Exploring the Application of Graphene Oxide-Based Nanomaterials in the Repair of Osteoporotic Fractures
Abstract
:1. Introduction
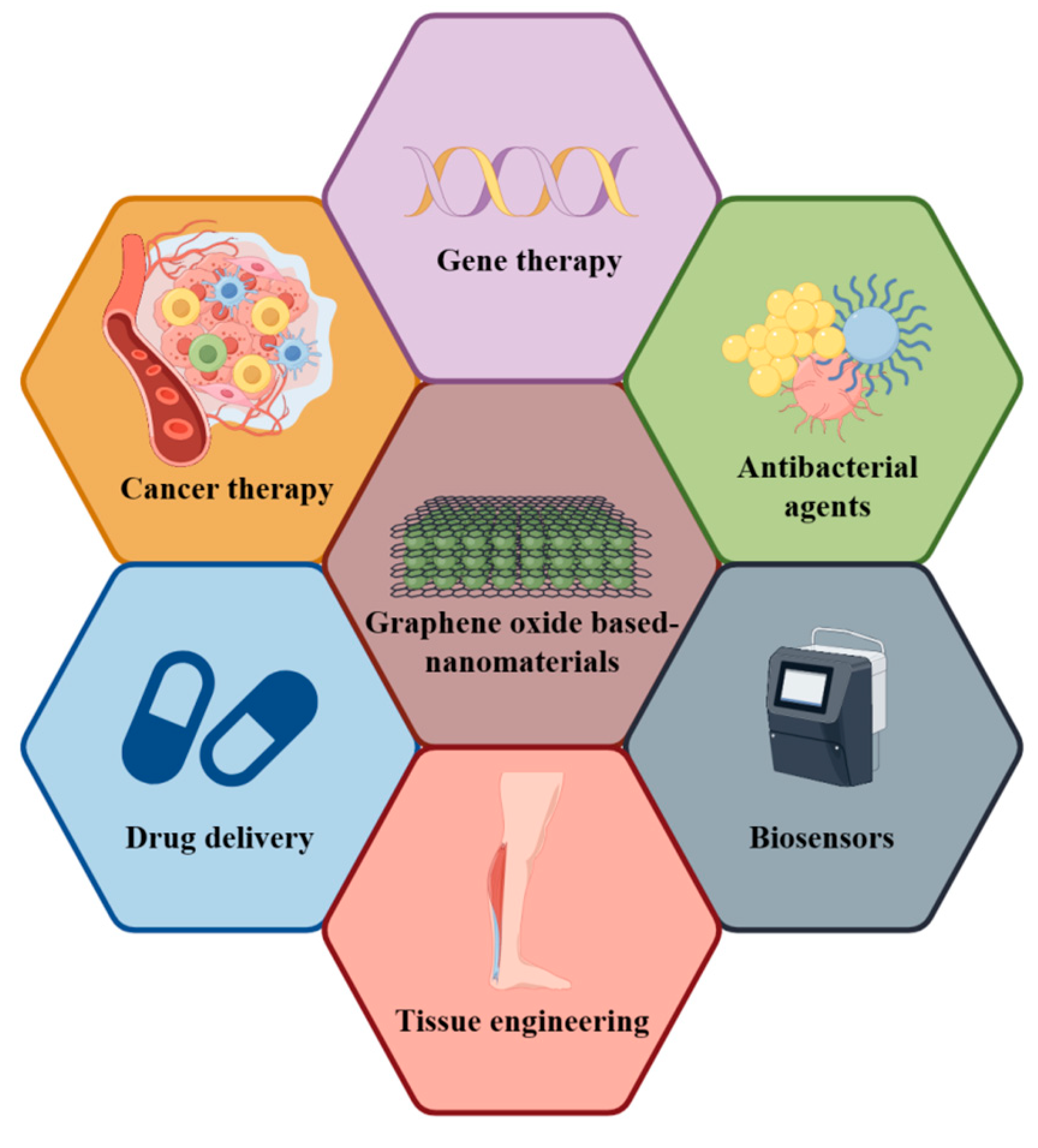
An Introduction to GO and GO-Based Nanomaterials
2. The Advantages of Using GO-Based Nanomaterials in the Treatment of Osteoporotic Fractures
2.1. Enhancing Material Properties to Promote Bone Tissue Repair: The Potential of GO and Its Derivatives
2.2. Harnessing Excellent Antimicrobial Properties: The Potential of GO-Based Nanomaterials
2.3. Promoting Bone Repair through Immune Regulation: The Potential of GO-Based Nanomaterials
2.4. Enhancing the Treatment of Osteoporotic Fractures: The Role of Drugs, Cells, and miRNA Loaded into GO-Based Nanomaterials
3. Potential Mechanisms and Related Signaling Pathways of Graphene Oxide-Based Materials in Promoting the Repair of Osteoporotic Fractures
3.1. Common Signaling Pathways in the Promotion of Osteoporotic Fracture Repair by Graphene Oxide-Based Nanomaterials
3.2. Mechanisms of Bone Tissue Repair Promoted by Graphene Oxide Composite-Based Nanomaterials through Immune Regulation
4. Cytotoxicity of Graphene Oxide Limits Its Application in Tissue Engineering
5. Conclusions and Perspective
Author Contributions
Funding
Conflicts of Interest
References
- Consensus development conference: Diagnosis, prophylaxis, and treatment of osteoporosis. Am. J. Med. 1993, 94, 646–650. [CrossRef]
- Compston, J.E.; McClung, M.R.; Leslie, W.D. Osteoporosis. Lancet 2019, 393, 364–376. [Google Scholar] [CrossRef]
- Gruber, R.; Koch, H.; Doll, B.A.; Tegtmeier, F.; Einhorn, T.A.; Hollinger, J.O. Fracture healing in the elderly patient. Exp. Gerontol. 2006, 41, 1080–1093. [Google Scholar] [CrossRef]
- Kammerlander, C.; Gebhard, F.; Meier, C.; Lenich, A.; Linhart, W.; Clasbrummel, B.; Neubauer-Gartzke, T.; Garcia-Alonso, M.; Pavelka, T.; Blauth, M. Standardised cement augmentation of the PFNA using a perforated blade: A new technique and preliminary clinical results. A prospective multicentre trial. Injury 2011, 42, 1484–1490. [Google Scholar] [CrossRef]
- Hollensteiner, M.; Sandriesser, S.; Bliven, E.; von Rüden, C.; Augat, P. Biomechanics of Osteoporotic Fracture Fixation. Curr. Osteoporos. Rep. 2019, 17, 363–374. [Google Scholar] [CrossRef]
- Osterhoff, G.; Morgan, E.F.; Shefelbine, S.J.; Karim, L.; McNamara, L.M.; Augat, P. Bone mechanical properties and changes with osteoporosis. Injury 2016, 47 (Suppl. S2), S11–S20. [Google Scholar] [CrossRef]
- Maki, B.E.; McIlroy, W.E. Control of rapid limb movements for balance recovery: Age-related changes and implications for fall prevention. Age Ageing 2006, 35 (Suppl. S2), ii12–ii18. [Google Scholar] [CrossRef]
- Gale, C.R.; Cooper, C.; Aihie Sayer, A. Prevalence and risk factors for falls in older men and women: The English Longitudinal Study of Ageing. Age Ageing 2016, 45, 789–794. [Google Scholar] [CrossRef]
- Röderer, G.; Scola, A.; Schmölz, W.; Gebhard, F.; Windolf, M.; Hofmann-Fliri, L. Biomechanical in vitro assessment of screw augmentation in locked plating of proximal humerus fractures. Injury 2013, 44, 1327–1332. [Google Scholar] [CrossRef]
- Wu, X.; Wang, Z.; Li, H.; Li, Y.; Wang, H.; Tian, W. Biomechanical evaluation of osteoporotic fracture: Metal fixation versus absorbable fixation in Sawbones models. Injury 2019, 50, 1272–1276. [Google Scholar] [CrossRef]
- von Rüden, C.; Augat, P. Failure of fracture fixation in osteoporotic bone. Injury 2016, 47 (Suppl. S2), S3–S10. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.J.; Zhang, X.Q.; Liu, Q.; Zhang, J.; Zhou, G. Nanotechnology: A promising method for oral cancer detection and diagnosis. J. Nanobiotechnol. 2018, 16, 52. [Google Scholar] [CrossRef]
- Ziąbka, M.; Menaszek, E.; Tarasiuk, J.; Wroński, S. Biocompatible Nanocomposite Implant with Silver Nanoparticles for Otology-In Vivo Evaluation. Nanomaterials 2018, 8, 764. [Google Scholar] [CrossRef]
- Cheng, X.; Wan, Q.; Pei, X. Graphene Family Materials in Bone Tissue Regeneration: Perspectives and Challenges. Nanoscale Res. Lett. 2018, 13, 289. [Google Scholar] [CrossRef]
- Mahmoudi, E.; Ang, W.L.; Ng, C.Y.; Ng, L.Y.; Mohammad, A.W.; Benamor, A. Distinguishing characteristics and usability of graphene oxide based on different sources of graphite feedstock. J. Colloid. Interf. Sci. 2019, 542, 429–440. [Google Scholar] [CrossRef]
- Xie, H.; Cao, T.; Rodríguez-Lozano, F.J.; Luong-Van, E.K.; Rosa, V. Graphene for the development of the next-generation of biocomposites for dental and medical applications. Dent. Mater. 2017, 33, 765–774. [Google Scholar] [CrossRef]
- Govindarajan, D.; Saravanan, S.; Sudhakar, S.; Vimalraj, S. Graphene: A Multifaceted Carbon-Based Material for Bone Tissue Engineering Applications. ACS Omega 2023, 9, 67–80. [Google Scholar] [CrossRef]
- Sofer, Z.; Jankovský, O.; Šimek, P.; Sedmidubský, D.; Šturala, J.; Kosina, J.; Mikšová, R.; Macková, A.; Mikulics, M.; Pumera, M. Insight into the mechanism of the thermal reduction of graphite oxide: Deuterium-labeled graphite oxide is the key. ACS Nano 2015, 9, 5478–5485. [Google Scholar] [CrossRef]
- Miao, Y.; Wang, X.; Liu, Y.; Liu, Z.; Chen, W. Preparation of Graphene Oxide/Cellulose Composites with Microcrystalline Cellulose Acid Hydrolysis Using the Waste Acids Generated by the Hummers Method of Graphene Oxide Synthesis. Polymers 2021, 13, 4453. [Google Scholar] [CrossRef]
- Soltani, T.; Lee, B.-K. Low intensity-ultrasonic irradiation for highly efficient, eco-friendly and fast synthesis of graphene oxide. Ultrason. Sonochem 2017, 38, 693–703. [Google Scholar] [CrossRef]
- Yu, H.; Zhang, B.; Bulin, C.; Li, R.; Xing, R. High-efficient Synthesis of Graphene Oxide Based on Improved Hummers Method. Sci. Rep. 2016, 6, 36143. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Z.; Wang, J.; Li, J.; Lin, Y. Graphene and graphene oxide: Biofunctionalization and applications in biotechnology. Trends Biotechnol. 2011, 29, 205–212. [Google Scholar] [CrossRef]
- Kinloch, I.A.; Suhr, J.; Lou, J.; Young, R.J.; Ajayan, P.M. Composites with carbon nanotubes and graphene: An outlook. Science 2018, 362, 547–553. [Google Scholar] [CrossRef]
- Yuan, Z.; Xiao, X.; Li, J.; Zhao, Z.; Yu, D.; Li, Q. Self-Assembled Graphene-Based Architectures and Their Applications. Adv. Sci. 2018, 5, 1700626. [Google Scholar] [CrossRef]
- Nanda, S.S.; Yi, D.K.; Kim, K. Study of antibacterial mechanism of graphene oxide using Raman spectroscopy. Sci. Rep. 2016, 6, 28443. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, Y.; Cheng, H.; Hu, Y.; Shi, G.; Dai, L.; Qu, L. Nitrogen-doped graphene quantum dots with oxygen-rich functional groups. J. Am. Chem. Soc. 2012, 134, 15–18. [Google Scholar] [CrossRef]
- Lim, S.Y.; Shen, W.; Gao, Z. Carbon quantum dots and their applications. Chem. Soc. Rev. 2015, 44, 362–381. [Google Scholar] [CrossRef]
- Lin, L.; Zhang, S. Creating high yield water soluble luminescent graphene quantum dots via exfoliating and disintegrating carbon nanotubes and graphite flakes. Chem. Commun. 2012, 48, 10177–10179. [Google Scholar] [CrossRef]
- Lin, T.N.; Chih, K.H.; Yuan, C.T.; Shen, J.L.; Lin, C.a.J.; Liu, W.R. Laser-ablation production of graphene oxide nanostructures: From ribbons to quantum dots. Nanoscale 2015, 7, 2708–2715. [Google Scholar] [CrossRef]
- Huang, Z.; Shen, Y.; Li, Y.; Zheng, W.; Xue, Y.; Qin, C.; Zhang, B.; Hao, J.; Feng, W. Facile synthesis of analogous graphene quantum dots with sp(2) hybridized carbon atom dominant structures and their photovoltaic application. Nanoscale 2014, 6, 13043–13052. [Google Scholar] [CrossRef]
- Li, X.; Cai, W.; An, J.; Kim, S.; Nah, J.; Yang, D.; Piner, R.; Velamakanni, A.; Jung, I.; Tutuc, E.; et al. Large-area synthesis of high-quality and uniform graphene films on copper foils. Science 2009, 324, 1312–1314. [Google Scholar] [CrossRef]
- Foroutan, T.; Nazemi, N.; Tavana, M.; Kassaee, M.Z.; Motamedi, E.; Soieshargh, S.; Zare Zardini, H. Suspended graphene oxide nanoparticle for accelerated multilayer osteoblast attachment. J. Biomed. Mater. Res. A 2018, 106, 293–303. [Google Scholar] [CrossRef]
- Sokolov, D.A.; Shepperd, K.R.; Orlando, T.M. Formation of Graphene Features from Direct Laser-Induced Reduction of Graphite Oxide. J. Phys. Chem. Lett. 2010, 1, 2633–2636. [Google Scholar] [CrossRef]
- Rai, V.K.; Mahata, S.; Kashyap, H.; Singh, M.; Rai, A. Bio-reduction of Graphene Oxide: Catalytic Applications of (Reduced) GO in Organic Synthesis. Curr. Org. Synth. 2020, 17, 164–191. [Google Scholar] [CrossRef]
- Gilje, S.; Dubin, S.; Badakhshan, A.; Farrar, J.; Danczyk, S.A.; Kaner, R.B. Photothermal deoxygenation of graphene oxide for patterning and distributed ignition applications. Adv. Mater. 2010, 22, 419–423. [Google Scholar] [CrossRef]
- Tan, Y.; Chen, Y.; Lu, T.; Witman, N.; Yan, B.; Gong, Y.; Ai, X.; Yang, L.; Liu, M.; Luo, R.; et al. Engineering a conduction-consistent cardiac patch with rGO/PLCL electrospun nanofibrous membranes and human iPSC-derived cardiomyocytes. Front. Bioeng. Biotech. 2023, 11, 1094397. [Google Scholar] [CrossRef]
- Ghasemlou, M.; Mayes, E.L.H.; Murdoch, B.J.; Le, P.H.; Dekiwadia, C.; Aburto-Medina, A.; Daver, F.; Ivanova, E.P.; Adhikari, B. Silicon-Doped Graphene Oxide Quantum Dots as Efficient Nanoconjugates for Multifunctional Nanocomposites. ACS Appl. Mater. Interfaces 2022, 14, 7161–7174. [Google Scholar] [CrossRef]
- Shi, C.; Yu, Y.; Wu, H.; Liu, H.; Guo, M.; Wang, W.; Wang, D.; Wei, C.; Zhai, H.; Yan, G.; et al. A graphene oxide-loaded processed pyritum composite hydrogel for accelerated bone regeneration via mediation of M2 macrophage polarization. Mater. Today Bio 2023, 22, 100753. [Google Scholar] [CrossRef]
- Tavakoli, M.; Emadi, R.; Salehi, H.; Labbaf, S.; Varshosaz, J. Incorporation of graphene oxide as a coupling agent in a 3D printed polylactic acid/hardystonite nanocomposite scaffold for bone tissue regeneration applications. Int. J. Biol. Macromol. 2023, 253 Pt 1, 126510. [Google Scholar] [CrossRef]
- Wang, Q.; Li, M.; Cui, T.; Wu, R.; Guo, F.; Fu, M.; Zhu, Y.; Yang, C.; Chen, B.; Sun, G. A Novel Zwitterionic Hydrogel Incorporated with Graphene Oxide for Bone Tissue Engineering: Synthesis, Characterization, and Promotion of Osteogenic Differentiation of Bone Mesenchymal Stem Cells. Int. J. Mol. Sci. 2023, 24, 2691. [Google Scholar] [CrossRef]
- Fu, M.; Li, J.; Liu, M.; Yang, C.; Wang, Q.; Wang, H.; Chen, B.; Fu, Q.; Sun, G. Sericin/Nano-Hydroxyapatite Hydrogels Based on Graphene Oxide for Effective Bone Regeneration via Immunomodulation and Osteoinduction. Int. J. Nanomed. 2023, 18, 1875–1895. [Google Scholar] [CrossRef]
- Chen, W.-C.; Huang, B.-Y.; Huang, S.-M.; Liu, S.-M.; Chang, K.-C.; Ko, C.-L.; Lin, C.-L. In vitro evaluation of electrospun polyvinylidene fluoride hybrid nanoparticles as direct piezoelectric membranes for guided bone regeneration. Mater. Sci. Eng. C 2023, 144, 213228. [Google Scholar] [CrossRef] [PubMed]
- Seonwoo, H.; Choung, H.-W.; Park, S.; Choi, K.S.; Jang, K.-J.; Kim, J.; Lim, K.-T.; Kim, Y.; Garg, P.; Pandey, S.; et al. Reduced graphene oxide-incorporated calcium phosphate cements with pulsed electromagnetic fields for bone regeneration. RSC Adv. 2022, 12, 39. [Google Scholar] [CrossRef]
- Tabatabaee, S.; Baheiraei, N.; Salehnia, M. Fabrication and characterization of PHEMA-gelatin scaffold enriched with graphene oxide for bone tissue engineering. J. Orthop. Surg. Res. 2022, 17, 33. [Google Scholar] [CrossRef] [PubMed]
- Baheti, W.; Lv, S.; Mila; Ma, L.; Amantai, D.; Sun, H.; He, H. Graphene/hydroxyapatite coating deposit on titanium alloys for implant application. J. Appl. Biomater. Func. 2023, 21, 22808000221148104. [Google Scholar] [CrossRef]
- Yuan, B.; Chen, H.; Zhao, R.; Deng, X.; Chen, G.; Yang, X.; Xiao, Z.; Aurora, A.; Iulia, B.A.; Zhang, K.; et al. Construction of a magnesium hydroxide/graphene oxide/hydroxyapatite composite coating on Mg-Ca-Zn-Ag alloy to inhibit bacterial infection and promote bone regeneration. Bioact. Mater. 2022, 18, 354–367. [Google Scholar] [CrossRef]
- San, H.; Paresoglou, M.; Minneboo, M.; van Hengel, I.A.J.; Yilmaz, A.; Gonzalez-Garcia, Y.; Fluit, A.C.; Hagedoorn, P.-L.; Fratila-Apachitei, L.E.; Apachitei, I.; et al. Fighting Antibiotic-Resistant Bacterial Infections by Surface Biofunctionalization of 3D-Printed Porous Titanium Implants with Reduced Graphene Oxide and Silver Nanoparticles. Int. J. Mol. Sci. 2022, 23, 9204. [Google Scholar] [CrossRef]
- Han, X.-Y.; Meng, T.; Ye, J.-X.; Yin, H.-B.; Song, D.-W. Enhanced Antibacterial and Osteogenic Properties of Graphene Oxide Loaded with Berberine on Biomedical Titanium. J. Biomed. Nanotechnol. 2022, 18, 36. [Google Scholar] [CrossRef]
- Long, X.; Duan, L.; Weng, W.; Cheng, K.; Wang, D.; Ouyang, H. Light-induced osteogenic differentiation of BMSCs with graphene/TiO2 composite coating on Ti implant. Colloids Surf. B Biointerfaces 2021, 207, 49. [Google Scholar] [CrossRef]
- Guo, C.; Lu, R.; Wang, X.; Chen, S. Antibacterial activity, bio-compatibility and osteogenic differentiation of graphene oxide coating on 3D-network poly-ether-ether-ketone for orthopaedic implants. J. Mater. Sci. Mater. Med. 2021, 32, 50. [Google Scholar] [CrossRef]
- Fu, C.; Jiang, Y.; Yang, X.; Wang, Y.; Ji, W.; Jia, G. Mussel-Inspired Gold Nanoparticle and PLGA/L-Lysine-g-Graphene Oxide Composite Scaffolds for Bone Defect Repair. Int. J. Nanomed. 2021, 16, 6693–6718. [Google Scholar] [CrossRef]
- He, Y.; Zhao, Y.; Fan, L.; Wang, X.; Duan, M.; Wang, H.; Zhu, X.; Liu, J. Injectable Affinity and Remote Magnetothermal Effects of Bi-Based Alloy for Long-Term Bone Defect Repair and Analgesia. Adv. Sci. 2021, 8, e2100719. [Google Scholar] [CrossRef]
- Fei, F.; Yao, H.; Wang, Y.; Wei, J. Graphene Oxide/RhPTH(1-34)/Polylactide Composite Nanofibrous Scaffold for Bone Tissue Engineering. Int. J. Mol. Sci. 2023, 24, 5799. [Google Scholar] [CrossRef]
- Huang, Y.; Deng, H.; Fan, Y.; Zheng, L.; Che, J.; Li, X.; Aifantis, K.E. Conductive nanostructured Si biomaterials enhance osteogeneration through electrical stimulation. Mater. Sci. Eng. C 2019, 103, 109748. [Google Scholar] [CrossRef]
- Shen, J.; Sun, D.; Fu, J.; Wang, S.; Wang, X.; Xie, Z. Management of surgical site infection post-open reduction and internal fixation for tibial plateau fractures. Bone Jt. Res. 2021, 10, 380–387. [Google Scholar] [CrossRef]
- Medda, S.; Hsu, J.R. Simplified Antibiotic-Coated Plating for Infected Nonunion, Fracture-Related Infection, and Single-Stage Prophylactic Fixation. J. Orthop. Trauma. 2022, 36, e255–e259. [Google Scholar] [CrossRef]
- Li, J.; Wong, R.M.Y.; Chung, Y.L.; Leung, S.S.Y.; Chow, S.K.-H.; Ip, M.; Cheung, W.-H. Fracture-related infection in osteoporotic bone causes more severe infection and further delays healing. Bone Jt. Res. 2022, 11, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Man, K.-W.; Li, G.H.-Y.; Tan, K.C.; Kung, A.W.-C.; Cheung, C.-L. Osteoporosis is a novel risk factor of infections and sepsis: A cohort study. EClinicalMedicine 2022, 49, 101488. [Google Scholar] [CrossRef] [PubMed]
- Tomizawa, T.; Nishitani, K.; Ito, H.; Okae, Y.; Morita, Y.; Doi, K.; Saito, M.; Ishie, S.; Yoshida, S.; Murata, K.; et al. The limitations of mono- and combination antibiotic therapies on immature biofilms in a murine model of implant-associated osteomyelitis. J. Orthop. Res. 2021, 39, 449–457. [Google Scholar] [CrossRef]
- Masters, E.A.; Ricciardi, B.F.; Bentley, K.L.d.M.; Moriarty, T.F.; Schwarz, E.M.; Muthukrishnan, G. Skeletal infections: Microbial pathogenesis, immunity and clinical management. Nat. Rev. Microbiol. 2022, 20, 385–400. [Google Scholar] [CrossRef]
- Davies, D. Understanding biofilm resistance to antibacterial agents. Nat. Rev. Drug Discov. 2003, 2, 114–122. [Google Scholar] [CrossRef]
- Keller, D.M.; Pizzo, R.A.; Patel, J.N.; Viola, A.; Yoon, R.S.; Liporace, F.A. Use of antibiotic-cement coated locking plates in the setting of periprosthetic infection and infected nonunion. Injury 2022, 53, 2567–2572. [Google Scholar] [CrossRef]
- Zou, X.; Zhang, L.; Wang, Z.; Luo, Y. Mechanisms of the Antimicrobial Activities of Graphene Materials. J. Am. Chem. Soc. 2016, 138, 2064–2077. [Google Scholar] [CrossRef]
- Agarwalla, S.V.; Ellepola, K.; Silikas, N.; Castro Neto, A.H.; Seneviratne, C.J.; Rosa, V. Persistent inhibition of Candida albicans biofilm and hyphae growth on titanium by graphene nanocoating. Dent. Mater. 2021, 37, 370–377. [Google Scholar] [CrossRef]
- Song, S.; Guo, Y.; Yang, Y.; Fu, D. Advances in pathogenesis and therapeutic strategies for osteoporosis. Pharmacol. Therapeut 2022, 237, 108168. [Google Scholar] [CrossRef]
- Black, D.M.; Rosen, C.J. Clinical Practice. Postmenopausal Osteoporosis. N. Engl. J. Med. 2016, 374, 254–262. [Google Scholar] [CrossRef]
- Buckley, L.; Humphrey, M.B. Glucocorticoid-Induced Osteoporosis. N. Engl. J. Med. 2018, 379, 2547–2556. [Google Scholar] [CrossRef]
- McDonald, M.M.; Khoo, W.H.; Ng, P.Y.; Xiao, Y.; Zamerli, J.; Thatcher, P.; Kyaw, W.; Pathmanandavel, K.; Grootveld, A.K.; Moran, I.; et al. Osteoclasts recycle via osteomorphs during RANKL-stimulated bone resorption. Cell 2021, 184, 1330–1347. [Google Scholar] [CrossRef]
- Kim, T.-H.; Yang, K.; Kim, M.; Kim, H.-S.; Kang, J.L. Apoptosis inhibitor of macrophage (AIM) contributes to IL-10-induced anti-inflammatory response through inhibition of inflammasome activation. Cell Death Dis. 2021, 12, 19. [Google Scholar] [CrossRef]
- Sinder, B.P.; Pettit, A.R.; McCauley, L.K. Macrophages: Their Emerging Roles in Bone. J. Bone Miner. Res. 2015, 30, 2140–2149. [Google Scholar] [CrossRef]
- Schlundt, C.; Fischer, H.; Bucher, C.H.; Rendenbach, C.; Duda, G.N.; Schmidt-Bleek, K. The multifaceted roles of macrophages in bone regeneration: A story of polarization, activation and time. Acta Biomater. 2021, 133, 46–57. [Google Scholar] [CrossRef]
- Xue, D.; Chen, E.; Zhong, H.; Zhang, W.; Wang, S.; Joomun, M.U.; Yao, T.; Tan, Y.; Lin, S.; Zheng, Q.; et al. Immunomodulatory properties of graphene oxide for osteogenesis and angiogenesis. Int. J. Nanomed. 2018, 13, 5799–5810. [Google Scholar] [CrossRef]
- Xue, H.; Zhang, Z.; Lin, Z.; Su, J.; Panayi, A.C.; Xiong, Y.; Hu, L.; Hu, Y.; Chen, L.; Yan, C.; et al. Enhanced tissue regeneration through immunomodulation of angiogenesis and osteogenesis with a multifaceted nanohybrid modified bioactive scaffold. Bioact. Mater. 2022, 18, 552–568. [Google Scholar] [CrossRef] [PubMed]
- Karimi Shervedani, R.; Mirhosseini, H.; Samiei Foroushani, M.; Torabi, M.; Rahsepar, F.R.; Norouzi-Barough, L. Immobilization of methotrexate anticancer drug onto the graphene surface and interaction with calf thymus DNA and 4T1 cancer cells. Bioelectrochemistry 2018, 119, 1–9. [Google Scholar] [CrossRef] [PubMed]
- D’Amora, U.; Dacrory, S.; Hasanin, M.S.; Longo, A.; Soriente, A.; Kamel, S.; Raucci, M.G.; Ambrosio, L.; Scialla, S. Advances in the Physico-Chemical, Antimicrobial and Angiogenic Properties of Graphene-Oxide/Cellulose Nanocomposites for Wound Healing. Pharmaceutics 2023, 15, 338. [Google Scholar] [CrossRef]
- Wu, X.; Li, H.; Xiao, N. Advancement of Near-infrared (NIR) laser interceded surface enactment of proline functionalized graphene oxide with silver nanoparticles for proficient antibacterial, antifungal and wound recuperating therapy in nursing care in hospitals. J. Photochem. Photobiol. B 2018, 187, 89–95. [Google Scholar] [CrossRef]
- Cao, L.; Liu, G.; Gan, Y.; Fan, Q.; Yang, F.; Zhang, X.; Tang, T.; Dai, K. The use of autologous enriched bone marrow MSCs to enhance osteoporotic bone defect repair in long-term estrogen deficient goats. Biomaterials 2012, 33, 5076–5084. [Google Scholar] [CrossRef]
- Roche, B.; Vanden-Bossche, A.; Malaval, L.; Normand, M.; Jannot, M.; Chaux, R.; Vico, L.; Lafage-Proust, M.-H. Parathyroid hormone 1-84 targets bone vascular structure and perfusion in mice: Impacts of its administration regimen and of ovariectomy. J. Bone Miner. Res. 2014, 29, 1608–1618. [Google Scholar] [CrossRef]
- Bai, Z.; Wei, J.; Yu, C.; Han, X.; Qin, X.; Zhang, C.; Liao, W.; Li, L.; Huang, W. Non-viral nanocarriers for intracellular delivery of microRNA therapeutics. J. Mater. Chem. B 2019, 7, 1209–1225. [Google Scholar] [CrossRef]
- Zeng, Y.; Zhou, M.; Chen, L.; Fang, H.; Liu, S.; Zhou, C.; Sun, J.; Wang, Z. Alendronate loaded graphene oxide functionalized collagen sponge for the dual effects of osteogenesis and anti-osteoclastogenesis in osteoporotic rats. Bioact. Mater. 2020, 5, 60. [Google Scholar] [CrossRef]
- Qin, H.; Ji, Y.; Li, G.; Xu, X.; Zhang, C.; Zhong, W.; Xu, S.; Yin, Y.; Song, J. MicroRNA-29b/graphene oxide-polyethyleneglycol-polyethylenimine complex incorporated within chitosan hydrogel promotes osteogenesis. Front. Chem. 2022, 10, 43. [Google Scholar] [CrossRef]
- Yu, K.; Huangfu, H.; Qin, Q.; Zhang, Y.; Gu, X.; Liu, X.; Zhang, Y.; Zhou, Y. Application of Bone Marrow-Derived Macrophages Combined with Bone Mesenchymal Stem Cells in Dual-Channel Three-Dimensional Bioprinting Scaffolds for Early Immune Regulation and Osteogenic Induction in Rat Calvarial Defects. ACS Appl. Mater. Interfaces 2022, 14, 47052–47065. [Google Scholar] [CrossRef] [PubMed]
- Wank, I.; Niedermair, T.; Kronenberg, D.; Stange, R.; Brochhausen, C.; Hess, A.; Grässel, S. Influence of the Peripheral Nervous System on Murine Osteoporotic Fracture Healing and Fracture-Induced Hyperalgesia. Int. J. Mol. Sci. 2022, 24, 510. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, H.; Zhang, Y.; Huangfu, H.; Yang, Y.; Qin, Q.; Zhang, Y.; Zhou, Y. 3D printed reduced graphene oxide-GelMA hybrid hydrogel scaffolds for potential neuralized bone regeneration. J. Mater. Chem. B 2023, 11, 1288–1301. [Google Scholar] [CrossRef]
- Rostami, F.; Tamjid, E.; Behmanesh, M. Drug-eluting PCL/graphene oxide nanocomposite scaffolds for enhanced osteogenic differentiation of mesenchymal stem cells. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 115, 63. [Google Scholar] [CrossRef]
- Wu, M.; Zou, L.; Jiang, L.; Zhao, Z.; Liu, J. Osteoinductive and antimicrobial mechanisms of graphene-based materials for enhancing bone tissue engineering. J. Tissue Eng. Regen. M. 2021, 15, 47. [Google Scholar] [CrossRef]
- Chen, Z.; Klein, T.; Murray, R.Z.; Crawford, R.; Chang, J.; Wu, C.; Xiao, Y. Osteoimmunomodulation for the development of advanced bone biomaterials. Mater. Today 2016, 19, 304–321. [Google Scholar] [CrossRef]
- He, Y.; Li, Y.; Chen, G.; Wei, C.; Zhang, X.; Zeng, B.; Yi, C.; Wang, C.; Yu, D. Concentration-dependent cellular behavior and osteogenic differentiation effect induced in bone marrow mesenchymal stem cells treated with magnetic graphene oxide. J. Biomed. Mater. Res. A 2020, 108, 79. [Google Scholar] [CrossRef]
- Xu, D.; Wang, C.; Wu, J.; Fu, Y.; Li, S.; Hou, W.; Lin, L.; Li, P.; Yu, D.; Zhao, W. Effects of Low-Concentration Graphene Oxide Quantum Dots on Improving the Proliferation and Differentiation Ability of Bone Marrow Mesenchymal Stem Cells through the Wnt/β-Catenin Signaling Pathway. ACS Omega 2022, 7, 32. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhao, Q.; Chen, J.; Liu, J.; Lin, J.; Lu, J.; Li, W.; Yu, D.; Zhao, W. Graphene Oxide Quantum Dots Promote Osteogenic Differentiation of Stem Cells from Human Exfoliated Deciduous Teeth via the Wnt/β-Catenin Signaling Pathway. Stem Cells Int. 2021, 2021, 58. [Google Scholar] [CrossRef]
- Zhao, M.; Dai, Y.; Li, X.; Li, Y.; Zhang, Y.; Wu, H.; Wen, Z.; Dai, C. Evaluation of long-term biocompatibility and osteogenic differentiation of graphene nanosheet doped calcium phosphate-chitosan AZ91D composites. Mater. Sci. Eng. C Mater. Biol. Appl. 2018, 90, 365–378. [Google Scholar] [CrossRef]
- Chen, Y.; Zheng, Z.; Zhou, R.; Zhang, H.; Chen, C.; Xiong, Z.; Liu, K.; Wang, X. Developing a Strontium-Releasing Graphene Oxide-/Collagen-Based Organic-Inorganic Nanobiocomposite for Large Bone Defect Regeneration via MAPK Signaling Pathway. ACS Appl. Mater. Interfaces 2019, 11, 98. [Google Scholar] [CrossRef]
- Zhang, W.; Chang, Q.; Xu, L.; Li, G.; Yang, G.; Ding, X.; Wang, X.; Cui, D.; Jiang, X. Graphene Oxide-Copper Nanocomposite-Coated Porous CaP Scaffold for Vascularized Bone Regeneration via Activation of Hif-1α. Adv. Healthc. Mater. 2016, 5, 1299–1309. [Google Scholar] [CrossRef]
- Shim, N.Y.; Heo, J.S. Performance of the Polydopamine-Graphene Oxide Composite Substrate in the Osteogenic Differentiation of Mouse Embryonic Stem Cells. Int. J. Mol. Sci. 2021, 22, 54. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Gao, R.; Rong, X.; Zhu, S.; Cui, Y.; Liu, H.; Li, M. Immunoporosis: Role of immune system in the pathophysiology of different types of osteoporosis. Front. Endocrinol. 2022, 13, 965258. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Liang, H.; Liu, X.; Wu, J.; Yang, C.; Wong, T.M.; Kwan, K.Y.H.; Cheung, K.M.C.; Wu, S.; Yeung, K.W.K. Regulation of macrophage polarization through surface topography design to facilitate implant-to-bone osteointegration. Sci. Adv. 2021, 7, eabf6654. [Google Scholar] [CrossRef]
- Franz, S.; Rammelt, S.; Scharnweber, D.; Simon, J.C. Immune responses to implants—A review of the implications for the design of immunomodulatory biomaterials. Biomaterials 2011, 32, 6692–6709. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Gaihre, B.; Park, S.; Li, L.; Dashtdar, B.; Astudillo Potes, M.D.; Terzic, A.; Elder, B.D.; Lu, L. 3D-printed scaffolds with 2D hetero-nanostructures and immunomodulatory cytokines provide pro-healing microenvironment for enhanced bone regeneration. Bioact. Mater. 2023, 27, 216–230. [Google Scholar] [CrossRef]
- Lv, B.; Wu, J.; Xiong, Y.; Xie, X.; Lin, Z.; Mi, B.; Liu, G. Functionalized multidimensional biomaterials for bone microenvironment engineering applications: Focus on osteoimmunomodulation. Front. Bioeng. Biotech. 2022, 10, 1023231. [Google Scholar] [CrossRef]
- Su, J.; Du, Z.; Xiao, L.; Wei, F.; Yang, Y.; Li, M.; Qiu, Y.; Liu, J.; Chen, J.; Xiao, Y. Graphene oxide coated Titanium Surfaces with Osteoimmunomodulatory Role to Enhance Osteogenesis. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 113, 66. [Google Scholar] [CrossRef]
- Zhou, J.; Li, Y.; He, J.; Liu, L.; Hu, S.; Guo, M.; Liu, T.; Liu, J.; Wang, J.; Guo, B.; et al. ROS Scavenging Graphene-Based Hydrogel Enhances Type H Vessel Formation and Vascularized Bone Regeneration via ZEB1/Notch1 Mediation. Macromol. Biosci. 2023, 23, e2200502. [Google Scholar] [CrossRef]
- Chen, M.; Yin, J.; Liang, Y.; Yuan, S.; Wang, F.; Song, M.; Wang, H. Oxidative stress and immunotoxicity induced by graphene oxide in zebrafish. Aquat. Toxicol. 2016, 174, 54–60. [Google Scholar] [CrossRef]
- Liu, S.; Xu, A.; Gao, Y.; Xie, Y.; Liu, Z.; Sun, M.; Mao, H.; Wang, X. Graphene oxide exacerbates dextran sodium sulfate-induced colitis via ROS/AMPK/p53 signaling to mediate apoptosis. J. Nanobiotechnol. 2021, 19, 85. [Google Scholar] [CrossRef]
- Mrózek, O.; Melounková, L.; Smržová, D.; Machálková, A.; Vinklárek, J.; Němečková, Z.; Komárková, B.; Ecorchard, P. Salt-washed graphene oxide and its cytotoxicity. J. Hazard. Mater. 2020, 398, 123114. [Google Scholar] [CrossRef]
- Syama, S.; Mohanan, P.V. Safety and biocompatibility of graphene: A new generation nanomaterial for biomedical application. Int. J. Biol. Macromol. 2016, 86, 546–555. [Google Scholar] [CrossRef]
- Xu, M.; Zhu, J.; Wang, F.; Xiong, Y.; Wu, Y.; Wang, Q.; Weng, J.; Zhang, Z.; Chen, W.; Liu, S. Improved In Vitro and In Vivo Biocompatibility of Graphene Oxide through Surface Modification: Poly(Acrylic Acid)-Functionalization is Superior to PEGylation. ACS Nano 2016, 10, 3267–3281. [Google Scholar] [CrossRef] [PubMed]
- Pelin, M.; Fusco, L.; León, V.; Martín, C.; Criado, A.; Sosa, S.; Vázquez, E.; Tubaro, A.; Prato, M. Differential cytotoxic effects of graphene and graphene oxide on skin keratinocytes. Sci. Rep. 2017, 7, 40572. [Google Scholar] [CrossRef] [PubMed]
- Duan, G.; Zhang, Y.; Luan, B.; Weber, J.K.; Zhou, R.W.; Yang, Z.; Zhao, L.; Xu, J.; Luo, J.; Zhou, R. Graphene-Induced Pore Formation on Cell Membranes. Sci. Rep. 2017, 7, 42767. [Google Scholar] [CrossRef] [PubMed]
- McCallion, C.; Burthem, J.; Rees-Unwin, K.; Golovanov, A.; Pluen, A. Graphene in therapeutics delivery: Problems, solutions and future opportunities. Eur. J. Pharm. Biopharm. 2016, 104, 235–250. [Google Scholar] [CrossRef]


| Type | Name | Compose | Animal Species | Cytotoxicity Tests | Biocompatibility | Conclusion | Reference |
|---|---|---|---|---|---|---|---|
| Scaffold | PP/GO@PEGDA/CMC | GO, Pyritum, Polydiacrylate, Carboxymethyl chitosan | SD rats with bilateral skull defect model | Non-toxic to macrophages | Induced macrophage polarizes to M2 phenotype | It has both immunomodulatory and osteoinductive properties | [38] |
| PLA-HT-GO | Polylactic acid, Hardystonite, GO | NA | Non-toxic to MG63 | Enhanced the proliferation and adhesion of MG63 | HT-GO nanoparticles improved the mechanical properties and osteoinductive properties | [39] | |
| Z-CS/β-TCP/GO | GO, Maleicanhydride, L-cysteine, Maleilated chitosan | SD rats with bilateral skull defect model | Non-toxic to BMSCs | Enhanced the proliferation and adhesion of BMSCs | GO improved physicochemical properties and osteogenic differentiation of rBMSCs | [40] | |
| Alg/GO/Ser/nHAP | Alginate, GO, Sericin, Nanohydroxyapatite | SD rats with bilateral skull defect | Non-toxic to BMSCs | 1. Induced macrophage polarizes to M2 phenotype 2. Enhanced the proliferation and adhesion of BMSCS | It has both immunomodulatory and osteoinductive properties | [41] | |
| GO-PVDF | GO, Polyvinylidene fluoride | NA | Non-toxic to osteoprogenitor D1 cells | Enhanced the proliferation and mineralization of osteoprogenitor D1 cells | Exhibits excellent tensile and piezoelectric properties, high flexibility, and good biocompatibility | [42] | |
| RGO-CPCs | RGO, Calcium phosphate cements | SD rats with bilateral skull defect model | Slight toxicity at 12 h and became marginal at 24 h to MC3T3-E1 and rASCs | Improved osteogenic differentiation of MC3T3-E1 and rASCs | The mechanical properties and the bone-inducing activity of the rGO-CPCs were enhanced in comparison with CPCs | [43] | |
| PHEMA-Gel-GO | Poly(2-hydroxyethyl methacrylate), Geltain, GO | NA | Non-toxic to BMSCs | Enhanced the proliferation and adhesion of BMSCs | Mechanical properties, electroactivity, and osteogenic differentiation ability can be improved through the GO | [44] | |
| Coating | HA-GO-Ti | Hydroxyapatite, GO, Ti | SD rats with distal femurs defect model | Non-toxic to BMSCs | Enhanced the proliferation and adhesion of BMSCs | HA-GO nanocoating improve the osteogenesis of the Ti | [45] |
| Mg(OH)2/GO/HA-ZQ71 | Mg(OH)2, GO, Hydroxyapatite, ZQ71 alloy | NA | Non-toxic to MC3T3-E1 | Enhanced the proliferation and adhesion of MC3T3-E1 | Mg(OH)2/GO/HA composite coating improved the corrosion resistance and osteogenesis and reduced the degradation rate | [46] | |
| Ag-RGO-Ti | Ag, rGO, Ti | NA | Non-toxic to MC3T3-E1 | Enhanced the proliferation and adhesion of MC3T3-E1 | RGO+Ag coating improved the antibacterial activity and osteogenesis of Ti | [47] | |
| Berberine-GO-Ti | Berberine, GO, Ti | SD rats with distal femurs defect model | Non-toxic to MC3T3-E1 | Enhanced the proliferation and adhesion of MC3T3-E1 | Berberine-loaded GO coating improved the antibacterial activity and osteogenesis of Ti | [48] | |
| GO/TiO2/Ti | GO, TiO2, Ti | NA | Non-toxic to BMSCs | Enhanced the adhesion of BMSCs | The rGO/TiO2 has good biocompatibility and light-induced surface potential and could promote BMSC osteogenic differentiation | [49] | |
| SPEEK-GO | GO, Poly-ether-ether-ketone, 98% sulfuric acid | NA | Non-toxic to MC3T3-E1 | Enhanced the proliferation and adhesion of MC3T3-E1 | The SPEEK-GO coating exhibits strong antibacterial properties and excellent cell compatibility | [50] | |
| AuNPs-PDA@PLGA/Lys-g-GO | L-lysine functionalized-GO, Polydopamine, Au, PLGA | Rabbits with radius defects | Non-toxic to MC3T3-E1 | Enhanced the proliferation and adhesion of MC3T3-E1 | Lys-g-GO nanoparticles and AuNPs-PDA coating enhanced the hydrophilicity, mechanical properties, and antibacterial properties, resulting in good osteogenic activity. | [51] |
| Name | Compose | Animal Species | Cytotoxicity Tests | Biocompatibility | Conclusion | Reference |
|---|---|---|---|---|---|---|
| PCL/GO-DEX | Polycaprolactone, GO, Dexamethasone | NA | Non-toxic to BMSCs | Enhanced the proliferation and adhesion of BMSCs | The synergistic effect of GO and dexamethasone induce osteogenesis of BMSCs | [85] |
| Aln-GO-Col | Alendronate, Collagen, GO | SDrats with bilateral skull defect model | Toxic to BMSCs at high concentration of GO | 1. Enhanced the proliferation and adhesion of BMSCs 2. Inhibited osteoclast differentiation | Exhibited active anti-osteoclastogenesis and osteogenesis ability | [80] |
| PLA/GO/RhPTH(1-34) | Polylactide, GO, RhPTH(1-34) | NA | Non-toxic to MC3T3-E1 | Enhanced the proliferation and adhesion of MC3T3-E1 | Mechanical properties and osteogenic differentiation ability can be improved through the scaffolds | [53] |
| miR-29b/GO-PEG-PEI@CS | GO, Polyethyleneglycol, Polyethylenimine, miR-29b, Chitosan | SD rats with bilateral skull defect model | Non-toxic to BMSCs | Enhanced the proliferation and adhesion of BMSCs | It can promote bone regeneration without inflammatory responses | [81] |
| BMSCS/SCS/rGO/GelMA | BMSCs, SCs, rGO, GelMA | SD rats with bilateral skull defect model | Non-toxic to BMSCs and SCs | Enhanced the proliferation and adhesion of BMSCs and SCs | It can promote synergistic regeneration of nerves and bone | [84] |
| BMSCS/BMMS/GelMA/HAMA/Alginate/GO | BMSCS, BMMS, Methacrylamidated gelatin, Methacrylamidated Hyaluronic, Alginate | Rat subcutaneous transplantation model | Non-toxic to BMSCs | 1.Induced macrophage polarizes to M2 phenotype 2.Enhanced the proliferation and adhesion of BMSCs | The paracrine of BMMs and BMSCs effectively promoted the M2-type polarization and bone repair. | [82] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, H.; Chen, J.; Zhang, X.; Chen, J.; Chen, J.; Jia, S.; Wang, D.; Zeng, H.; Weng, J.; Yu, F. Exploring the Application of Graphene Oxide-Based Nanomaterials in the Repair of Osteoporotic Fractures. Nanomaterials 2024, 14, 553. https://doi.org/10.3390/nano14060553
Zhou H, Chen J, Zhang X, Chen J, Chen J, Jia S, Wang D, Zeng H, Weng J, Yu F. Exploring the Application of Graphene Oxide-Based Nanomaterials in the Repair of Osteoporotic Fractures. Nanomaterials. 2024; 14(6):553. https://doi.org/10.3390/nano14060553
Chicago/Turabian StyleZhou, Hongfa, Jinyuan Chen, Xuan Zhang, JingJing Chen, Jiayou Chen, Shicheng Jia, Deli Wang, Hui Zeng, Jian Weng, and Fei Yu. 2024. "Exploring the Application of Graphene Oxide-Based Nanomaterials in the Repair of Osteoporotic Fractures" Nanomaterials 14, no. 6: 553. https://doi.org/10.3390/nano14060553





