Titanium Nitride and Nitrogen Ion Implanted Coated Dental Materials
Abstract
:1. Introduction
2. Coating Methodologies and Structural Analysis
| Coating Method | Type/Detail | Reference |
| Physical Vapor Deposition | No further detail beyond “Physical Vapor Deposition” | [2,3,4,5,6,7] |
| Ion Plating | [8,9,10,11,12,13,14] | |
| Cathodic Arc | [15,16,17,18,19] | |
| Radiofrequency sputtering | [20,21,22,23,24,25,26,27] | |
| Arc ion plating | [28,29,30,31] | |
| Plasma immersion implantation | [32,33,34] | |
| Ion beam/Ionic implantation | [8,9,35,36,37,38,39,40,41,42] | |
| Thermal | 500 °C for 480 min | [35] |
| 850 °C for 7 h | [43] | |
| 800–1000 °C for 5–30 min | [44,45] | |
| Chemical Vapor/Chemical | Reaction of wet NH3 with NiTi at 300 °C | [46] |
| MOCVD (metal organic chemical vapor deposition) via evaporation of Ti(Et2N)4 | [28,46] | |
| Plasma chemical vapor | [38] | |
| Boiling in 30% nitric acid for 24 h | [34] | |
| No method stated | [47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68] | |
| Structural Analysis | Comment | Reference |
| X-Ray Photoelectron Spectroscopy (XPS) | [N], [Ti], and sometimes other elements and ratios determined | [3,28,29,32,33,34,35,46] |
| X-Ray Diffraction (XRD) | TiN Identified | [27,29,30,42,67] |
| TiN and Ti2N Identified | [43] | |
| Unidentified oxynitrides | [44,45] | |
| Nuclear Reaction Analysis | [N] depth | [36,37] |
| Method to Determine Coating Thickness | Thickness | Reference |
| Scanning Electron Microscopy (SEM) | 1–2 μm | [29] |
| 2 μm | [20,43] | |
| ~10 μm | [44,45] | |
| Electron Probe MicroAnalysis (EPMA) | 0.3 μm average | [26] |
| XPS | [N]max within 10 nm; [N] detected up to 60 nm depth | [35] |
| Nuclear Reaction Analysis | [N] detected up to 60 nm | [36,37] |
| Ball-cratering method | 1.5 μm | [21] |
| Light Microscopy | 8 μm | [67] |
| Given via a reference, manufacturer data, equipment parameters, or other unconfirmed sources | <650 nm | [40] |
| 0.3 μm N-implanted; 3 μm TiN | [8,9] | |
| 1 μm | [27] | |
| 1.5 μm | [17,18] | |
| 1.8 μm | [22,23,24,25] | |
| 2 μm | [14,42] | |
| 1-5 μm | [15] | |
| 2-5 μm | [47] | |
| 10 μm | [19] |
2.1. Coatings in Implant Dentistry
| Duration (Weeks) | Animal Model | Prior Surface Treatment | BIC (%) | Reference | |
|---|---|---|---|---|---|
| Ti | TiN | ||||
| 8 | Rats | Machining | 59.0 ± 3.1 | 58.0 ± 3.0 | [5] |
| 8 | Rats | Sandblasting | 64.0 ± 4.1 | 66.0 ± 3.5 | [5] |
| 8 | Rats | TPS | 72.0 ± 2.5 | 70.0 ± 2.1 | [5] |
| 8 | Rats | 42.6 | 40.8 | [43] | |
| 8 | Dogs | 69.7 ± 1.3 | 70.6 ± 1.7 | [48] | |
| 12 | Rabbits | 58.8 | 52.7 | [39] | |
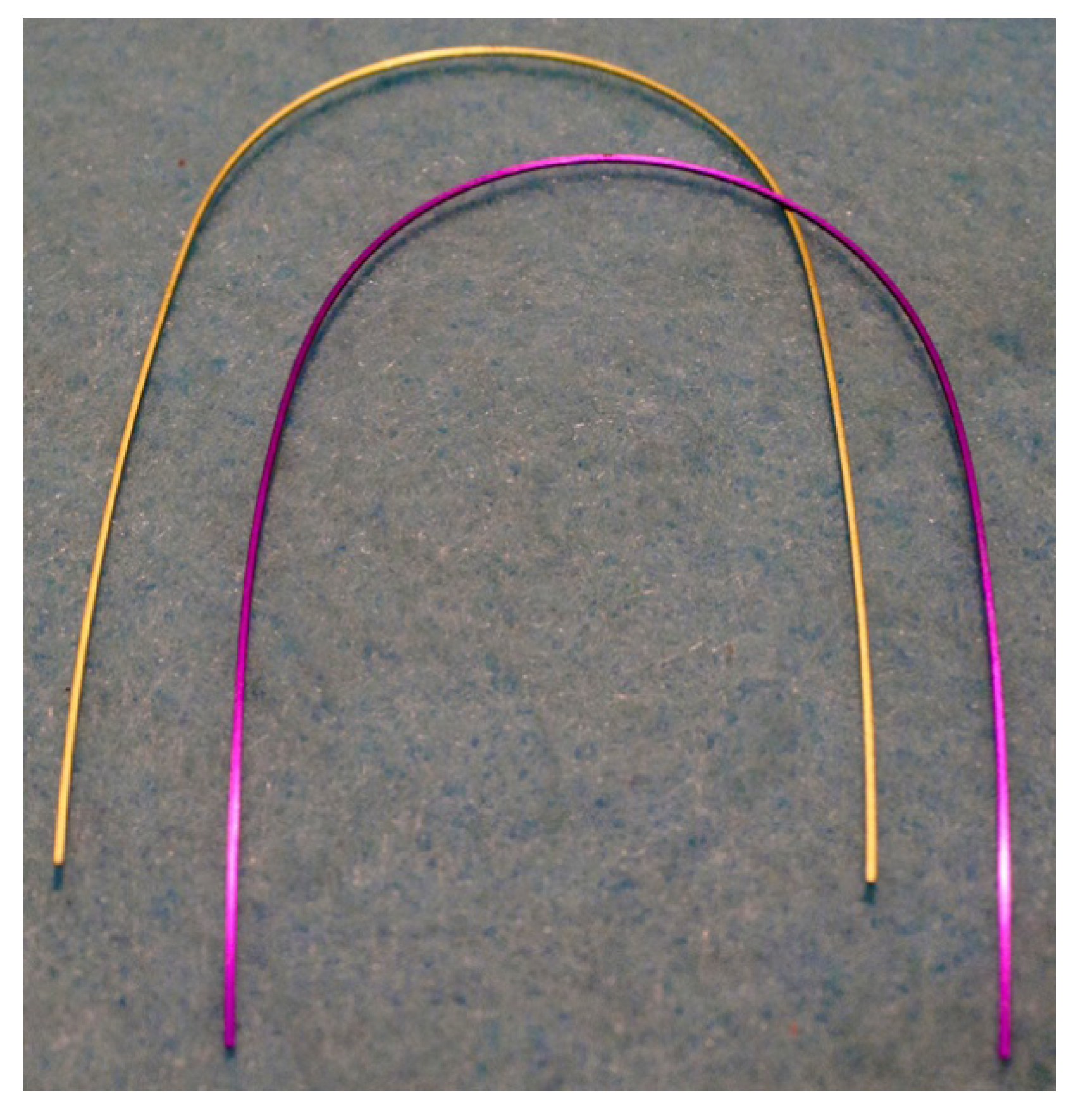
2.2. Coatings in Orthodontics
| Wire Type | Commercial Product Name (Manufacturer) | Coupled Material for Friction (if specified) | Amount of Friction Compared to Control (non-coated counterpart) | Reference |
|---|---|---|---|---|
| NiTi | Ti-6Al-4V | 45% | [44] | |
| NiTi | Stainless steel | 59% | ||
| NiTi | Neo Sentalloy F80 Ionguard (GAC Int., Bohemia, NY, USA) | 77% | [51] | |
| β-titanium | Purple TMA (Ormco) | Stainless steel | 25% (static) 20% (kinetic) | [6] |
| β-titanium | Ion-implanted TMA (Ormco) | Ti implanted alumina | 47% (static) 66% (kinetic) | [40] |
| β-titanium | Ion-implanted TMA (Ormco) | Stainless steel | 100% (static) 108% (kinetic) | [54] |
| β-titanium | Aqua TMA (Ormco) | Stainless steel | 105% (static) 111% (kinetic) | [55] |
| β-titanium | Honeydew TMA (Ormco) | Stainless steel | 49% (static) 55% (kinetic) | |
| β-titanium | Purple TMA (Ormco) | Stainless steel | 102% (static) 104% (kinetic) | |
| β-titanium | Violet TMA (Ormco) | Stainless steel | 96% (static) 102% (kinetic) | |
| β-titanium | Ion-implanted TMA (Ormco) | Stainless steel | 51% (static) 55% (kinetic) |
2.3. Coatings in Endodontics

2.4. Coatings in Prosthodontics
2.5. Coatings in Dental Instrumentation
3. Conclusions
Acknowledgments
References
- Mezger, P.R.; Creugers, N.H. Titanium nitride coatings in clinical dentistry. J. Dent. 1992, 20, 342–344. [Google Scholar] [CrossRef]
- Scarano, A.; Piattelli, M.; Vrespa, G.; Caputi, S.; Piattelli, A. Bacterial adhesion on titanium nitride-coated and uncoated implants: An in vivo human study. J. Oral Implant. 2003, 29, 80–85. [Google Scholar] [CrossRef]
- Durual, S.; Pernet, F.; Rieder, P.; Mekki, M.; Cattani-Lorente, M.; Wiskott, H.W. Titanium nitride oxide coating on rough titanium stimulates the proliferation of human primary osteoblasts. Clin. Oral Implant. Res. 2011, 22, 552–559. [Google Scholar] [CrossRef]
- Annunziata, M.; Guida, L.; Perillo, L.; Aversa, R.; Passaro, I.; Oliva, A. Biological response of human bone marrow stromal cells to sandblasted titanium nitride-coated implant surfaces. J. Mater. Sci. Mater. Med. 2008, 19, 3585–3591. [Google Scholar] [CrossRef]
- Scarano, A.; Piattelli, M.; Vrespa, G.; Petrone, G.; Iezzi, G.; Piattelli, A. Bone healing around titanium and titanium nitride-coated dental implants with three surfaces: An experimental study in rats. Clin. Implant Dent. Relat. Res. 2003, 5, 103–111. [Google Scholar] [CrossRef]
- Burstone, C.J.; Farzin-Nia, F. Production of low-friction and colored TMA by ion implantation. J. Clin. Orthod. 1995, 29, 453–461. [Google Scholar]
- Bonaccorso, A.; Tripi, T.R.; Rondelli, G.; Condorelli, G.G.; Cantatore, G.; Schäfer, E. Pitting corrosion resistance of nickel-titanium rotary instruments with different surface treatments in seventeen percent ethylenediaminetetraacetic acid and sodium chloride solutions. J. Endod. 2008, 34, 208–211. [Google Scholar] [CrossRef]
- Yoshinari, M.; Oda, Y.; Kato, T.; Okuda, K. Influence of surface modifications to titanium on antibacterial activity in vitro. Biomaterials 2001, 22, 2043–2048. [Google Scholar] [CrossRef]
- Yoshinari, M.; Oda, Y.; Kato, T.; Okuda, K.; Hirayama, A. Influence of surface modifications to titanium on oral bacterial adhesion in vitro. J. Biomed. Mater. Res. 2000, 2, 388–394. [Google Scholar]
- Satomi, K.; Akagawa, Y.; Nikai, H.; Tsuru, H. Tissue response to implanted ceramic-coated titanium alloys in rats. J. Oral Rehabil. 1988, 15, 339–345. [Google Scholar] [CrossRef]
- Kao, C.T.; Guo, J.U.; Huang, T.H. Comparison of friction force between corroded and noncorroded titanium nitride plating of metal brackets. Am. J. Orthod. Dentofac. Orthoped. 2011, 139, 594–600. [Google Scholar] [CrossRef]
- Kao, C.T.; Ding, S.J.; Chen, Y.C.; Huang, T.H. The anticorrosion ability of titanium nitride (TiN) plating on an orthodontic metal bracket and its biocompatibility. J. Biomed. Mater. Res. 2002, 63, 786–792. [Google Scholar] [CrossRef]
- Hai, K.; Sawase, T.; Matsumura, H.; Atsuta, M.; Baba, K.; Hatada, R. Corrosion resistance of a magnetic stainless steel ion-plated with titanium nitride. J. Oral Rehabil. 2000, 27, 361–366. [Google Scholar] [CrossRef]
- Taira, Y.; Hai, K.; Matsumura, H.; Atsuta, M. Adhesive bonding of titanium nitride-plated stainless steel for magnetic attachments. Eur. J. Oral Sci. 2001, 109, 204–207. [Google Scholar] [CrossRef]
- Mengel, R.; Meer, C.; Flores-de-Jacoby, L. The treatment of uncoated and titanium nitride-coated abutments with different instruments. Int. J. Oral Maxillofac. Implant. 2004, 19, 232–238. [Google Scholar]
- Annunziata, M.; Oliva, A.; Basile, M.A.; Giordano, M.; Mazzola, N.; Rizzo, A.; Lanza, A.; Guida, L. The effects of titanium nitride-coating on the topographic and biological features of TPS implant surfaces. J. Dent. 2011, 39, 720–728. [Google Scholar] [CrossRef]
- Schäfer, E. Effect of physical vapor deposition on cutting efficiency of nickel-titanium files. J. Endod. 2002, 28, 800–802. [Google Scholar] [CrossRef]
- Schäfer, E. Effect of sterilization on the cutting efficiency of PVD-coated nickel-titanium endodontic instruments. Int. Endod. J. 2002, 35, 867–872. [Google Scholar] [CrossRef]
- Wu, J.C.; Lai, L.C.; Sheets, C.G.; Earthman, J.; Newcomb, R. A comparison of the marginal adaptation of cathode-arc vapor-deposited titanium and cast base metal copings. J. Prosthet. Dent. 2011, 105, 403–409. [Google Scholar] [CrossRef]
- Chung, K.H.; Duh, J.G.; Shin, D.; Cagna, D.R.; Cronin, R.J., Jr. Characteristics and porcelain bond strength of (Ti,Al)N coating on dental alloys. J. Biomed. Mater. Res. 2002, 63, 516–521. [Google Scholar] [CrossRef]
- Kurt, M.; Külünk, T.; Ural, C.; Külünk, S.; Danişman, S.; Savaş, S. The effect of different surface treatments on retention of cement retained implant supported restorations. J. Oral Implant. 2010. [Google Scholar]
- Grössner-Schreiber, B.; Griepentrog, M.; Haustein, I.; Müller, W.D.; Lange, K.P.; Briedigkeit, H.; Göbel, U.B. Plaque formation on surface modified dental implants: An in vitro study. Clin. Oral Implant. Res. 2001, 12, 543–551. [Google Scholar] [CrossRef]
- Groessner-Schreiber, B.; Hannig, M.; Dück, A.; Griepentrog, M.; Wenderoth, D.F. Do different implant surfaces exposed in the oral cavity of humans show different biofilm compositions and activities? Eur. J. Oral Sci. 2004, 112, 516–522. [Google Scholar] [CrossRef]
- Groessner-Schreiber, B.; Neubert, A.; Müller, W.D.; Hopp, M.; Griepentrog, M.; Lange, K.P. Fibroblast growth on surface-modified dental implants: An in vitro study. J. Biomed. Mater. Res. A 2003, 64, 591–599. [Google Scholar]
- Grössner-Schreiber, B.; Herzog, M.; Hedderich, J.; Dück, A.; Hannig, M.; Griepentrog, M. Focal adhesion contact formation by fibroblasts cultured on surface-modified dental implants: An in vitro study. Clin. Oral Implant. Res. 2006, 17, 736–745. [Google Scholar] [CrossRef]
- Tanaka, K.; Kimoto, K.; Sawada, T.; Toyoda, M. Shear bond strength of veneering composite resin to titanium nitride coating alloy deposited by radiofrequency sputtering. J. Dent. 2006, 34, 277–282. [Google Scholar] [CrossRef]
- Chien, C.C.; Liu, K.T.; Duh, J.G.; Chang, K.W.; Chung, K.H. Effect of nitride film coatings on cell compatibility. Dent. Mater. 2008, 24, 986–993. [Google Scholar] [CrossRef]
- Tripi, T.R.; Bonaccorso, A.; Rapisarda, E.; Tripi, V.; Condorelli, G.G.; Marino, R.; Fragalà, I. Depositions of nitrogen on NiTi instruments. J. Endod. 2002, 28, 497–500. [Google Scholar] [CrossRef]
- Endo, K.; Sachdeva, R.; Araki, Y.; Ohno, H. Effects of titanium nitride coatings on surface and corrosion characteristics of Ni-Ti alloy. Dent. Mater. J. 1994, 13, 228–239. [Google Scholar] [CrossRef]
- Oshida, Y.; Hashem, A. Titanium-porcelain system Part I: Oxidation kinetics of nitrided pure titanium, simulated to porcelain firing process. Biomed. Mater. Eng. 1993, 3, 185–198. [Google Scholar]
- Lim, H.P.; Kim, J.H.; Lee, K.M.; Park, S.W. Fracture load of titanium crowns coated with gold or titanium nitride and bonded to low-fusing porcelain. J. Prosthet. Dent. 2011, 10, 164–170. [Google Scholar]
- Alves-Claro, A.P.; Claro, F.A.; Uzumaki, E.T. Wear resistance of nickel-titanium endodontic files after surface treatment. J. Mater. Sci. Mater. Med. 2008, 19, 3273–3277. [Google Scholar] [CrossRef]
- Iijima, M.; Yuasa, T.; Endo, K.; Muguruma, T.; Ohno, H.; Mizoguchi, I. Corrosion behavior of ion implanted nickel-titanium orthodontic wire in fluoride mouth rinse solutions. Dent. Mater. J. 2010, 29, 53–58. [Google Scholar] [CrossRef]
- Li, U.M.; Iijima, M.; Endo, K.; Brantley, W.A.; Alapati, S.B.; Lin, C.P. Application of plasma immersion ion implantation for surface modification of nickel-titanium rotary instruments. Dent. Mater. J. 2007, 26, 467–473. [Google Scholar] [CrossRef]
- Rapisarda, E.; Bonaccorso, A.; Tripi, T.R.; Fragalk, I.; Condorelli, G.G. The effect of surface treatments of nickel-titanium files on wear and cutting efficiency. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 89, 363–368. [Google Scholar] [CrossRef]
- Gavini, G.; Pessoa, O.F.; Barletta, F.B.; Vasconcellos, M.A.; Caldeira, C.L. Cyclic fatigue resistance of rotary nickel-titanium instruments submitted to nitrogen ion implantation. J. Endod. 2010, 36, 1183–1186. [Google Scholar] [CrossRef]
- Wolle, C.F.; Vasconcellos, M.A.; Hinrichs, R.; Becker, A.N.; Barletta, F.B. The effect of argon and nitrogen ion implantation on nickel-titanium rotary instruments. J. Endod. 2009, 35, 1558–1562. [Google Scholar] [CrossRef]
- Catledge, S.A.; Vohra, Y.K.; Bellis, S.L.; Sawyer, A.A. Mesenchymal stem cell adhesion and spreading on nanostructured biomaterials. J. Nanosci. Nanotechnol. 2004, 4, 986–989. [Google Scholar] [CrossRef]
- De Maeztu, M.A.; Alava, J.I.; Gay-Escoda, C. Ion implantation: Surface treatment for improving the bone integration of titanium and Ti6Al4V dental implants. Clin. Oral Implant. Res. 2003, 14, 57–62. [Google Scholar] [CrossRef]
- Kusy, R.P.; Tobin, E.J.; Whitley, J.Q.; Sioshansi, P. Frictional coefficients of ion-implanted alumina against ion-implanted beta-titanium in the low load, low velocity, single pass regime. Dent. Mater. 1992, 8, 167–172. [Google Scholar] [CrossRef]
- Rapisarda, E.; Bonaccorso, A.; Tripi, T.R.; Condorelli, G.G.; Torrisi, L. Wear of nickel-titanium endodontic instruments evaluated by scanning electron microscopy: Effect of ion implantation. J. Endod. 2001, 27, 588–592. [Google Scholar] [CrossRef]
- Sawase, T.; Yoshida, K.; Taira, Y.; Kamada, K.; Atsuta, M.; Baba, K. Abrasion resistance of titanium nitride coatings formed on titanium by ion-beam-assisted deposition. J. Oral Rehabil. 2005, 32, 151–157. [Google Scholar] [CrossRef]
- Tamura, Y.; Yokoyama, A.; Watari, F.; Kawasaki, T. Surface properties and biocompatibility of nitrided titanium for abrasion resistant implant materials. Dent. Mater. J. 2002, 21, 355–372. [Google Scholar] [CrossRef]
- Gil, F.J.; Solano, E.; Campos, A.; Boccio, F.; Sáez, I.; Alfonso, M.V.; Planell, J.A. Improvement of the friction behaviour of NiTi orthodontic archwires by nitrogen diffusion. Biomed. Mater. Eng. 1998, 8, 335–342. [Google Scholar]
- Gil, F.J.; Solano, E.; Mendoza, A.; Pena, J. Inhibition of Ni release from NiTi and NiTiCu orthodontic archwires by nitrogen diffusion treatment. J. Appl. Biomater. Biomech. 2004, 2, 151–155. [Google Scholar]
- Tripi, T.R.; Bonaccorso, A.; Condorelli, G.G. Fabrication of hard coatings on NiTi instruments. J. Endod. 2003, 29, 132–134. [Google Scholar] [CrossRef]
- Alsabeeha, N.H.; Swain, M.V.; Payne, A.G. Clinical performance and material properties of single-implant overdenture attachment systems. Int. J. Prosthodont. 2011, 24, 247–254. [Google Scholar]
- Yi, K.J.; Kim, S.G.; Moon, S.Y.; Lim, S.C.; Son, J.S.; Kim, C.G.; Chung, K. Vertical distraction osteogenesis using a titanium nitride-coated distractor. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, e5–e9. [Google Scholar]
- Abi Nader, S.; de Souza, R.F.; Fortin, D.; de Koninck, L.; Fromentin, O.; Albuquerque, R.F., Jr. Effect of simulated masticatory loading on the retention of stud attachments for implant overdentures. J. Oral Rehabil. 2011, 38, 157–164. [Google Scholar] [CrossRef]
- Assunção, W.G.; Delben, J.A.; Tabata, L.F.; Barão, V.A.; Gomes, E.A.; Garcia, I.R., Jr. Preload evaluation of different screws in external hexagon joint. Implant Dent. 2012, 21, 46–50. [Google Scholar] [CrossRef]
- Wichelhaus, A.; Geserick, M.; Hibst, R.; Sander, F.G. The effect of surface treatment and clinical use on friction in NiTi orthodontic wires. Dent. Mater. 2005, 21, 938–945. [Google Scholar] [CrossRef]
- D’Antò, V.; Rongo, R.; Ametrano, G.; Spagnuolo, G.; Manzo, P.; Martina, R.; Paduano, S.; Valletta, R. Evaluation of surface roughness of orthodontic wires by means of atomic force microscopy. Angle Orthod. 2012. [Google Scholar]
- Husmann, P.; Bourauel, C.; Wessinger, M.; Jäger, A. The frictional behavior of coated guiding archwires. J. Orofac. Orthop. 2002, 63, 199–211. [Google Scholar] [CrossRef]
- Kusy, R.P.; Whitley, J.Q.; de Araújo Gurgel, J. Comparisons of surface roughnesses and sliding resistances of 6 titanium-based or TMA-type archwires. Am. J. Orthod. Dentofac. 2004, 126, 589–603. [Google Scholar] [CrossRef]
- Cash, A.; Curtis, R.; Garrigia-Majo, D.; McDonald, F. A comparative study of the static and kinetic frictional resistance of titanium molybdenum alloy archwires in stainless steel brackets. Eur. J. Orthodont. 2004, 26, 105–111. [Google Scholar] [CrossRef]
- Neumann, P.; Bourauel, C.; Jäger, A. Corrosion and permanent fracture resistance of coated and conventional orthodontic wires. J. Mater. Sci. Mater. Med. 2002, 13, 141–147. [Google Scholar] [CrossRef]
- Peitsch, T.; Klocke, A.; Kahl-Nieke, B.; Prymak, O.; Epple, M. The release of nickel from orthodontic NiTi wires is increased by dynamic mechanical loading but not constrained by surface nitridation. J. Biomed. Mater. Res. A 2007, 82, 731–739. [Google Scholar]
- Kim, H.; Johnson, J.W. Corrosion of stainless steel, nickel-titanium, coated nickel-titanium, and titanium orthodontic wires. Angle Orthod. 1999, 69, 39–44. [Google Scholar]
- Schuster, G.; Reichle, R.; Bauer, R.R.; Schopf, P.M. Allergies induced by orthodontic alloys: Incidence and impact on treatment-Results of a survey in private orthodontic offices in the Federal State of Hesse, Germany. J. Orofac. Orthop. 2004, 65, 48–59. [Google Scholar] [CrossRef]
- Pernier, C.; Grosgogeat, B.; Ponsonnet, L.; Benay, G.; Lissac, M. Influence of autoclave sterilization on the surface parameters and mechanical properties of six orthodontic wires. Eur. J. Orthodont. 2005, 27, 72–81. [Google Scholar] [CrossRef]
- Ryan, R.; Walker, G.; Freeman, K.; Cisneros, G.J. The effects of ion implantation on rate of tooth movement: An in vitro model. Am. J. Orthod. Dentofac. 1997, 112, 64–68. [Google Scholar] [CrossRef]
- Cobb, N.W.; Kula, K.S.; Phillips, C.; Proffit, W.R. Efficiency of multi-strand steel, superelastic Ni-Ti and ion-implanted Ni-Ti archwires for initial alignment. Clin. Orthod. Res. 1998, 1, 12–19. [Google Scholar]
- Kula, K.; Phillips, C.; Gibilaro, A.; Proffit, W.R. Effect of ion implantation of TMA archwires on the rate of orthodontic sliding space closure. Am. J. Orthod. Dentofac. 1998, 114, 577–580. [Google Scholar] [CrossRef]
- Sisera, M.; Hofer, D.J.; Sener, B.; Attin, T.; Schmidlin, P.R. In vitro evaluation of three curettes with edge retention technology after extended use. Schweiz Monatsschr Zahnmed. 2009, 119, 1200–1208. [Google Scholar]
- Aspriello, S.D.; Piemontese, M.; Levrini, L.; Sauro, S. Ultramorphology of the root surface subsequent to hand-ultrasonic simultaneous instrumentation during non-surgical periodontal treatments: An in vitro study. J. Appl. Oral Sci. 2011, 19, 74–81. [Google Scholar] [CrossRef]
- Steele, J.G.; McCabe, J.F.; Barnes, I.E. Properties of a titanium nitride coating for dental instruments. J. Dent. 1991, 19, 226–229. [Google Scholar] [CrossRef]
- Rawlings, R.D.; Robinson, P.B.; Rogers, P.S. The durability of ceramic coated dental instruments. Eur. J. Prosthodont. Restor. Dent. 1995, 3, 211–216. [Google Scholar]
- Jackson, M.J.; Sein, H.; Ahmed, W.; Woodwards, R. Novel diamond-coated tools for dental drilling applications. J. Med. Eng. Technol. 2007, 31, 81–93. [Google Scholar] [CrossRef]
- Andreasen, G.F.; Hilleman, T.B. An evaluation of 55 cobalt substituted Nitinol wire for use in orthodontics. J. Am. Dent. Assoc. 1971, 82, 1373–1375. [Google Scholar]
- Goldberg, J.; Burstone, C.J. An evaluation of beta titanium alloys for use in orthodontic appliances. J. Dent. Res. 1979, 58, 593–599. [Google Scholar] [CrossRef]
- Walia, H.; Brantley, W.A.; Gerstein, H. An initial investigation of the bending and torsional properties of Nitinol root canal files. J. Endod. 1988, 14, 346–351. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Jabbari, Y.S.A.; Fehrman, J.; Barnes, A.C.; Zapf, A.M.; Zinelis, S.; Berzins, D.W. Titanium Nitride and Nitrogen Ion Implanted Coated Dental Materials. Coatings 2012, 2, 160-178. https://doi.org/10.3390/coatings2030160
Jabbari YSA, Fehrman J, Barnes AC, Zapf AM, Zinelis S, Berzins DW. Titanium Nitride and Nitrogen Ion Implanted Coated Dental Materials. Coatings. 2012; 2(3):160-178. https://doi.org/10.3390/coatings2030160
Chicago/Turabian StyleJabbari, Youssef S. Al, Jennifer Fehrman, Ashley C. Barnes, Angela M. Zapf, Spiros Zinelis, and David W. Berzins. 2012. "Titanium Nitride and Nitrogen Ion Implanted Coated Dental Materials" Coatings 2, no. 3: 160-178. https://doi.org/10.3390/coatings2030160




