Optimising Interventions for Catheter-Associated Urinary Tract Infections (CAUTI) in Primary, Secondary and Care Home Settings
Abstract
:1. Introduction
- The Health and Social Care Act 2008 Code of Practice on the prevention and control of infections and related guidance (HSC Act 2008)—Guidelines for primary, secondary and community setting
- NICE QS90: Urinary Tract Infections in Adults (NICE QS90)—Guidelines for community setting
- NICE QS61: Infection prevention and control (NICE QS61)—Guidelines for primary, secondary and community setting
- NICE catheter audit tools—tools to help implementation of the clinical guidelines for primary and community setting
- Department of Health and Public Health England (2013): Prevention and control of infections in care homes: an informative resource (DH PHE 2013)—Guidelines for care homes
- Safety thermometer—a tool for HCP in primary, secondary, community and care homes setting
- Epic 3—guidelines for preventing healthcare-associated infections in acute settings
- High Impact Intervention for best practice insertion and care (High Impact)—intervention tools for community and secondary care setting
- Catheter Care: Royal College of Nursing Guidance for nurses (Catheter Care)—guidelines for nurses in primary, community, secondary and nursing homes setting
- HOUDINI Protocol (HOUDINI)—a nurse-led catheter removal protocol for secondary care
- Catheter Passport—document to be completed by both patients and HCPs to consistently manage and remove catheters for primary, community and nursing homes setting
- (1)
- Which interventions, targeting HCP behaviours, are effective at reducing incidence of CAUTI?
- (2)
- What is the content of interventions shown to be effective in research studies in comparison to national interventions?
- (3)
- To what extent are key influences on HCP behaviour addressed by effective interventions in comparison to national interventions?
- (4)
- How can we better address key influences on HCP behaviour?
2. Results
2.1. Rapid Review
2.2. Behavioural Analysis of Intervention Content
Intervention Content Matched against Key Influences on Behaviour
2.3. Stakeholder Feedback
2.4. Survey
3. Discussion
3.1. Implications for Existing CAUTI Interventions
3.2. Optimising National Interventions
3.3. Strengths and Limitations
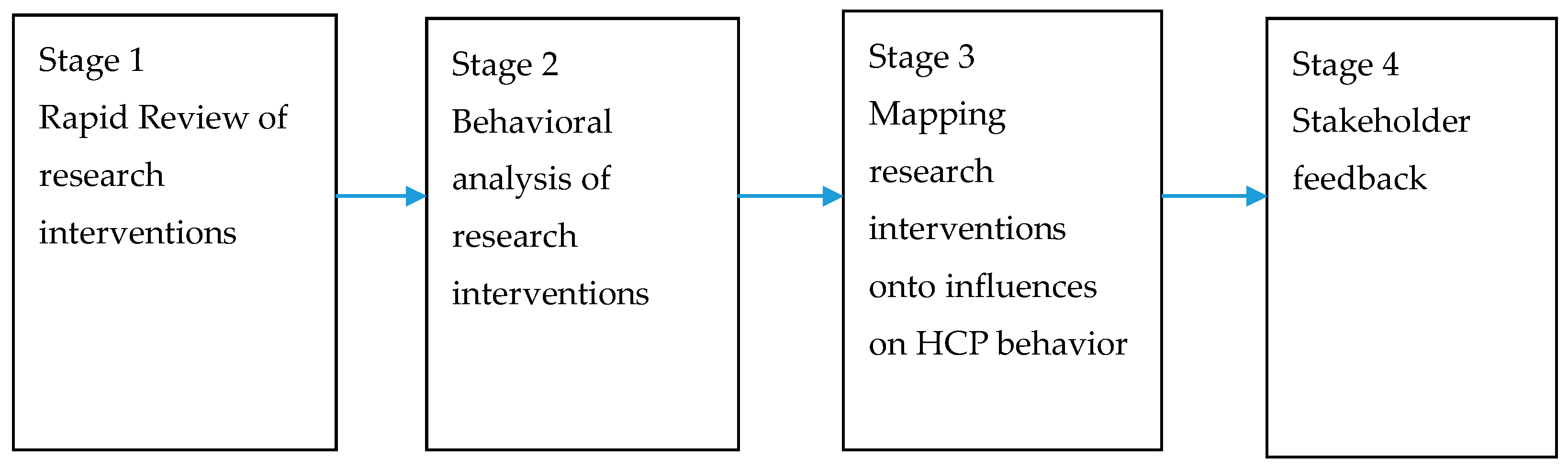
4. Materials and Methods
4.1. Rapid Review to Identify Effective Research Interventions
4.2. Behavioural Analysis of Research Interventions in Comparison to National Interventions
4.3. Assessing the Behavioural Content of Research Interventions against Key Influences on Healthcare Professional Behaviours
4.4. Stakeholder Feedback Using a Focus Group and Survey
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Health Protection Agency. English National Point Prevalence Survey on Healthcare-Associated Infections and Antimicrobial Use, 2011: Preliminary Data; HPA: London, UK, 2012. [Google Scholar]
- Codd, J. Implementation of a patient-held urinary catheter passport to improve catheter management, by prompting for early removal and enhancing patient compliance. J. Infect. Prev. 2014, 15, 88–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meddings, J.; Rogers, M.; Krein, S.L.; Fakih, M.G.; Olmsted, R.N.; Saint, S. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: An integrative review. BMJ Qual. Saf. 2014, 23, 277–289. [Google Scholar] [CrossRef]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel: A Guide to Designing Interventions, 1st ed.; Silverback Publishing: Surrey, UK, 2014. [Google Scholar]
- Atkins, L.; Sallis, A.; Chadborn, T.; Shaw, K.; Schneider, A.; Hopkins, S.; Bunten, A.; Michie, S.; Lorencatto, F. Reducing catheter associated urinary tract infections: A systematic review of barriers and facilitators and strategic behavioural analysis of interventions. Implement. Sci. 2020, 15, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.M.; Alaestante, G.; Finch, C. A multidisciplinary intervention to prevent catheter-associated urinary tract infections using education, continuum of care, and systemwide buy-in. Ochsner J. 2016, 16, 96–100. [Google Scholar]
- Carr, A.N. CAUTI prevention: Streaming quality care in a progressive care unit. Med. Surg. Nurs. 2017, 26, 306–310. [Google Scholar]
- Cartwright, A. Reducing catheter-associated urinary tract infections: Standardising practice. Br. J. Nurs. 2018, 27, 7–12. [Google Scholar] [CrossRef]
- Cho, H.J.; Khalil, S.; Poeran, J.; Mazumdar, M.; Bravo, N.; Wallach, F.; Markoff, B.; Lee, N.; Dunn, A.S. “Lose the Tube”: A Choosing Wisely initiative to reduce catheter-associated urinary tract infections in hospitalist-led inpatient units. Am. J. Infect. Control 2017, 45, 333–335. [Google Scholar] [CrossRef] [PubMed]
- Davies, P.E.; Daley, M.J.; Hecht, J.; Hobbs, A.; Burger, C.; Watkins, L.; Murray, T.; Shea, K.; Ali, S.; Brown, L.H.; et al. Effectiveness of a bundled approach to reduce urinary catheters and infection rates in trauma patients. Am. J. Infect. Control 2018, 46, 758–763. [Google Scholar] [CrossRef]
- Dawson, C.H.; Gallo, M.; Prevc, K. TWOC around the clock: A multimodal approach to improving catheter care. J. Infect. Prev. 2017, 18, 57–64. [Google Scholar] [CrossRef]
- Dy, S.; Major-Joynes, B.; Pegues, D.; Bradway, C. A nurse-driven protocol for removal of indwelling urinary catheters across a multi-hospital academic healthcare system. Urol. Nurs. 2016, 36, 243. [Google Scholar] [CrossRef]
- Halperin, J.J.; Moran, S.; Prasek, D.; Richards, A.; Ruggiero, C.; Maund, C. Reducing Hospital-Acquired Infections Among the Neurologically Critically Ill. Neurocrit. Care 2016, 25, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.; Gilman, A.; Lintner, A.; Buckner, E. Nurse-Driven Catheter-Associated Urinary Tract Infection Reduction Process and Protocol: Development Through an Academic-Practice Partnership. Crit. Care Nurs. Q. 2016, 39, 352–362. [Google Scholar] [CrossRef]
- Kachare, S.D.; Sanders, C.; Myatt, K.; Fitzgerald, T.L.; Zervos, E.E. Toward eliminating catheter-associated urinary tract infections in an academic health center. J. Surg. Res. 2014, 192, 280–285. [Google Scholar] [CrossRef]
- Maxwell, M. Changing ICU culture to reducecatheter-associated urinary tract infections. Infect. Control 2018, 33, 39–43. [Google Scholar]
- McCalla, S.; Reilly, M.; Thomas, R.; McSpedon-Rai, D.; McMahon, L.A. PalumboAn automated hand hygiene compliance system is associated with decreased rates of health care-associated infections. Am. J. Infect. Control 2018, 46, 1381–1386. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.; Briody, C.; Casey, D.; Kane, J.K.; Mitchell, D.; Patel, B.; Ritter, C.; Seckel, M.; Wakai, S.; Drees, M. Using the Comprehensive Unit-based Safety Program model for sustained reduction in hospital infections. Am. J. Infect. Control 2016, 44, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Mody, L.; Greene, M.T.; Meddings, J.; Krein, S.L.; McNamara, S.E.; Trautner, B.W.; Ratz, D.; Stone, N.D.; Min, L.; Schweon, S.J.; et al. A National Implementation Project to Prevent Catheter-Associated Urinary Tract Infection in Nursing Home Residents. JAMA Intern. Med. 2017, 177, 1154–1162. [Google Scholar] [CrossRef]
- Mody, L.; Krein, S.L.; Saint, S.; Min, L.C.; Montoya, A.; Lansing, B.; McNamara, S.E.; Symons, K.; Fisch, J.; Koo, E.; et al. A targeted infection prevention intervention in nursing home residents with indwelling devices: A randomized clinical trial. JAMA Intern. Med. 2015, 175, 714–723. [Google Scholar] [CrossRef]
- Mori, C. A-voiding catastrophe: Implementing a nurse-driven protocol. Medsurg Nurs. 2014, 23, 15–21. [Google Scholar]
- Mullin, K.M. A Multifaceted Approach to Reduction of Catheter-Associated Urinary Tract Infections in the Innsive Care Unit with an Emphasis on “Stewardship of Culturing”. Infect. Control Hosp. Epidemiol. 2017, 38, 186–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nealon, S.W.; Hale, A.L.; Haynes, E.; Hagood-Thompson, C.; Marguet, C.G.; Ewing, J.A.; Springhart, P.W. Improving Patient Outcomes and Health Care Provider Communication with a Small, Yellow Plastic Band: The Patient URinary Catheter Extraction (PURCE) Protocol©. Urol. Pract. 2018, 5, 1–6. [Google Scholar] [CrossRef]
- Pashnik, B.; Creta, A.; Alberti, L. Effectiveness of a Nurse-Led Initiative, Peer-to-Peer Teaching, on Organizational CAUTI Rates and Related Costs. J. Nurs. Care Qual. 2017, 32, 324–330. [Google Scholar] [CrossRef]
- Purvis, S.; Gion, T.; Kennedy, G.; Rees, S.; Safdar, N.; VanDenBergh, S.; Weber, J. Catheter-associated urinary tract infection: A successful prevention effort employing a multipronged initiative at an academic medical center. J. Nurs. Care Qual. 2014, 29, 141–148. [Google Scholar] [CrossRef]
- Purvis, S.; Kennedy, G.D.; Knobloch, M.J.; Marver, A.; Marx, J.; Rees, S.; Safdar, N.; Shirley, D. Incorporation of Leadership Rounds in CAUTI Prevention Efforts. J. Nurs. Care Qual. 2017, 32, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Quinn, P. Chasing Zero: A Nurse-Driven Process For Catheter-Associated Urinary Tract Infection Reduction in a Community Hospital. Nurs. Econ. 2015, 33, 320–325. [Google Scholar] [PubMed]
- Rhee, C.; Phelps, M.E.; Meyer, B.; Reed, W.G. Viewing Prevention of Catheter-Associated Urinary Tract Infection as a System: Using Systems Engineering and Human Factors Engineering in a Quality Improvement Project in an Academic Medical Center. Jt. Comm. J. Qual. Patient Saf. 2016, 42, 447–471. [Google Scholar] [CrossRef]
- Rhone, C.; Breiter, Y.; Benson, L.; Petri, H.; Thompson, P.; Murphy, C. The Impact of Two-Person Indwelling Urinary Catheter Insertion in the Emergency Department Using Technical and Socioadaptive Interventions. J. Clin. Outcomes Manag. 2017, 24. Available online: https://www.mdedge.com/jcomjournal/article/149684/emergency-medicine/impact-two-person-indwelling-urinary-catheter (accessed on 29 June 2020).
- Richards, B.; Sebastian, B.; Sullivan, H.; Reyes, R.; D’Agostino, J.F.; Hagerty, T. TDecreasing Catheter-Associated Urinary Tract Infections in the Neurological Intensive Care Unit: One Unit’s Success. Crit. Care Nurse 2017, 37, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Saint, S.; Greene, M.T.; Krein, S.L.; Rogers, M.A.; Ratz, D.; Fowler, K.E.; Edson, B.S.; Watson, S.R.; Meyer-Lucas, B.; Masuga, M.; et al. A Program to Prevent Catheter-Ass ociated Urinary Tract Infection in Acute Care. N. Engl. J. Med. 2016, 374, 2111–2119. [Google Scholar] [CrossRef]
- Sampathkumar, P.; Barth, J.W.; Johnson, M.; Marosek, N.; Johnson, M.; Worden, W.; Lembke, J.; Twing, H.; Buechler, T.; Dhanorker, S.; et al. Mayo Clinic Reduces Catheter-Associated Urinary Tract Infections Through a Bundled 6-C Approach. Jt. Comm. J. Qual. Patient Saf. 2016, 42, 254–261. [Google Scholar] [PubMed]
- Scanlon, K.; Wells, C.; Woolforde, L.; Khameraj, A.; Baumgarten, J. Saving Lives and Reducing Harm: A CAUTI Reduction Program. Nurs. Econ. 2017, 35, 134–141. [Google Scholar]
- Sutherland, T.; Beloff, J.; McGrath, A. A Single-Center Multidisciplinary Initiative to Reduce Catheter-Associated Urinary Tract Infection Rates: Quality and Financial Implications. Health Care Manag. 2015, 34, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Ternavasio-de la Vega, H.G.; Ventura, A.B.; Castano-Romero, F.; Sauchelli, F.D.; Acosta, A.P.; Alcázar, F.R.; Sánchez, A.V.; Antúnez, E.R.; Marcos, M.; Laso, J. Assessment of a multi-modal intervention for the prevention of catheter-associated urinary tract infections. J. Hosp. Infect. 2016, 94, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.L. Reduction of Catheter-Associated Urinary Tract Infections Through the Use of an Evidence-Based Nursing Algorithm and the Implementation of Shift Nursing Rounds: A Quality Improvement Project. J. Wound Ostomy Cont. Nurs. 2016, 43, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Tuttle, J.C. Cutting CAUTIs in critical care. J. Clin. Outcomes Manag. 2017, 24, 267–272. [Google Scholar]
- Tyson, A.F.; Campbell, E.F.; Spangler, L.R.; Ross, S.W.; Reinke, C.E.; Passaretti, C.L.; Sing, R.F. Implementation of a Nurse-Driven Protocol for Catheter Removal to Decrease Catheter-Associated Urinary Tract Infection Rate in a Surgical Trauma ICU. J. Intensive Care Med. 2018, 35, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Umer, A.; Shapiro, D.S.; Hughes, C.R.; Ross-Richardson, C.; Ellner, S. The Use of an Indwelling Catheter Protocol to Reduce Rates of Postoperative Urinary Tract Infections. Connect. Med. 2016, 80, 197–203. [Google Scholar]
- Youngerman, B.E.; Salmasian, H.; Carter, E.J.; Loftus, M.L.; Perotte, R.; Ross, B.G.; Furuya, E.Y.; Green, R.A.; Vawdrey, D.K. Reducing indwelling urinary catheter use through staged introduction of electronic clinical decision support in a multicenter hospital system. Infect. Control Hosp. Epidemiol. 2018, 39, 902–908. [Google Scholar] [CrossRef]
- Zubkoff, L.; Neily, J.; Quigley, P.; Soncrant, C.; Young-Xu, Y.; Boar, S.; Mills, P.D. Virtual Breakthrough Series, Part 2: Improving Fall Prevention Practices in the Veterans Health Administration. Jt. Comm. J. Qual. Patient Saf. 2016, 42, 497–505. [Google Scholar] [CrossRef]
- Zurmehly, J. Implementing a Nurse-Driven Protocol to Reduce Catheter-Associated Urinary Tract Infections in a Long-Term Acute Care Hospital. J. Contin. Educ. Nurs. 2018, 49, 372–377. [Google Scholar] [CrossRef]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Thornley, T.; Ashiru-Oredope, D.; Beech, E.; Howard, P.; Kirkdale, C.L.; Elliott, H.; Harris, C.; Roberts, A. Antimicrobial use in UK long-term care facilities: Results of a point prevalence survey. J. Antimicrob. Chemother. 2019, 74, 2083–2090. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NHS Improvement. Reducing Gram-Negative Bloodstream Infections—Urinary Tract Infections. 2020. Available online: https://improvement.nhs.uk/resources/reducing-gram-negative-bloodstream-infections-urinary-tract-infections/ (accessed on 26 February 2020).
- Squires, J.E.; Grimshaw, J.M.; Taljaard, M.; Linklater, S.; Chassé, M.; Shemie, S.D.; Knoll, G.A. Design, implementation, and evaluation of a knowledge translation intervention to increase organ donation after cardiocirculatory death in Canada: A study protocol. Implemt. Sci. 2014, 9, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinmo, S.; Fuller, C.; Stone, S.P.; Michie, S. Characterising an implementation intervention in terms of behaviour change techniques and theory: The ‘Sepsis Six’clinical care bundle. Implement. Sci. 2015, 10, 111. [Google Scholar] [CrossRef] [Green Version]
- Steinmo, S.H.; Michie, S.; Fuller, C.; Stanley, S.; Stapleton, C.; Stone, S.P. Bridging the gap between pragmatic intervention design and theory: Using behavioural science tools to modify an existing quality improvement programme to implement “Sepsis Six”. Implement. Sci. 2015, 11, 14. [Google Scholar] [CrossRef] [Green Version]
- Borek, A.J.; Wanat, M.; Sallis, A.; Ashiru-Oredope, D.; Atkins, L.; Beech, E.; Hopkins, S.; Jones, L.; McNulty, C.; Shaw, K.; et al. How can national antimicrobial stewardship interventions in primary care be improved? A stakeholder consultation. Antibiotics 2019, 8, 207. [Google Scholar] [CrossRef] [Green Version]
| Intervention Function | National Interventions (n = 11) | Research Interventions (n = 37) |
| Education | 11 | 37 |
| Enablement | 7 | 31 |
| Training | 4 | 22 |
| Modelling | 2 | 3 |
| Incentivisation | 1 | 5 |
| Environmental restructuring | 0 | 25 |
| Persuasion | 0 | 6 |
| Coercion | 0 | 0 |
| Restriction | 0 | 0 |
| Policy Category | National Interventions (n = 11) | Research Interventions (n = 37) |
| Guidelines | 9 | 17 |
| Service provision | 1 | 36 |
| Legislation | 1 | 0 |
| Communication/marketing | 0 | 17 |
| Regulation | 0 | 0 |
| Fiscal measures | 0 | 0 |
| Environmental/social planning | 0 | 0 |
| National Interventions Top 10 BCTs (n = 11) | Frequency | Research Interventions Top 10 BCTs (n = 37) | Frequency |
|---|---|---|---|
| Instruction on how to perform a behavior * | 10 | Instruction on how to perform a behaviour | 36 |
| Information about health consequences | 9 | Feedback on behaviour | 27 |
| Self-monitoring of behaviour | 5 | Adding objects to the environment | 22 |
| Social support practical | 4 | Prompts/cues | 15 |
| Information about social environmental consequences | 4 | Behavioural practice/rehearsal | 14 |
| Goal setting behaviour | 4 | Social support practical | 13 |
| Monitoring of behaviour by others without feedback | 3 | Feedback on outcome of behaviour | 13 |
| Feedback on behaviour | 3 | Action planning | 9 |
| Feedback on outcome of behaviour | 3 | Behavioural substitution | 9 |
| Self-monitoring of outcome of behaviour | 3 | Restructuring the social environment | 8 |
| Intervention Component | Primary/ Community Care | Secondary Care | Care Homes |
|---|---|---|---|
| Creating the rule that staff transferring catheterised patients to another setting, check/review the need for a catheter with the receiving team; could be prompted by a checklist for discharge/admission of patients to another setting Barriers: Transitions of care; Pre-emptively deciding to insert catheters; Cultural norms regarding standard catheterisation practice for specific patient groups | + | + | + |
| Before inserting catheters, staff required to inform patients and relatives about pros and cons of catheters, risks associated with catheter use, including sepsis and antibiotic resistance and the importance of hydration (with or without written resources) and record that this has been explained to patients. Barriers: Requests from patients and their carers | + | + | + |
| Ensure availability of setting and profession specific guidelines which are in agreement and which include examples of how to adapt to local contexts where possible. Barriers: CAUTI guidelines not perceived as relevant | + | + | |
| Standardised nationwide computer-based documentation, accessible across healthcare sectors, requiring person initiating urinary catheterisation to insert detailed information such as date of catheter insertion, reason for catheterisation, an action plan for review and removal and details of difficult catheterisation (if relevant). Provided when transferring patients across settings. Barriers: inconsistent documentation and records; Transitions of care; No information regarding placement/ duration of catheters | + | + | |
| Intervention to persuade staff of benefits of not using catheters for both patients (e.g., loss of mobility, bed sores, lower risk of infection) and staff (e.g., fewer patients developing infection, improved patient outcomes, lower costs). Reassure staff that not using catheters does not lead to suboptimal care and reframing severity of CAUTI as patient safety issue with a story of a patient who contracted CAUTI. Barriers: Convenience and ease of monitoring; Perceived severity of CAUTI; Lack of perceived benefits to CAUTI interventions; Lack of awareness of the risks related to catheters | + | ||
| Introduction of “CAUTI Champions” (nurses and doctors). Champions role model how to manage patient/carer requests for catheter, lead on staff education and provide practical support for colleagues wanting to support patients to TWOC (trial without catheter) Barriers: Physicians dictate nurses’ practice; Lack of peer support and buy-in | + | ||
| Provision of bladder scanners, accompanied by staff training on how to use scanners, to aid decisions in relation to problems with urinary retention. Barriers: Unavailability of medical alternatives to urinary catheterisation; Lack of knowledge of how to manage patients without catheters | + |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wanat, M.; Borek, A.J.; Atkins, L.; Sallis, A.; Ashiru-Oredope, D.; Beech, E.; Butler, C.C.; Chadborn, T.; Hopkins, S.; Jones, L.; et al. Optimising Interventions for Catheter-Associated Urinary Tract Infections (CAUTI) in Primary, Secondary and Care Home Settings. Antibiotics 2020, 9, 419. https://doi.org/10.3390/antibiotics9070419
Wanat M, Borek AJ, Atkins L, Sallis A, Ashiru-Oredope D, Beech E, Butler CC, Chadborn T, Hopkins S, Jones L, et al. Optimising Interventions for Catheter-Associated Urinary Tract Infections (CAUTI) in Primary, Secondary and Care Home Settings. Antibiotics. 2020; 9(7):419. https://doi.org/10.3390/antibiotics9070419
Chicago/Turabian StyleWanat, Marta, Aleksandra J. Borek, Lou Atkins, Anna Sallis, Diane Ashiru-Oredope, Elizabeth Beech, Christopher C. Butler, Tim Chadborn, Susan Hopkins, Leah Jones, and et al. 2020. "Optimising Interventions for Catheter-Associated Urinary Tract Infections (CAUTI) in Primary, Secondary and Care Home Settings" Antibiotics 9, no. 7: 419. https://doi.org/10.3390/antibiotics9070419






