. Biomaterials 2010, 31, 7250–7256. [Google Scholar]
- Cohen, D.L.; Malone, E.; Lipson, H.; Bonassar, L.J. Direct freeform fabrication of seeded hydrogels in arbitrary geometries. Tissue Eng. 2006, 12, 1325–1335. [Google Scholar] [CrossRef]
- Xu, T.; Jin, J.; Gregory, C.; Hickman, J.J.; Boland, T. Inkjet printing of viable mammalian cells. Biomaterials 2005, 26, 93–99. [Google Scholar] [CrossRef]
- Chung, C.; Mesa, J.; Randolph, M.A.; Yaremchuk, M.; Burdick, J.A. Influence of gel properties on neocartilage formation by auricular chondrocytes photoencapsulated in hyaluronic acid networks. J. Biomed. Mater. Res. A 2006, 77, 518–525. [Google Scholar]
- Erickson, I.E.; Huang, A.H.; Sengupta, S.; Kestle, S.; Burdick, J.A.; Mauck, R.L. Macromer density influences mesenchymal stem cell chondrogenesis and maturation in photocrosslinked hyaluronic acid hydrogels. Osteoarth. Cart. 2009, 17, 1639–1648. [Google Scholar]
- Bryant, S.J.; Anseth, K.S. Controlling the spatial distribution of ecm components in degradable PEG hydrogels for tissue engineering cartilage. J. Biomed. Mater. Res. 2003, 64A, 70–79. [Google Scholar] [CrossRef]
- Bryant, S.J.; Durand, K.L.; Anseth, K.S. Manipulations in hydrogel chemistry control photoencapsulated chondrocyte behavior and their extracellular matrix production. J. Biomed. Mater. Res. 2003, 67A, 1430–1436. [Google Scholar] [CrossRef]
- Sontjens, S.H.M.; Nettles, D.L.; Carnahan, M.A.; Setton, L.A.; Grinstaff, M.W. Biodendrimer-based hydrogel scaffolds for cartilage tissue repair. Biomacromolecules 2006, 7, 310–316. [Google Scholar] [CrossRef]
- Nicodemus, G.D.; Bryant, S.J. Cell encapsulation in biodegradable hydrogels for tissue engineering applications. Tissue Eng. Part B Rev. 2008, 14, 149–165. [Google Scholar] [CrossRef]
- Jeong, C.G.; Hollister, S.J. A comparison of the influence of material on in vitro cartilage tissue engineering with PCL, PGS, and POC 3D scaffold architecture seeded with chondrocytes. Biomaterials 2010, 31, 4304–4312. [Google Scholar] [CrossRef]
- Annabi, N.; Nichol, J.W.; Zhong, X.; Ji, C.; Koshy, S.; Khademhosseini, A.; Dehghani, F. Controlling the porosity and microarchitecture of hydrogels for tissue engineering. Tissue Eng. Part B 2010, 16, 371–383. [Google Scholar] [CrossRef]
- Mohan, N.; Nair, P.D. Polyvinyl alcohol-poly (caprolactone) semi IPN scaffold with implication for cartilage tissue engineering. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 84, 584–594. [Google Scholar]
- Park, J.S.; Woo, D.G.; Sun, B.K.; Chung, H.-M.; Im, S.J.; Choi, Y.M.; Park, K.; Huh, K.M.; Park, K.-H. In vitro and in vivo test of PEG/PCL-based hydrogel scaffold for cell delivery application. J. Control Release 2007, 124, 51–59. [Google Scholar] [CrossRef]
- Suh, S.W.; Shin, J.Y.; Kim, J.; Kim, J.; Beak, C.H.; Kim, D.I.; Kim, H.; Jeon, S.S.; Choo, I.W. Effect of different particles on cell proliferation in polymer scaffolds using a solvent-casting and particulate leaching technique. ASAIO J. 2002, 48, 460–464. [Google Scholar] [CrossRef]
- Kemppainen, J.M.; Hollister, S.J. Differential effects of designed scaffold permeability on chondrogenesis by chondrocytes and bone marrow stromal cells. Biomaterials 2010, 31, 279–287. [Google Scholar] [CrossRef]
- Heydarkhan-Hagvall, S.; Schenke-Layland, K.; Dhanasopon, A.P.; Rofail, F.; Smith, H.; Wu, B.M.; Shemin, R.; Beygui, R.E.; Maclellan, W.R. Three-dimensional electronspun ECM-based hybrid scaffolds for cardiovascular tissue engineering. Biomaterials 2008, 29, 2907–2914. [Google Scholar] [CrossRef]
- Pham, Q.P.; Sharma, U.; Mikos, A.G. Electrospun poly (e-caprolactone) microfiber and multilayer nanofiber- microfiber scaffolds: Characterization of scaffolds and measurement of cellular infiltration. Biomacromolecules 2006, 7, 2796–2805. [Google Scholar]
- Matthews, J.A.; Boland, E.D.; Wnek, G.E.; Simpson, D.G.; Bowlin, G.L. Electrospinning of collagen type II: A feasibility study. J. Bioact. Compat. Pol. 2003, 18, 125–134. [Google Scholar] [CrossRef]
- Komistek, R.D.; Kane, T.R.; Mahfouz, M.; Ochoa, J.A.; Dennis, D.A. Knee mechanics: A review of past and present techniques to determine in vivo loads. J. Biomech. 2005, 38, 215–228. [Google Scholar] [CrossRef]
- Natoli, R.M.; Athanasiou, K.A. P188 reduces cell death and IGF-I reduces GAG release following single-impact loading of articular cartilage. J. Biomech. Eng. 2008, 130. [Google Scholar] [CrossRef]
- Treppo, S.; Koepp, H.; Quan, E.C.; Cole, A.A.; Kuettner, K.E.; Grodzinsky, A.J. Comparison of biomechanical and biochemical properties of cartilage from human knee and ankle pairs. J. Orthop. Res. 2000, 18, 739–748. [Google Scholar] [CrossRef]
- Tanaka, Y.; Yamaoka, H.; Nishizawa, S.; Nagata, S.; Ogasawara, T.; Asawa, Y.; Fujihara, Y.; Takato, T.; Hoshi, K. The optimization of porous polymeric scaffolds for chondrocyte/atelocollagen based tissue-engineered cartilage. Biomaterials 2010, 31, 4506–4516. [Google Scholar] [CrossRef]
- Xie, J.; Ihara, M.; Jung, Y.; Kwonk, K.; Kim, S.H.; Kim, Y.H.; Mastuda, T. Mechano-active scaffold design based on microporous poly(L-lactide-co-ε-caprolactone) for articular cartilage tissue engineering: Dependence of porosity on compression force-applied mechanical behaviors. Tissue Eng. 2006, 12, 449–458. [Google Scholar] [CrossRef]
- Moroni, L.; de Wijn, J.R.; van Blitterswijk, C.A. 3D fiber-deposited scaffolds for tissue engineering: Influence of pores geometry and architecture on dynamic mechanical properties. Biomaterials 2006, 27, 974–985. [Google Scholar] [CrossRef]
- Jeong, C.G.; Hollister, S.J. Mechanical and biochemical assessments of three-dimensional poly(1,8-Octanediol-co-Citrate) scaffold pore shape and permeability effects on in vitro chondrogenesis using primary chondrocytes. Tissue Eng. Part A. 2010, 16, 3759–3768. [Google Scholar] [CrossRef]
- Chen, G.; Sato, T.; Ushida, T.; Hirochika, R.; Shirasaki, Y.; Ochiai, N.; Tateishi, T. The use of a novel PLGA fiber/collagen composite web as a scaffold for engineering of articular cartilage tissue with adjustable thickness. J. Biomed. Mater. Res. A 2003, 67, 1170–1180. [Google Scholar]
- Waldman, S.D.; Grynpas, M.D.; Pilliar, R.M.; Kandel, R.A. The use of specific chondrocyte populations to modulate the properties of tissue-engineered cartilage. J. Orthop. Res. 2003, 21, 132–138. [Google Scholar] [CrossRef]
- Liao, E.; Yaszemski, M.; Krebsbach, P.; Hollister, S. Tissue-engineered cartilage constructs using composite hyaluronic acid/collagen I hydrogels and designed poly(propylene fumarate) scaffolds. Tissue Eng. 2007, 13, 537–550. [Google Scholar] [CrossRef]
- Liao, E.E. Enhancement of Chondrogenesis by Directing Cellular Condensation through Chondroinductive Microenvironments and Designed Solid Freeform Fabricated Scaffolds. Ph.D. Thesis, University of Michigan, Ann Arbor, MI, USA, 2007. [Google Scholar]
- Chung, T.W.; Yang, J.; Akaike, T.; Cho, K.Y.; Nah, J.W.; Kim, S.I.; Cho, C.S. Preparation of alginate/galactosylated chitosan scaffold for hepatocyte attachment. Biomaterials 2002, 23, 2827–2834. [Google Scholar]
- Chuang, W.Y.; Young, T.H.; Yao, C.H.; Chiu, W.Y. Properties of the poly (vinyl alcohol)/chitosan blend and its effect on the culture of fibroblast in vitro. Biomaterials 1999, 20, 1479–1487. [Google Scholar] [CrossRef]
- Zhang, M.; Li, X.H.; Gong, Y.D.; Zhao, N.M.; Zhang, X.F. Properties and biocompatibility of chitosan films modified by blending with PEG. Biomaterials 2002, 23, 2641–2648. [Google Scholar]
- Bryant, S.J.; Davis-Arehart, K.A.; Luo, N.; Shoemaker, R.K.; Arthur, J.A.; Anseth, K.S. Synthesis and characterization of photopolymerized multifunctional hydrogels: Water soluble poly (vinyl alcohol) and chondroitin sulfate macromers for chondrocyte encapsulation. Macromolecules 2004, 37, 6726–6733. [Google Scholar]
- Kuo, Y.C.; Lin, C.Y. Effect of Genipin-crosslinked chitin-chitosan scaffolds with hydroxyapatite modifications on the cultivation of bovine knee chrondrocytes. Biotechnol. Bioeng. 2006, 95, 132–137. [Google Scholar] [CrossRef]
- Bryant, S.J.; Bender, R.J.; Durand, K.L.; Anseth, K.S. Encapsulating chondrocytes in degrading PEG hydrogels with high modulus: Engineering gel structural changes to facilitate cartilaginous tissue production. Biotechnol. Bioeng. 2004, 86, 747–755. [Google Scholar] [CrossRef]
- Fedorovich, N.E.; Alblas, J.; de Wijn, J.R.; Hennink, W.E.; Verbout, A.J.; Dhert, W.J.A. Hydrogels as extracellular matrices for skeletal tissue engineering: state-of-the-art and novel application in organ printing. Tissue Eng. 2007, 13, 1905–1925. [Google Scholar] [CrossRef]
- Chen, C.S.; Ingber, D.E. Tensegrity and mechanoregulation: From skeleton to cytoskeleton. Osteoarth. Cart. 1999, 7, 81–94. [Google Scholar] [CrossRef]
- Martin, I.; Obradovic, B.; Treppo, S.; Grodzinsky, A.J.; Langer, R.; Freed, L.E.; Vunjak-Novakovic, G. Modulation of the mechanical properties of tissue engineered cartilage. Biorheology 2000, 37, 141–147. [Google Scholar]
- Gratz, K.R.; Wong, V.W.; Chen, A.C.; Fortier, L.A.; Nixon, A.J.; Sah, R.L. Biomechanical assessment of tissue retrieved after in vivo cartilage defect repair: Tensile modulus of repair tissue and integration with host cartilage. J. Biomech. 2006, 39, 138–146. [Google Scholar]
- Natoli, R.M.; Responte, D.J.; Lu, B.Y.; Athanasiou, K.A. Effects of multiple chondroitinase ABC applications on tissue engineered articular cartilage. J. Orthop. Res. 2009, 27, 949–956. [Google Scholar] [CrossRef]
- Natoli, R.M.; Revell, C.M.; Athanasiou, K.A. Chondroitinase ABC treatment results in greater tensile properties of self-assembled tissue-engineered articular cartilage. Tissue Eng. Part A 2009, 15, 3119–3128. [Google Scholar] [CrossRef]
- Hoemann, C.D.; Sun, J.; Legare, A.; McKee, M.D.; Buschmann, M.D. Tissue engineering of cartilage using an injectable and adhesive chitosan-based cell-delivery vehicle. Osteoarth. Cart. 2005, 13, 318–329. [Google Scholar] [CrossRef]
- Bawolin, N.K.; Li, M.G.; Chen, X.B.; Zhang, W.J. Modeling material-degradation-induced elastic property of tissue engineering scaffolds. J. Biomech. Eng. 2010, 132. [Google Scholar] [CrossRef]
- Liebschner, M.; Bucklen, B.; Wettergreen, M. Mechanical aspects of tissue engineering. Semin. Plast. Surg. 2005, 19, 217–228. [Google Scholar] [CrossRef]
- Little, C.J.; Bawolin, N.K.; Chen, X. Mechanical properties of natural cartilage and tissue-engineered constructs. Tissue Eng. Part B Rev. 2011, 17, 213–227. [Google Scholar]
- Akizuki, S.; Mow, V.C.; Müller, F.J.; Pita, J.C.; Howell, D.S.; Manicour, D.H. Tensile properties of human knee joint cartilage: I. Influence of ionic conditions, weight bearing, and fibrillation on the tensile modulus. J. Orthop. Res. 1986, 4, 379–392. [Google Scholar]
- Setton, L.A.; Mow, V.C.; Müller, F.J.; Pita, J.C.; Howell, D.S. Mechanical properties of canine articular cartilage are significantly altered following transection of the anterior cruciate ligament. J. Orthop. Res. 1994, 12, 451–463. [Google Scholar] [CrossRef]
- Elliott, D.M.; Guilak, F.; Vail, T.P.; Wang, J.Y.; Setton, L.A. Tensile properties of articular cartilage are altered by meniscectomy in a canine model of osteoarthritis. J. Orthop. Res. 1999, 17, 503–508. [Google Scholar]
- Sakkers, R.J.B.; de Wijn, J.R.; Dalmeyer, R.A.J.; Brand, R.; van Blitterswijk, C.A. Evaluation of copolymers of polyethylene oxide and poly buthylene terephthalate (polyactives): Mechanical behaviour. J. Mater. Sci. 1998, 9, 375–379. [Google Scholar] [CrossRef]
- Temenoff, J.S.; Athanasiou, K.A.; Lebaron, R.G.; Mikos, A.G. Effect of poly (ethylene glycol) molecular weight on tensile and swelling properties of oligo (poly (ethylene glycol) fumarate) hydrogels for cartilage tissue engineering. J. Biomed. Mater. Res. A 2002, 59, 429–437. [Google Scholar] [CrossRef]
- Kempson, G.E.; Muir, H.; Pollard, C.; Tuke, M. The tensile properties of the cartilage of human femoral condyles related to the content of collagen and glycosaminoglycans. Biochim. Biophys. Acta 1973, 297, 456–472. [Google Scholar] [CrossRef]
- Bader, D.L.; Kempson, G.E.; Barrett, A.J.; Webb, W. The effects of leucocyte elastase on the mechanical properties of adult human articular cartilage in tension. Biochim. Biophys. Acta. 1981, 677, 103–108. [Google Scholar] [CrossRef]
- Mow, V.C.; Guo, X. Mechano-electrochemical properties of articular cartilage: Their inhomogeneities and anisotropies. Annu. Rev. Biomed. Eng. 2002, 4, 175–209. [Google Scholar] [CrossRef]
- Mow, V.C.; Gibbs, M.C.; Lai, W.M.; Zhu, W.B.; Athanasiou, K.A. Biphasic indentation of articular cartilage—II. A numerical algorithm and an experimental Study. J. Biomech. 1989, 22, 853–861. [Google Scholar] [CrossRef]
- Jurvelin, J.S.; Buschmann, M.D.; Hunziker, E.B. Optical and mechanical determination of poisson’s ratio of adult bovine humeral articular cartilage. J. Biomech. 1997, 30, 235–241. [Google Scholar]
- Zhu, W.; Mow, V.C.; Koob, T.J.; Eyre, D.R. Viscoelastic shear properties of articular cartilage and the effects of glycosidase treatments. J. Orthop. Res. 1993, 11, 771–781. [Google Scholar] [CrossRef]
- LeRoux, M.A.; Guilak, F.; Setton, L.A. Compressive and shear properties of alginate gel: Effects of sodium ions and alginate concentration. J. Biomed. Mater. Res. 1999, 47, 46–53. [Google Scholar] [CrossRef]
- Babensee, J.E.; Anderson, J.M.; McIntire, L.V.; Mikos, A.G. Host response to tissue engineered devices. Adv. Drug Deliver. Rev. 1998, 33, 111–139. [Google Scholar] [CrossRef]
- Martins, A.M,; Pham, Q.P.; Malafaya, P.B.; Raphael, R.M.; Kasper, F.K.; Reis, R.L.; Mikos, A.G. Natural stimulus responsive scaffolds/cells for bone tissue engineering: Influence of lysozyme upon scaffold degradation and osteogenic differentiation of cultured marrow stromal cells induced by CaP coatings. Tissue Eng. Part A. 2009, 15, 1953–1963. [Google Scholar]
- Jeong, C.G.; Hollister, S.J. Mechanical, permeability, and degradation properties of 3D designed poly (1,8 octanediol-co-citrate) scaffolds for soft tissue engineering. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 93, 141–149. [Google Scholar]
- Zhang, H.; Neau, S.H. In vitro degradation of chitosan by a commercial enzyme preparation: effect of molecular weight and degree of deacetylation. Biomaterials 2001, 22, 1653–1658. [Google Scholar] [CrossRef]
- Salinas, C.N.; Anseth, K.S. The influence of the RGD peptide motif and its contextual presentation in PEG gels on human mesenchymal stem cell viability. J. Tissue Eng. Regen. Med. 2008, 2, 296–304. [Google Scholar] [CrossRef]
- Sahoo, S.; Chung, C.; Khetan, S.; Burdick, J.A. Hydrolytically degradable hyaluronic acid hydrogels with controlled temporal structures. Biomacromolecules 2008, 9, 1088–1092. [Google Scholar] [CrossRef]
- Chung, C.; Beecham, M.; Mauck, R.L.; Burdick, J.A. The influence of degradation characteristics of hyaluronic acid hydrogels on in vitro neocartilage formation by mesenchymal stem cells. Biomaterials 2009, 30, 4287–4296. [Google Scholar] [CrossRef]
- Middleton, J.C.; Tipton, A.J. Synthetic biodegradable polymers as orthopedic devices. Biomaterials 2000, 21, 2335–2346. [Google Scholar] [CrossRef]
- Wu, L.B.; Ding, J.D. In vitro degradation of three-dimensional porous poly (D,L-lactide-co-glycolide) scaffolds for tissue engineering. Biomaterials 2004, 25, 5821–5830. [Google Scholar] [CrossRef]
- Kofron, M.D.; Griswold, A.; Kumbar, S.G.; Martin, K.; Wen, X.; Laurencin, C.T. The implications of polymer selection in regenerative medicine: A comparison of amorphous and semi-crystalline polymer for tissue regeneration. Adv. Funct. Mater. 2009, 19, 1351–1359. [Google Scholar]
- Pan, Z.; Ding, J. Engineering and regenerative medicine poly (lactide-co-glycolide) porous scaffolds for tissue. Interface Focus 2012, 2, 366–377. [Google Scholar] [CrossRef]
- Yang, Y.; Zhao, Y.; Tang, G.; Li, H.; Yuan, X.; Fan, Y. In vitro degradation of porous poly (L-lactide-co-glycolide)/b-tricalcium phosphate (PLGA/b-TCP) scaffolds under dynamic and static conditions. Polym. Degrad. Stabil. 2008, 93, 1838–1845. [Google Scholar] [CrossRef]
- Yoshioka, T.; Kawazoe, N.; Tateishi, T.; Chen, G. In vitro evaluation of biodegradation of poly (lactic-coglycolic acid) sponges. Biomaterials 2008, 29, 3438–3443. [Google Scholar]
- Odelius, K.; Hoglund, A.; Kumar, S.; Hakkarainen, M.; Ghosh, A.K.; Bhatnagar, N.; Albertsson, A.-C. Porosity and pore size regulate the degradation product profile of polylactide. Biomacromolecules 2011, 12, 1250–1258. [Google Scholar] [CrossRef]
- Wu, L.B.; Ding, J.D. Effects of porosity and pore size on in vitro degradation of three-dimensional porous poly (D,L-lactide-co-glycolide) scaffolds for tissue engineering. J. Biomed. Mater. Res. Part A 2005, 75, 767–777. [Google Scholar]
- Sawhney, A.S.; Pathak, C.P.; Hubbell, J.A. Bioerodible hydrogels based on photopolymerized poly (ethylene glycol)-co-poly(alpha-hydroxy acid) diacrylate macromers. Macromolecules 1993, 26, 581–587. [Google Scholar] [CrossRef]
- Wang, W.; Li, B.; Li, Y.; Jiang, Y.; Ouyang, H.; Gao, C. In vivo restoration of full-thickness cartilage defects by poly (lactide-co-glycolide) sponges filled with fibrin gel, bone marrow mesenchymal stem cells and dna complexes. Biomaterials 2010, 31, 5953–5965. [Google Scholar] [CrossRef]
- Yu, L.; Zhang, Z.; Zhang, H.; Ding, J. Biodegradability and biocompatibility of thermoreversible hydrogels formed from mixing a sol and a precipitate of block copolymers in water. Biomacromolecules 2010, 11, 2169–2178. [Google Scholar] [CrossRef]
- Zhang, Z.; Ni, J.; Chen, L.; Yu, L.; Xu, J.; Ding, J. Biodegradable and thermoreversible PCLA-PEG-PCLA hydrogel as a barrier for prevention of post-operative adhesion. Biomaterials 2011, 32, 4725–4736. [Google Scholar] [CrossRef]
- Edwards, S.L.; Mitchell, W.; Matthews, J.B.; Ingham, E.; Russell, S.J. Design of nonwoven scaffolds structures for tissue engineering of the anterior cruciate ligament. AUTEX Res. J. 2004, 4, 86–94. [Google Scholar]
- Lu, L.; Mikos, A. The importance of new processing techniques in tissue engineering. MRS Bull. 1996, 21, 28–32. [Google Scholar]
- Whang, K.; Thomas, C.H.; Healy, K.E.; Nuber, G. A novel method to fabricate bioabsorbable scaffolds. Polymers 1995, 36, 837–842. [Google Scholar] [CrossRef]
- Whang, K.; Tsai, D.C.; Nam, E.K.; Aitken, M.; Sprague, S.M.; Patel, P.K.; Healy, K.E. Ectopic bone formation via rhBMP-2 Delivery from porous bioresorbable polymer scaffolds. J. Biomed. Mater. Res. 1998, 42, 491–499. [Google Scholar] [CrossRef]
- Sachlos, E.; Czernuszka, J.T. Making tissue engineering scaffolds work. Review: The application of solid freeform fabrication technology to the production of tissue engineering scaffolds. Eur. Cell. Mater. 2003, 5, 29–39. [Google Scholar]
- Kim, J.; Reneker, D.H. Mechanical properties of composites using ultrafine electrospun fibers. Polym. Comp. 1999, 20, 124–131. [Google Scholar] [CrossRef]
- Sittinger, M.; Bujia, J.; Rotter, N.; Reitzel, D.; Minuth, W.W.; Burmester, G.R. Tissue engineering and autologous transplant formation: practical approaches with resorbable biomaterials and new cell culture techniques. Biomaterials 1996, 17, 237–242. [Google Scholar]
- Soliman, S.; Sant, S.; Nichol, J.W.; Khabiry, M.; Traversa, E.; Khademhosseini, A. Controlling the porosity of fibrous scaffolds by modulating the fiber diameter and packing density. J. Biomed. Mater. Res. A 2011, 96, 566–574. [Google Scholar]
- Nerurkar, N.L.; Sen, S.; Baker, B.M.; Elliott, D.M.; Mauck, R.L. Dynamic culture enhances stem cell infiltration and modulates extracellular matrix production on aligned electrospun nanofibrous scaffolds. Acta Biomate. 2011, 7, 485–491. [Google Scholar] [CrossRef]
- Li, W.J.; Mauck, R.L.; Cooper, J.A.; Yuan, X.; Tuan, R.S. Engineering controllable anisotropy in electrospun biodegradable nanofibrous scaffolds for musculoskeletal tissue engineering. J. Biomech. 2007, 40, 1686–1693. [Google Scholar]
- Dalton, P.D.; Joergensen, N.T.; Groll, J.; Moeller, M. Patterned melt electrospun substrates for tissue engineering. Biomed. Mater. 2008, 3. [Google Scholar] [CrossRef]
- Dalton, P.D.; Klinkhammer, K.; Salber, J.; Klee, D.; Möller, M. Direct in vitro electrospinning with polymer melts. Biomacromolecules 2006, 7, 686–690. [Google Scholar] [CrossRef]
- Moroni, L.; Hendriks, J.A.A.; Schotel, R.; de Wijn, J.R.; van Blitterswijk, C.A. Design of biphasic polymeric 3-Dimensional fiber deposited scaffolds for cartilage tissue engineering applications. Tissue Eng. 2007, 13, 361–371. [Google Scholar] [CrossRef]
- Shao, X.; Goh, J.C.H.; Hutmacher, D.W.; Lee, E.H.; Zigang, G. Repair of large articular osteochondral defects using hybrid scaffolds and bone marrow-derived mesenchymal stem cells in a rabbit model. Tissue Eng. 2006, 12, 1539–1551. [Google Scholar] [CrossRef]
- Vozzi, G.; Flaim, C.; Ahluwalia, A.; Bhatia, S. Fabrication of PLGA scaffolds using soft lithography and microsyringe deposition. Biomaterials 2003, 24, 2533–2540. [Google Scholar]
- Wiria, F.E.; Chua, C.K.; Leong, K.F.; Quah, Z.Y.; Chandrasekaran, M.; Lee, M.W. Improved biocomposite development of poly(vinyl alcohol) and hydroxyapatite for tissue engineering scaffold fabrication using selective laser sintering. J. Mater. Sci. Mater. Med. 2008, 19, 989–996. [Google Scholar] [CrossRef]
- Ramanath, H.S.; Chandrasekaran, M.; Chua, C.K.; Leong, K.F.; Shah, K.D. Melt flow behaviour of poly-ε-caprolactone in fused deposition modeling. J. Mater. Sci. Mater. Med. 2008, 19, 2541–2550. [Google Scholar] [CrossRef]
- Sudarmadji, N.; Tan, J.Y.; Leong, K.F.; Chua, C.K.; Loh, Y.T. Investigation of the mechanical properties and porosity relationships in selective laser-sintered polyhedral for functionally graded scaffolds. Acta Biomater. 2011, 7, 530–537. [Google Scholar]
- Landers, R.; Mulhaupt, R. Desktop manufacturing of complex objects, prototypes and biomedical scaffolds by means of computer-assisted design combined with computer-guided 3d plotting of polymers and reactive oligomers. Macromolec. Mater. Eng. 2000, 282, 17–21. [Google Scholar] [CrossRef]
- Sobral, J.M.; Caridade, S.G.; Sousa, R.A.; Mano, J.F.; Reis, R.L. Three-dimensional plotted scaffolds with controlled pore size gradients: Effect of scaffold geometry on mechanical performance and cell seeding efficiency. Acta Biomater. 2011, 7, 1009–1018. [Google Scholar] [CrossRef] [Green Version]
- Maher, P.S.; Keatch, R.P.; Donnelly, K. Characterisation of rapid prototyping techniques for studies in cell behaviour. Rapid Prototyp. J. 2010, 16, 116–123. [Google Scholar] [CrossRef]
- Melchels, F.P.W.; Barradas, A.M.C.; van Blitterswijk, C.A.; de Boer, J.; Feijen, J.; Grijpma, D.W. Effects of the architecture of tissue engineering scaffolds on cell seeding and culturing. Acta Biomater. 2010, 6, 4208–4217. [Google Scholar] [CrossRef] [Green Version]
- Chua, C.K.; Liu, M.J.J.; Chou, S.M. Additive manufacturing-assisted scaffold-based tissue engineering. In Innovative Developments in Virtual and Physical Prototyping, Proceedings of the 5th International Conference on Advanced Research in Virtual and Rapid Prototyping, Leiria, Portugal, 28 September–1 October 2011; Bartolo, P.J., Ed.; CRC Press: London, UK, 2011. [Google Scholar]
- Saunders, R.E.; Gough, J.E.; Derby, B. Delivery of human fibroblast cells by piezoelectric drop-on-demand inkjet printing. Biomaterials 2008, 292, 193–203. [Google Scholar]
- Miller, E.D.; Li, K.; Kanade, T.; Weiss, L.E.; Walker, L.M.; Campbell, P.G. Spatially directed guidance of stem cell population migration by immobilized patterns of growth factors. Biomaterials 2011, 32, 2775–2785. [Google Scholar]
- Duan, B.; Wang, M.; Zhou, W.Y.; Cheung, W.L.; Li, Z.Y.; Lu, W.W. Three-dimensional nanocomposite scaffolds fabricated via selective laser sintering for bone tissue engineering. Acta Biomater. 2010, 6, 4495–4505. [Google Scholar] [CrossRef]
- Li, X.; Li, D.; Lu, B.; Wang, C. Fabrication of bioceramic scaffolds with pre-designed internal architecture by gel casting and indirect stereolithography techniques. J. Porous Mater. 2008, 15, 667–671. [Google Scholar] [CrossRef]
- Taboas, J.M.; Maddox, R.D.; Krebsbach, P.H.; Hollister, S.J. Indirect solid free form fabrication of local and global porous, biomimetic and composite 3D polymer-ceramic scaffolds. Biomaterials 2003, 24, 181–194. [Google Scholar] [CrossRef]
- Vozzi, G. Microsyringe-based deposition of two-dimensional and three-dimensional polymer scaffolds with a well-defined geometry for application to tissue engineering. Tissue Eng. 2002, 8, 1089–1098. [Google Scholar] [CrossRef]
- Landers, R.; Pfister, A.; Hubner, U.; John, H.; Schmelzeisen, R.; Mulhaupt, R. Fabrication of soft tissue engineering scaffolds by means of rapid prototyping techniques. J. Mater. Sci. 2002, 37, 3107–3116. [Google Scholar] [CrossRef]
- Schuurman, W.; Khristov, V.; Pot, M.W.; van Weeren, P.R.; Dhert, W.J.A.; Malda, J. Bioprinting of hybrid tissue constructs with tailorable mechanical properties. Biofabrication 2011, 3, 021001. [Google Scholar] [CrossRef]
- Shim, J.H.; Kim, J.Y.; Park, M.; Park, J.; Cho, D.W. Development of a hybrid scaffold with synthetic biomaterials and hydrogel using solid freeform fabrication technology. Biofabrication 2011, 3, 034102. [Google Scholar] [CrossRef]
- Martin, I.; Wendt, D.; Heberer, M. The role of bioreactors in tissue engineering. Trends Biotechnol. 2004, 22, 80–86. [Google Scholar] [CrossRef]
- Wendt, D.; Marsano, A.; Jakob, M.; Heberer, M.; Martin, I. Oscillating perfusion of cell suspensions through three-dimensional scaffolds enhances cell seeding efficiency and uniformity. Biotechnol. Bioeng. 2003, 84, 205–214. [Google Scholar] [CrossRef]
- Davisson, T.; Sah, R.L.; Ratcliffe, A. Perfusion increases cell content and matrix synthesis in chondrocyte three-dimensional cultures. Tissue Eng. 2002, 8, 807–816. [Google Scholar] [CrossRef]
- Vlasea, M.; Shanjani, Y.; Basalah, A.; Toyserkani, E. Additive manufacturing of scaffolds for tissue engineering of bone and cartilage: Review. IJAMS 2011, 13, 123–141. [Google Scholar]
- Melchels, F.P.W.; Domingos, M.A.N.; Klein, T.J.; Malda, J.; Bartolo, P.J.; Hutmacher, D.W. Additive manufacturing of tissues and organs. Prog. Polym. Sci. 2012, 37, 1079–1104. [Google Scholar] [CrossRef] [Green Version]
- Sittinger, M.; Reitzel, D.; Dauner, M.; Hierlemann, H.; Hammer, C.; Kastenbauer, E.; Planck, H.; Burmester, G.R.; Bujia, J. Resorbable polyesters in cartilage engineering: Affinity and biocompatibility of polymer fiber structures to chondrocytes. J. Biomed. Mater. Res. Appl. Biomater. 1996, 33, 57–63. [Google Scholar] [CrossRef]
- Stankus, J.J.; Guan, J.; Fujimoto, K.; Wagner, W.R. Microintegrating smooth muscle cells into a biodegradable, elastomeric fiber matrix. Biomaterials 2006, 27, 735–744. [Google Scholar] [CrossRef]
- Baker, B.M.; Gee, A.O.; Metter, R.B.; Nathan, A.S.; Marklein, R.A.; Burdick, J.A. The potential to improve cell infiltration in composite fiber-aligned electrospun scaffolds by the selective removal of sacrificial fibers. Biomaterials 2008, 29, 2348–2358. [Google Scholar] [CrossRef]
- Nam, J.; Huang, Y.; Agarwal, S.; Lannutti, J. Improved cellular infiltration in electrospun fiber via engineered porosity. Tissue Eng. 2007, 13, 2249–2257. [Google Scholar] [CrossRef]
- Baker, B.M.; Mauck, R.L. The effect of nanofiber alignment on the maturation of engineered meniscus constructs. Biomaterials 2007, 28, 1967–1977. [Google Scholar] [CrossRef]
- Baker, B.M.; Nathan, A.S.; Huffman, G.R.; Mauck, R.L. Tissue engineering with meniscus cells derived from surgical debris. Osteoarth. Cart. 2009, 17, 336–345. [Google Scholar] [CrossRef]
- Li, W.J.; Jiang, Y.J.; Tuan, R.S. Cell-nanofiber-based cartilage tissue engineering using improved cell seeding, growth factor, and bioreactor technologies. Tissue Eng. Part A 2008, 14, 639–648. [Google Scholar] [CrossRef]
- Yousefi, A.M.; Gauvin, C.; Sun, L.; DiRaddo, R.W.; Fernandes, J. Design and fabrication of 3D-plotted polymeric scaffolds in functional tissue engineering. Polym. Eng. Sci. 2007, 47, 608–618. [Google Scholar] [CrossRef]
- Envision TEC BioPlotter V4. Altair Consulting Website. Available online: http://www.altair-consulting.com/envisiontec_bioplotter_v4.htm (accessed on May 2011).
- Caterson, E.J.; Nesti, L.J.; Li, W.J.; Danielson, K.G.; Albert, T.J.; Vaccaro, A.R.; Tuan, R.S. Three-dimensional cartilage formation by bone marrow-derived cells seeded ion polylactide/alginate amalgam. J. Biomed. Mater. Res. 2001, 57, 394–403. [Google Scholar] [CrossRef]
- Ameer, G.A.; Mahmood, T.A.; Langer, R. A biodegradable composite scaffold for cell transplantation. J. Orthop. Res. 2002, 20, 16–19. [Google Scholar] [CrossRef]
- Marijnissen, W.J.; van Osch, G.J.; Aigner, J.; Verwoerd-Verhoef, H.L.; Verhaar, J.A. Tissue-engineered cartilage using serially passaged articular chondrocytes. Chondrocytes in alginate, combined in vivo with a synthetic (E210) or biologic biodegradable carrier (DBM). Biomaterials 2000, 21, 571–580. [Google Scholar]
- Dai, W.; Kawazoe, N.; Lin, X.; Dong, J.; Chen, G. The influence of structural design of PLGA/collagen hybrid scaffolds in cartilage tissue engineering. Biomaterials 2010, 31, 2141–2152. [Google Scholar]
- Shahin, K. In Vitro Production of Human Hyaline Cartilage using Tissue Engineering. Ph.D. Thesis, University of New South Wales, Sydney, Australia, 2008. [Google Scholar]
- Wayne, J.S.; McDowell, C.L.; Shields, K.J.; Tuan, R.S. In vivo response of polylactic acid-alginate scaffolds and bone marrow-derived cells for cartilage tissue engineering. Tissue Eng. 2005, 11, 953–963. [Google Scholar] [CrossRef]
- Sang, Y.H.; Lee, E.A.; Yoon, J.J.; Park, T.G. Hyaluronic acid modified biodegradable scaffolds for cartilage tissue engineering. Biomaterials 2005, 26, 1925–1933. [Google Scholar] [CrossRef]
- Wang, W.; Li, B.; Yang, J.; Xin, L.; Li, Y.; Yin, H.; Qi, Y.; Jiang, Y.; Ouyang, H.; Gao, C. The restoration of full-thickness cartilage defects with bmscs and tgf-beta 1 loaded PLGA/Fibrin gel constructs. Biomaterials 2010, 31, 8964–8973. [Google Scholar] [CrossRef]
- Schek, R.M.; Taboas, J.M.; Segvich, S.J.; Hollister, S.J.; Krebsbach, P.H. Engineered osteochondral grafts using biphasic composite solid free-form fabricated scaffolds. Tissue Eng. 2004, 10, 1376–1385. [Google Scholar]
- Jung, Y.; Kim, S.H.; Kim, Y.H.; Kim, S.H. The effect of hybridization of hydrogels and poly (L-lactide-co-epsilon-caprolactone) scaffold on cartilage tissue engineering. J. Biomat. Sci. Polym. E 2010, 21, 581–592. [Google Scholar] [CrossRef]
- Kawazoe, N.; Inoue, C.; Tateishi, T.; Chen, G. A cell leakproof PLGA-collagen hybrid scaffold for cartilage tissue engineering. Biotechnol. Prog. 2010, 26, 819–826. [Google Scholar]
- Chen, G.; Sato, T.; Ushida, T.; Ochiai, N.; Tateishi, T. Tissue engineering of cartilage using a hybrid scaffold of synthetic polymer and collagen. Tissue Eng. 2004, 10, 323–330. [Google Scholar] [CrossRef]
- Hiraoka, Y.; Kimura, Y.; Ueda, H.; Tabata, Y. fabrication and biocompatibility of collagen sponge reinforced with poly (glycolic acid) fiber. Tissue Eng. 2003, 9, 1101–1112. [Google Scholar] [CrossRef]
- Jung, Y.; Kim, S.-H.; Kim, Y.H.; Kim, S.H. The effects of dynamic and three-dimensional environments on chondrogenic differentiation of bone marrow stromal cells source. Biomed. Mater. 2009, 4. [Google Scholar] [CrossRef]
- Lee, H.; Yeo, M.; Ahn, S.; Kang, D.O.; Jang, C.H.; Lee, H.; Park, G.M.; Kim, G.H. Designed hybrid scaffolds consisting of polycaprolactone microstrands and electrospun collagen-nanofibers for bone tissue regeneration. J. Biomed. Mater. Res. B Appl. Biomater. 2011, 97, 263–270. [Google Scholar]
- Klein, T.J.; Schumacher, B.L.; Schmidt, T.A.; Li, K.W.; Voegtline, M.S.; Masuda, K.; Thonar, E.J.; Sah, R.L. Tissue engineering of stratified articular cartilage from chondrocyte subpopulations. Osteoarth. Cart. 2003, 11, 595–602. [Google Scholar] [CrossRef]
- Yu, H.; Grynpas, M.; Kandel, R.A. Composition of cartilagenous tissue with mineralized and non-mineralized zones formed in vitro. Biomaterials 1997, 18, 1425–1432. [Google Scholar] [CrossRef]
- Hu, J.C.; Athanasiou, K.A. A self-assembling process in articular cartilage tissue engineering. Tissue Eng. 2006, 12, 969–979. [Google Scholar]
- Elder, B.D.; Athanasiou, K.A. Effects of temporal hydrostatic pressure on tissue-engineered bovine articular cartilage constructs. Tissue Eng. Part A 2009, 15, 1151–1158. [Google Scholar] [CrossRef]
- Elder, S.H.; Cooley, A.J., Jr.; Borazjani, A.; Sowell, B.L.; To, H.; Tran, S.C. Production of hyaline-like cartilage by bone marrow mesenchymal stem cells in a self-assembly model. Tissue Eng. Part A 2009, 15, 3025–3036. [Google Scholar] [CrossRef]
- Ofek, G.; Revell, C.M.; Hu, J.C.; Allison, D.D.; Grande-Allen, K.J.; Athanasiou, K.A. Matrix development in self-assembly of articular cartilage. PLoS One 2008, 3, e2795. [Google Scholar]
- Jakab, K.; Norotte, C.; Marga, F.; Murphy, K.; Vunjak-Novakovic, G.; Forgacs, G. Tissue engineering by self-assembly and bio-printing of living cells. Biofabrication 2010, 2, 022001. [Google Scholar] [CrossRef]
- Wise, J.K.; Yarin, A.L.; Megaridis, C.M.; Cho, M. Chondrogenic differentiation of human mesenchymal stem cells on oriented nanofibrous scaffolds: engineering the superficial zone of articular cartilage. Tissue Eng. A 2009, 15, 913–921. [Google Scholar]
- Ng, K.; Wang, C.C.; Guo, X.E.; Ateshian, G.A.; Hung, C.T. Characterization of inhomogeneous Bi-layered chondrocyte-seeded agarose constructs of differing agarose concentrations. In Transactions of the Orthopedic Research Society, Proceedings of 49th Annual Meeting; Orthopedic Research Society, Chicago, III, Ed. The Orthopedic Research Society: New Orleans, LA, USA, 2003; Volume 28. Abstract no. 960. [Google Scholar]
- Ng, K.W.; Wang, C.C.; Mauck, R.L.; Kelly, T.N.; Chahine, N.O.; Costa, K.D.; Ateshian, G.A.; Hung, C.T. A Layered agarose approach to fabricate depth-dependent inhomogeneity in chondrocyte-seeded constructs. J. Orthop. Res. 2005, 23, 134–141. [Google Scholar] [CrossRef]
- Kim, T.K.; Sharma, B.; Williams, C.G.; Ruffner, M.A.; Malik, A.; McFarland, E.G.; Elisseeff, J.H. Experimental model for cartilage tissue engineering to regenerate the zonal organization of articular cartilage. Osteoarth. Cart. 2003, 11, 653–664. [Google Scholar] [CrossRef]
- Sharma, B.; Williams, C.G.; Kim, T.K.; Malik, A.; Elisseeff, J.H. Multi-layered hydrogel constructs recreate zonal organization of articular cartilage. In Transactions of the Orthopedic Research Society, Proceedings of the 49th Annual Meeting, Orthopedic Research Society, Chicago, III, Ed. The Orthopedic Research Society: New Orleans, LA, 2003; Volume 28. Abstract no. 948. [Google Scholar]
- Klein, T.J.; Schumacher, B.L.; Li, K.W.; Voegtline, M.; Masuda, K.; Thonar, E.J.; Sah, R.L. Tissue engineered articular cartilage with functional stratification: Targeted delivery of chondrocytes expressing superficial zone protein. In Transactions of the Orthopedic Research Society, Proceedings of 48th Annual Meeting, Orthopedic Research Society, Chicago, III, Ed. The Orthopedic Research Society: Dallas, TX, USA, 2002; Volume 27. abstract no.212. [Google Scholar]
- Nguyen, L.H.; Kudva, A.K.; Guckert, N.L.; Linse, K.D.; Roy, K. Unique biomaterial compositions direct bone marrow stem cells into specific chondrocytic phenotypes corresponding to the various zones of articular cartilage. Biomaterials 2011, 32, 1327–1338. [Google Scholar]
- Thomson, B.; Smith, M.; Boyer, S.; Turner, R.; Kidd, D.; Riggs, H.; Dowthwaite, G.; Archer, C. Coated biomaterials, zonal cell-seeding and cartilage tissue engineering. In Transactions of the Orthopedic Research Society, Proceedings of 48th Annual Meeting, Orthopedic Research Society, Chicago, III, Ed. The Orthopedic Research Society: Dallas, TX, USA, 2002; Volume 27. abstract no. 477. [Google Scholar]
- Hwang, N.S.; Varghese, S.; Janice, H.L.; Theprungsirikul, P.; Canver, A.; Sharma, B.; Elisseeff, J. Response of zonal chondrocytes to extracellular matrix-hydrogels. FEBS Lett. 2007, 581, 4172–4178. [Google Scholar]
- Ng, K.W.; Ateshian, G.A.; Hung, C.T. Zonal chondrocytes seeded in a layered agarose hydrogel create engineered cartilage with depth-dependent cellular and mechanical inhomogeneity. Tissue Eng. Part A 2009, 15, 2315–2324. [Google Scholar] [CrossRef]
- Sharma, B.; Williams, C.G.; Kim, T.K.; Sun, D.; Malik, A.; Khan, M.; Leong, K.; Elisseeff, J.H. Designing zonal organization into tissue-engineered cartilage. Tissue Eng. 2007, 13, 405–414. [Google Scholar] [CrossRef]
- Gillette, B.M.; Rossen, N.S.; Das, N.; Leong, D.; Wang, M.; Dugar, A.; Sia, S.K. Engineering extracellular matrix structure in 3D multiphase tissues. Biomaterials 2011, 32, 8067–8076. [Google Scholar] [CrossRef]
- Grayson, W.L.; Bhumiratana, S.; Grace-Chao, P.H.; Hung, C.T.; Vunjak-Novakovic, G. Spatial regulation of human mesenchymal stem cell differentiation in engineered osteochondral constructs: Effects of pre-differentiation, soluble factors and medium perfusion. Osteoarth. Cart. 2010, 18, 714–723. [Google Scholar]
- Erisken, C.; Kalyon, D.M.; Wang, H. Functionally graded electrospun polycaprolactone and beta-tricalcium phosphate nanocomposites for tissue engineering applications. Biomaterials 2008, 29, 4065–4073. [Google Scholar] [CrossRef]
- O’Shea, T.M.; Miao, X. Bilayered scaffolds for osteochondral tissue engineering. Tissue Eng. Part B Rev. 2008, 14, 447–464. [Google Scholar] [CrossRef]
- Jeon, J.E.; Schrobback, K.; Hutmacher, D.W.; Klein, T.J. Dynamic compression improves biosynthesis of human zonal chondrocytes from osteoarthritis patients. Osteoarth. Cart. 2012, 20, 906–915. [Google Scholar] [CrossRef] [Green Version]
- Marsano, A.; Wendt, D.; Quinn, T.M.; Sims, T.J.; Farhadi, J.; Jakob, M.; Heberer, M.; Martin, I. Bi-zonal cartilaginous tissues engineered in a rotary cell culture system. Biorheology 2006, 43, 553–560. [Google Scholar]
- Mizuno, S. A novel method for assessing effects of hydrostatic fluid pressure on intracellular calcium: A study with bovine articular chondrocytes. Am. J. Physiol. Cell. Physiol. 2005, 288, C329–C337. [Google Scholar] [CrossRef]
- Klein, T.J.; Rizzi, S.C.; Reichert, J.C.; Georgi, N.; Malda, J.; Schuurman, W.; Crawford, R.W.; Hutmacher, D.W. Strategies for zonal cartilage repair using hydrogels. Macromol. Biosci. 2009, 9, 1049–1058. [Google Scholar] [CrossRef]
- Laasanen, M.S.; Toyras, J.; Korhonen, R.K.; Rieppo, J.; Saarakkala, S.; Nieminen, M.T.; Hirvonen, J.; Jurvelin, J.S. Biomechanical properties of knee articular cartilage. Biorheology 2003, 40, 133–140. [Google Scholar]
- Gepp, M.M.; Ehrhart, F.; Shirley, S.G.; Howitz, S.; Zimmermann, H. Dispensing of very low volumes of ultra high viscosity alginate gels: A new tool for encapsulation of adherent cells and rapid prototyping of scaffolds and implants. Biotechniques 2009, 46, 31–34. [Google Scholar]
- Tonde, M.P. Retrofitting a stereolithography system within a laminar flow hood. ETD Collection for University of Texas, El Paso. Paper AAI1473894. Available online: http://digitalcommons.utep.edu/dissertations/AAI1473894 (accessed on 8 September,2012).
- Ostrander, R.V.; Goomer, R.S.; Tontz, W.L.; Khatod, M.; Harwood, F.L.; Maris, T.M.; Amiel, D. Donor cell fate in tissue engineering for articular cartilage repair. Clin. Orthop. Relat. Res. 2001, 389, 228–237. [Google Scholar] [CrossRef]
- Mierisch, C.M.; Wilson, H.A.; Turner, M.A.; Milbrandt, T.A.; Berthoux, L.; Hammarskjold, M.L.; Rekosh, D.; Balian, G.; Diduch, D.R. Chondrocyte transplantation into articular cartilage defects with use of calcium alginate: The fate of the cells. J. Bone Joint Surg. Am. 2003, 85A, 1757–1767. [Google Scholar]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Izadifar, Z.; Chen, X.; Kulyk, W. Strategic Design and Fabrication of Engineered Scaffolds for Articular Cartilage Repair. J. Funct. Biomater. 2012, 3, 799-838. https://doi.org/10.3390/jfb3040799
Izadifar Z, Chen X, Kulyk W. Strategic Design and Fabrication of Engineered Scaffolds for Articular Cartilage Repair. Journal of Functional Biomaterials. 2012; 3(4):799-838. https://doi.org/10.3390/jfb3040799
Chicago/Turabian StyleIzadifar, Zohreh, Xiongbiao Chen, and William Kulyk. 2012. "Strategic Design and Fabrication of Engineered Scaffolds for Articular Cartilage Repair" Journal of Functional Biomaterials 3, no. 4: 799-838. https://doi.org/10.3390/jfb3040799