Overview of Potential Clinical Applications of Hemoglobin Vesicles (HbV) as Artificial Red Cells, Evidenced by Preclinical Studies of the Academic Research Consortium
Abstract
:1. Introduction
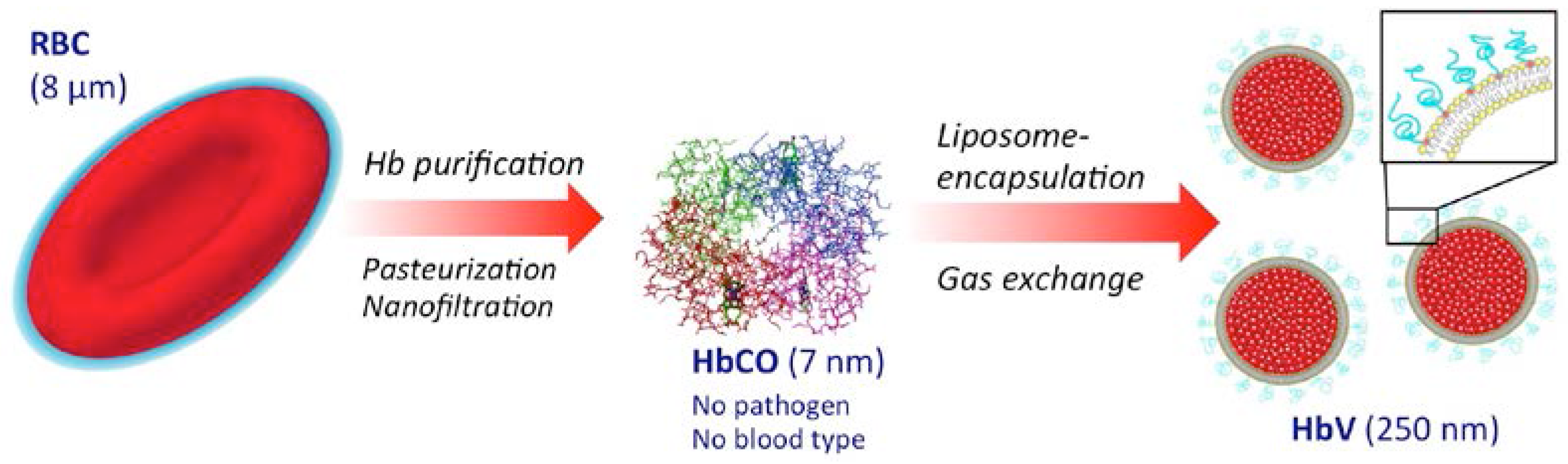
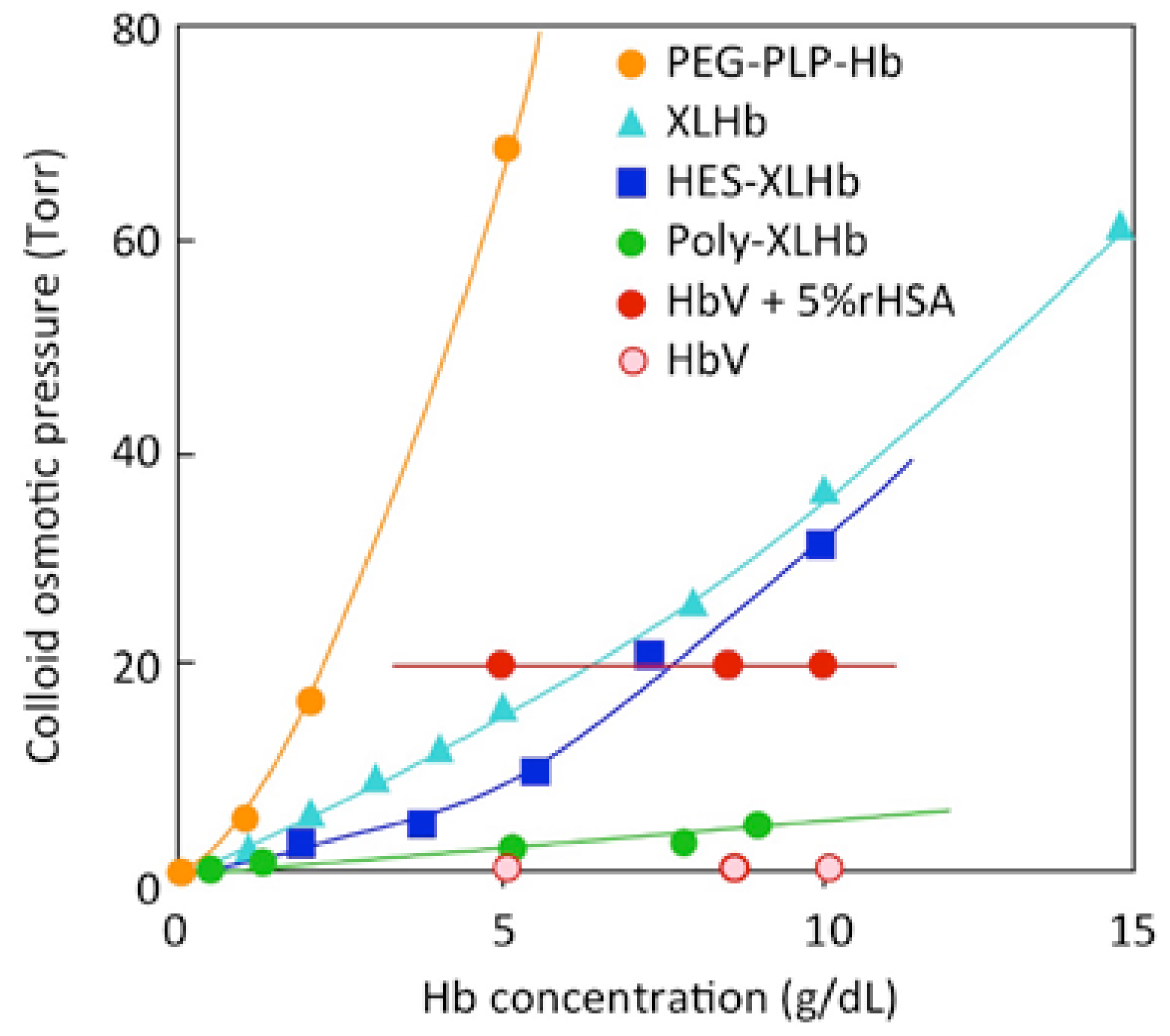
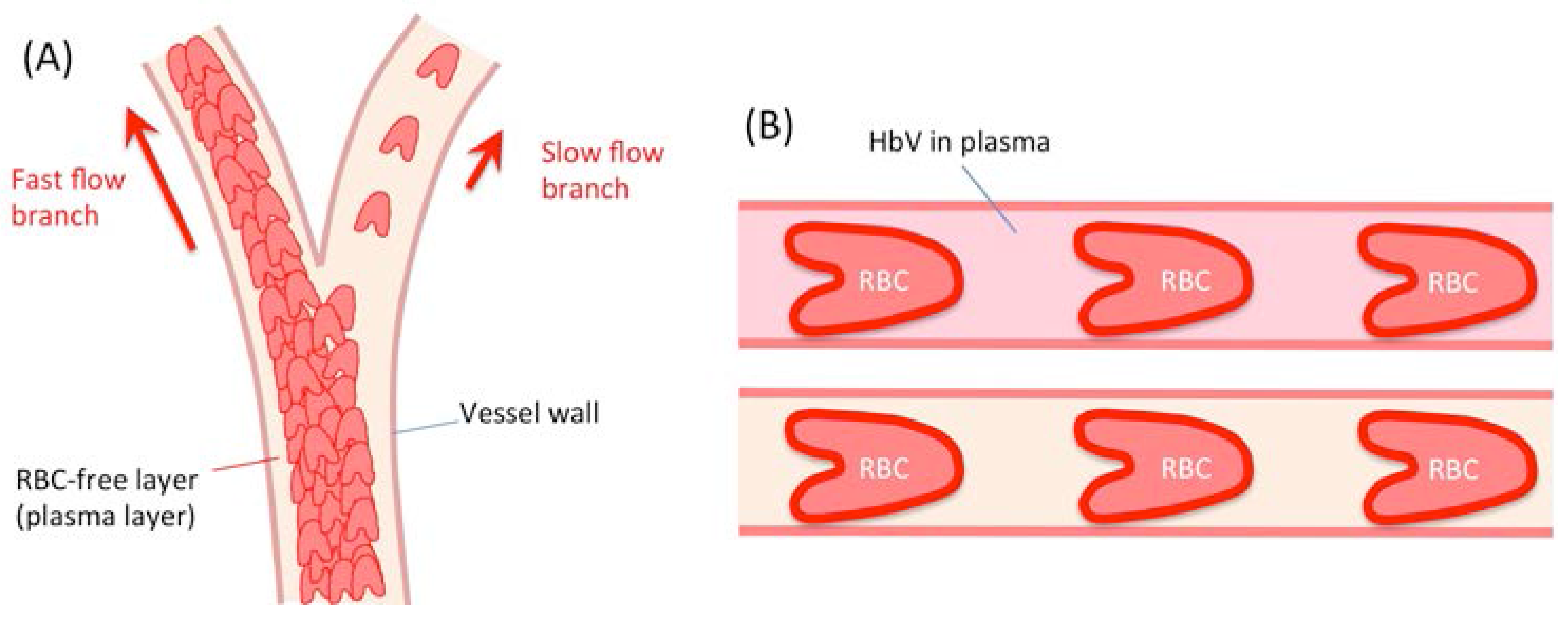
2. Preparation, Characteristics and Biocompatibility of HbV
3. Potential Usage of HbV as a Transfusion Alternative
4. Potential Usage of HbV as an Oxygen Carrier for Ischemic Disease and Ex Vivo Perfusion, a Photosensitizer, etc.
5. Potential Usage of HbV as a Carbon Monoxide Carrier
6. Conclusions
Acknowledgments
Conflicts of Interest
References
- Winslow, R.M. (Ed.) Blood Substitutes; Elsevier: Amsterdam, The Netherlands, 2005.
- Natanson, C.; Kern, S.J.; Lurie, P.; Banks, S.M.; Wolfe, S.M. Cell-free hemoglobin-based blood substitutes and risk of myocardial infarction and death: A metaanalysis. JAMA 2008, 299, 2304–2312. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.M. Semipermeable microcapsules. Science 1964, 164, 524–525. [Google Scholar] [CrossRef]
- Bangham, A.D.; Horne, R.W. Negative staining of phospholipids and their structure modification by surface-active agents as observed in the electron microscope. J. Mol. Biol. 1964, 8, 660–668. [Google Scholar] [CrossRef]
- Djordjevich, L.; Miller, I.F. Lipid encapsulated hemoglobin as a synthetic erythrocyte. Fed. Proc. 1977, 36, 567. [Google Scholar]
- Sakai, H.; Sou, K.; Tsuchida, E. Hemoglobin-vesicles as an artificial oxygen carrier. Methods Enzymol. 2009, 465, 363–384. [Google Scholar] [PubMed]
- Sato, T.; Sakai, H.; Sou, K.; Medebach, M.; Glatter, O.; Tsuchida, E. Static structures and dynamics of hemoglobin vesicle (HbV) developed as a transfusion alternative. J. Phys. Chem. B 2009, 113, 8418–8428. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Hara, H.; Yuasa, M.; Tsai, A.G.; Takeoka, S.; Tsuchida, E.; Intaglietta, M. Molecular dimensions of Hb-based O2 carriers determine constriction of resistance arteries and hypertension. Am. J. Physiol. Heart Circ. Physiol. 2000, 279, H908–H915. [Google Scholar] [PubMed]
- Takeoka, S.; Teramura, Y.; Atoji, T.; Tsuchida, E. Effect of Hb-encapsulation with vesicles on H2O2 reaction and lipid peroxidation. Bioconjug. Chem. 2002, 13, 1302–1308. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Sato, A.; Masuda, K.; Takeoka, S.; Tsuchida, E. Encapsulation of concentrated hemoglobin solution in phospholipid vesicles retards the reaction with NO, but not CO, by intracellular diffusion barrier. J. Biol. Chem. 2008, 283, 1508–1517. [Google Scholar] [CrossRef] [PubMed]
- Abe, H.; Fujihara, M.; Azuma, H.; Ikeda, H.; Ikebuchi, K.; Takeoka, S.; Tsuchida, E.; Harashima, H. Interaction of hemoglobin vesicles, a cellular-type artificial oxygen carrier, with human plasma: Effects on coagulation, kallikrein-kinin, and complement systems. Artif. Cells Blood Substit. Immobil. Biotechnol. 2006, 34, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wakamoto, S.; Fujihara, M.; Abe, H.; Yamaguchi, M.; Azuma, H.; Ikeda, H.; Takeoka, S.; Tsuchida, E. Effects of hemoglobin vesicles on resting and agonist-stimulated human platelets in vitro. Artif. Cells Blood Substit. Immobil. Biotechnol. 2005, 33, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Suzuki, Y.; Sou, K.; Kano, M. Cardiopulmonary hemodynamic responses to the small injection of hemoglobin vesicles (artificial oxygen carriers) in miniature pigs. J. Biomed. Mater. Res. A 2012, 100, 2668–2677. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, D.; Azuma, H.; Sakai, H.; Sou, K.; Wakita, D.; Abe, H.; Fujihara, M.; Horinouchi, H.; Nishimura, T.; Kobayashi, K.; et al. Phagocytosis of liposome particles by rat splenic immature monocytes makes them transiently and highly immunosuppressive in ex vivo culture conditions. J. Pharmacol. Exp. Ther. 2011, 337, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Horinouchi, H.; Yamamoto, M.; Ikeda, E.; Takeoka, S.; Takaori, M.; Tsuchida, E.; Kobayashi, K. Acute 40 percent exchange-transfusion with hemoglobin-vesicles (HbV) suspended in recombinant human serum albumin solution: Degradation of HbV and erythropoiesis in a rat spleen for 2 weeks. Transfusion 2006, 46, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Sou, K.; Tsuchida, E. Electrostatic interactions and complement activation on the surface of phospholipid vesicle containing acidic lipids: Effect of the structure of acidic groups. Biochim. Biophys. Acta 2008, 1778, 1035–1041. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Masada, Y.; Horinouchi, H.; Ikeda, E.; Sou, K.; Takeoka, S.; Suematsu, M.; Takaori, M.; Kobayashi, K.; Tsuchida, E. Physiological capacity of the reticuloendothelial system for the degradation of hemoglobin vesicles (artificial oxygen carriers) after massive intravenous doses by daily repeated infusions for 14 days. J. Pharmacol. Exp. Ther. 2004, 311, 874–884. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Horinouchi, H.; Masada, Y.; Takeoka, S.; Ikeda, E.; Takaori, M.; Kobayashi, K.; Tsuchida, E. Metabolism of hemoglobin-vesicles (artificial oxygen carriers) and their influence on organ functions in a rat model. Biomaterials 2004, 25, 4317–4325. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, K.; Urata, Y.; Anraku, M.; Maruyama, T.; Watanabe, H.; Sakai, H.; Horinouchi, H.; Kobayashi, K.; Tsuchida, E.; Kai, T.; et al. Pharmacokinetic study of enclosed hemoglobin and outer lipid component after the administration of hemoglobin vesicles as an artificial oxygen carrier. Drug Metab. Dispos. 2009, 37, 1456–1463. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Yuasa, M.; Onuma, H.; Takeoka, S.; Tsuchida, E. Synthesis and physicochemical characterization of a series of hemoglobin-based oxygen carriers: Objective comparison between cellular and acellular types. Bioconjug. Chem. 2000, 11, 56–64. [Google Scholar] [CrossRef]
- Sakai, H.; Miyagawa, N.; Horinouchi, H.; Takeoka, S.; Takaori, M.; Tsuchida, E.; Kobayashi, K. Intravenous infusion of Hb-vesicles (artificial oxygen carriers) after repetitive blood exchange with a series of plasma expanders (water-soluble biopolymers) in a rat model. Polym. Adv. Technol. 2011, 22, 1216–1222. [Google Scholar] [CrossRef]
- Sakai, H.; Takeoka, S.; Park, S.; Kose, T.; Nishide, H.; Izumi, Y.; Yoshizu, A.; Kobayashi, K.; Tsuchida, E. Surface modification of hemoglobin vesicles with poly(ethylene glycol) and affects on aggregation, viscosity, and blood flow during 90% exchange transfusion in anesthetized rats. Bioconjug. Chem. 1997, 8, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Tsai, A.G.; Kerger, H.; Park, S.; Takeoka, S.; Nishide, H.; Tsuchida, E.; Intaglietta, M. Subcutaneous microvascular responses to hemodilution with a red cell substitute consisting of polyethyleneglycol-modified vesicles encapsulating hemoglobin. J. Biomed. Mater. Res. 1998, 40, 66–78. [Google Scholar] [CrossRef]
- Sakai, H.; Tsai, A.G.; Rohlfs, R.J.; Hara, H.; Takeoka, S.; Tsuchida, E.; Intaglietta, M. Microvascular responses to hemodilution with Hb vesicles as red blood cell substitutes: Influence of O2 affinity. Am. J. Physiol. Heart Circ. Physiol. 1999, 276, H553–H562. [Google Scholar]
- Sakai, H.; Masada, Y.; Horinouchi, H.; Yamamoto, M.; Ikeda, E.; Takeoka, S.; Kobayashi, K.; Tsuchida, E. Hemoglobin-vesicles suspended in recombinant human serum albumin for resuscitation from hemorrhagic shock in anesthetized rats. Crit. Care Med. 2004, 32, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Yoshizu, A.; Izumi, Y.; Park, S.; Sakai, H.; Takeoka, S.; Horinouchi, H.; Ikeda, E.; Tsuchida, E.; Kobayashi, K. Hemorrhagic shock resuscitation with an artificial oxygen carrier, hemoglobin vesicle, maintain intestinal perfusion and suppress the increase in plasma tumor necrosis factor-α. ASAIO J. 2004, 50, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Terajima, K.; Tsueshita, T.; Sakamoto, A.; Ogawa, R. Fluid resuscitation with hemoglobin vesicles in a rabbit model of acute hemorrhagic shock. Shock 2006, 25, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Seishi, Y.; Obata, Y.; Takeoka, S.; Horinouchi, H.; Tsuchida, E.; Kobayashi, K. Fluid resuscitation with artificial oxygen carriers in hemorrhaged rats: Profiles of hemoglobin vesicles degradation and hematopoiesis for 14 days. Shock 2009, 31, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Tokuno, M.; Taguchi, K.; Yamasaki, K.; Sakai, H.; Otagiri, M. Long-term stored hemoglobin-vesicles, a cellular type of hemoglobin-based oxygen carrier, has resuscitative effects comparable to that for fresh red blood cells in a rat model with massive hemorrhage without post-transfusion lung injury. PLoS ONE 2016, 11, e0165557. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Horinouchi, H.; Kobayashi, K.; Seishi, Y.; Sato, N.; Itoh, M.; Sakai, H. Fluid resuscitation of hemorrhagic shock with hemoglobin vesicles in beagle dogs: Pilot study. Artif. Cells Blood Substit. Biotechnol. 2012, 40, 179–195. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, T.; Horinouchi, H.; Izumi, Y.; Sakai, H.; Kobayashi, K. Cellular-type hemoglobin-based oxygen carrier as a resuscitative fluid for hemorrhagic shock: Acute and long-term safety evaluation using beagle dogs. In Hemoglobin-Based Oxygen Carriers as Red Cell Substitutes and Oxygen Therapeutics; Kim, H.W., Greenburg, A.G., Eds.; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Seishi, Y.; Horinouchi, H.; Sakai, H.; Kobayashi, K. Effect of the cellular-type artificial oxygen carrier hemoglobin vesicle as a resuscitative fluid for prehospital treatment: Experiments in a rat uncontrolled hemorrhagic shock model. Shock 2012, 38, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, M.; Aeba, R.; Yozu, R.; Kobayashi, K. Use of hemoglobin vesicles during cardiopulmonary bypass priming prevents neurocognitive decline in rats. Circulation 2006, 114 (Suppl. SI), I-220–I-225. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, H.; Furuya, T.; Sato, N.; Ohta, K.; Matsuura, A.; Ohmura, T.; Takagi, S.; Matsuura, M.; Yamashita, M.; Itoda, M.; et al. Effect of hemoglobin vesicle, a cellular-type artificial oxygen carrier, on middle cerebral artery occlusion- and arachidonic acid-induced stroke models in rats. Neurosci. Lett. 2007, 421, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Plock, J.A.; Tromp, A.E.; Contaldo, C.; Spanholtz, T.; Sinovcic, D.; Sakai, H.; Tsuchida, E.; Leung, M.; Banic, A.; Erni, D. Hemoglobin vesicles reduce hypoxia-related inflammation in critically ischemic hamster flap tissue. Crit. Care Med. 2007, 35, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Plock, J.A.; Rafatmehr, N.; Sinovcic, D.; Schnider, J.; Sakai, H.; Tsuchida, E.; Banic, A.; Erni, D. Hemoglobin vesicles improve wound healing and tissue survival in critically ischemic skin in mice. Am. J. Physiol. Heart Circ. Physiol. 2009, 297, H905–H910. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Ohta, H.; Tahara, Y.; Nakamura, S.; Taguchi, K.; Nakagawa, M.; Oishi, Y.; Goto, Y.; Wada, K.; Kaga, M.; et al. Artificial oxygen carriers rescue placental hypoxia and improve fetal development in the rat pre-eclampsia model. Sci. Rep. 2015, 5, 15271. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Izumi, Y.; Horinouchi, H.; Teramura, Y.; Sakai, H.; Kohno, M.; Watanabe, M.; Kawamura, M.; Adachi, T.; Ikeda, E.; et al. Systemic administration of hemoglobin vesicle elevates tumor tissue oxygen tension and modifies tumor response to irradiation. J. Surg. Res. 2009, 151, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.; Mori, T.; Kiyono, Y.; Tiwari, V.N.; Maruyama, R.; Kawai, K.; Okazawa, H. Cerebral oxygen metabolism of rats using injectable 15O-oxygen with a steady-state method. J. Cereb. Blood Flow Metab. 2012, 32, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, V.N.; Kiyono, Y.; Kobayashi, M.; Mori, T.; Kudo, T.; Okazawa, H.; Fujibayashi, Y. Automatic labeling method for injectable 15O-oxygen using hemoglobin-containing liposome vesicles and its application for measurement of brain oxygen consumption by PET. Nucl. Med. Biol. 2010, 37, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Verdu, E.F.; Bercik, P.; Huang, X.X.; Lu, J.; Al-Mutawaly, N.; Sakai, H.; Tompkins, T.A.; Croitoru, K.; Tsuchida, E.; Perdue, M.; et al. The role of luminal factors in the recovery of gastric function and behavioral changes after chronic Helicobacter pylori infection. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 295, G664–G670. [Google Scholar] [CrossRef] [PubMed]
- Araki, J.; Sakai, H.; Takeuchi, D.; Kagaya, Y.; Tashiro, K.; Naito, M.; Mihara, M.; Narushima, M.; Iida, T.; Koshima, I. Normothermic preservation of the rat hind limb with artificial oxygen-carrying hemoglobin vesicles. Transplantation 2015, 99, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Montagne, K.; Huang, H.; Ohara, K.; Matsumoto, K.; Mizuno, A.; Ohta, K.; Sakai, Y. Use of liposome encapsulated hemoglobin as an oxygen carrier for fetal and adult rat liver cell culture. J. Biosci. Bioeng. 2011, 112, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Rikihisa, N.; Watanabe, S.; Satoh, K.; Saito, K.; Sakai, H. Photosensitizer effects of artificial red cells on dye laser irradiation in an animal model assuming port-wine stain treatment. Plast. Reconstr. Surg. 2017, 139, 707e–716e. [Google Scholar] [CrossRef] [PubMed]
- Naito, Y.; Sakai, H.; Inoue, S.; Kawaguchi, M. Hemoglobin vesicles prolong the time to circulatory collapse in rats during apnea. BMC Anesth. 2017, 17, 44. [Google Scholar] [CrossRef]
- Motterlini, R.; Clark, J.E.; Foresti, R.; Sarathchandra, P.; Mann, B.E.; Green, C.J. Carbon monoxide-releasing molecules: Characterization of biochemical and vascular activities. Circ. Res. 2002, 90, e17–e24. [Google Scholar] [CrossRef] [PubMed]
- Cabrales, P.; Tsai, A.G.; Intaglietta, M. Hemorrhagic shock resuscitation with carbon monoxide saturated blood. Resuscitation 2007, 72, 306–318. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Horinouchi, H.; Tsuchida, E.; Kobayashi, K. Hemoglobin vesicles and red blood cells as carriers of carbon monoxide prior to oxygen for resuscitation after hemorrhagic shock in a rat model. Shock 2009, 31, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Nagao, S.; Taguchi, K.; Sakai, H.; Tanaka, R.; Horinouchi, H.; Watanabe, H.; Kobayashi, K.; Otagiri, M.; Maruyama, T. Carbon monoxide-bound hemoglobin-vesicles for the treatment of bleomycin-induced pulmonary fibrosis. Biomaterials 2014, 35, 6553–6562. [Google Scholar] [CrossRef] [PubMed]
- Nagao, S.; Taguchi, K.; Miyazaki, Y.; Wakayama, T.; Chuang, V.T.; Yamasaki, K.; Watanabe, H.; Sakai, H.; Otagiri, M.; Maruyama, T. Evaluation of a new type of nano-sized carbon monoxide donor on treating mice with experimentally induced colitis. J. Control. Release 2016, 234, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Nagao, S.; Taguchi, K.; Sakai, H.; Yamasaki, K.; Watanabe, H.; Otagiri, M.; Maruyama, T. Carbon monoxide-bound hemoglobin vesicles ameliorate multiorgan injuries induced by severe acute pancreatitis in mice by their anti-inflammatory and antioxidative properties. Int. J. Nanomed. 2016, 11, 5611–5620. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Horinouchi, H.; Azuma, H.; Otagiri, M.; Kobayashi, K. Safety evaluation of artificial red cells (hemoglobin-vesicles) as a transfusion alternative. Artif. Blood 2013, 21, 36–48. [Google Scholar]
| Application | Animal Species | Brief Description of Main Results | References |
|---|---|---|---|
| Isovolemic hemodilution (repeated injection at hemorrhage) | Wistar rats | 90% blood exchange with HbV suspended in HSA showed stable hemodynamics | [22] |
| Syrian golden hamsters | 80% blood exchange with HbV suspended in HSA showed stable hemodynamics and microvascular responses | [23,24] | |
| Wistar rats | 40% blood exchange with HbV suspended in rHSA, and 14 days observation | [15] | |
| Wistar rats | 60% blood exchange with a plasma expander (high Mw HES, low Mw HES, MFG, or rHSA) and subsequent injection of HbV (20 mL/kg) | [21] | |
| Hemorrhagic shock | Wistar rats | 50% blood withdrawal and resuscitation, 6 h observation | [25] |
| Japanese white rabbits | Twice of 40% blood withdrawal and resuscitation | [26] | |
| New Zealand white rabbits | Withdrawing blood to a mean arterial blood pressure of 30–35 mm Hg, and resuscitation with HbV/rHSA | [27] | |
| Wistar rats | 50% blood withdrawal and resuscitation, 14 days observation | [28] | |
| Lewis rats | 40% blood withdrawal and resuscitation, 6 h observation showed absence of acute lung injury. One-year-stored HbV was used for resuscitation | [29] | |
| Beagle dogs | 50% blood withdrawal and resuscitation. 4 h observation of hemodynamics | [30] | |
| Beagle dogs | 40% blood withdrawal and resuscitation, one year safety observation | [31] | |
| Uncontrolled hemorrhage | Wistar rats | Animals were heparinized and bled continuously from caudal artery. Injection of HbV suspended in HSA extended survival | [32] |
| Priming of ECMO | Wistar rats | Use of HbV for cardiopulmonary bypass priming prevented neurocognitive decline | [33] |
| Application | Animal Species | Brief Description of Main Results | References |
|---|---|---|---|
| Brain ischemia | Wistar rats | HbV injection to a middle cerebral artery occlusion/reperfusion model reduced cerebral infarct volume. HbV injection to an arachidonic acid-induced stroke model improved motor dysfunction score and suppressed edema | [34] |
| Skin flap ischemia | Syrian golden hamsters | Dorsal skin flap oxygenation was improved by systemic application of a highly viscous left-shifted HbV (P50 = 9 Torr) | [35] |
| DDY mice | Dorsal skin flap oxygenation and wound healing was improved by systemic application of left-shifted HbV (P50 = 9 Torr) | [36] | |
| Pre-eclampsia | Wistar rats | L-NAME was infused intravenously for 7 consecutive days between gestational day 14 (G14) and G21 to prepare a pre-eclampsia model with narrow placental spinal artery remodeling and impaired fetal growth. Co-injection of HbV improved fetal oxygenation and growth | [37] |
| Tumor | C57BL/6 mice | Lewis lung carcinoma in the left hind leg of mice. HbV administration increased tumor tissue oxygen tension and, following 20-Gy irradiation, delayed tumor growth | [38] |
| 15O-PET | Sprague Dawley rats | 15O2-HbV was injected to measure the cerebral metabolic rate of oxygen for diagnosis of brain infarction | [39,40] |
| Organ perfusion | BALB/c mice | Ex vivo arterial perfusion of intestine with HbV/HSA for 2 h maintained peristaltic motion | [41] |
| Wistar rats | Amputated hind limb was perfused with HbV/ET-kyoto for 6 h and re-planted. The rat used the replanted leg after 3 months | [42] | |
| Cell culturing | Rat hepatocyte | Culturing rat hepatocytes with HbV in 2D flat-plate perfusion bioreactor | [43] |
| Photo-sensitizer | Chicken wattle as a model of port-wine stain | Injection of HbV increases the capillary content of total Hb as a target of dye laser treatment. It would produce more heat and photocoagulation by the treatment | [44] |
| Apnea | Sprague Dawley rats | Injection of HbV prolonged the time to circulatory collapse during apnea in anesthesia | [45] |
| Application | Animal Species | Brief Description of Main Results | Reference |
|---|---|---|---|
| Hemorrhagic shock | Wistar rats | Hemorrhagic shocked rats were resuscitated with CO-HbV suspended in HSA. AST and ALT levels were reduced as compared to O2-HbV injection | [48] |
| Pulmonary fibrosis | Sea-ICR mice | Bleomycin-induced pulmonary fibrosis mice that received CO-HbV showed suppression of progression of fibrosis and improved respiratory function | [49] |
| Colitis | Sea-ICR mice | Dextran sulfate sodium-induced colitis model mice receiving CO-HbV improved colitis symptoms, colonic histopathological changes and the duration of survival compared to both saline and O2-HbV administration | [50] |
| Pancreatitis | BALB/cN mice | Pancreatitis model mice were prepared with a choline-deficient ethionine-supplemented diet. CO-HbV inhibited the production of systemic proinflammatory cytokines, neutrophil infiltration, and oxidative injuries | [51] |
© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakai, H. Overview of Potential Clinical Applications of Hemoglobin Vesicles (HbV) as Artificial Red Cells, Evidenced by Preclinical Studies of the Academic Research Consortium. J. Funct. Biomater. 2017, 8, 10. https://doi.org/10.3390/jfb8010010
Sakai H. Overview of Potential Clinical Applications of Hemoglobin Vesicles (HbV) as Artificial Red Cells, Evidenced by Preclinical Studies of the Academic Research Consortium. Journal of Functional Biomaterials. 2017; 8(1):10. https://doi.org/10.3390/jfb8010010
Chicago/Turabian StyleSakai, Hiromi. 2017. "Overview of Potential Clinical Applications of Hemoglobin Vesicles (HbV) as Artificial Red Cells, Evidenced by Preclinical Studies of the Academic Research Consortium" Journal of Functional Biomaterials 8, no. 1: 10. https://doi.org/10.3390/jfb8010010






