Pitch and Flat Roof Factors’ Association with Spatiotemporal Patterns of Dengue Disease Analysed Using Pan-Sharpened Worldview 2 Imagery
Abstract
:1. Introduction
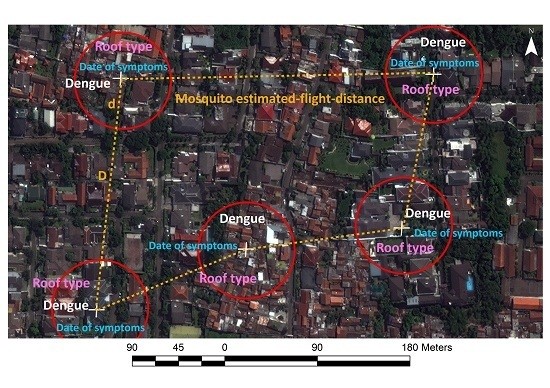
2. Methods
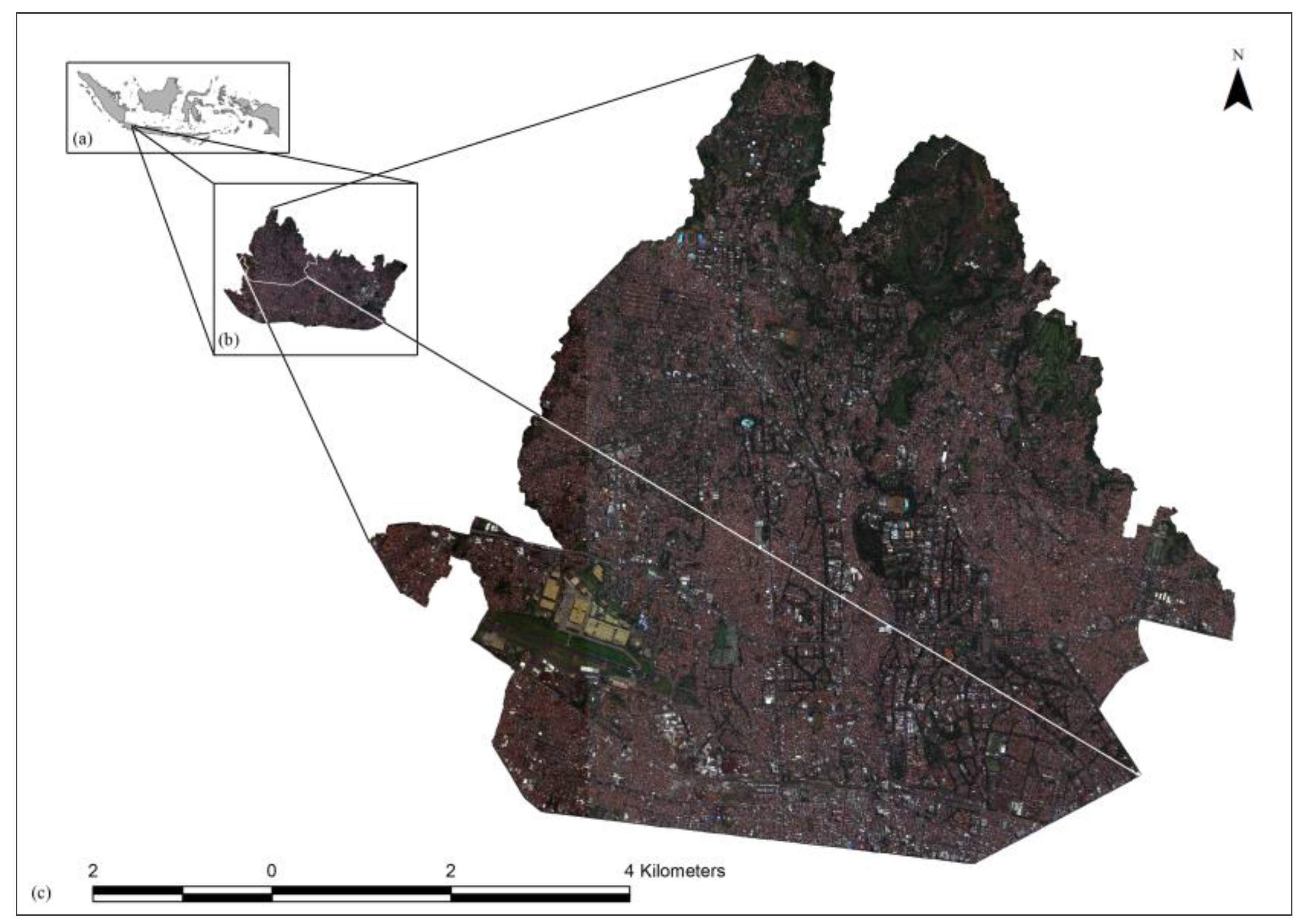
2.1. Study Area and Data
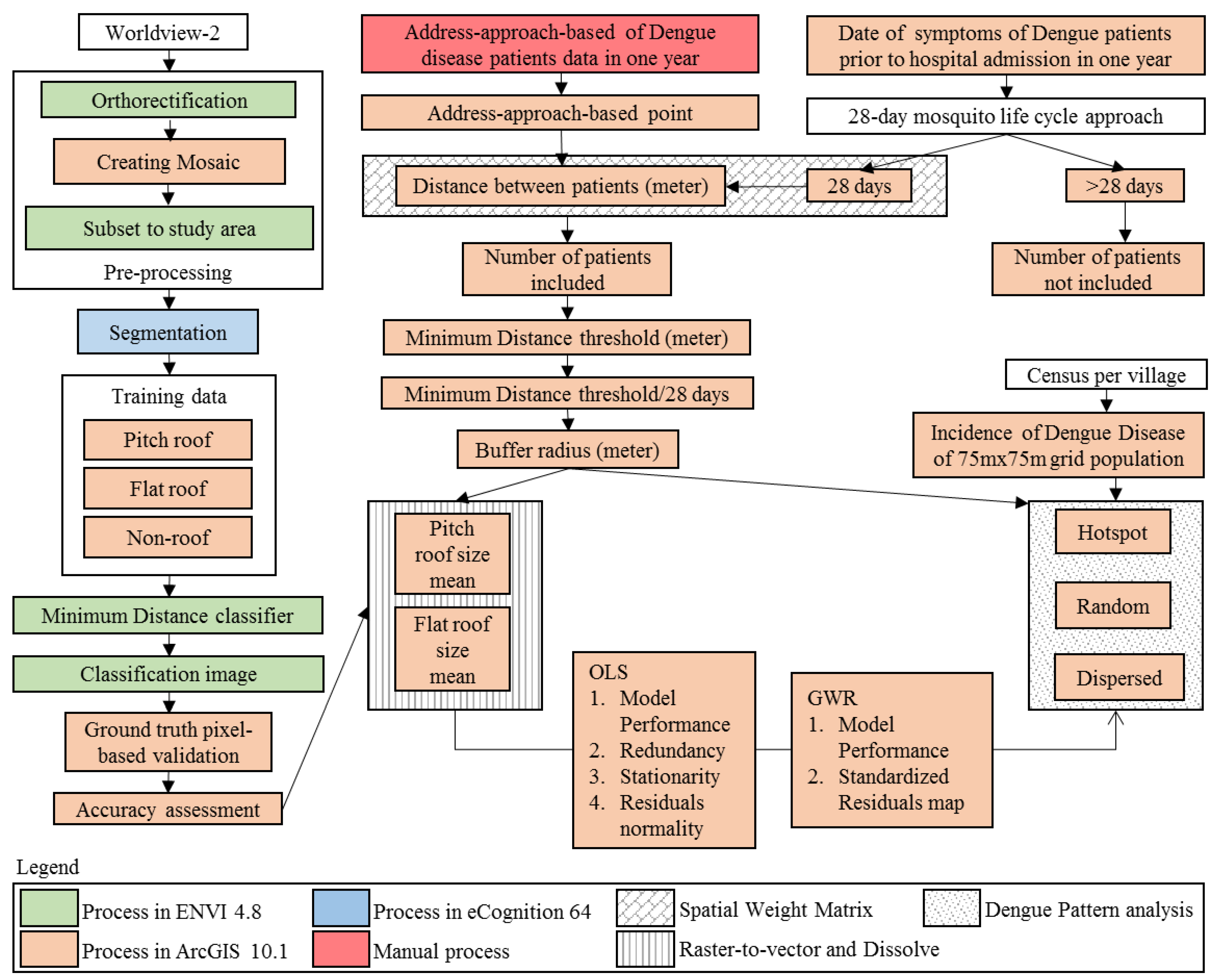

2.2. Analysis
| Roof | Pitched Roof | Flat Roof | ||||
|---|---|---|---|---|---|---|
| Color composite (DN) | R | G | B | R | G | B |
| Minimum | 140 | 261 | 233 | 163 | 319 | 271 |
| Maximum | 576 | 619 | 459 | 830 | 1079 | 716 |
| Mean | 282.18 | 403.21 | 321.18 | 415.79 | 598.08 | 438.38 |
| Standard deviation | 71.56 | 47.60 | 27.03 | 105.02 | 128.65 | 77.14 |
3. Results and Discussion
3.1. Accuracy Assessment of Roof Classification
| Classified Data | Reference Data | User Accuracy (%) | |||
|---|---|---|---|---|---|
| Pitched Roof | Flat Roof | Non-Roof | Total | ||
| Pitched Roof | 34 | 7 | 47 | 88 | 38.64 |
| Flat Roof | 3 | 41 | 5 | 49 | 83.67 |
| Non-Roof | 15 | 3 | 117 | 135 | 86.67 |
| Total | 52 | 51 | 169 | 272 | |
| Producer accuracy (%) | 65.38 | 80.39 | 69.23 | ||
| Overall accuracy % | 70.59 | ||||
| Kappa coefficient | 0.51 | ||||

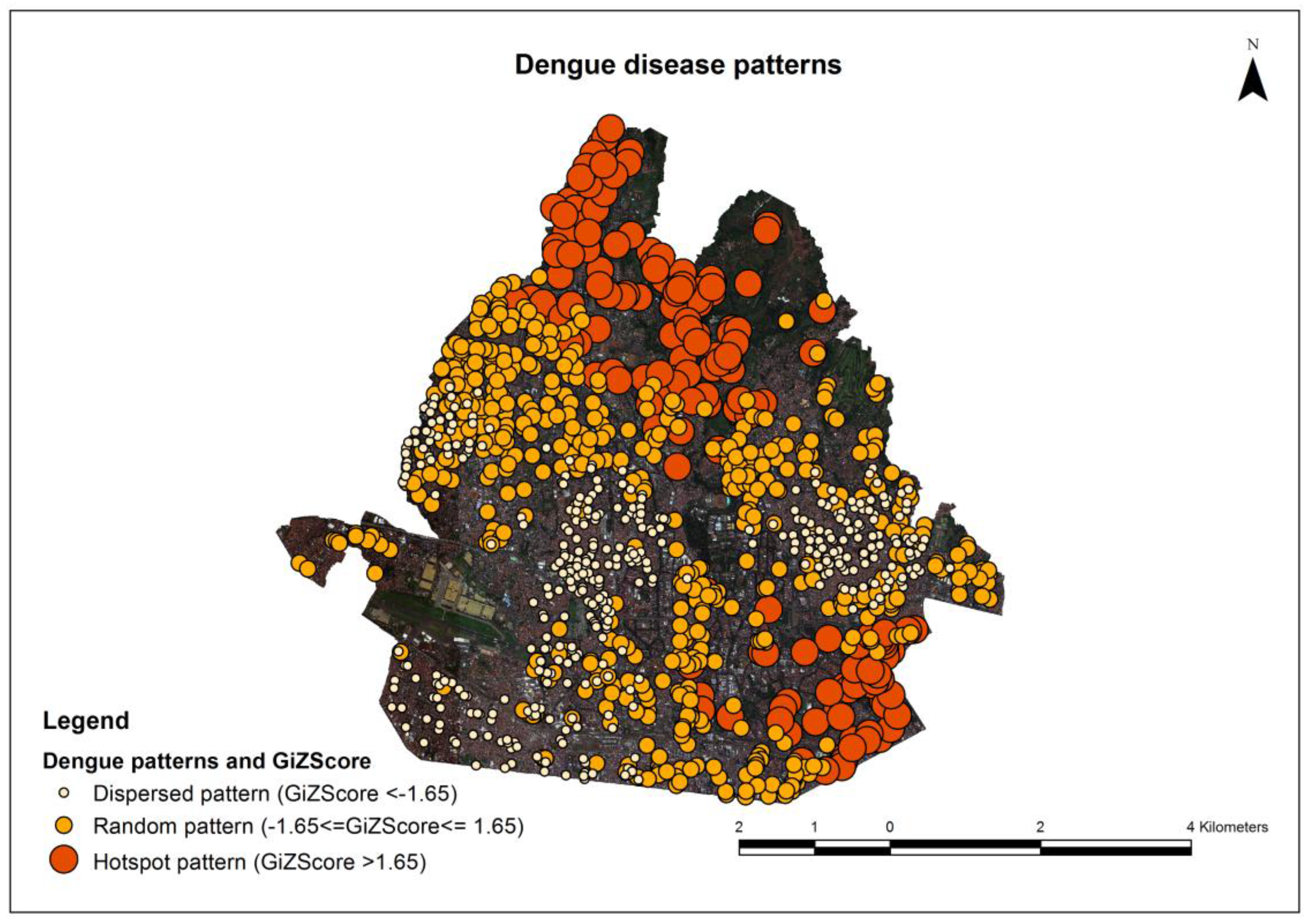
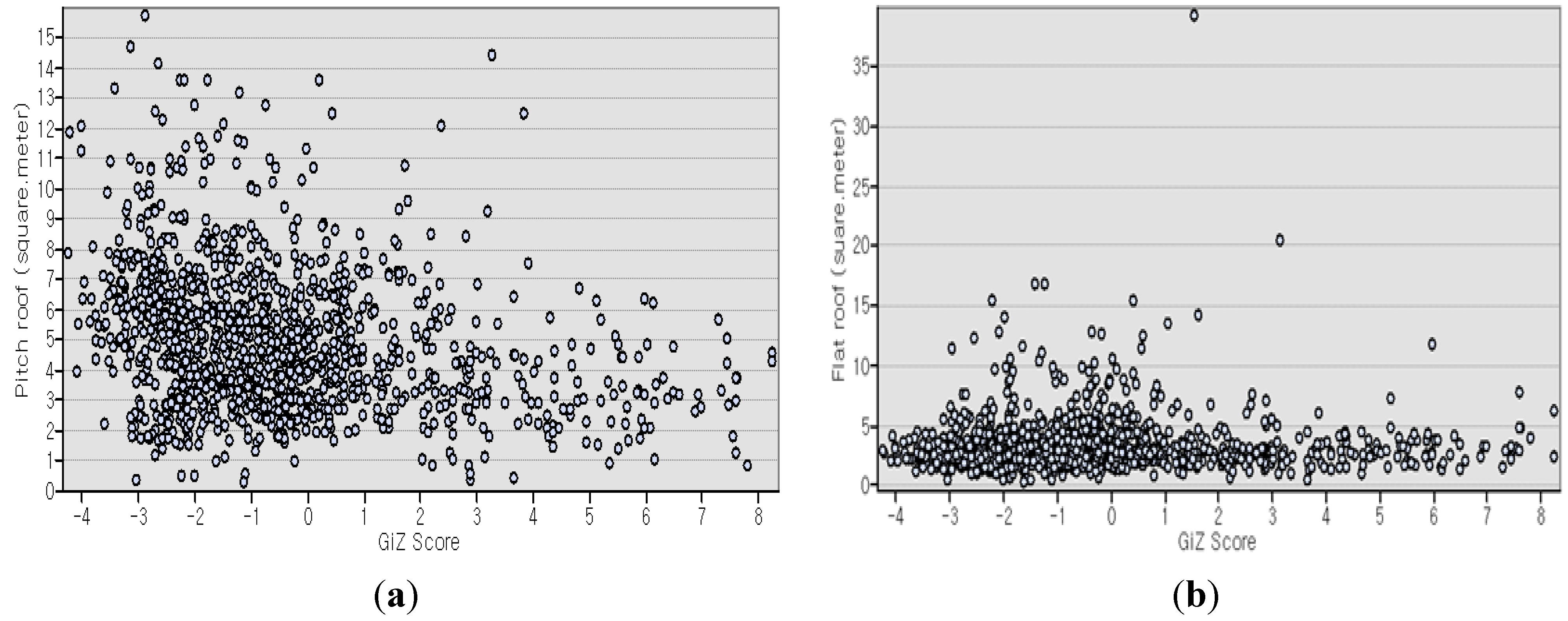
3.2. Dengue Disease Patterns
| Variables | Dengue Disease Patterns | ||
|---|---|---|---|
| Hotspot | Random | Dispersed | |
| Count (address-point) | 184 | 555 | 415 |
| Pitched roof (m2) | |||
| Minimum | 0.33 | 0.25 | 0.32 |
| Maximum | 14.41 | 13.59 | 15.72 |
| Mean | 3.83 | 4.85 | 5.65 |
| Standard deviation | 2.15 | 2.15 | 2.67 |
| Flat roof (m2) | |||
| Minimum | 0.38 | 0.23 | 0.34 |
| Maximum | 20.45 | 39.2 | 15.38 |
| Mean | 2.99 | 3.45 | 2.97 |
| Standard deviation | 1.97 | 2.76 | 1.86 |
| GiZ Score | |||
| Minimum | 1.68 | −1.64 | −4.24 |
| Maximum | 8.25 | 1.64 | −1.65 |
| Mean | 3.99 | −0.28 | −2.53 |
| Standard deviation | 1.73 | 0.83 | 0.57 |
3.3. OLS Regression and GWR Model
| Parameter | All | Hotspot | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimated Value | Std. Error | p Value | VIF | Estimated Value | Std. Error | p Value | VIF | |||||||
| OLS | GWR | OLS | GWR | OLS | OLS | OLS | ||||||||
| Outlier | Outlier | Outlier | Outlier | Outlier | ||||||||||
| with | without | without | with | without | with | without | with | without | ||||||
| Number of observations | 1154 | 1154 | 1154 | 1154 | 1154 | 184 | 183 | 183 | 184 | 183 | 184 | 183 | 184 | 183 |
| Intercept | 0.81 | 0.18 | 0.00 | 4.46 | 4.23 | 0.33 | 0.36 | 0.00 | 0.00 | |||||
| Pitched roof | −0.27 | 0.03 | 0.00 | 1.00 | −0.16 | −0.17 | 0.06 | 0.06 | 0.00 | 0.00 | 1.00 | 1.00 | ||
| Flat roof | 0.04 | 0.03 | 0.00 | 1.00 | 0.05 | 0.14 | 0.06 | 0.08 | 0.52 | 0.12 | 1.00 | 1.00 | ||
| R2 | 0.076 | 0.76 | 0.04 | 0.06 | 0.39 | |||||||||
| Adjusted R2 | 0.075 | 0.75 | 0.03 | 0.05 | 0.30 | |||||||||
| AICc | 5184.97 | 3709.59 | 723 | 717.7 | 670.30 | |||||||||
| Koenker test | 29.99 | 0.00 | 3.68 | 3.58 | 0.16 | 0.17 | ||||||||
| Jarque-Bera | 320.22 | 0.00 | 15.1 | 14.02 | 0.00 | 0.00 | ||||||||
| Parameter | Random | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimated Value | Std. Error | p Value | VIF | ||||||
| OLS | GWR | OLS | OLS | OLS | |||||
| Outlier | Outlier | Outlier | Outlier | Outlier | |||||
| with | without | with | with | without | with | without | with | without | |
| Number of observations | 555 | 554 | 555 | 555 | 554 | 555 | 554 | 555 | 554 |
| Intercept | −0.30 | −0.27 | 0.10 | 0.10 | 0.00 | 0.00 | |||
| Pitched roof | −0.01 | −0.01 | 0.02 | 0.02 | 0.36 | 0.36 | 1.00 | 1.00 | |
| Flat roof | 0.03 | 0.02 | 0.01 | 0.02 | 0.05 | 0.30 | 1.00 | 1.00 | |
| R2 | 0.01 | 0.004 | 0.37 | ||||||
| Adjusted R2 | 0.01 | 0.000 | 0.32 | ||||||
| AICc | 1376.14 | 1373.15 | 1179.64 | ||||||
| Koenker test | 0.53 | 0.90 | 0.77 | 0.64 | |||||
| Jarque-Bera | 23.04 | 23.52 | 0.00 | 0.00 | |||||
| Parameter | Dispersed | ||||
|---|---|---|---|---|---|
| Estimated Value | Std. Error | p Value | VIF | ||
| OLS | GWR | OLS | OLS | OLS | |
| Outlier | Outlier | Outlier | Outlier | Outlier | |
| with | with | with | with | with | |
| Number of observations | 415 | 415 | 415 | 415 | 415 |
| Intercept | −2.36 | 0.08 | 0.00 | ||
| Pitched roof | −0.04 | 0.01 | 0.00 | 1.00 | |
| Flat roof | 0.02 | 0.01 | 0.04 | 1.00 | |
| R2 | 0.04 | 0.23 | |||
| Adjusted R2 | 0.04 | 0.18 | |||
| AICc | 701.82 | 644.74 | |||
| Koenker test | 10.40 | 0.006 | |||
| Jarque-Bera | 18.22 | 0.00 | |||

4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Getis, A.; Morrison, A.C.; Gray, K.; Scott, T.W. Characteristics of the spatial pattern of the dengue vector, Aedes aegypti, in Iquitos, Peru. Am. J. Trop. Med. Hyg. 2003, 69, 494–505. [Google Scholar] [PubMed]
- Pal, T.; Dutta, S.K.; Mandal, S.; Saha, B.; Tripathi, A. Differential clinical symptoms among acute phase Indian patients revealed significant association with dengue viral load and serum IFN-gamma level. J. Clin. Virol. 2014, 61, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Zakaria, Z.; Zainordin, N.A.; Sim, B.L.H.; Zaid, M.; Haridan, U.S.; Aziz, A.T.A.; Shueb, R.H.; Mustafa, M.; Yusoff, N.K.N.; Malik, A.S.; et al. An evaluation of the World Health Organization’s 1997 and 2009 dengue classifications in 3 hospitalized dengue patients in Malaysia. J. Infect. Dev. Ctries. 2014, 8, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Sahana, K.S.; Sujatha, R. Clinical profile of dengue among children according to revised who classification: Analysis of a 2012 outbreak from southern India. Indian J. Pediatr. 2015, 82, 109–113. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Dengue: Guideline for Diagnosis, Treatment, Prevention, and Control, 2009. Available online: http://whqlibdoc.who.int/publications/2009/9789241547871_eng.pdf (accessed on 21 February 2014).
- Chadee, D.D.; Martinez, R. Landing periodicity of Aedes aegypti with implications for dengue transmission in Trinidad, West Indies. J. Vector Ecol. 2000, 25, 158–163. [Google Scholar] [PubMed]
- Hugo, L.E.; Jeffery, J.A.L.; Trewin, B.J.; Wockner, L.F.; Nguyen Thi, Y.; Nguyen Hoang, L.; le Trung, N.; Hine, E.; Ryan, P.A.; Kay, B.H. Adult survivorship of the dengue mosquito Aedes aegypti varies seasonally in central Vietnam. PLoS Negl. Trop. Dis. 2014, 8. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, B.L.; Ritchie, S.A. Roof gutters: A key container for Aedes aegypti and Ochlerotatus notoscriptus (diptera: Culicidae) in Australia. Am. J. Trop. Med. Hyg. 2002, 67, 244–246. [Google Scholar] [PubMed]
- Center for Disease Control. Dengue Fever. Center for Disease Control, 2013. Available online: http://www.health.nt.gov.au/library/scripts/objectifyMedia.aspx?file=pdf/45/15.pdf (accessed on 14 November 2013).
- Khormi, H.M.; Kumar, L. Examples of using spatial information technologies for mapping and modelling mosquito-borne diseases based on environmental, climatic and socioeconomic factors and different spatial statistics, temporal risk indices and spatial analysis: A review. J. Food Agric. Environ. 2011, 9, 41–49. [Google Scholar]
- Louis, V.R.; Phalkey, R.; Horstick, O.; Ratanawong, P.; Wilder-Smith, A.; Tozan, Y.; Dambach, P. Modeling tools for dengue risk mapping—A systematic review. Int. J. Health Geogr. 2014, 13. [Google Scholar] [CrossRef] [PubMed]
- Fuller, D.O.; Troyo, A.; Calderon-Arguedas, O.; Beier, J.C. Dengue vector (Aedes aegypti) larval habitats in an urban environment of Costa Rica analysed with ASTER and QuickBird imagery. Int. J. Remote Sens. 2010, 31, 3–11. [Google Scholar] [CrossRef]
- Dom, N.C.; Ahmad, A.H.; Abd-Latif, Z.; Ismail, R.; Pradhan, B. Coupling of remote sensing data and environmental-related parameters for dengue transmission risk assessment in Subang Jaya, Malaysia. Geocarto Int. 2013, 28, 258–272. [Google Scholar] [CrossRef] [Green Version]
- Carbajo, A.E.; Curto, S.I.; Schweigmann, N.J. Spatial distribution pattern of oviposition in the mosquito Aedes aegypti in relation to urbanization in Buenos Aires: Southern fringe bionomics of an introduced vector. Med. Vet. Entomol. 2006, 20, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Savage, H.M.; Fritz, C.L.; Rutstein, D.; Yolwa, A.; Vorndam, V.; Gubler, D.J. Epidemic of dengue-4 virus in Yap state, Federated States of Micronesia, and implication of Aedes hensilli as an epidemic vector. Am. J. Trop. Med. Hyg. 1998, 58, 519–524. [Google Scholar] [PubMed]
- Napolano, L.; Menna, C.; Asprone, D.; Prota, A.; Manfredi, G. Life cycle environmental impact of different replacement options for a typical old flat roof. Int. J. Life Cycle Assess. 2015, 20, 694–708. [Google Scholar] [CrossRef]
- Farreny, R.; Morales-Pinzon, T.; Guisasola, A.; Taya, C.; Rieradevall, J.; Gabarrell, X. Roof selection for rainwater harvesting: Quantity and quality assessments in Spain. Water Res. 2011, 45, 3245–3254. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Kamara, F.; Zhou, G.; Puthiyakunnon, S.; Li, C.; Liu, Y.; Zhou, Y.; Yao, L.; Yan, G.; Chen, X.-G. Urbanization increases Aedes albopictus larval habitats and accelerates mosquito development and survivorship. PLoS Negl. Trop. Dis. 2014, 8. [Google Scholar] [CrossRef] [PubMed]
- Manrique-Saide, P.; Coleman, P.; McCall, P.J.; Lenhart, A.; Vazquez-Prokopec, G.; Davies, C.R. Multi-scale analysis of the associations among egg, larval and pupal surveys and the presence and abundance of adult female Aedes aegypti (Stegomyia aegypti) in the city of Merida, Mexico. Med. Vet. Entomol. 2014, 28, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, M.A.; Saldaña, M.M.; Aguilar, F.J. Geoeye-1 and worldview-2 pan-sharpened imagery for object-based classification in urban environments. Int. J. Remote Sens. 2013, 34, 2583–2606. [Google Scholar] [CrossRef]
- Zhou, Y.; Qiu, F. Fusion of high spatial resolution Worldview-2 imagery and lidar pseudo-waveform for object-based image analysis. ISPRS J. Photogramm. Remote Sens. 2015, 101, 221–232. [Google Scholar] [CrossRef]
- Longbotham, N.; Chaapel, C.; Bleiler, L.; Padwick, C.; Emery, W.J.; Pacifici, F. Very high resolution multiangle urban classification analysis. IEEE Trans. Geosci. Remote Sens. 2012, 50, 1155–1170. [Google Scholar] [CrossRef]
- Machault, V.; Vignolles, C.; Pages, F.; Gadiaga, L.; Tourre, Y.M.; Gaye, A.; Sokhna, C.; Trape, J.-F.; Lacaux, J.-P.; Rogier, C. Risk mapping of Anopheles gambiae s.l. densities using remotely sensed environmental and meteorological data in an urban area: Dakar, Senegal. PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masuoka, P.M.; Claborn, D.M.; Andre, R.G.; Nigro, J.; Gordon, S.W.; Klein, T.A.; Kim, H.C. Use of Ikonos and Landsat for malaria control in the Republic of Korea. Remote Sens. Environ. 2003, 88, 187–194. [Google Scholar] [CrossRef]
- McFeeters, S.K. Using the normalized difference water index (NDWI) within a geographic information system to detect swimming pools for mosquito abatement: A practical approach. Remote Sens. 2013, 5, 3544–3561. [Google Scholar] [CrossRef]
- Troyo, A.; Fuller, D.O.; Calderon-Arguedas, O.; Solano, M.E.; Beier, J.C. Urban structure and dengue incidence in Puntarenas, Costa Rica. Singap. J. Trop. Geogr. 2009, 30, 265–282. [Google Scholar] [CrossRef] [PubMed]
- Machault, V.; Yebakima, A.; Etienne, M.; Vignolles, C.; Palany, P.; Tourre, Y.M.; Guerecheau, M.; Lacaux, J.-P. Mapping entomological dengue risk levels in Martinique using high-resolution remote-sensing environmental data. ISPRS Int. J. Geo-Inf. 2014, 3, 1352–1371. [Google Scholar] [CrossRef]
- Cianci, D.; Hartemink, N.; Zeimes, C.B.; Vanwambeke, S.O.; Ienco, A.; Caputo, B. High resolution spatial analysis of habitat preference of Aedes albopictus (diptera: Culicidae) in an urban environment. J. Med. Entomol. 2015, 52, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Vanwambeke, S.O.; Somboon, P.; Harbach, R.E.; Isenstadt, M.; Lambin, E.F.; Walton, C.; Butlin, R.K. Landscape and land cover factors influence the presence of Aedes and Anopheles larvae. J. Med. Entomol. 2007, 44, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Anders, K.L.; le Nga, H.; Thuy, N.T.; Ngoc, T.V.; Tam, C.T.; Tai, L.T.; Truong, N.T.; Duyen, H.T.; Trung, V.T.; Kien, D.T.; et al. Households as foci for dengue transmission in highly urban Vietnam. PLoS Negl. Trop. Dis. 2015, 9. [Google Scholar] [CrossRef] [PubMed]
- Myint, S.W.; Galletti, C.S.; Kaplan, S.; Kim, W.K. Object vs. Pixel: A systematic evaluation in urban environments. Geocarto Int. 2013, 28, 657–678. [Google Scholar] [CrossRef]
- Witharana, C.; Civco, D.L.; Meyer, T.H. Evaluation of data fusion and image segmentation in earth observation based rapid mapping workflows. ISPRS J. Photogramm. Remote Sens. 2014, 87, 1–18. [Google Scholar] [CrossRef]
- Kressler, F.P.; Steinnocher, K.; Franzen, M. Object-oriented classification of orthophotos to support update of spatial databases. In Proceedings of the 2005 IEEE International Geoscience and Remote Sensing Symposium, Seoul, Korea, 25–29 July 2005; pp. 253–256.
- Khormi, H.M.; Kumar, L. Modeling dengue fever risk based on socioeconomic parameters, nationality and age groups: GIS and remote sensing based case study. Sci. Total Environ. 2011, 409, 4713–4719. [Google Scholar] [CrossRef] [PubMed]
- Lillesand, T.M.; Kiefer, R.W. Remote Sensing and Image Interpretation, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 1987. [Google Scholar]
- Lin, C.-H.; Wen, T.-H. Using geographically weighted regression (GWR) to explore spatial varying relationships of immature mosquitoes and human densities with the incidence of dengue. Int. J. Environ. Res. Public Health 2011, 8, 2798–2815. [Google Scholar] [CrossRef] [PubMed]
- Elliott, P.; Cuzick, J.; English, D.; Stern, R. Geographical and Environmental Epidemiology. Methods for Small-Area Studies, 1st ed.; Oxford University Press: New York, NY, USA, 2000. [Google Scholar]
- Yassi, A.; Kjellstrom, T.; de Kock, T.; Guidotti, T.L. Basic Environmental Health, 1st ed.; Oxford University Press: New York, NY, USA, 2001. [Google Scholar]
- Muir, L.E.; Kay, B.H. Aedes aegypti survival and dispersal estimated by mark-release-recapture in northern Australia. Am. J. Trop. Med. Hyg. 1998, 58, 277–282. [Google Scholar] [PubMed]
- Kumar, A.; Pandey, A.C.; Jeyaseelan, A.T. Built-up and vegetation extraction and density mapping using Worldview-ii. Geocarto Int. 2012, 27, 557–568. [Google Scholar] [CrossRef]
- Ord, J.K.; Getis, A. Local spatial autocorrelation statistics—Distributional issues and an application. Geogr. Anal. 1995, 27, 286–306. [Google Scholar] [CrossRef]
- Harrington, L.C.; Scott, T.W.; Lerdthusnee, K.; Coleman, R.C.; Costero, A.; Clark, G.G.; Jones, J.J.; Kitthawee, S.; Kittayapong, P.; Sithiprasasna, R.; et al. Dispersal of the dengue vector Aedes aegypti within and between rural communities. Am. J. Trop. Med. Hyg. 2005, 72, 209–220. [Google Scholar] [PubMed]
- Sarfraz, M.S.; Tripathi, N.K.; Kitamoto, A. Near real-time characterisation of urban environments: A holistic approach for monitoring dengue fever risk areas. Int. J. Digit. Earth 2014, 7, 916–934. [Google Scholar] [CrossRef]
- Brunsdon, C.; Fotheringham, A.S.; Charlton, M.E. Geographically weighted regression: A method for exploring spatial nonstationarity. Geogr. Anal. 1996, 28, 281–298. [Google Scholar] [CrossRef]
- Congalton, R.G.; Green, K. Assessing the Accuracy of Remotely Sensed Data, 2nd ed.; CRC Press Taylor & Francis Group: Boca Raton, FL, USA, 2009. [Google Scholar]
- Yuhendra, Y.; Alimuddin, I.; Sumantyo, J.T.S.; Kuze, H. Assessment of pan-sharpening methods applied to image fusion of remotely sensed multi-band data. Int. J. Appl. Earth Obs. Geoinf. 2012, 18, 165–175. [Google Scholar] [CrossRef]
- Peres, R.C.; Rego, R.; Maciel-de-Freitas, R. The use of the premise condition index (PCI) to provide guidelines for Aedes aegypti surveys. J. Vector Ecol. 2013, 38, 190–192. [Google Scholar] [CrossRef] [PubMed]
- Basker, P.; Ezhil, R. Study on the correlation of the premises condition index and the presence of larva of Aedes species mosquitoes in human dwellings of the Cudallore district of Tamil Nadu, India. Osong Public Health Res. Perspect. 2012, 3, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Kinear, P.R.; Gray, C.D. SPSS 12 Made Simple, 1st ed.; Psychology Press: New York, NY, USA, 2004. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rinawan, F.R.; Tateishi, R.; Raksanagara, A.S.; Agustian, D.; Alsaaideh, B.; Natalia, Y.A.; Raksanagara, A. Pitch and Flat Roof Factors’ Association with Spatiotemporal Patterns of Dengue Disease Analysed Using Pan-Sharpened Worldview 2 Imagery. ISPRS Int. J. Geo-Inf. 2015, 4, 2586-2603. https://doi.org/10.3390/ijgi4042586
Rinawan FR, Tateishi R, Raksanagara AS, Agustian D, Alsaaideh B, Natalia YA, Raksanagara A. Pitch and Flat Roof Factors’ Association with Spatiotemporal Patterns of Dengue Disease Analysed Using Pan-Sharpened Worldview 2 Imagery. ISPRS International Journal of Geo-Information. 2015; 4(4):2586-2603. https://doi.org/10.3390/ijgi4042586
Chicago/Turabian StyleRinawan, Fedri Ruluwedrata, Ryutaro Tateishi, Ardini Saptaningsih Raksanagara, Dwi Agustian, Bayan Alsaaideh, Yessika Adelwin Natalia, and Ahyani Raksanagara. 2015. "Pitch and Flat Roof Factors’ Association with Spatiotemporal Patterns of Dengue Disease Analysed Using Pan-Sharpened Worldview 2 Imagery" ISPRS International Journal of Geo-Information 4, no. 4: 2586-2603. https://doi.org/10.3390/ijgi4042586
APA StyleRinawan, F. R., Tateishi, R., Raksanagara, A. S., Agustian, D., Alsaaideh, B., Natalia, Y. A., & Raksanagara, A. (2015). Pitch and Flat Roof Factors’ Association with Spatiotemporal Patterns of Dengue Disease Analysed Using Pan-Sharpened Worldview 2 Imagery. ISPRS International Journal of Geo-Information, 4(4), 2586-2603. https://doi.org/10.3390/ijgi4042586