Medical Smart Textiles Based on Fiber Optic Technology: An Overview
Abstract
:1. Introduction
2. Working Principle of Fiber Optic Sensors Used in Smart Textiles
2.1. Fiber Bragg Grating Sensors

2.2. Intensity Modulated FOSs

3. Smart Textiles Based on Fiber Optic Sensors: Medical Applications
3.1. Smart Textiles Based on FBG Sensors: Medical Applications

| Reference | Working Principle | Medical Application | Metrological Properties and Other Features |
|---|---|---|---|
| [52,53,56] | Silica FBGs | Respiratory monitoring during MRI procedures | Non-invasive; MR compatible; good linearity in a wide range of strains with sensitivity = 0.35 nm/%; accuracy better than 0.1% of elongation |
| [58,59] | Silica FBGs | Cardiac and Respiratory monitoring during MRI procedures | Non-invasive; MR compatible; sensitivity of 0.8 nm/µε−1 |
| [59] | Silica FBGs | Cardiac and Respiratory monitoring | Non-invasive; Sensitivity of 8 nm/%; good linear trend; thermal sensitivity ≈ 10.7 × 10−3 nm/°C |
| [60,62] | Silica FBGs | Cardiac and Respiratory monitoring during MRI procedures | Non-invasive; MR compatible; Simple design; Good accuracy in terms of breathing rate (±1 bpm) and heartbeat per minute (±3 bpm); relative error in patients during MRI procedures <8% |
| [61] | Silica FBGs | Cardiac and Respiratory monitoring during MRI | Non-invasive; Simple design; Flat frequency response in the range of interest (0.5 Hz up to 20 Hz); maximum relative error of 12% |
| [63] | Silica FBG | Heart rate monitoring | Non-invasive; MR compatible; Root mean square error lower than 6 beats per minute |
| [64] | Silica FBGs | Respiratory function monitoring | Non-invasive; 6% of error on the average volume |
| [65] | Bare FBG | Body temperature monitoring | Non-invasive; Sensitivity of 150 pm/°C in the range of interest (from 33 °C to 42 °C); accuracy 0.1 °C |
| [52,53,56] | Macro-bending/OTDR technique | Respiratory monitoring | Non-invasive; MR compatible; Good sensitivity stability after 172800 cycles (variations < 10%); low cost component for their interrogation |
| [66] | Intensity modulated | Respiratory monitoring | Non-invasive; MR compatible; low cost component |
| [67,68] | Intensity modulated | Respiratory monitoring | Non-invasive; low cost component |
| [69,70] | Macrobending hetero-core fiber optic | Respiratory monitoring | Non-invasive; low cost component; good agreement with the breathing rate measured by a commercial device |
| [71] | microbending | Respiratory monitoring during MRI procedures | Non-invasive; MR compatible; Accuracy better than ±2 breaths per minute |
| [72] | microbending | Respiratory rate and heart rate | Non-invasive; MR compatible; Accuracy better than ±2 breaths or beats per minute for respiratory monitoring heart rate |
| [73] | microbending | Heartbeat and respiratory monitoring | Non-invasive; low cost component; good agreement with the heart beat measured by a commercial device |
3.2. Smart Textiles Based on Intensity-Modulated FOSs

4. Discussion
Author Contributions
Conflicts of Interest
References
- Lymberis, A.; Olsson, S. Intelligent Biomedical Clothing for Personal Health and Disease Management: State of the Art and Future Vision. Telemed. J. E-Health 2003, 9, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Lobodzinski, S.S.; Laks, M.M. New devices for very long-term ECG monitoring. Cardiol. J. 2012, 19, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Lobodzinski, S.S. ECG patch monitors for assessment of cardiac rhythm abnormalities. Prog. Cardiovas. Dis. 2013, 56, 224–229. [Google Scholar] [CrossRef]
- Inan, O.T.; Etemadi, M.; Wiard, R.M.; Giovangrandi, L.; Kovacs, G.T. Robust ballistocardiogram acquisition for home monitoring. Physiol. Meas. 2009, 30, 169–185. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Tao, X. Smart textiles: Passive smart. Text. Asia 2001, 45–49. [Google Scholar]
- Zhang, X.; Tao, X. Smart textiles: Active smart. Text. Asia 2001, 49–52. [Google Scholar]
- Krehel, M.; Wolf, M.; Boesel, L.F.; Rossi, R.M.; Bona, G.L.; Scherer, L.G. Development of a luminous textile for reflective pulse oximetry measurements. Biomed. Opt. Express 2014, 5, 2537–2547. [Google Scholar] [CrossRef] [PubMed]
- Li, H.N.; Li, D.S.; Song, G.B. Recent applications of fiber optic sensors to health monitoring in civil engineering. Eng. Struct. 2014, 26, 1647–1657. [Google Scholar] [CrossRef]
- Da Silva, A.F.; Gonçalves, A.F.; de Almeida Ferreira, L.A.; Araújo, F.M.M.; Mendes, P.M.; Correia, J.H. PVC smart sensing foil for advanced strain measurements. IEEE Sens. J. 2010, 10, 1149–1155. [Google Scholar]
- Silvestri, S.; Schena, E. Optical-fiber measurement systems for medical applications. In Optelectronics: Devices and Applications; Predeep, P., Ed.; InTech: Rijeka, Croatia, 2011. [Google Scholar]
- Lee, B. Review of the present status of optical fiber sensors. Opt. Fiber Technol. 2003, 9, 57–79. [Google Scholar] [CrossRef]
- Marazuela, M.; Moreno-Bondi, M. Fiber-optic biosensors—An overview. Anal. Bioanal. Chem. 2002, 372, 664–682. [Google Scholar] [CrossRef] [PubMed]
- Grattan, K.T.V.; Meggitt, B.T. Optical Fiber Sensor Technology, Vol. 2—Devices and Technology; Chapman & Hall: London, USA, 1998. [Google Scholar]
- Udd, E. Fiber Optic Sensors, 1st ed.; John Wiley & Sons, Inc.: Hoboken, New Jersey, 2006. [Google Scholar]
- Wang, X.D.; Wolfbeis, O.S. Fiber-optic chemical sensors and biosensors (2008–2012). Anal. Chem. 2012, 85, 487–508. [Google Scholar] [CrossRef] [PubMed]
- Krebber, K.; Liehr, S.; Witt, J. Smart technical textiles based on fibre optic sensors. In Proceedings of the 22nd International Conference on Optical Fiber Sensors, Beijing, China, 14 October 2012.
- Ghosh, S.; Amidei, C.; Furrow, K. Development of a sensor-embedded flexible textile structure for apparel or large area applications. Indian J. Fibre Text. 2005, 30, 42–48. [Google Scholar]
- Quandt, B.M.; Scherer, L.J.; Boesel, L.F.; Wolf, M.; Bona, G.L.; Rossi, R.M. Body-monitoring and health supervision by means of optical fiber-based sensing systems in medical textiles. Adv. Healthc. Mater. 2015, 4, 330–355. [Google Scholar] [CrossRef] [PubMed]
- Hill, K.O.; Fujii, Y.; Johnson, D.C.; Kawasaki, B.S. Photosensitivity in optical fiber waveguides: Application to reflection filter fabrication. Appl. Phys. Lett. 1978, 32, 647–649. [Google Scholar] [CrossRef]
- Meltz, G.; Morey, W.W.; Glenn, W.H. Formation of Bragg gratings in optical fibers by a transverse holographic method. Opt. Lett. 1989, 14, 823–825. [Google Scholar] [CrossRef] [PubMed]
- Rao, Y.J.; Webb, D.J.; Jackson, D.A.; Zhang, L.; Bennion, I. Optical in-fiber bragg grating sensor systems for medical applications. J. Biomed. Opt. 1998, 3, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Gurkan, D.; Starodubov, D.; Yuan, X. Monitoring of the heartbeat sounds using an optical fiber bragg grating sensor. In Proceedings of the 4th IEEE Conference Sensors 2005, Irvine, CA, USA, 30 October–3 November 2005.
- Haines, D.E. Determinants of lesion size during radiofrequency catheter ablation: The role of electrode-tissue contact pressure and duration of energy delivery. J. Cariovasc. Electrophysiol. 1991, 2, 509–515. [Google Scholar] [CrossRef]
- Yokoyama, K.; Nakagawa, H.; Shah, D.C.; Lambert, H.; Leo, G.; Aeby, N.; Ikeda, A.; Pitha, J.V.; Sharma, T.; Lazzara, R.; et al. Novel contact force sensor incorporated in irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop and thrombus. Circ. Arrhythm. Electrophysiol. 2008, 1, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.Z.; Tan, K.M.; Tjin, S.C.; Liaw, C.Y.; Roy Chaudhuri, P.; Cuo, X.; Lu, Cu. Design of a foot-pressure monitoring transducer for diabetic patients based on FBG sensors. In Proceedings of the LEOS, the 16th Annual Meeting of the IEEE, Tucson, AZ, USA, 27–30 October 2003; pp. 23–24.
- Al-Fakih, E.; Abu Osman, N.A.; Mahamd Adikan, F.R. The use of fiber Bragg grating sensors in biomechanics and rehabilitation applications: The state-of-the-art and ongoing research topics. Sensors 2012, 12, 12890–12926. [Google Scholar] [CrossRef] [PubMed]
- Tjin, S.C.; Tan, Y.K.; Yow, M.; Lam, Y.Z.; Hao, J. Recording compliance of dental splint use in obstructive sleep apnoea patients by force and temperature modeling. Med. Biol. Eng. Comput. 2001, 39, 182–184. [Google Scholar] [CrossRef] [PubMed]
- Saccomandi, P.; Schena, E.; Caponero, M.A.; di Matteo, F.M.; Martino, M.; Pandolfi, M.; Silvestri, S. Theoretical analysis and experimental evaluation of laser-induced interstitial thermotherapy in ex vivo porcine pancreas. IEEE Trans. Biomed. Eng. 2012, 59, 2958–2964. [Google Scholar] [CrossRef] [PubMed]
- Di Matteo, F.; Martino, M.; Rea, R.; Pandolfi, M.; Panzera, F.; Stigliano, E.; Schena, E.; Saccomandi, P.; Silvestri, S.; Pacella, C.M.; et al. US-guided application of Nd: YAG laser in porcine pancreatic tissue: An ex vivo study and numerical simulation. Gastrointest. Endosc. 2013, 78, 750–755. [Google Scholar] [CrossRef] [PubMed]
- Saccomandi, P.; Schena, E.; Giurazza, F.; del Vescovo, R.; Caponero, M.A.; Mortato, L.; Panzera, F.; Cazzato, R.L.; Grasso, F.R.; di Matteo, F.M.; et al. Temperature monitoring and lesion volume estimation during double-applicator laser-induced thermotherapy in ex vivo swine pancreas: A preliminary study. Laser Med. Sci. 2014, 29, 607–614. [Google Scholar] [CrossRef]
- Saccomandi, P.; Schena, E.; di Matteo, F.M.; Pandolfi, M.; Martino, M.; Rea, R.; Silvestri, S. Laser Interstitial Thermotherapy for pancreatic tumor ablation: Theoretical model and experimental validation. In Proceedings of the 2011 Annual International Conference of the IEEE on Engineering in Medicine and Biology Society, EMBC, Boston, MA, USA, 30 August–3 September 2011; pp. 5585–5588.
- Wehrle, G.; Nohama, P.; Kalinowski, H.J.; Torres, P.I.; Valente, L.C.G. A fibre optic Bragg grating strain sensor for monitoring ventilatory movements. Meas. Sci. Technol. 2001, 12, 805. [Google Scholar] [CrossRef]
- Allsop, T.; Miller, M.; Bennion, I.; Carroll, K.; Lloyd, G.; Webb, D.J. Application of long-period-grating sensors to respiratory plethysmography. J. Biomed. Opt. 2007, 12. [Google Scholar] [CrossRef]
- Cowie, B.M.; Webb, D.J.; Tam, B.; Slack, P.; Brett, P.N. Fibre Bragg grating sensors for distributive tactile sensing. Meas. Sci. Technol. 2007, 18. [Google Scholar] [CrossRef]
- Saccomandi, P.; Schena, E.; Oddo, C.M.; Zollo, L.; Silvestri, S.; Guglielmelli, E. Microfabricated Tactile Sensors for Biomedical Applications: A Review. Biosensors 2014, 4, 422–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mishra, V.; Singh, N.; Tiwari, U.; Kapur, P. Fiber grating sensors in medicine: Current and emerging applications. Sens. Actuat A Phys. 2011, 167, 279–290. [Google Scholar] [CrossRef]
- Taffoni, F.; Formica, D.; Saccomandi, P.; Pino, G.D.; Schena, E. Optical fiber-based MR-compatible sensors for medical applications: An overview. Sensors 2013, 13, 14105–14120. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Tajima, K.; Kubota, Y. Macrobending characteristics of a hetero-core splice fiber optic sensor for displacement and liquid detection. IEICE Trans. Electron. 2000, 83, 309–314. [Google Scholar]
- Nishiyama, M.; Sasaki, H.; Watanabe, K. A deformation sensitive pad-structure embedded with hetero-core optic fiber sensors. Sens. Actuat A Phys. 2007, 136, 205–211. [Google Scholar] [CrossRef]
- Lekholm, A.; Lindstrom, L. Optoelectronic transducer for intravascular measurements of pressure variations. Med. Biol. Eng. 1969, 7, 333–335. [Google Scholar] [CrossRef] [PubMed]
- Wald, A.; Post, K.; Ransohoff, J.; Hass, W.; Epstein, F. A new technique for monitoring epidural intracranial pressure. Med. Instrum. 1977, 11, 352–354. [Google Scholar] [PubMed]
- Piper, I.; Barnes, A.; Smith, D.; Dunn, L. The Camino intracranial pressure sensor: Is it optimal technology? An internal audit with a review of current intracranial pressure monitoring technologies. Neurosurgery 2001, 49, 1158–1165. [Google Scholar] [PubMed]
- Wolthuis, R.A.; Mitchell, G.L.; Hartl, J.C.; Saaski, E. Development of a dual function sensor system for measuring pressure and temperature at the tip of a single optical fiber. IEEE Trans. Biomed. Eng. 1993, 40, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Babchenko, A.; Khanokh, B.; Shomer, Y.; Nitzan, M. Fiber optic sensor for the measurement of respiratory chest circumference changes. J. Biomed. Opt. 1999, 4, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Maletras, F.X.; Augousti, A.T.; Mason, J. Construction and calibration of a new design of Fiber Optic Respiratory Plethysmograph (FORP). In Proceedings of the SPIE 4444, Optomechanical Design and Engineering 2001, San Diego, CA, USA, 29 July 2001; p. 285.
- Nishyama, M.; Miyamoto, M.; Watanabe, K. Respiration and body movement analysis during sleep in bed using hetero-core fiber optic pressure sensors without constraint to human activity. J. Biomed. Opt. 2011, 16. [Google Scholar] [CrossRef]
- Schena, E.; Saccomandi, P.; Silvestri, S. A high sensitivity fiber optic macro-bend based gas flow rate transducer for low flow rates: Theory, working principle, and static calibration. Rev. Sci. Instrum. 2013, 84. [Google Scholar] [CrossRef]
- Saccomandi, P.; Schena, E.; Silvestri, S. A novel target-type low pressure drop bidirectional optoelectronic air flow sensor for infant artificial ventilation: Measurement principle and static calibration. Rev. Sci. Instrum. 2011, 82. [Google Scholar] [CrossRef]
- Husdi, I.R.; Nakamura, K.; Ueha, S. Sensing characteristics of plastic optical fibres measured by optical time-domain refelectometry. Meas. Sci. Technol. 2004, 15, 1553–1559. [Google Scholar] [CrossRef]
- Augousti, A.T.; Maletras, F.X.; Mason, J. Improved fibre optic respiratory monitoring using a figure-of-eight coil. Physiol. Meas. 2005, 26, 585–590. [Google Scholar] [CrossRef] [PubMed]
- Augousti, A.T.; Raza, A.; Graves, M. Design and characterisation of a fibre optic respiratory plethysmograph (FORP). In Proceedings of the SPIE 1996, Biomedical Sensing, Imaging, and Tracking Technologies I, San Jose, CA, USA, 27 January 1996; pp. 250–257.
- Narbonneau, F.; Kinet, D.; Paquet, B.; Depré, A.; de Jonckheere, J.; Logier, R.; Zinke, J.; Witt, J.; Krebber, K. Smart textile embedding optical fibre sensors for healthcare monitoring during MRI. Adv. Sci. Tech. 2008, 60, 134–143. [Google Scholar] [CrossRef]
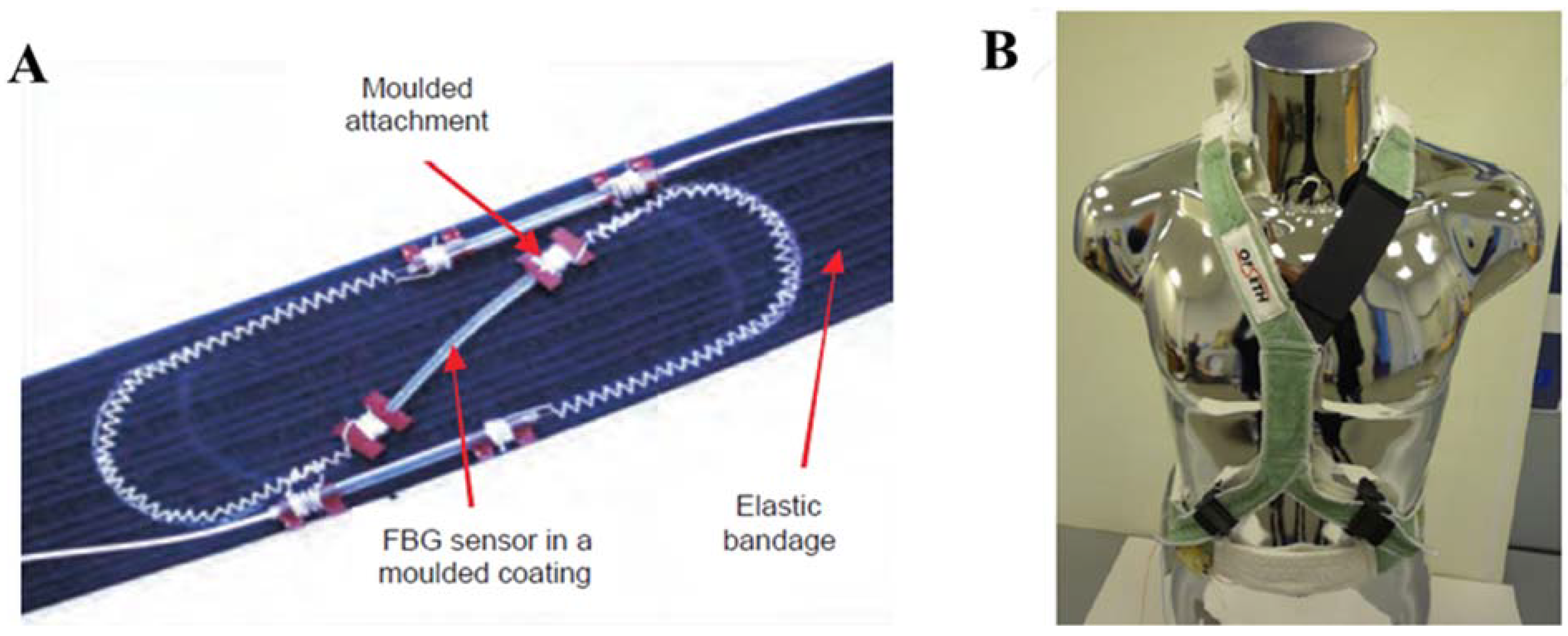
- Grillet, A.; Kinet, D.; Witt, J.; Schukar, M.; Krebber, K.; Pirotte, F.; Depré, A. Optical fiber sensors embedded into medical textiles for healthcare monitoring. IEEE Sens. J. 2008, 8, 1215–1222. [Google Scholar] [CrossRef]
- De Jonckheere, J.; Jeanne, M.; Narbonneau, F.; Witt, J.; Paquet, B.; Kinet, D.; Kreber, K.; Logier, R. OFSETH: A breathing motions monitoring system for patients under MRI. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, USA, 2-6 September 2009; pp. 1016–1019.
- Narbonneau, F.; D’Angelo, L.T.; Witt, J.; Paquet, B.; Kinet, D.; Kreber, K.; Logier, R. FBG-based smart textiles for continuous monitoring of respiratory movements for healthcare applications. In Proceedings of the 12th IEEE International Conference on e-Health Networking Applications and Services (Healthcom), Lyon, France, 1–3 July 2010; pp. 277–282.
- Witt, J.; Narbonneau, F.; Schukar, M.; Krebber, K.; de Jonckheere, J.; Jeanne, M.; Kinet, D.; Paquet, B.; Depré, A.; D’Angelo, L.T.; et al. Medical textiles with embedded fiber optic sensors for monitoring of respiratory movement. IEEE Sens. J. 2012, 12, 246–254. [Google Scholar] [CrossRef]
- Krebber, K. Smart Technical Textiles Based on Fiber Optic Sensors. In Current Developments in Optical Fiber Technology; InTech: Rijeka, Croatia, 2013; pp. 319–344. [Google Scholar]
- Silva, A.F.; Carmo, J.P.; Mendes, P.M.; Correia, J.H. Simultaneous cardiac and respiratory frequency measurement based on a single fiber Bragg grating sensor. Meas. Sci. Tech. 2011, 22. [Google Scholar] [CrossRef]
- Carmo, J.P.; da Silva, A.M. F.; Rocha, R.P.; Correia, J.H. Application of fiber Bragg gratings to wearable garments. IEEE Sens. J. 2012, 12, 261–266. [Google Scholar] [CrossRef]
- Dziuda, Ĺ.; Skibniewski, F.W.; Krej, M.; Baran, P.M. Fiber Bragg grating-based sensor for monitoring respiration and heart activity during magnetic resonance imaging examinations. J. Biomed. Opt. 2013, 18. [Google Scholar] [CrossRef]
- Dziuda, Ĺ.; Skibniewski, F.W.; Krej, M.; Lewandowski, J. Monitoring respiration and cardiac activity using fiber Bragg grating-based sensor. IEEE Trans. Biomed. Eng. 2012, 59, 1934–1942. [Google Scholar] [CrossRef] [PubMed]
- Dziuda, L.; Krej, M.; Skibniewski, F.W. Fiber Bragg grating strain sensor incorporated to monitor patient vital signs during MRI. IEEE Sens. J. 2013, 13, 4986–4991. [Google Scholar] [CrossRef]
- Krej, M.; Dziuda, L.; Skibniewski, F. A method of detecting heartbeat locations in the ballistocardiographic signal from the fiber-optic vital signs sensor. IEEE J. Biomed. Health Inform. 2015. [Google Scholar] [CrossRef]
- Allsop, T.; Bhamber, R.; Lloyd, G.; Miller, M.R.; Dixon, A.; Webb, D.; Castañón, J.D. A.; Bennion, I. Respiratory function monitoring using a real-time three-dimensional fiber-optic shaping sensing scheme based upon fiber Bragg gratings. J. Biomed. Opt. 2012, 17. [Google Scholar] [CrossRef]
- Li, H.; Yang, H.; Li, E.; Liu, Z.; Wei, K. Wearable sensors in intelligent clothing for measuring human body temperature based on optical fiber Bragg grating. Opt. Express 2012, 20, 11740–11752. [Google Scholar] [CrossRef] [PubMed]
- Yoo, W.J.; Jang, K.W.; Seo, J.K.; Heo, J.Y.; Moon, J.S.; Park, J.Y.; Lee, B.S. Development of respiration sensors using plastic optical fiber for respiratory monitoring inside MRI system. J. Opt. Soc. Korea 2010, 14, 235–239. [Google Scholar] [CrossRef]
- Krehel, M.; Rossi, R.M.; Bona, G.L.; Scherer, L.J. Characterization of flexible copolymer optical fibers for force sensing applications. Sensors 2013, 13, 11956–11968. [Google Scholar] [CrossRef] [PubMed]
- Krehel, M.; Schmid, M.; Rossi, R.M.; Boesel, L.F.; Bona, G.L.; Scherer, L.J. An optical fibre-based sensor for respiratory monitoring. Sensors 2014, 14, 13088–13101. [Google Scholar] [CrossRef] [PubMed]
- Alemdar, K.; Likoglu, S.; Fidanboylu, K.; Toker, O. A novel periodic macrobending hetero-core fiber optic sensor embedded in textiles. In Proceedings of the SPIE 9062, Smart Sensor Phenomena, Technology, Networks, and Systems Integration, San Diego, CA, USA, 8 March 2014.
- Alemdar, K.; Likoglu, S.; Fidanboylu, K.; Toker, O. A novel periodic macrobending hetero-core fiber optic sensor embedded in textiles. In Proceedings of the 8th International Conference on Electrical and Electronics Engineering (ELECO), Bursa, Turkey, 28–30 November 2013; pp. 467–471.
- Lau, D.; Chen, Z.; Teo, J.T.; Ng, S.H.; Rumpel, H.; Lian, Y.; Yang, H.; Kei, P.L. Intensity-Modulated Microbend Fiber Optic Sensor for Respiratory Monitoring and Gating During MRI. IEEE Trans. Biomed. Eng. 2013, 60, 2655–2662. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Lau, D.; Teo, J.T.; Ng, S.H.; Yang, X.; Kei, P.L. Simultaneous measurement of breathing rate and heart rate using a microbend multimode fiber optic sensor. J. Biomed. Opt. 2014, 19. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Chen, Z.; Chia, S.; Lam, H.; Ng, S.; Teo, J.; Wu, R. Textile Fiber Optic Micro Bend Sensor Used for Heartbeat and Respiration Monitoring. IEEE Sens. J. 2015, 15, 757–761. [Google Scholar] [CrossRef]
- Kinet, D.; Mégret, P.; Goossen, K.W.; Qiu, L.; Heider, D.; Caucheteur, C. Fiber Bragg Grating Sensors toward Structural Health Monitoring in Composite Materials: Challenges and Solutions. Sensors 2014, 14, 7394–7419. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Massaroni, C.; Saccomandi, P.; Schena, E. Medical Smart Textiles Based on Fiber Optic Technology: An Overview. J. Funct. Biomater. 2015, 6, 204-221. https://doi.org/10.3390/jfb6020204
Massaroni C, Saccomandi P, Schena E. Medical Smart Textiles Based on Fiber Optic Technology: An Overview. Journal of Functional Biomaterials. 2015; 6(2):204-221. https://doi.org/10.3390/jfb6020204
Chicago/Turabian StyleMassaroni, Carlo, Paola Saccomandi, and Emiliano Schena. 2015. "Medical Smart Textiles Based on Fiber Optic Technology: An Overview" Journal of Functional Biomaterials 6, no. 2: 204-221. https://doi.org/10.3390/jfb6020204







