Measuring Spatial Accessibility of Healthcare Facilities in Marinduque, Philippines
Abstract
:1. Introduction
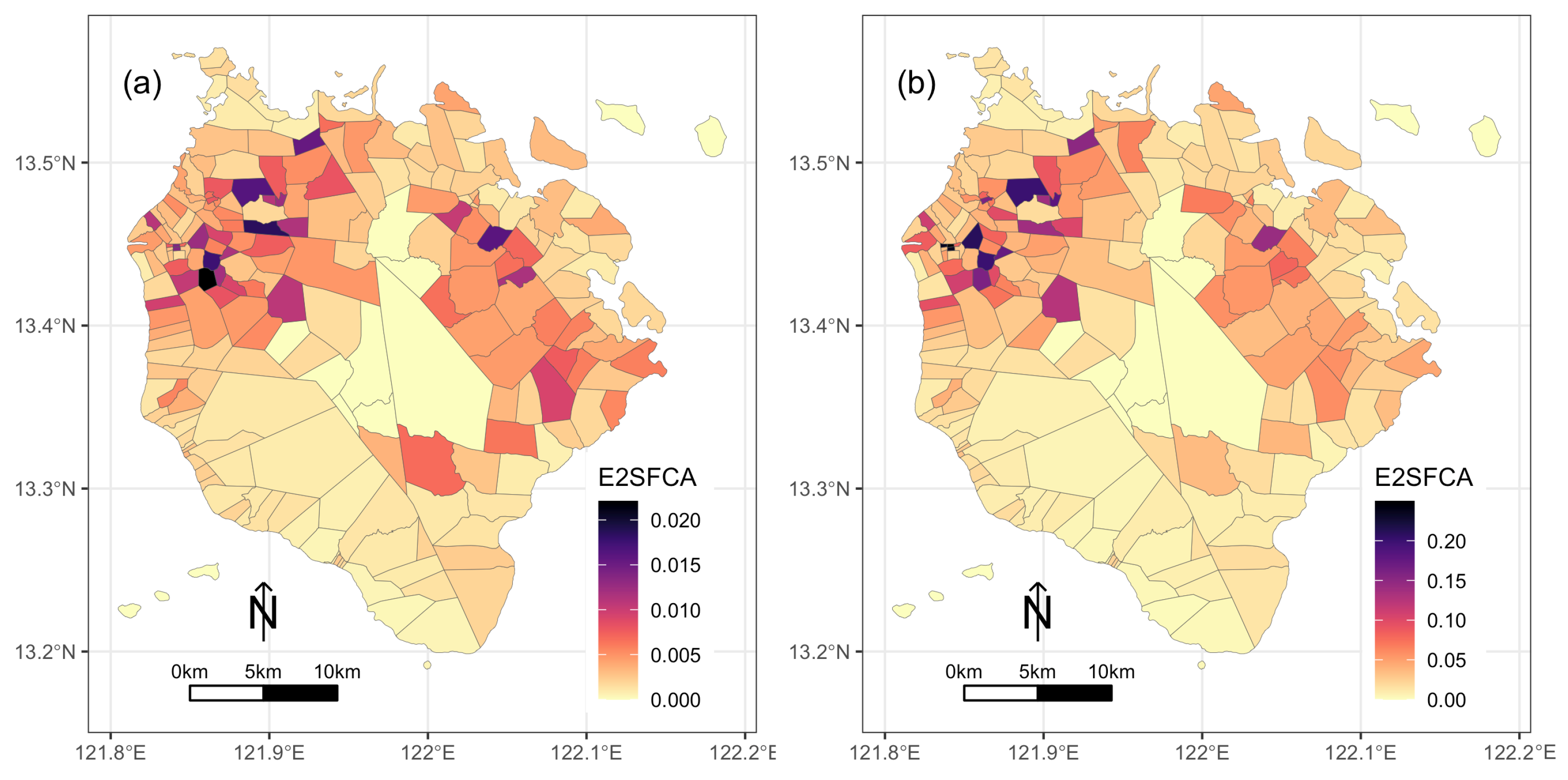
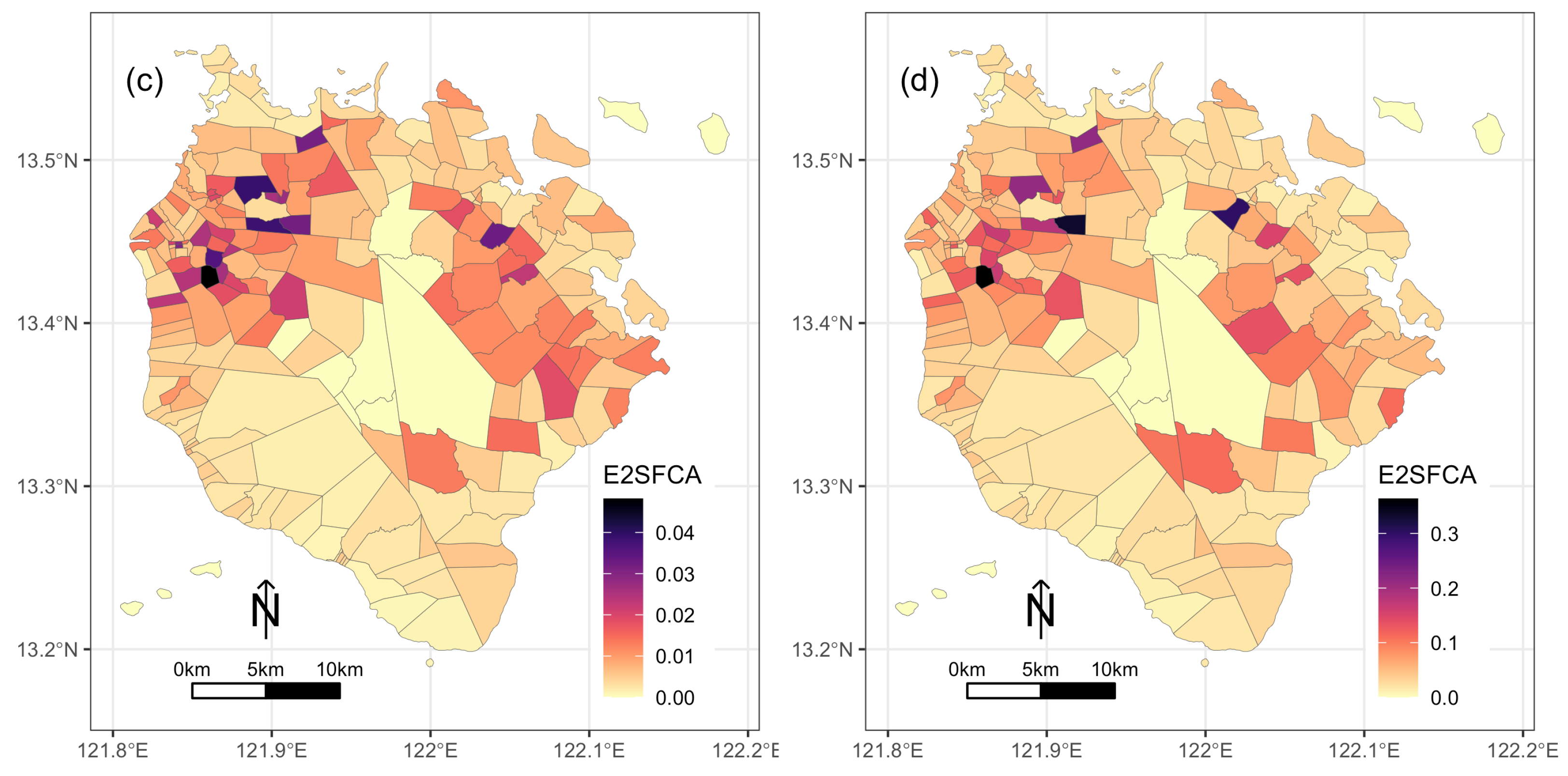
2. Materials and Methods
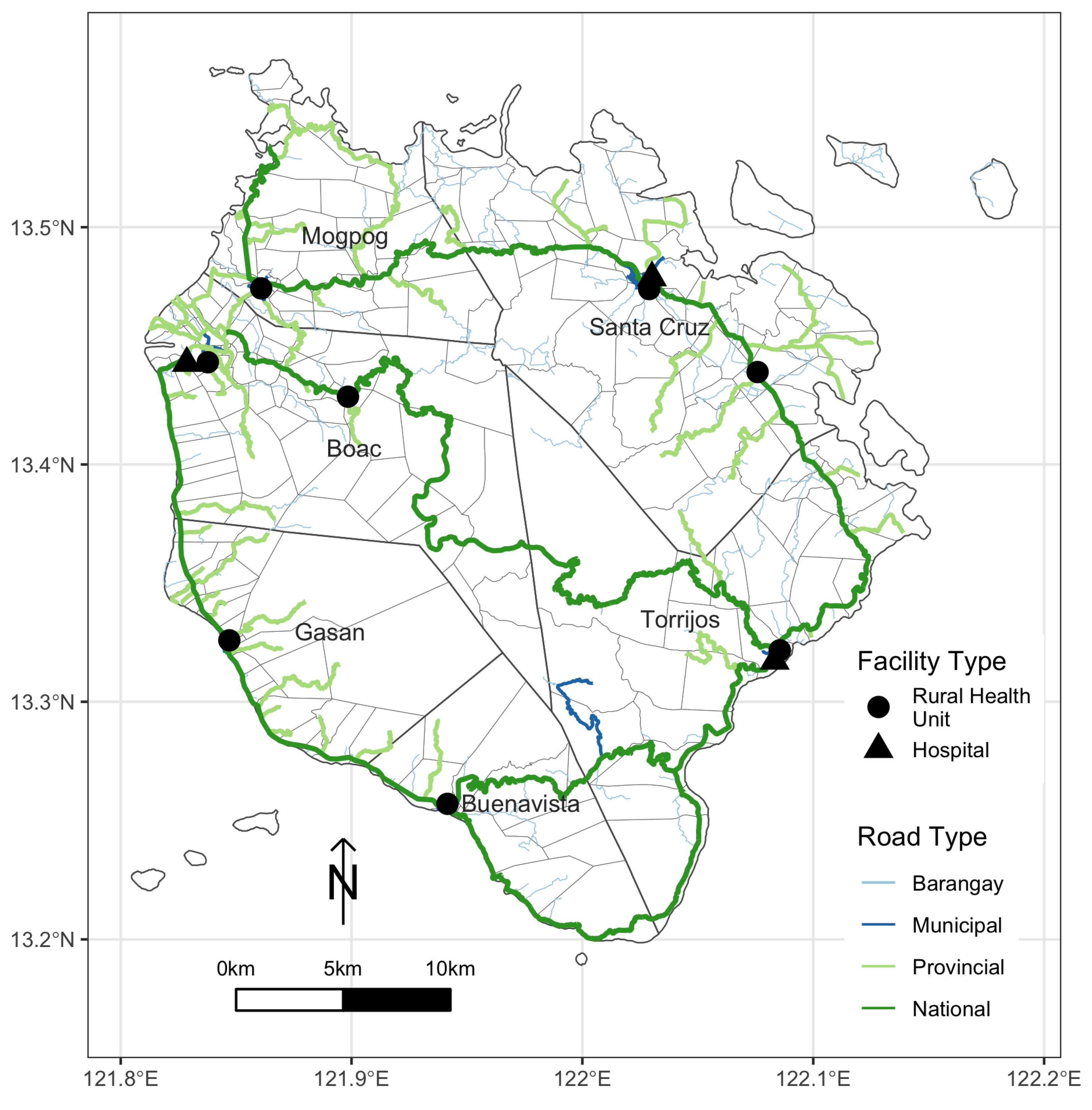
2.1. Study Area
2.2. Data
2.3. Distance and Travel Time Measurement
2.4. E2SFCA
3. Results
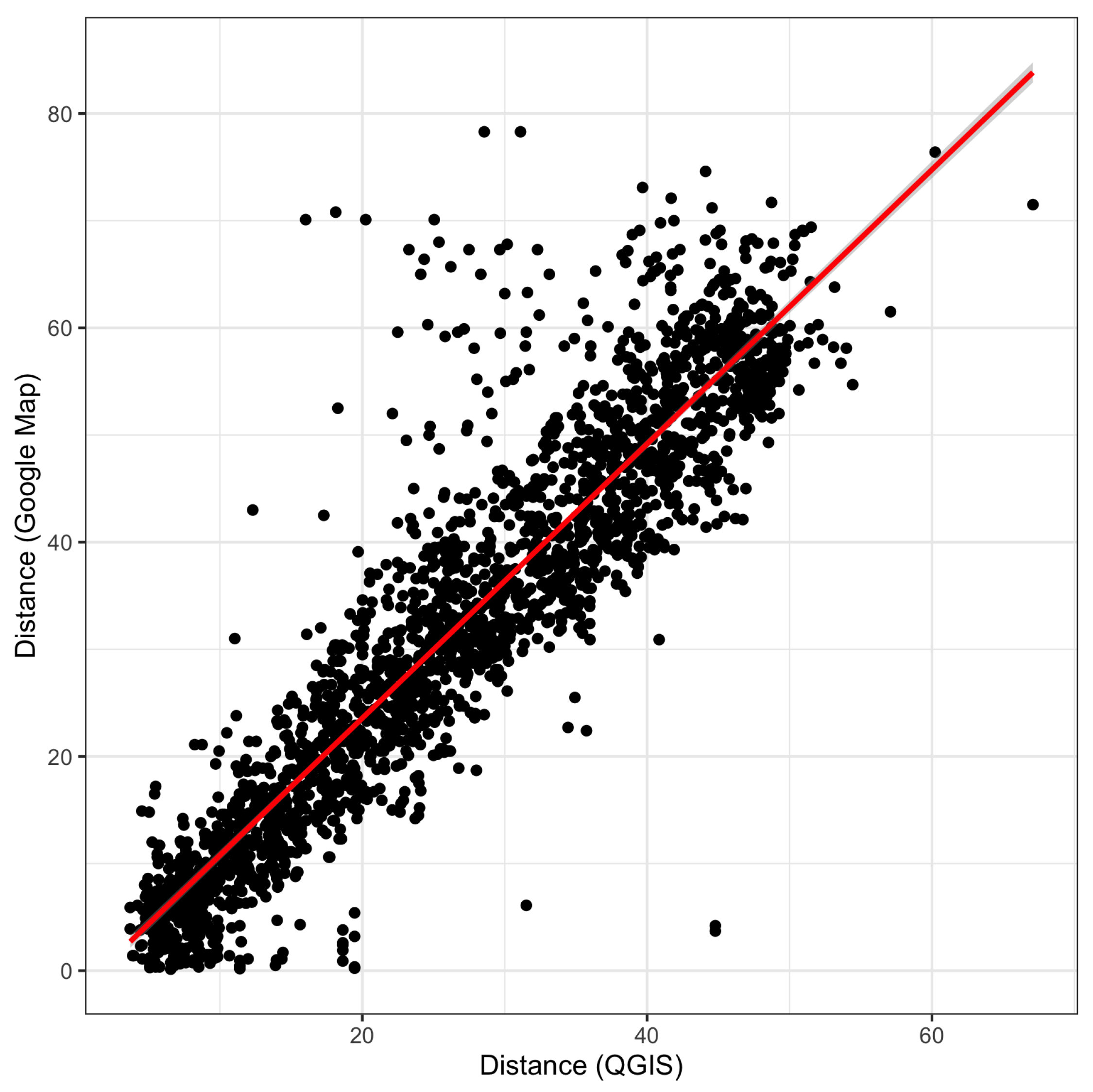
3.1. Distance Measurement
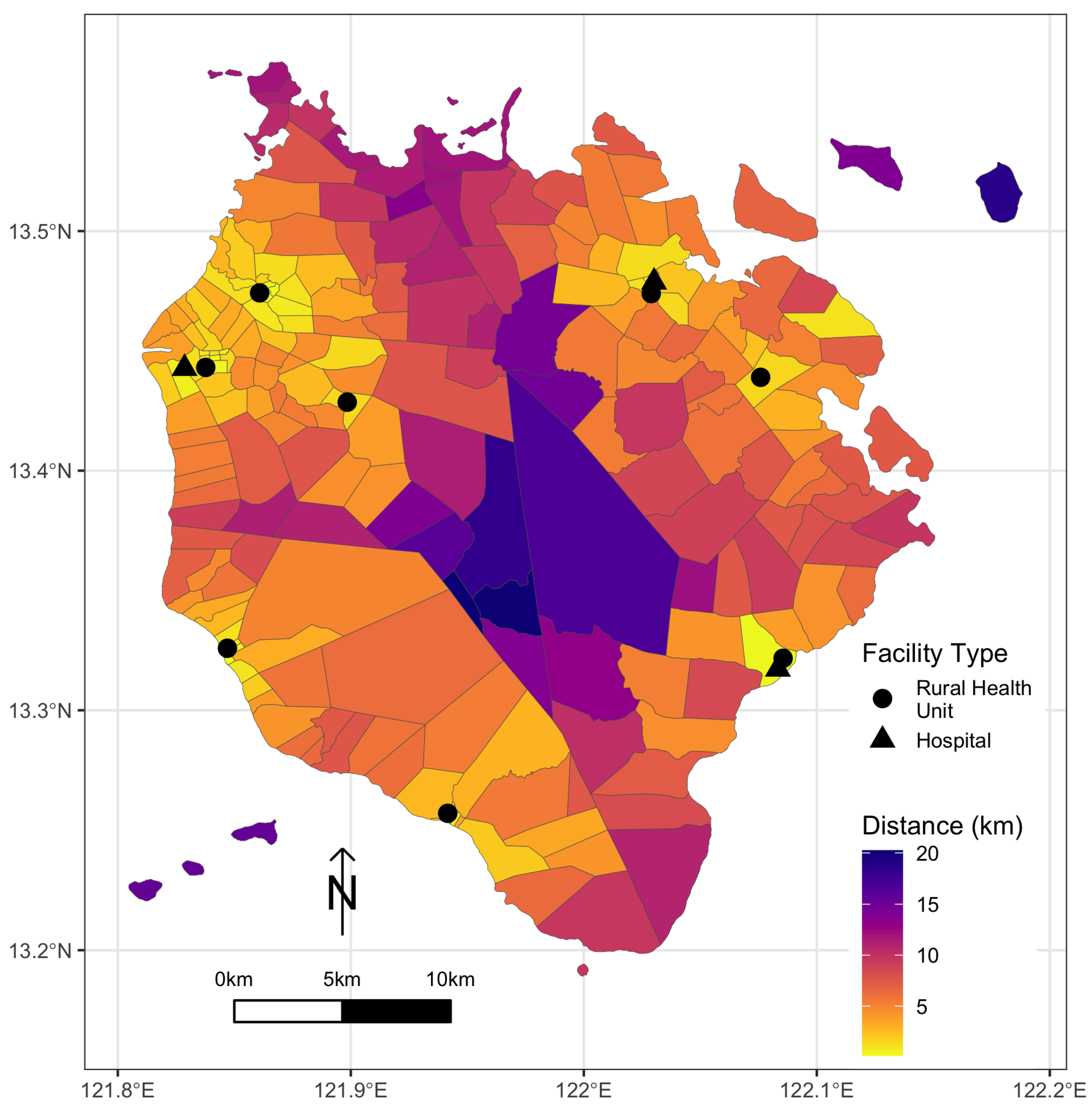
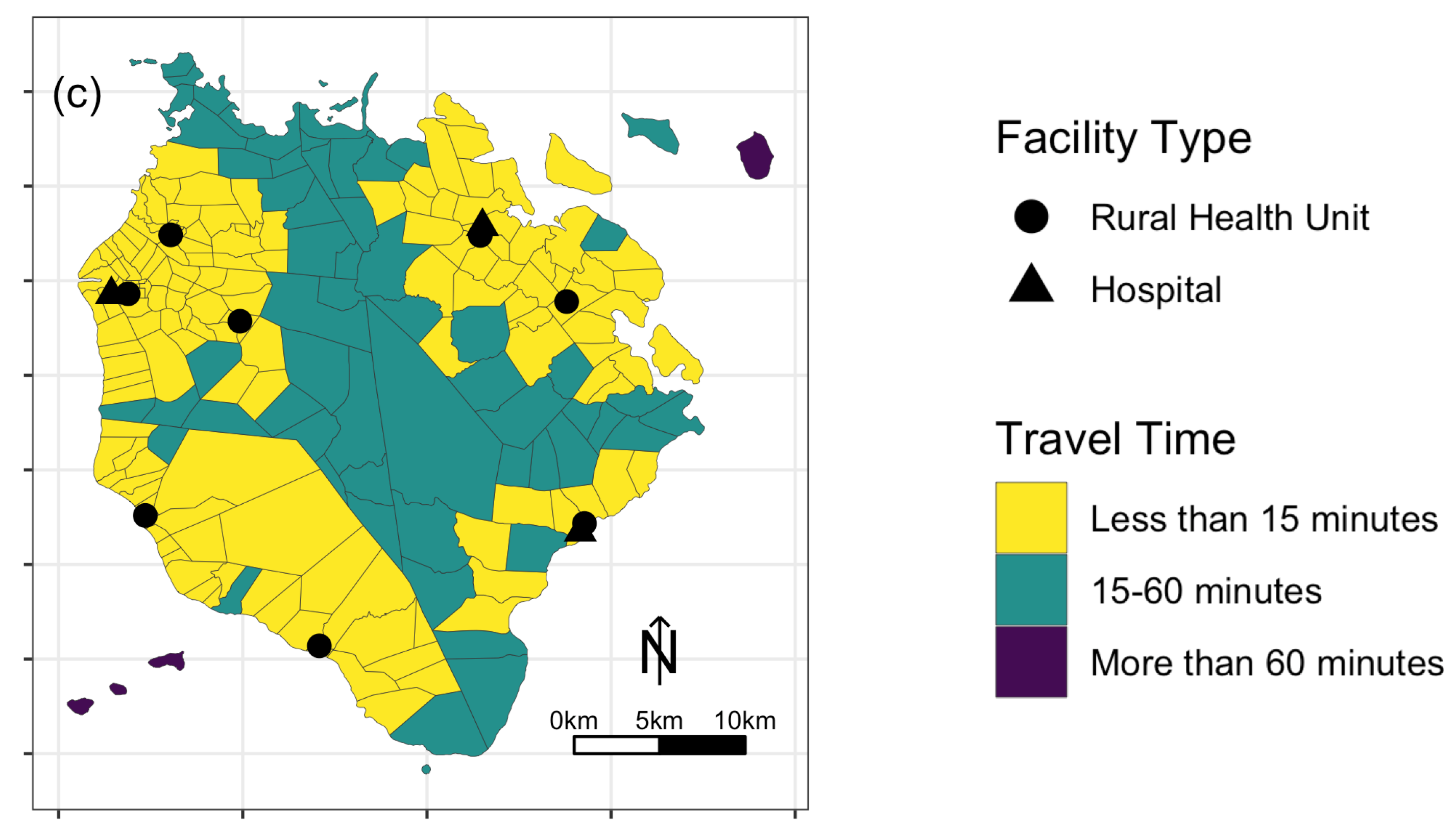
3.2. Minimum Distance and Travel Time
3.3. Accessibility Scores
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dodd, W.; Kipp, A.; Nicholson, B.; Lau, L.L.; Little, M.; Walley, J.; Wei, X. Governance of community health worker programs in a decentralized health system: A qualitative study in the Philippines. BMC Health Serv. Res. 2021, 21, 451. [Google Scholar] [CrossRef] [PubMed]
- Eckermann, E. SDG 3: A Missed Opportunity to Transform Understandings and Monitoring of Health, Well-Being and Development? Appl. Res. Qual. Life 2018, 13, 261–272. [Google Scholar] [CrossRef]
- Lawal, O.; Anyiam, F.E. Modelling geographic accessibility to Primary Health Care Facilities: Combining open data and geospatial analysis. Geo-Spat. Inf. Sci. 2019, 22, 174–184. [Google Scholar] [CrossRef] [Green Version]
- Palozzi, G.; Schettini, I.; Chirico, A. Enhancing the Sustainable Goal of Access to Healthcare: Findings from a Literature Review on Telemedicine Employment in Rural Areas. Sustainability 2020, 12, 3318. [Google Scholar] [CrossRef] [Green Version]
- Guégan, J.F.; Suzán, G.; Kati-Coulibaly, S.; Bonpamgue, D.N.; Moatti, J.P.; Guégan, J.F.; Suzán, G.; Kati-Coulibaly, S.; Bonpamgue, D.N.; Moatti, J.P. Sustainable Development Goal #3, “health and well-being”, and the need for more integrative thinking. Vet. México OA 2018, 5. [Google Scholar] [CrossRef]
- Havea, P.; Hemstock, S.; des Combes, H. Improving health and well-being through climate change adaptation. In Advances in Health and Disease; Nova Science Publishers, Inc.: Hauppauge, NY, USA, 2018; Volume 4, pp. 215–230. [Google Scholar]
- Liu, R.; Dong, X.; Wang, X.C.; Zhang, P.; Liu, M.; Zhang, Y. Study on the relationship among the urbanization process, ecosystem services and human well-being in an arid region in the context of carbon flow: Taking the Manas river basin as an example. Ecol. Indic. 2021, 132, 108248. [Google Scholar] [CrossRef]
- Levesque, J.F.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef] [Green Version]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, W.; Qi, Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 1100–1107. [Google Scholar] [CrossRef]
- Evans, D.B.; Hsu, J.; Boerma, T. Universal health coverage and universal access. Bull. World Health Organ. 2013, 91, 546-546A. [Google Scholar] [CrossRef]
- McGrail, M.R.; Humphreys, J.S. The index of rural access: An innovative integrated approach for measuring primary care access. BMC Health Serv. Res. 2009, 9, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woolley, T.; Cristobal, F.; Siega-Sur, J.; Ross, S.; Neusy, A.J.; Halili, S.; Reeve, C. Positive implications from socially accountable, community-engaged medical education across two Philippines regions. Rural Remote Health 2018, 18, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Comber, A.J.; Brunsdon, C.; Radburn, R. A spatial analysis of variations in health access: Linking geography, socio-economic status and access perceptions. Int. J. Health Geogr. 2011, 10, 44. [Google Scholar] [CrossRef] [Green Version]
- Al-Taiar, A.; Clark, A.; Longenecker, J.C.; Whitty, C.J. Physical accessibility and utilization of health services in Yemen. Int. J. Health Geogr. 2010, 9, 38. [Google Scholar] [CrossRef] [Green Version]
- Luo, W.; Wang, F. Spatial accessibility to primary care and physician shortage area designation: A case study in Illinois with GIS approaches. Geogr. Inf. Syst. Health Appl. 2003, 260–278. [Google Scholar]
- Wang, X.; Yang, H.; Duan, Z.; Pan, J. Spatial accessibility of primary health care in China: A case study in Sichuan Province. Soc. Sci. Med. 2018, 209, 14–24. [Google Scholar] [CrossRef]
- Pu, Q.; Yoo, E.H.; Rothstein, D.H.; Cairo, S.; Malemo, L. Improving the spatial accessibility of healthcare in North Kivu, Democratic Republic of Congo. Appl. Geogr. 2020, 121, 102262. [Google Scholar] [CrossRef]
- Delamater, P.L.; Messina, J.P.; Shortridge, A.M.; Grady, S.C. Measuring geographic access to health care: Raster and network-based methods. Int. J. Health Geogr. 2012, 11, 15. [Google Scholar] [CrossRef] [Green Version]
- Peters, D.H.; Garg, A.; Bloom, G.; Walker, D.G.; Brieger, W.R.; Rahman, M.H. Poverty and Access to Health Care in Developing Countries. Ann. N. Y. Acad. Sci. 2008, 1136, 161–171. [Google Scholar] [CrossRef]
- Noor, A.M.; Zurovac, D.; Hay, S.I.; Ochola, S.A.; Snow, R.W. Defining equity in physical access to clinical services using geographical information systems as part of malaria planning and monitoring in Kenya. Trop. Med. Int. Health 2003, 8, 917–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mclafferty, S.; Williamson, D.; McGuire, P.G. Identifying Crime Hot Spots Using Kernel Smoothing. In Analyzing Crime Patterns: Frontiers of Practice; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2000; pp. 77–86. [Google Scholar] [CrossRef]
- dos Anjos Luis, A.; Cabral, P. Geographic accessibility to primary healthcare centers in Mozambique. Int. J. Equity Health 2016, 15, 173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathon, D.; Apparicio, P.; Lachapelle, U. Cross-border spatial accessibility of health care in the North-East Department of Haiti. Int. J. Health Geogr. 2018, 17, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul, J.; Edwards, E. Temporal availability of public health care in developing countries of the Caribbean: An improved two-step floating catchment area method for estimating spatial accessibility to health care. Int. J. Health Plan. Manag. 2019, 34, e536–e556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verma, V.R.; Dash, U. Geographical accessibility and spatial coverage modelling of public health care network in rural and remote India. PLoS ONE 2020, 15, e0239326. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, M.; Malik, N. Spatial distribution and accessibility to public sector tertiary care teaching general hospitals: Tale of Two Khyber Pakhtunkhwa districts—Peshawar and Abbottabad. J. Coll. Physicians Surg. Pak. 2019, 29, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Bakar, M.; Samat, N.; Yaacob, N. Spatial accessibility to health care services among children with cerebral palsy in Johor, Peninsular Malaysia. Geospat. Health 2021, 16, 987. [Google Scholar] [CrossRef]
- Fransen, K.; Neutens, T.; De Maeyer, P.; Deruyter, G. A commuter-based two-step floating catchment area method for measuring spatial accessibility of daycare centers. Health Place 2015, 32, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Radke, J.; Mu, L. Spatial decompositions, modeling and mapping service regions to predict access to social programs. Geogr. Inf. Sci. 2000, 6, 105–112. [Google Scholar] [CrossRef]
- Luo, W.; Wang, F. Measures of Spatial Accessibility to Health Care in a GIS Environment: Synthesis and a Case Study in the Chicago Region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, T.; Nakamura, A.; Mukuda, K.; Harada, M.; Kotani, K. Potential accessibility scores for hospital care in a province of Japan: GIS-based ecological study of the two-step floating catchment area method and the number of neighborhood hospitals. BMC Health Serv. Res. 2017, 17, 438. [Google Scholar] [CrossRef] [PubMed]
- Thind, A.; Cruz, A.M. Determinants of Children’s Health Services Utilization in the Philippines. J. Trop. Pediatr. 2003, 49, 269–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dror, D.M.; Soriano, E.S.; Lorenzo, M.E.; Sarol, J.N.; Azcuna, R.S.; Koren, R. Field based evidence of enhanced healthcare utilization among persons insured by micro health insurance units in Philippines. Health Policy 2005, 73, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Quimbo, S.A.; Peabody, J.W.; Shimkhada, R.; Florentino, J.; Solon, O. Evidence of a causal link between health outcomes, insurance coverage, and a policy to expand access: Experimental data from children in the Philippines. Health Econ. 2011, 20, 620–630. [Google Scholar] [CrossRef] [PubMed]
- Gouda, H.; Hodge, A.; Bermejo, R., III; Zeck, W.; Jimenez-Soto, E. The impact of healthcare insurance on the utilisation of facility-based delivery for childbirth in the philippines. PLoS ONE 2016, 11, e0167268. [Google Scholar] [CrossRef] [PubMed]
- Bondy, J.N.; Thind, A.; Koval, J.J.; Speechley, K.N. Identifying the determinants of childhood immunization in the Philippines. Vaccine 2009, 27, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, M. Access to Diabetes Care and Medicines in the Philippines. Asia Pac. J. Public Health 2010, 22, 96S–102S. [Google Scholar] [CrossRef]
- Kim, S.A.; Capeding, M.R.Z.; Kilgore, P.E. Factors influencing healthcare utilization among children with pneumonia in Muntinlupa City, the Philippines. Southeast Asian J. Trop. Med. Public Health 2014, 45, 727–735. [Google Scholar]
- Salvacion, A. Exploring Determinants of Child Malnutrition in Marinduque Island, Philippines. Hum. Ecol. 2017, 45, 853–863. [Google Scholar] [CrossRef]
- Salvacion, A.R. Spatial pattern and determinants of village level poverty in Marinduque Island, Philippines. GeoJournal 2020, 85, 257–267. [Google Scholar] [CrossRef]
- Lutero, D.S.; Cerilo, G.E.A.; Eustaquio, A.M.; Buhat, C.A.H.; Nazareno, A.O.; Nazareno, A.L.; Salvacion, A.R. Optimal route planning for day tours in Marinduque, Philippines. Spat. Inf. Res. 2022, 30, 205–214. [Google Scholar] [CrossRef]
- Salvacion, A. Mapping land limitations for agricultural land use planning using fuzzy logic approach: A case study for Marinduque Island, Philippines. GeoJournal 2021, 86, 915–925. [Google Scholar] [CrossRef]
- Reyes, C.; Due, E. Fighting Poverty with Facts Community-Based Monitoring Systems; International Development Research Centre: Ottawa, ON, Canada, 2009. [Google Scholar]
- Reyes, C.; Mandap, A.; Quilitis, J.; Calubayan, S.; Nabiong, J.; Adudar, R.; Binas, V.; Bacud, E.; Moreto, J. The Many Faces of Poverty: Volume 8. Technical Report; De La Salle University: Manila, Philippines, 2017. [Google Scholar]
- Duran-Fernandez, R.; Santos, G. Gravity, distance, and traffic flows in Mexico. Res. Transp. Econ. 2014, 46, 30–35. [Google Scholar] [CrossRef]
- Wu, J.; Cai, Z.; Li, H. Accessibility of Medical Facilities in Multiple Traffic Modes: A Study in Guangzhou, China. Complexity 2020, 2020, e8819836. [Google Scholar] [CrossRef]
- Zhuge, C.; Shao, C.; Li, X.; Yu, M. Commuter’s choice behavior of travel time and travel mode. J. Transp. Syst. Eng. Inf. Technol. 2012, 12, 126–131. [Google Scholar]
- Wang, F.; Xu, Y. Estimating O–D travel time matrix by Google Maps API: Implementation, advantages, and implications. Ann. GIS 2011, 17, 199–209. [Google Scholar] [CrossRef]
- Weinhold, I.; Gurtner, S. Understanding shortages of sufficient health care in rural areas. Health Policy 2014, 118, 201–214. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Jaffrelot, M.; Deguen, S. Measuring hospital spatial accessibility using the enhanced two-step floating catchment area method to assess the impact of spatial accessibility to hospital and non-hospital care on the length of hospital stay. BMC Health Serv. Res. 2021, 21, 1078. [Google Scholar] [CrossRef]
- Rukmana, D. Vulnerable Populations. In Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 6989–6992. [Google Scholar] [CrossRef]



| Name | Municipality |
|---|---|
| Boach RHU1 | Boac |
| Boach RHU2 | Boac |
| Dr. Damian Reyes Memorial Hospital | Boac |
| Buenavista RHU | Buenavista |
| Gasan RHU | Gasan |
| Mogpog RHU | Mogpog |
| Sta. Cruz RHU1 | Sta. Cruz |
| Sta. Cruz RHU2 | Sta. Cruz |
| Sta. Cruz District Hospital | Sta. Cruz |
| Torrijos RHU | Torrijos |
| Torrijos Municipal Hospital | Torrijos |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salvacion, A.R. Measuring Spatial Accessibility of Healthcare Facilities in Marinduque, Philippines. ISPRS Int. J. Geo-Inf. 2022, 11, 516. https://doi.org/10.3390/ijgi11100516
Salvacion AR. Measuring Spatial Accessibility of Healthcare Facilities in Marinduque, Philippines. ISPRS International Journal of Geo-Information. 2022; 11(10):516. https://doi.org/10.3390/ijgi11100516
Chicago/Turabian StyleSalvacion, Arnold R. 2022. "Measuring Spatial Accessibility of Healthcare Facilities in Marinduque, Philippines" ISPRS International Journal of Geo-Information 11, no. 10: 516. https://doi.org/10.3390/ijgi11100516







