Endovascular Embolization by Transcatheter Delivery of Particles: Past, Present, and Future
Abstract
:1. Introduction
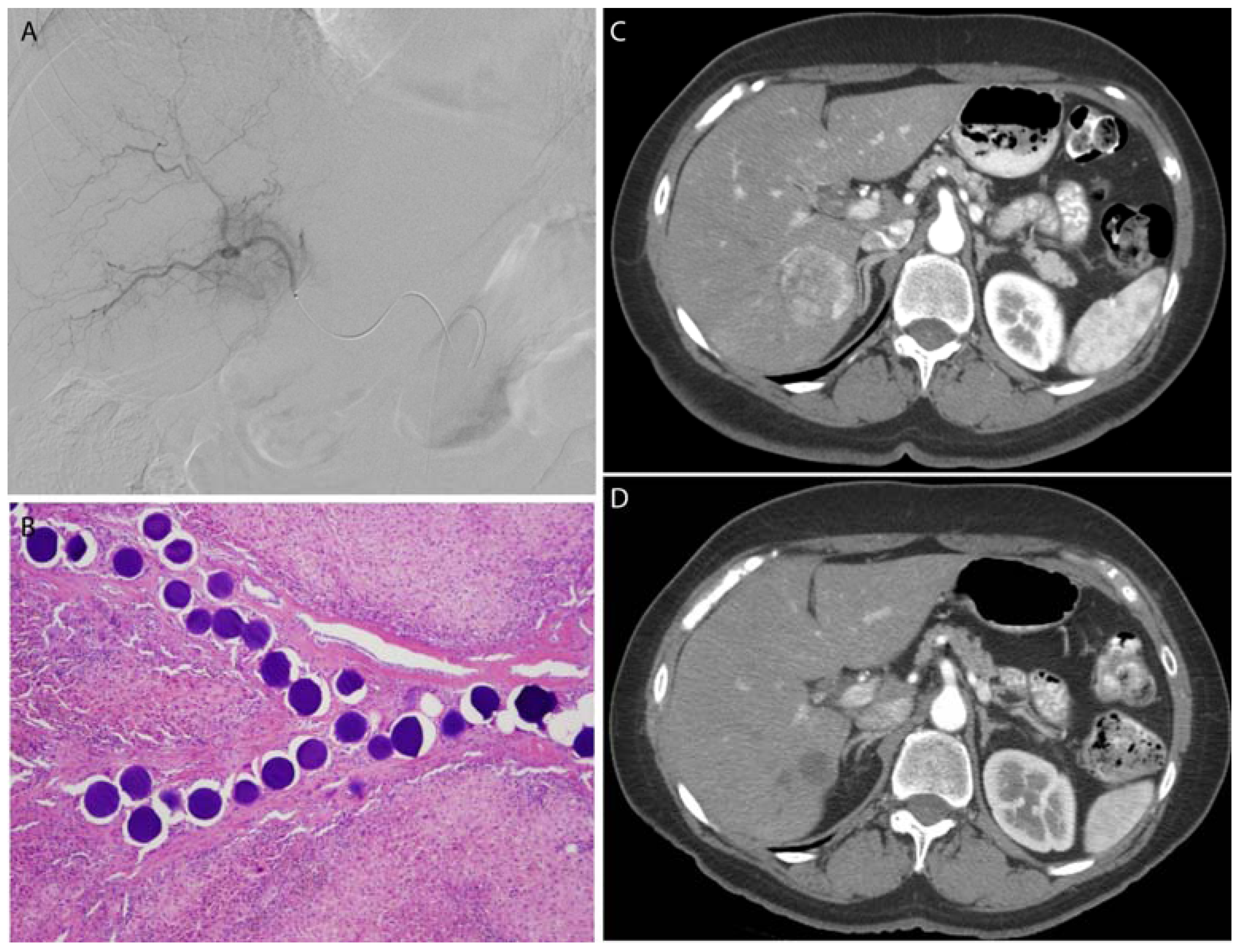
2. Historical Perspective on Particle Embolization Materials
3. Modern Particle Embolization: Synthesis, Applications, and Limitations
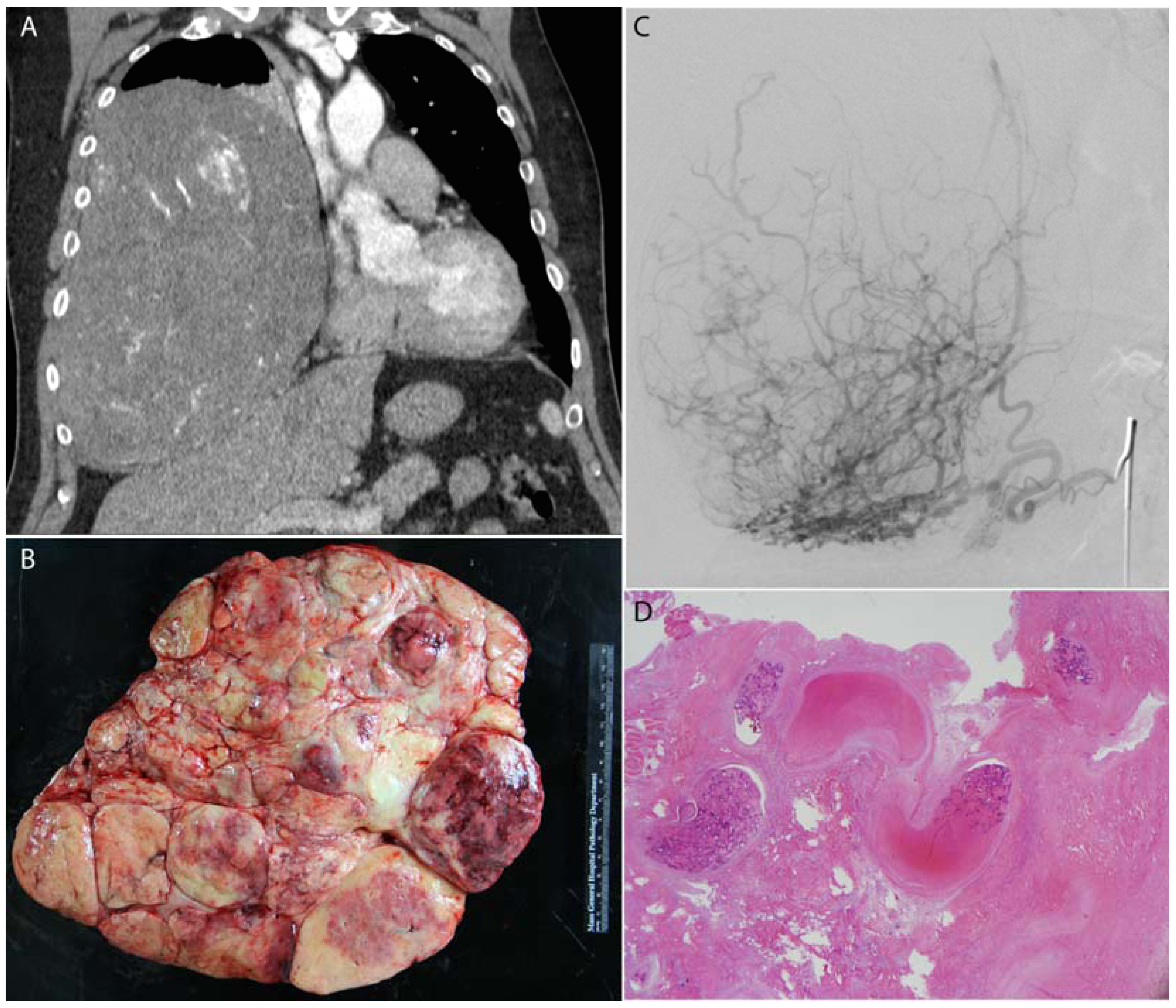
3.1. Polyvinyl Alcohol Particles
3.2. Gelatin Sponge
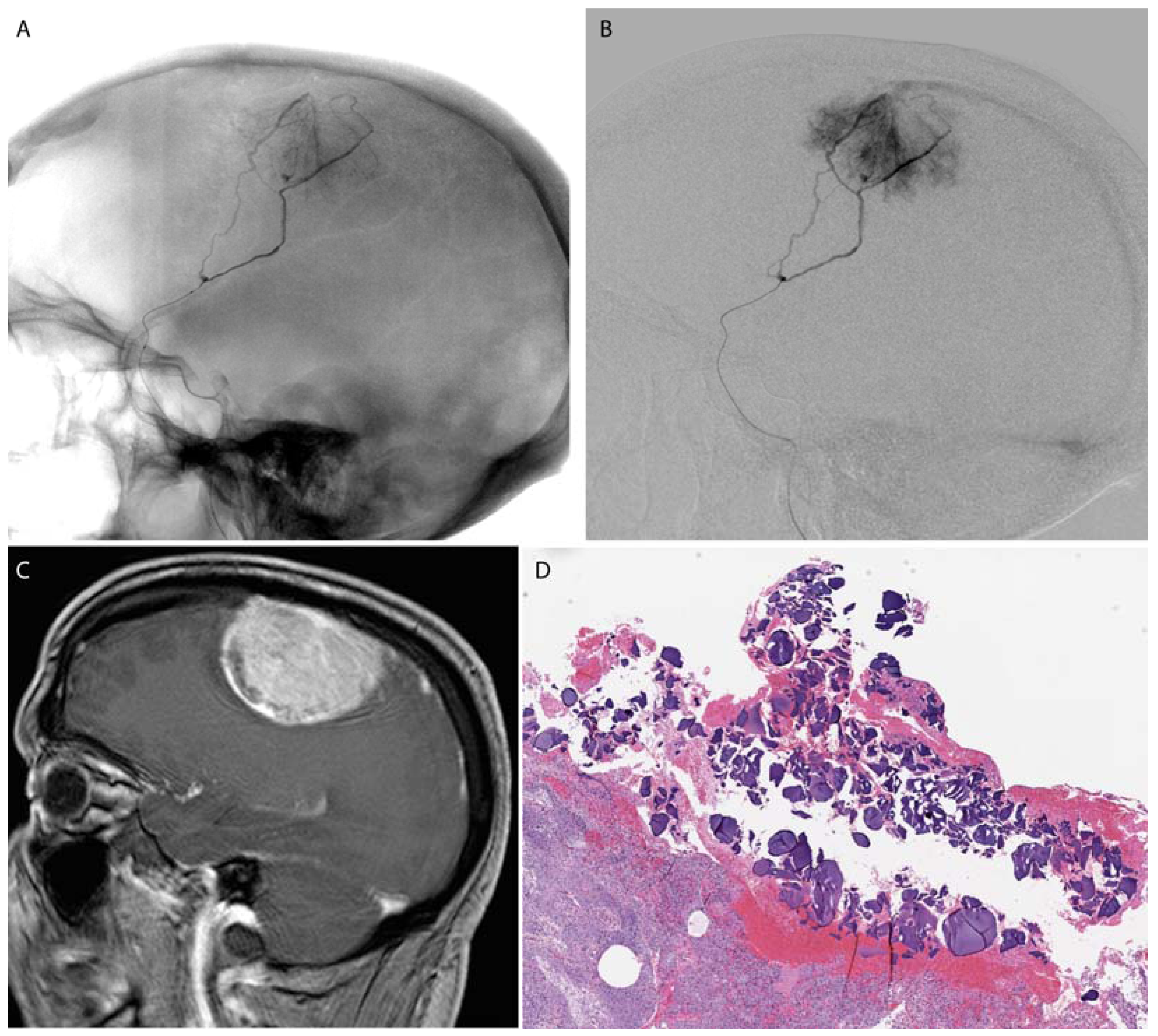
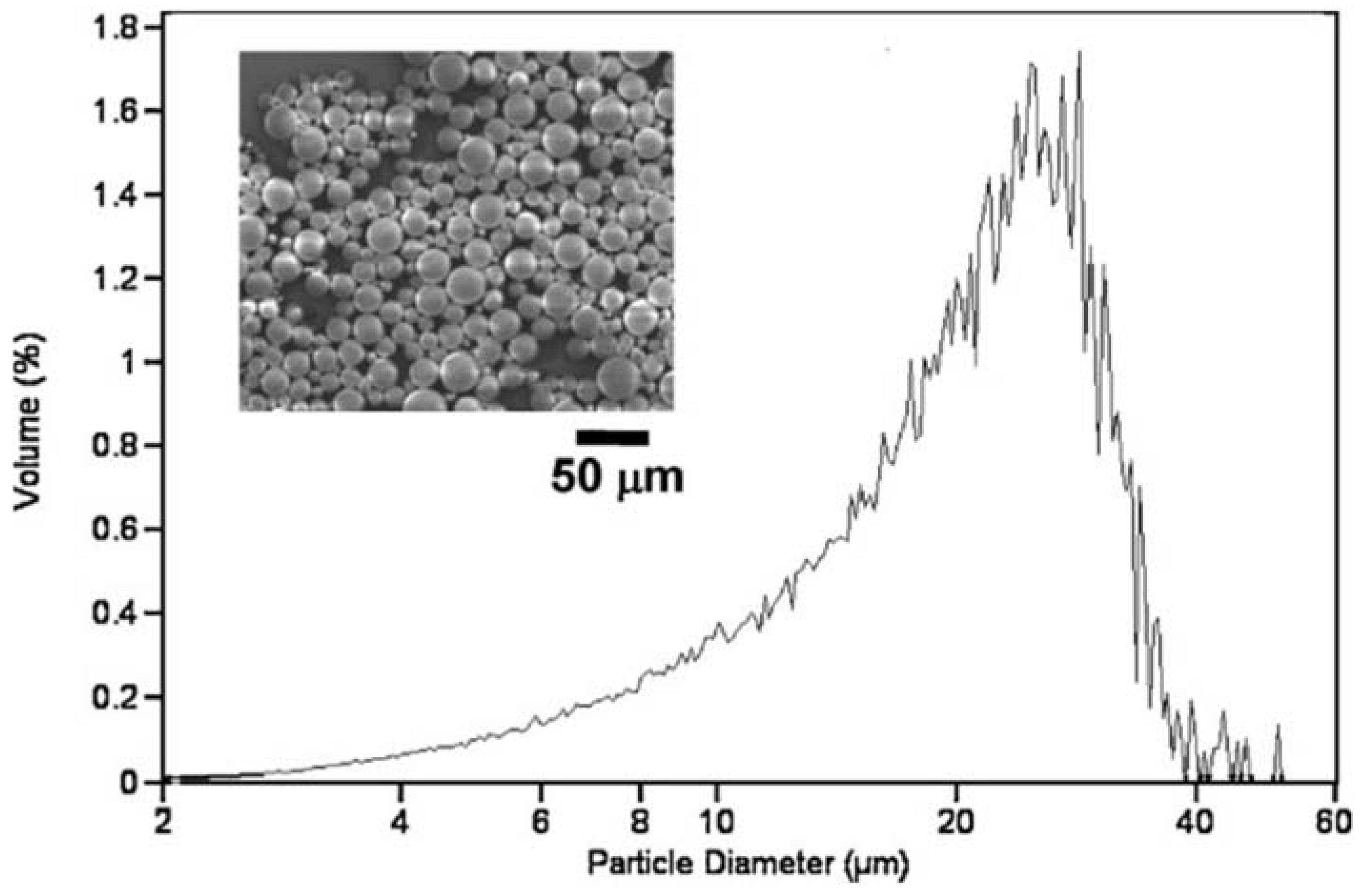
3.3. Microspheres
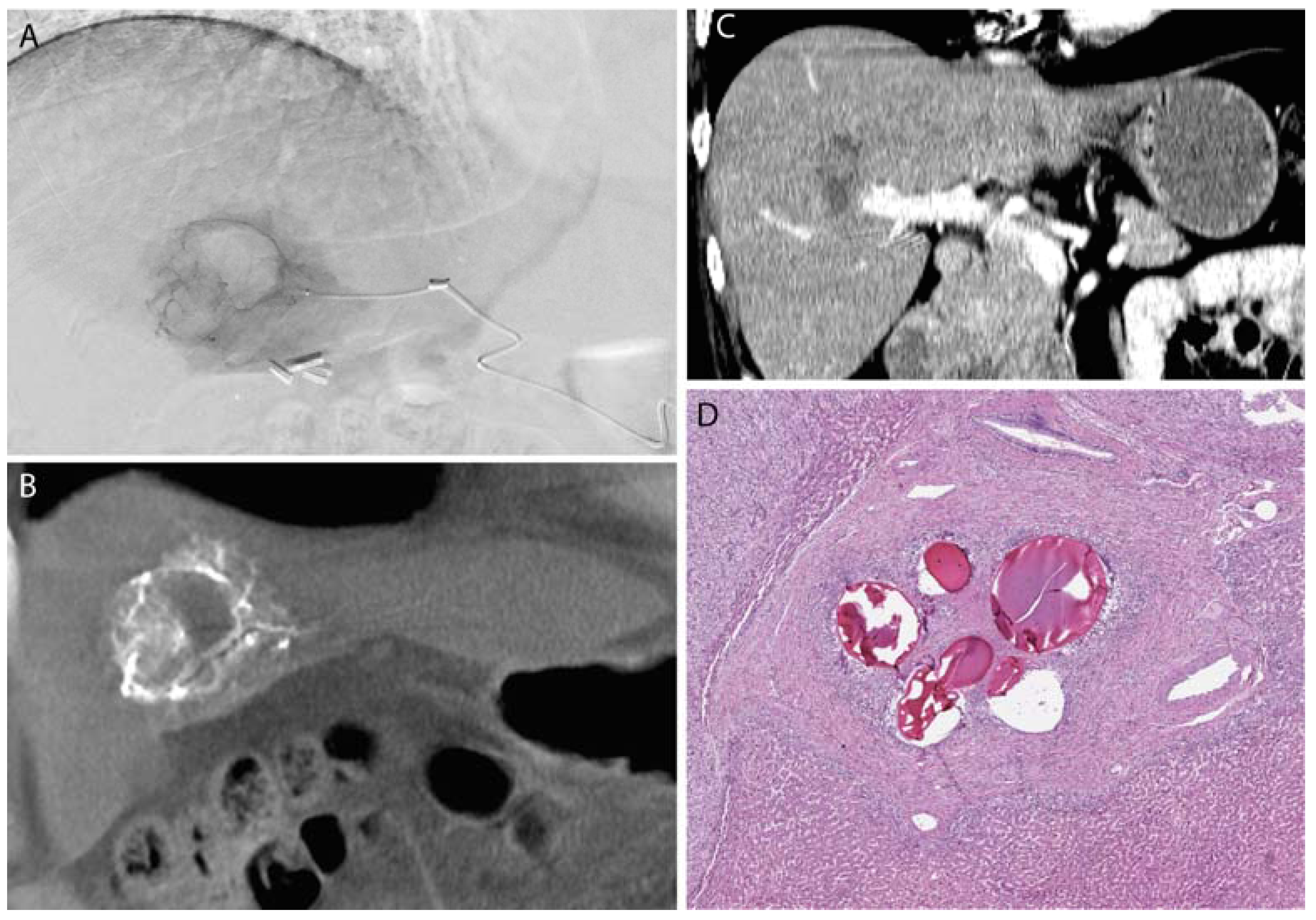
3.4. Drug Eluting Particles
4. Previewing the Future of Particle Embolization
4.1. Microfluidics
4.2. Tissue Engineering
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Dick, R. Therapeutic angiographic embolization. Br. J. Radiol. 1977, 50, 241–242. [Google Scholar] [CrossRef] [PubMed]
- Kunstlinger, F.; Brunelle, F.; Chaumont, P.; Doyon, D. Vascular occlusive agents. Am. J. Roentgenol. 1981, 136, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Rizk, G.K.; Atallah, N.K.; Bridi, G.I. Renal arteriovenous fistula treated by catheter embolization. Br. J. Radiol. 1973, 46, 222–224. [Google Scholar] [CrossRef] [PubMed]
- Kricheff, I.I.; Madayag, M.; Braunstein, P. Transfemoral catheter embolization of cerebral and posterior fossa arteriovenous malformations. Radiology 1972, 103, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Siskin, G.P.; Englander, M.; Stainken, B.F.; Ahn, J.; Dowling, K.; Dolen, E.G. Embolic agents used for uterine fibroid embolization. Am. J. Roentgenol. 2000, 175, 767–773. [Google Scholar] [CrossRef] [PubMed]
- Tadavarthy, S.M.; Knight, L.; Ovitt, T.W.; Snyder, C.; Amplatz, K. Therapeutic transcatheter arterial embolization. Radiology 1974, 112, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Marangos, N.; Schumacher, M. Facial palsy after glomus jugulare tumour embolization. J. Laryngol. Otol. 1999, 113, 268–270. [Google Scholar] [CrossRef] [PubMed]
- Sieber, P.R. Bladder necrosis secondary to pelvic artery embolization: Case report and literature review. J. Urol. 1994, 151, 422. [Google Scholar] [PubMed]
- Abada, H.T.; Golzarian, J. Gelatine sponge particles: Handling characteristics for endovascular use. Tech. Vasc. Interv. Radiol. 2007, 10, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Lubarsky, M.; Ray, C.E.; Funaki, B. Embolization agents-which one should be used when? Part 1: Large-vessel embolization. Semin. Interv. Radiol. 2009, 26, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Barth, K.H.; Strandberg, J.D.; White, R.I. Long term follow-up of transcatheter embolization with autologous clot, oxycel and gelfoam in domestic swine. Investig. Radiol. 1977, 12, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Jander, H.P.; Russinovich, N.A. Transcatheter gelfoam embolization in abdominal, retroperitoneal, and pelvic hemorrhage. Radiology 1980, 136, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Al-Thunyan, A.; Al-Meshal, O.; Al-Hussainan, H.; Al-Qahtani, M.H.; El-Sayed, A.A.F.; Al-Qattan, M.M. Buttock necrosis and paraplegia after bilateral internal iliac artery embolization for postpartum hemorrhage. Obstet. Gynecol. 2012, 120, 468–470. [Google Scholar] [CrossRef] [PubMed]
- Choo, Y.C.; Cho, K.J. Pelvic abscess complicating embolic therapy for control of bleeding cervical carcinoma and simultaneous radiation therapy. Obstet. Gynecol. 1980, 55, 76S–78S. [Google Scholar] [CrossRef] [PubMed]
- Stampfl, S.; Bellemann, N.; Stampfl, U.; Sommer, C.M.; Thierjung, H.; Lopez-Benitez, R.; Radeleff, B.; Berger, I. Arterial distribution characteristics of Embozene particles and comparison with other spherical embolic agents in the porcine acute embolization model. J. Vasc. Interv. Radiol. 2009, 20, 1597–1607. [Google Scholar] [CrossRef] [PubMed]
- Lewis, A.L.; Adams, C.; Busby, W.; Jones, S.A.; Wolfenden, L.C.; Leppard, S.W.; Palmer, R.R.; Small, S. Comparative in vitro evaluation of microspherical embolisation agents. J. Mater. Sci. Mater. Med. 2006, 17, 1193–1204. [Google Scholar] [CrossRef] [PubMed]
- Laurent, A. Microspheres and nonspherical particles for embolization. Tech. Vasc. Interv. Radiol. 2007, 10, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Spies, J.B. Current evidence on uterine embolization for fibroids. Semin. Interv. Radiol. 2013, 30, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Golzarian, J.; Lang, E.; Hovsepian, D.; Kroncke, T.; Lampmann, L.; Lohle, P.; Pelage, J.; Shlansky-Goldberg, R.; Valenti, D.; Vorwerk, D.; Spies, J. Higher rate of partial devascularization and clinical failure after uterine artery embolization for fibroids with spherical polyvinyl alcohol. Cardiovasc. Interv. Radiol. 2006, 29, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Liang, B.; Xiong, F.; Wu, H.; Wang, Y.; Dong, X.; Cheng, S.; Feng, G.S.; Zhou, G.F.; Xiong, B.; Liang, H.M.; et al. Effect of transcatheter intraarterial therapies on the distribution of Doxorubicin in liver cancer in a rabbit model. PLoS ONE 2013, 8, e76388. [Google Scholar] [CrossRef] [PubMed]
- Liapi, E.; Lee, K.-H.; Georgiades, C.C.; Hong, K.; Geschwind, J.-F.H. Drug-eluting particles for interventional pharmacology. Tech. Vasc. Interv. Radiol. 2007, 10, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.K.; Lee, D.S. Injectable biodegradable hydrogels. Macromol. Biosci. 2010, 10, 563–579. [Google Scholar] [CrossRef] [PubMed]
- Mani, K.; Campbell, A.; Fitzpatrick, J.; Modarai, B.; Carrell, T.; Rashid, H.; Zayed, H. A novel reverse thermosensitive polymer to achieve temporary atraumatic vessel occlusion in infra-popliteal bypasses. Eur. J. Vasc. Endovasc. Surg. 2013, 45, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Lewis, C.L.; Lin, Y.; Yang, C.; Manocchi, A.K.; Yuet, K.P.; Doyle, P.S.; Yi, H. Microfluidic fabrication of hydrogel microparticles containing functionalized viral nanotemplates. Langmuir 2010, 26, 13436–13441. [Google Scholar] [CrossRef] [PubMed]
- Tamatani, S.; Ozawa, T.; Minakawa, T.; Takeuchi, S.; Koike, T.; Tanaka, R. Histological interaction of cultured endothelial cells and endovascular embolic materials coated with extracellular matrix. J. Neurosurg. 1997, 86, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.P.; Yang, P.C.; Ma, Y.H.; Wu, T. Characterization of chitosan magnetic nanoparticles for in situ delivery of tissue plasminogen activator. Carbohydr. Polym. 2011, 84, 364–372. [Google Scholar] [CrossRef]
- Horák, D.; Svec, F.; Adamyan, A.; Titova, M.; Skuba, N.; Voronkova, O.; Trostenyuk, N.; Vishnevskii, V.; Gumargalieva, K. Haemostatic activity of ethamsylate and aminocaproic acid adsorbed poly(2-hydroxyethyl methacrylate) particles. Biomaterials 1992, 13, 521–526. [Google Scholar] [CrossRef]
- Saralidze, K.; van Hooy-Corstjens, C.S.J.; Koole, L.H.; Knetsch, M.L.W. New acrylic microspheres for arterial embolization: Combining radiopacity for precise localization with immobilized thrombin to trigger local blood coagulation. Biomaterials 2007, 28, 2457–2464. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Hashimoto, M.; Dang, T.T.; Hoare, T.; Kohane, D.S.; Whitesides, G.M.; Langer, R.; Anderson, D.G. Preparation of monodisperse biodegradable polymer microparticles using a microfluidic flow-focusing device for controlled drug delivery. Small 2009, 5, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- De Geest, B.G.; Urbanski, J.P.; Thorsen, T.; Demeester, J.; De Smedt, S.C. Synthesis of monodisperse biodegradable microgels in microfluidic devices. Langmuir 2005, 21, 10275–10279. [Google Scholar] [CrossRef] [PubMed]



© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheth, R.A.; Sabir, S.; Krishnamurthy, S.; Avery, R.K.; Zhang, Y.S.; Khademhosseini, A.; Oklu, R. Endovascular Embolization by Transcatheter Delivery of Particles: Past, Present, and Future. J. Funct. Biomater. 2017, 8, 12. https://doi.org/10.3390/jfb8020012
Sheth RA, Sabir S, Krishnamurthy S, Avery RK, Zhang YS, Khademhosseini A, Oklu R. Endovascular Embolization by Transcatheter Delivery of Particles: Past, Present, and Future. Journal of Functional Biomaterials. 2017; 8(2):12. https://doi.org/10.3390/jfb8020012
Chicago/Turabian StyleSheth, Rahul A., Sharjeel Sabir, Savitri Krishnamurthy, Reginald K. Avery, Yu Shrike Zhang, Ali Khademhosseini, and Rahmi Oklu. 2017. "Endovascular Embolization by Transcatheter Delivery of Particles: Past, Present, and Future" Journal of Functional Biomaterials 8, no. 2: 12. https://doi.org/10.3390/jfb8020012





