Development and Studies of VR-Assisted Hand Therapy Using a Customized Biomechatronic 3D Printed Orthosis
Abstract
:1. Introduction
1.1. Biomechatronics
1.2. 3D Printing Methods for Customized Orthotics
1.3. Virtual Reality Applications in Therapy
2. Materials and Methods
2.1. Research Main Concept and Plan
- Intuitiveness,
- Clear and easy interface (without much text),
- Quick loading time,
- Encouragement for the user to engage appropriately,
- Carry high-quality mechanics, graphics, and sounds, to be compelling mostly to young people (who are main target of the system).
- Ensuring accurate and up-to-date recording of hand movements, including independent finger movements simulating grasping,
- Possibility of simultaneous cooperation with another state-of-the-art movement registration system,
- Ensuring the mobility of the device and user,
- Cooperation of the device with the selected VR system,
- Low weight and ergonomic use,
- Independent power source,
- Basic aesthetics,
- External housing, with the option of attaching to the orthosis or switching between orthoses for various hand sizes,
- Low-cost build with available, cheap sensors.
2.2. AutoMedPrint System
2.3. Preliminary Studies—Patient Case and Customized Orthosis Description
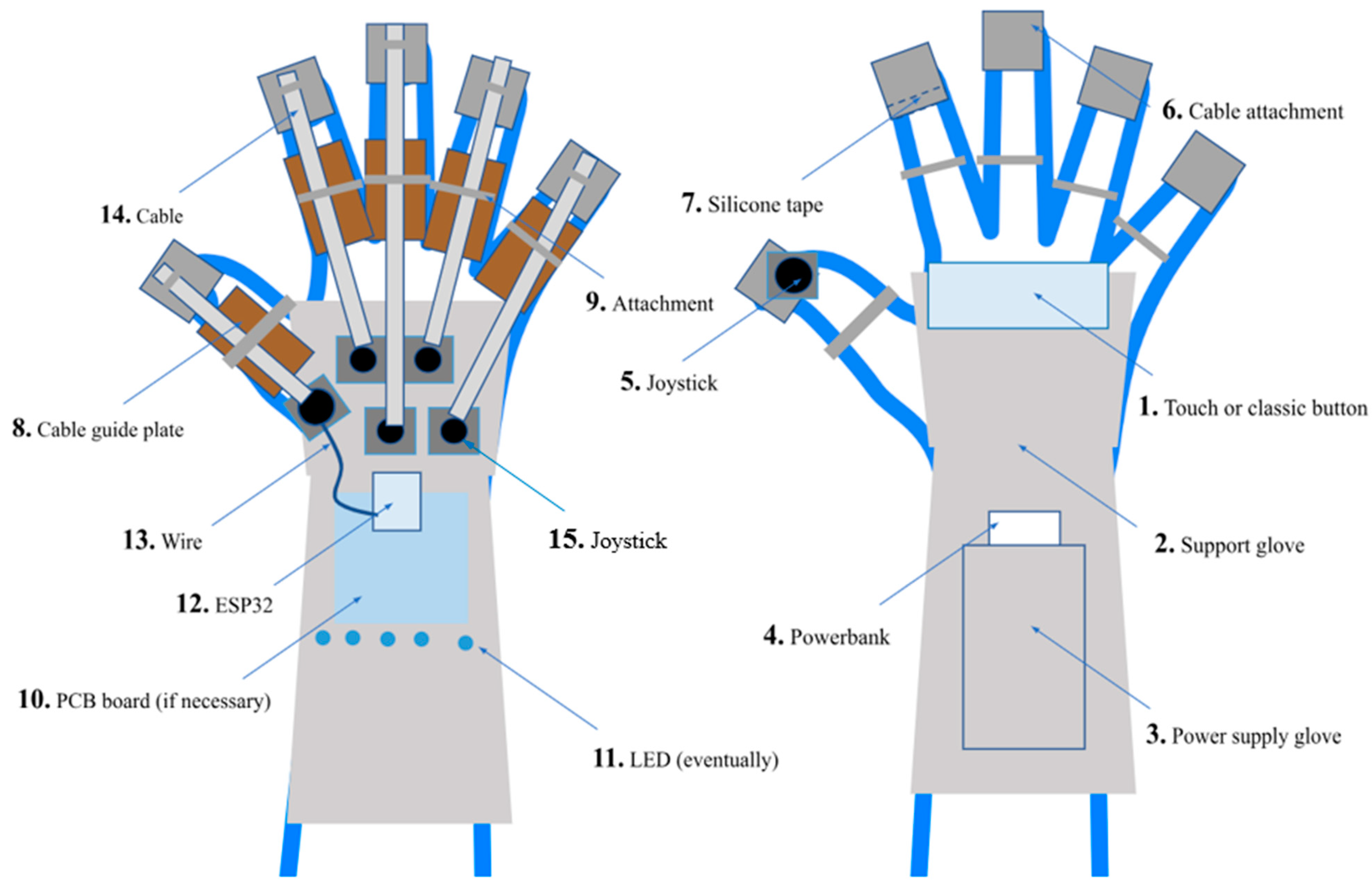
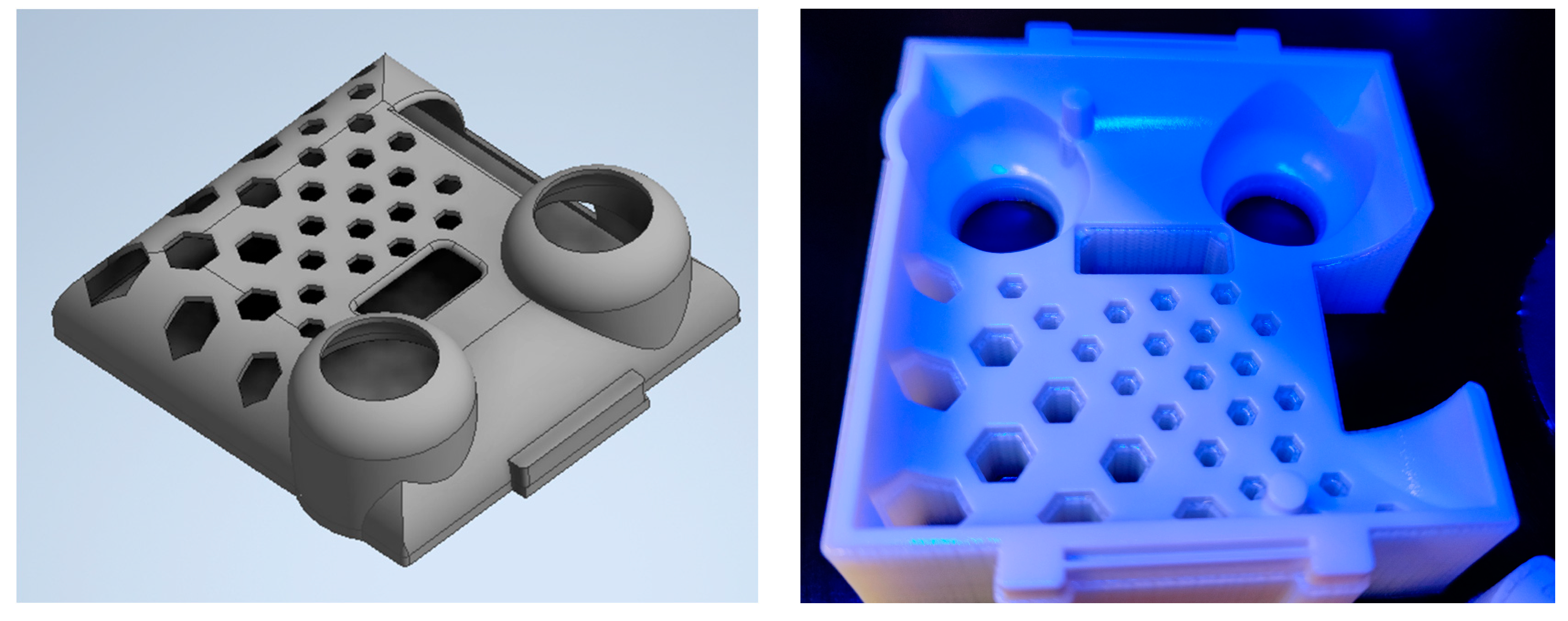
2.4. Design and Prototyping of a Motion Controller
- The controllers replace standard VR controllers for both hands—the healthy one and the one requiring therapy.
- The controllers should be easily attached and detached to/from the orthosis and user’s fingers.
- The controllers must detect rotational hand movement, as well as movements of two fingers (thumb and index).
- A button must be present in the palm of the hand to allow detection of grasping gestures.
- Another device should be used for pointing/teleportation inside the application.
- Hand positional tracking should be realized in compatibility with used VR system (e.g., HTC Vive, which was selected to be the main platform).
2.5. Conceiving the VR-Assisted Hand Therapy Application
2.6. Testing Methodology
- Part 1—evaluation of VR application and exercises, 8 questions, Likert scale (1–5),
- Part 2—evaluation of custom-made game controllers, 6 questions, Likert scale (1–5),
- Part 3—general assessment (1–5 scale), comments, observations, problems (open questions).
3. Results
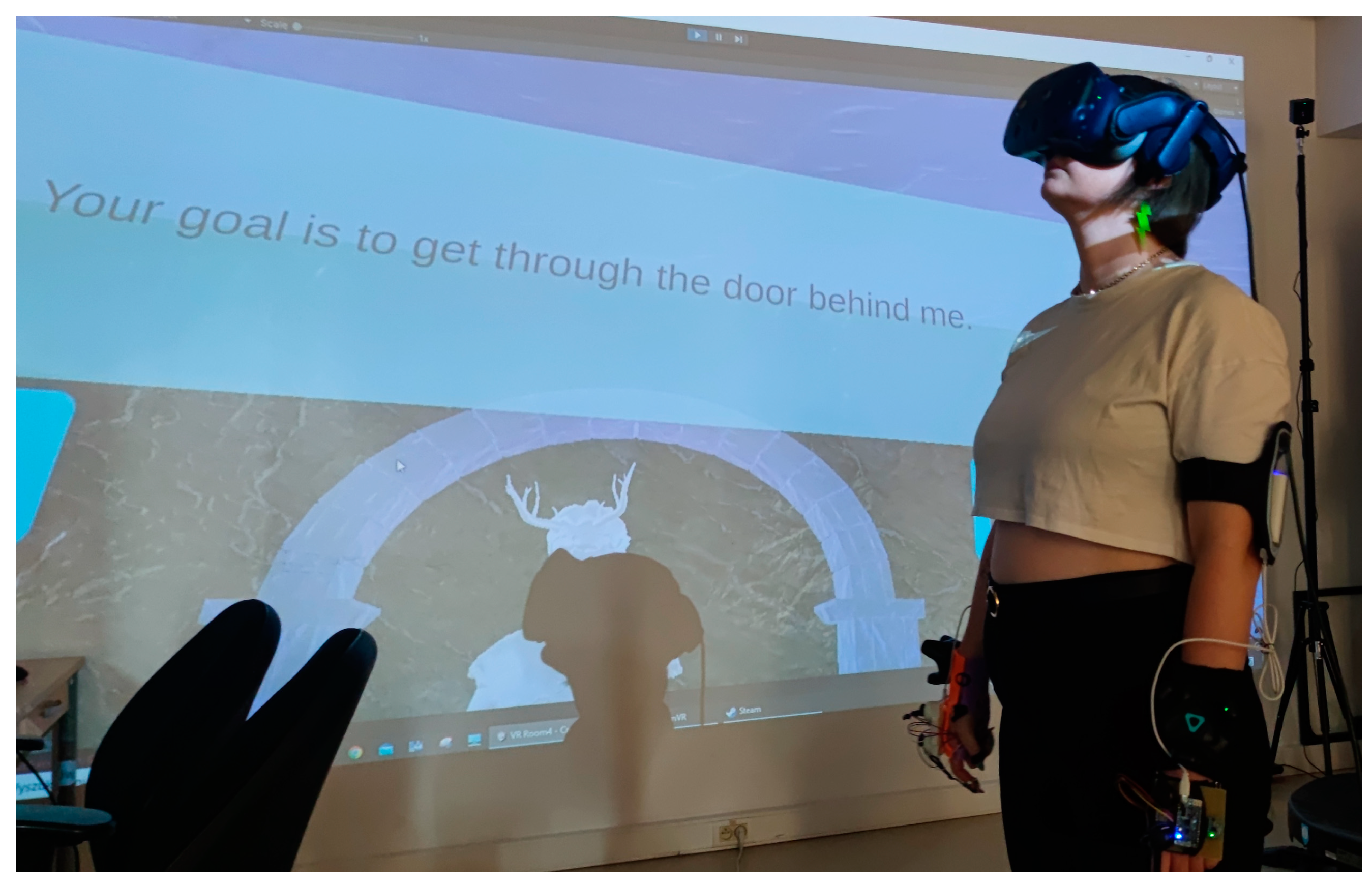
3.1. Orthosis and Controller Manufacturing and Assembly
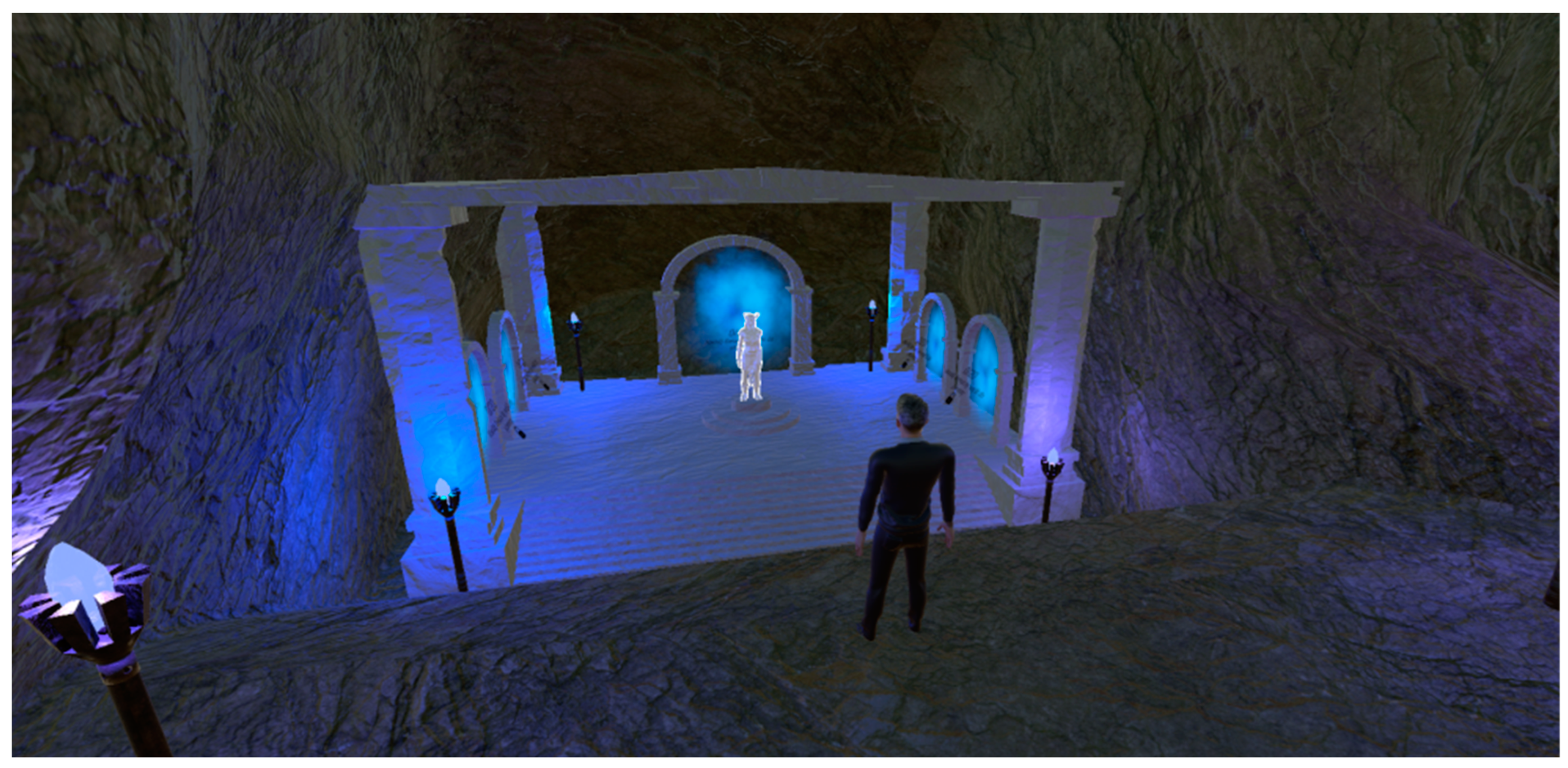
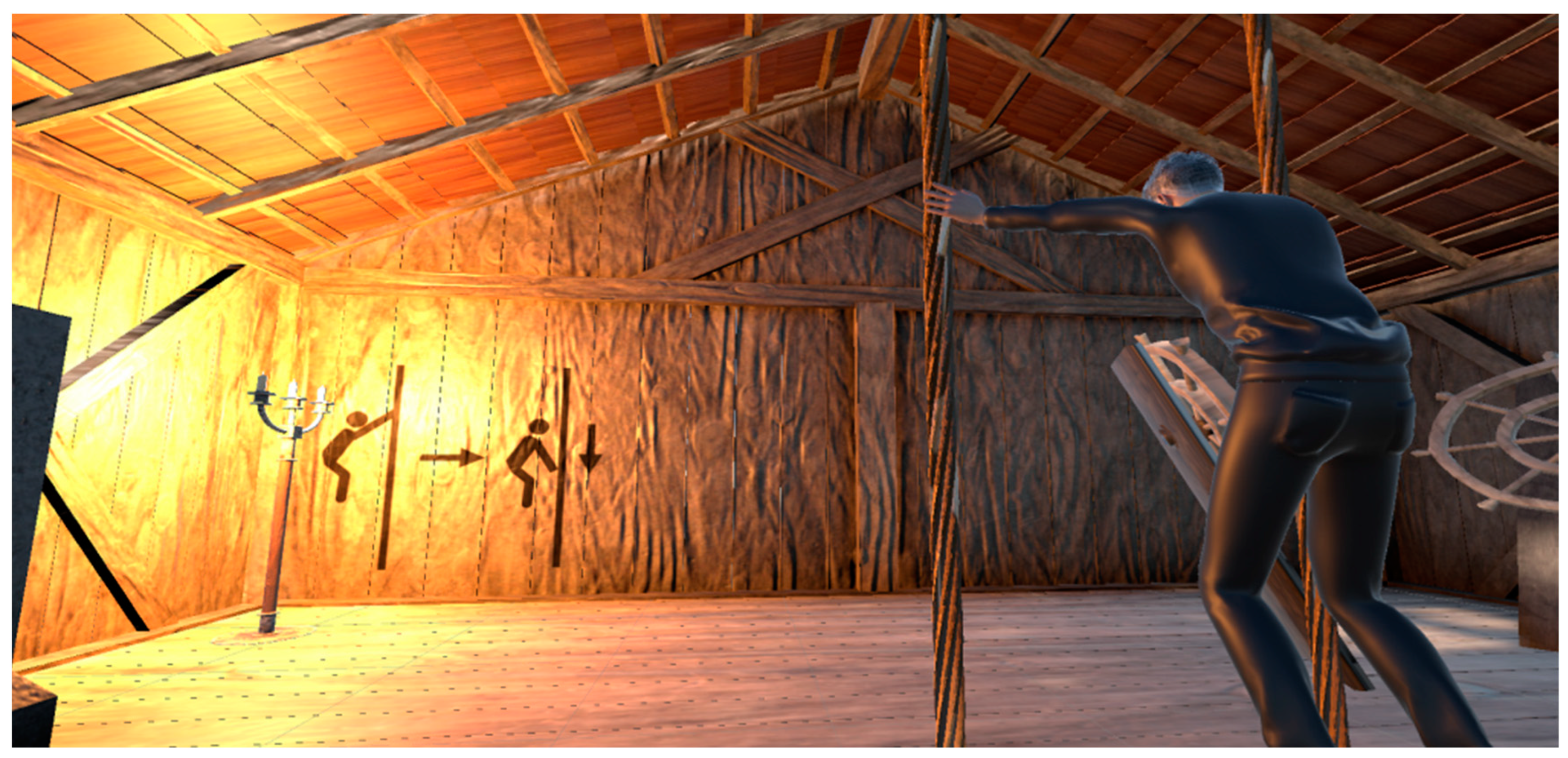
3.2. VR Application Building Results
3.3. User Test Results
- The average evaluation of the whole VR system by all test users is 4.45 in 5-point scale. Most assessments were 4 or 5, confirmed by positive opinions expressed by test participants, regardless of age and background. This means that the system was generally met with a favorable reception.
- The set of exercises were finished on average in a little above 20 min, some persons taking 16 min, and the longest time being 30 min. Including the tutorial and setting up the system, whole sets of exercises can be set to take one full hour of a physiotherapeutic session, which is acceptable from the point of view of hand therapy practice.
- All users agreed that this form of training is more interesting than the classical one and that they would be more frequently engaged in the training if it had that form.
- Graphics quality was assessed as acceptable or high, there was no problem with this aspect, although some users noted minor glitches, especially in behavior of the virtual avatar (deformation of hand and wrist during some movements).
- Interaction was generally evaluated positively, although most users had some minor problems with getting used to interacting with objects, mostly due to the steep learning curve of becoming familiar with the designed game controller.
- Most users observed their muscles to be warmed up during the exercises, but rarely fatigued, which is understandable considering the total length of the game.
- In the survey part related to the design of a custom orthosis-based controller, the evaluation was generally positive, but there are problem indicators. The controller was not very comfortable for all persons, and also not always intuitive and easy to use. However, most users liked it and of all questions, the highest answer and certainty was that it is better for the rehabilitation game than a typical VR controller.
- Test subjects of younger age tended to adapt to the controller and the game mechanics more rapidly (in general).
- Most users has problems with understanding pictures with instructions contained in the rooms and they had to obtain spoken hints on what to do in a given exercise.
- Limited times for certain exercises did not allow some subjects to complete them.
- The assumed course of realizing the exercises was not clearly followed by the users and as such the game would require plenty of improvements, to “forbid” certain behaviors (such as dragging the rope with both hands at once).
- There was a problem with IMU in the controller—it frequently noted a rotational drift, which accumulated over the course of the game. It vanished after the device was reset, but it was clearly disturbing the work.
- Teleporting around the scene was initially problematic for most test subjects.
- The thumb joystick also was not fully intuitive and required plenty of tries from most subjects to operate properly.
- Wired VR goggles hinder the movements of test subjects, especially during warmup. A wireless solution or special cable harnesses should be used in future development.
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Full Text of Realized Survey
| Age: | |
| Sex: | |
| Field of study (for students): | |
| Occupation: |
| I strongly disagree | I tend to disagree | I have no opinion | I tend to agree | I definetly agree |
| 1. I feel my muscles warming up. | ||||
| 2. I feel muscle fatigue. | ||||
| 3. The application is more interesting than classic training. | ||||
| 4. I feel that I would exercise more often if I had constant access to the presented system. | ||||
| 5. Using the application was pleasant and simple. | ||||
| 6. The exercises were engaging but possible to perform correctly. | ||||
| 7. The level of graphic quality was sufficient. | ||||
| 8. Interacting with objects was intuitive and easy to learn. | ||||
| I strongly disagree | I tend to disagree | I have no opinion | I tend to agree | I definetly agree |
| 1. The controller is comfortable | ||||
| 2. I like this controller solution | ||||
| 3. I believe this controller is better for this specific use than the classic one. | ||||
| 4. The response speed to signals from the controller was sufficient | ||||
| 5. Using the controller was pleasant and simple. | ||||
| 6. Interacting with objects using the controller was intuitive and easy to learn. | ||||
References
- Brooker, G.M. Introduction to Biomechatronics; SciTech Publishing Inc.: Raleigh, NC, USA, 2012. [Google Scholar]
- Jan, F.; Althoefer, K. Soft Biomimetic Prosthetic Hand: Design, Manufacturing and Preliminary Examination. In Proceedings of the 2018 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Madrid, Spain, 1–5 October 2018. [Google Scholar] [CrossRef]
- Chaichaowarat, R.; Prakthong, S.; Thitipankul, S. Transformable Wheelchair–Exoskeleton Hybrid Robot for Assisting Human Locomotion. Robotics 2023, 12, 16. [Google Scholar] [CrossRef]
- Safdar, M. Biomechatronics: Its Introduction and Working, Biotech Articles. 2011. Available online: https://www.biotecharticles.com/Biology-Article/Biomechatronics-Its-Introduction-and-Working-678.html (accessed on 1 July 2022).
- AZO Robotics. An Introduction to Biomechatronics. 2012. Available online: https://www.azorobotics.com/Article.aspx?ArticleID=48 (accessed on 1 July 2022).
- Mohebbi, A. Human-robot interaction in rehabilitation and assistance: A review. Curr. Robot. Rep. 2020, 1, 131–144. [Google Scholar] [CrossRef]
- Giggins, O.M.; Persson, U.M.; Caulfield, B. Biofeedback in rehabilitation. J. Neuroeng. Rehabil. 2013, 10, 60. [Google Scholar] [CrossRef] [PubMed]
- Van Rooij, M.; Lobel, A.; Harris, O.; Smit, N.; Granic, I. DEEP: A biofeedback virtual reality game for children at-risk for anxiety. In Proceedings of the 2016 CHI Conference Extended Abstracts on Human Factors in Computing Systems, San Jose, CA, USA, 7–12 May 2016; pp. 1989–1997. [Google Scholar]
- Lüddecke, R.; Felnhofer, A. Virtual reality biofeedback in health: A scoping review. Appl. Psychophysiol. Biofeedback 2022, 47, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Bencsik, A.L.; Lendvay, M. Development trends in bio-mechatronics. In Proceedings of the 2016 IEEE 14th International Symposium on Intelligent Systems and Informatics (SISY), Subotica, Serbia, 29–31 August 2016; pp. 117–122. [Google Scholar]
- Junaid, A.B.; Afzal, M.R.; Rasheed, T.; Tahir, S.; Ahmed, S.; Sohail, M.; Ali, M. Design and control of artificial robotic hand. In Proceedings of the 2014 International Conference on Robotics and Emerging Allied Technologies in Engineering (iCREATE), Islamabad, Pakistan, 22–24 April 2014; pp. 10–15. [Google Scholar]
- Li, Z.; Yang, C.; Burdet, E. Guest editorial an overview of biomedical robotics and bio-mechatronics systems and applications. IEEE Trans. Syst. Man Cybern. Syst. 2016, 46, 869–874. [Google Scholar] [CrossRef]
- Katt, B.; Imbergamo, C.; Seigerman, D.; Rivlin, M.; Beredjiklian, P.K. The use of 3D printed customized casts in children with upper extremity fractures: A report of two cases. Arch. Bone Jt. Surg. 2021, 9, 126. [Google Scholar]
- Banga, H.K.; Kalra, P.; Belokar, R.M.; Kumar, R. Customized design and additive manufacturing of kids’ ankle foot orthosis. Rapid Prototyp. J. 2020, 26, 1677–1685. [Google Scholar] [CrossRef]
- Venumbaka, S.A.; Covarubias, M.; Cesaro, G.; Ronca, A.; De Capitani, C.; Ambrosio, L.; Sorrentino, A. Application of multi materials additive manufacturing technique in the design and manufacturing of hand orthoses. In Proceedings of the Computers Helping People with Special Needs: 17th International Conference, ICCHP 2020, Lecco, Italy, 9–11 September 2020; Proceedings, Part II 17. Springer: Cham, Switzerland, 2020; pp. 461–468. [Google Scholar]
- Dubey, N.K.; Gangwar, S. Comparative Analysis of Different Composites for Ankle Foot Orthosis: A Review. In Advances in Engineering Materials: Select Proceedings of FLAME 2020; Springer: Singapore, 2021; pp. 305–317. [Google Scholar]
- Ganesan, S.; Ranganathan, R. Design and development of customized elbow orthosis using additive manufacturing. Proc. Inst. Mech. Eng. Part L J. Mater. Des. Appl. 2023, 2023, 14644207231158936. [Google Scholar] [CrossRef]
- Choo, Y.J.; Boudier-Revéret, M.; Chang, M.C. 3D printing technology applied to orthosis manufacturing: Narrative review. Ann. Palliat. Med. 2020, 9, 4262–4270. [Google Scholar] [CrossRef]
- Górski, F.; Zawadzki, P.; Wichniarek, R.; Kuczko, W.; Żukowska, M.; Wesołowska, I.; Wierzbicka, N. Automated design of customized 3D-printed wrist orthoses on the basis of 3D scanning. In Computational and Experimental Simulations in Engineering: Proceedings of ICCES2019 24 (Tokyo, Japan, 25–28 March 2019); Springer: Cham, Switzerland, 2020; pp. 1133–1143. [Google Scholar]
- Kesner, S.B.; Jentoft, L.; Hammond, F.L.; Howe, R.D.; Popovic, M. Design considerations for an active soft orthotic system for shoulder rehabilitation. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 8130–8134. [Google Scholar]
- Banga, H.K.; Kalra, P.; Belokar, R.M.; Kumar, R. Design and fabrication of prosthetic and orthotic product by 3D printing. In Prosthetics and Orthotics; IntechOpen: London, UK, 2020. [Google Scholar]
- Oud, T.A.M.; Lazzari, E.; Gijsbers, H.J.H.; Gobbo, M.; Nollet, F.; Brehm, M.A. Effectiveness of 3D-printed orthoses for traumatic and chronic hand conditions: A scoping review. PLoS ONE 2021, 16, e0260271. [Google Scholar] [CrossRef]
- Schwartz, D.A.; Schofield, K.A. Utilization of 3D printed orthoses for musculoskeletal conditions of the upper extremity: A systematic review. J. Hand Ther. 2021, 36, 166–178. [Google Scholar] [CrossRef] [PubMed]
- Damiao, J.; Calianese, N.; Cartwright, D.; Cherian, C.; Lee, E.; Mucek, D. Comparison of 3D Printing and Traditional Hand Orthosis Fabrication. Glob. J. Health Sci. 2023, 15, 1–42. [Google Scholar] [CrossRef]
- Rodrigues, A.C.T.; Garcez, L.V.M.; Medola, F.O.; Baleotti, L.R.; Sandnes, F.E.; Vaezipour, A. A Systematic Review of Differences Between Conventional Orthoses and 3D-Printed Orthoses. In Advances in Manufacturing, Production Management and Process Control, Proceedings of the AHFE 2021 Virtual Conferences on Human Aspects of Advanced Manufacturing, Advanced Production Management and Process Control, and Additive Manufacturing, Modeling Systems and 3D Prototyping, USA, 25–29 July 2021; Springer: Berlin/Heidelberg, Germany, 2021; pp. 53–60. [Google Scholar]
- Jiang, H.; Vimalesvaran, S.; Wang, J.K.; Lim, K.B.; Mogali, S.R.; Car, L.T. Virtual reality in medical students’ education: Scoping review. JMIR Med. Educ. 2022, 8, e34860. [Google Scholar] [CrossRef] [PubMed]
- Pregowska, A.; Osial, M.; Dolega-Dolegowski, D.; Kolecki, R.; Proniewska, K. Information and communication technologies combined with mixed reality as supporting tools in medical education. Electronics 2022, 11, 3778. [Google Scholar] [CrossRef]
- Sainsbury, B.; Wilz, O.; Ren, J.; Green, M.; Fergie, M.; Rossa, C. Preoperative Virtual Reality Surgical Rehearsal of Renal Access during Percutaneous Nephrolithotomy: A Pilot Study. Electronics 2022, 11, 1562. [Google Scholar] [CrossRef]
- Patle, D.S.; Manca, D.; Nazir, S.; Sharma, S. Operator training simulators in virtual reality environment for process operators: A review. Virtual Real. 2019, 23, 293–311. [Google Scholar] [CrossRef]
- Xie, B.; Liu, H.; Alghofaili, R.; Zhang, Y.; Jiang, Y.; Lobo, F.D.; Yu, L.F. A review on virtual reality skill training applications. Front. Virtual Real. 2021, 2, 645153. [Google Scholar] [CrossRef]
- Hauschild, M.; Davoodi, R.; Loeb, G.E. A virtual reality environment for designing and fitting neural prosthetic limbs. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 9–15. [Google Scholar] [CrossRef]
- Levac, D.; Miller, P.; Missiuna, C. Usual and virtual reality video game-based physiotherapy for children and youth with acquired brain injuries. Phys. Occup. Ther. Pediatr. 2012, 32, 180–195. [Google Scholar] [CrossRef]
- Boian, R.; Sharma, A.; Han, C.; Merians, A.; Burdea, G.; Adamovich, S.; Recce, M.; Tremaine, M.; Poizner, H. Virtual reality-based post-stroke hand rehabilitation. In Medicine Meets Virtual Reality 02/10; IOS Press: Amsterdam, The Netherlands, 2002; pp. 64–70. [Google Scholar]
- Eng, K.; Siekierka, E.; Cameirao, M.; Zimmerli, L.; Pyk, P.; Duff, A.; Verschure, P.F.M.J. Cognitive virtual-reality based stroke rehabilitation. In World Congress on Medical Physics and Biomedical Engineering 2006; Springer: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Brunner, I.; Skouen, J.S.; Hofstad, H.; Aßmus, J.; Becker, F.; Sanders, A.M.; Verheyden, G. Virtual reality training for upper extremity in subacute stroke (VIRTUES): A multicenter RCT. Neurology 2017, 89, 2413–2421. [Google Scholar] [CrossRef]
- Van Vugt, F.T.; Boullet, L.; Jabusch, H.C.; Altenmüller, E. Musician’s dystonia in pianists: Long-term evaluation of retraining and other therapies. Park. Relat. Disord. 2014, 20, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Waszczykowski, M.; Dziankowska-Bartkowiak, B.; Podgórski, M.; Fabiś, J.; Waszczykowska, A. Role and effectiveness of complex and supervised rehabilitation on overall and hand function in systemic sclerosis patients—One-year follow-up study. Sci. Rep. 2021, 11, 15174. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Otaka, Y.; Osu, R.; Kumagai, M.; Kitamura, S.; Yaeda, J. Motivation for rehabilitation in patients with subacute stroke: A qualitative study. Front. Rehabil. Sci. 2021, 2, 664758. [Google Scholar] [CrossRef] [PubMed]
- Górski, F.; Wichniarek, R.; Kuczko, W.; Żukowska, M.; Lulkiewicz, M.; Zawadzki, P. Experimental studies on 3D printing of automatically designed customized wrist-hand orthoses. Materials 2020, 13, 4091. [Google Scholar] [CrossRef]
- Zawadzki, P.; Wichniarek, R.; Kuczko, W.; Slupińska, S.; Żukowska, M. Automated Design and Rapid Manufacturing of Low-Cost Customized Upper Limb Prostheses. J. Phys. Conf. Ser. 2022, 2198, 012040. [Google Scholar]
- Górski, F.; Łabudzki, R.; Żukowska, M.; Sanfilippo, F.; Ottestad, M.; Zelenay, M.; Pacurar, R. Experimental Evaluation of Extended Reality Technologies in the Development of Individualized Three-Dimensionally Printed Upper Limb Prostheses. Appl. Sci. 2023, 13, 8035. [Google Scholar] [CrossRef]
- Górski, F.; Żukowska, M.; Kuczko, W.; Wichniarek, R.; Siwiec, S. Automated Design and 3D Printing of Therapeutic Wrist Hand Orthosis. In Proceedings of the HealthTech Innovation Conference, Zabrze, Poland, 10–11 October 2022. [Google Scholar]














| ID | Question | Avg. | Std. Dev. |
|---|---|---|---|
| VR1 | I feel my muscles warming up. | 4.08 | 0.51 |
| VR2 | I feel muscle fatigue. | 2.42 | 1.08 |
| VR3 | The application is more interesting than classic training. | 4.67 | 0.65 |
| VR4 | I feel that I would exercise more often if I had constant access to the presented system. | 4.33 | 0.98 |
| VR5 | Using the application was pleasant and simple. | 3.83 | 1.03 |
| VR6 | The exercises were engaging but possible to perform correctly. | 4.25 | 0.62 |
| VR7 | The level of graphic quality was sufficient. | 4.75 | 0.45 |
| VR8 | Interacting with objects was intuitive and easy to learn. | 3.50 | 1.00 |
| ID | Question | Average | Deviation |
|---|---|---|---|
| C1 | The controller is comfortable. | 3.42 | 0.90 |
| C2 | I like this controller solution. | 4.08 | 1.00 |
| C3 | I believe this controller is better for this specific use than the classic one. | 4.17 | 0.72 |
| C4 | The response speed to signals from the controller was sufficient. | 4.00 | 0.74 |
| C5 | Using the controller was pleasant and simple. | 3.50 | 1.24 |
| C6 | Interacting with objects using the controller was intuitive and easy to learn. | 3.75 | 1.06 |
| Total average | 3.82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Górski, F.; Grohs, A.; Kuczko, W.; Żukowska, M.; Wichniarek, R.; Siwiec, S.; Băilă, D.-I.; Zelenay, M.; Păcurar, R.; Sanfilippo, F. Development and Studies of VR-Assisted Hand Therapy Using a Customized Biomechatronic 3D Printed Orthosis. Electronics 2024, 13, 79. https://doi.org/10.3390/electronics13010079
Górski F, Grohs A, Kuczko W, Żukowska M, Wichniarek R, Siwiec S, Băilă D-I, Zelenay M, Păcurar R, Sanfilippo F. Development and Studies of VR-Assisted Hand Therapy Using a Customized Biomechatronic 3D Printed Orthosis. Electronics. 2024; 13(1):79. https://doi.org/10.3390/electronics13010079
Chicago/Turabian StyleGórski, Filip, Aleksandra Grohs, Wiesław Kuczko, Magdalena Żukowska, Radosław Wichniarek, Sabina Siwiec, Diana-Irinel Băilă, Martin Zelenay, Răzvan Păcurar, and Filippo Sanfilippo. 2024. "Development and Studies of VR-Assisted Hand Therapy Using a Customized Biomechatronic 3D Printed Orthosis" Electronics 13, no. 1: 79. https://doi.org/10.3390/electronics13010079









