Translating Developmental Origins: Improving the Health of Women and Their Children Using a Sustainable Approach to Behaviour Change
Abstract
:1. Introduction
2. Changing Health Behaviour
3. Healthy Conversation Skills
| Healthy Conversations: Five Key Skills |
| Identifying/Creating opportunities—for having a healthy conversation. |
| Asking open discovery questions—‘how’ and ‘what’ questions that lead people to explore their own world and find their own solutions. |
| Listening more than talking—empowering people to identify and take control of their own behaviour change. |
| Reflecting—on practice in order to be more effective. |
| Supporting goal-setting—using SMARTER action planning, staff and women have a sense of change and progress. |
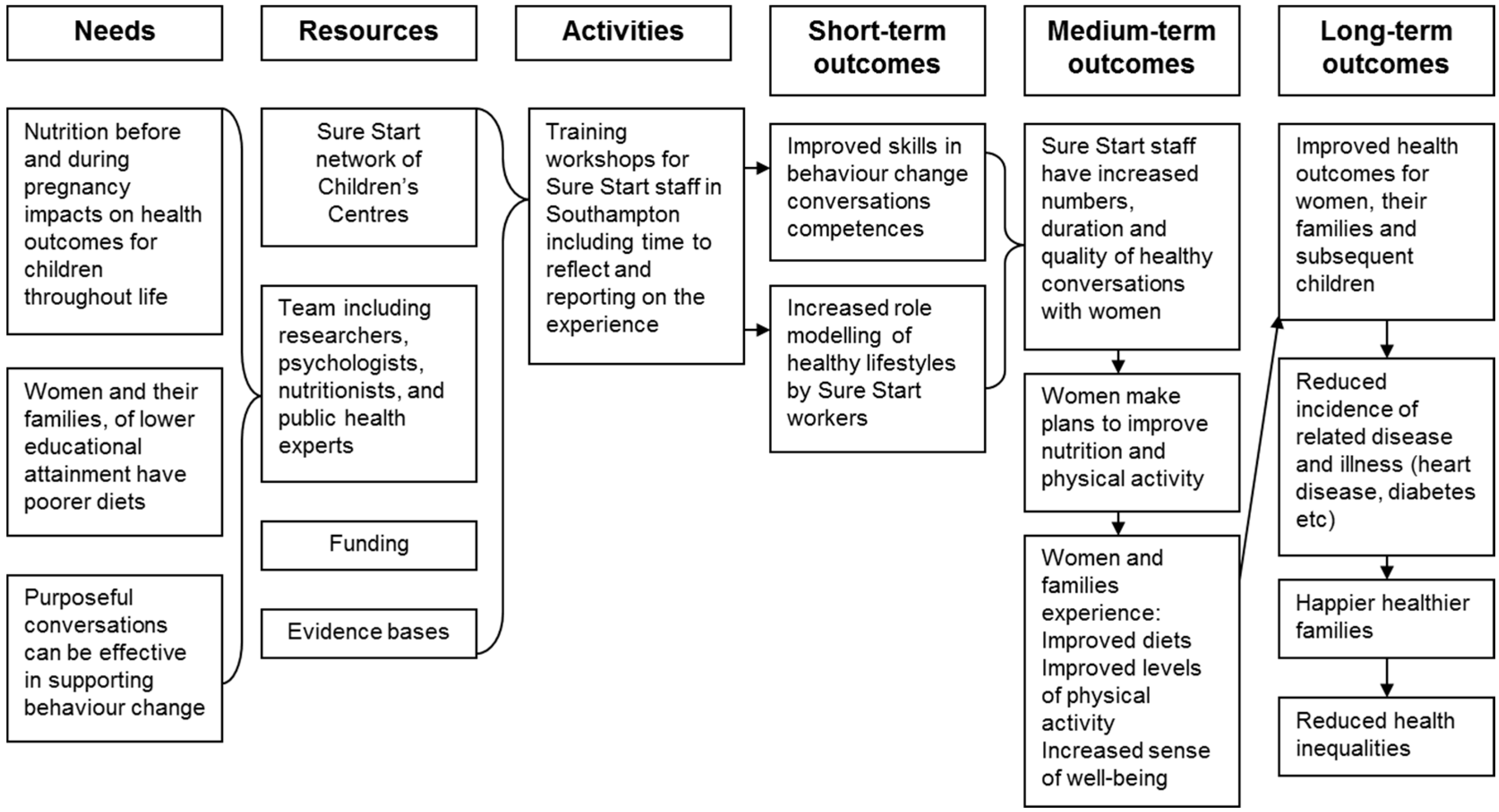
4. The Southampton Initiative for Health
4.1. Building Trust
| Timeline of Events in Progress of the Partnership That Supported the Development, Testing and Implementation of Healthy Conversation Skills Training. | |
| 2004 | Research team made contact with SureStart Children’s Centres and began a series of focus group discussions with Centre users to explore food choices and barriers to healthy eating. |
| 2005 | Research team set up Food Choice Action Group including research team of psychologists, nutritionists, public health experts, statisticians, external academic advisors, members of local health authority and SureStart Children’s Centre managers. |
| 2007 | The research arm of the Southampton Initiative for Health formally established. |
| Research team conducted a Nutrition and Well-being Survey in SureStart Children’s Centres with mothers. Local authority and Primary Care Trust carried out a training needs assessment of SureStart staff. | |
| 2008 | Research team met SureStart Children’s Centre managers, health visitors and health trainers to discuss results of the Nutrition and Well-being Survey. |
| Researchers from the University’s Medical Research Council Lifecourse Epidemiology Unit invited Southampton Primary Care Trust to discuss needs of the local area. | |
| Formal meeting was held of all local agencies from across the Primary Care Trust and City Council to discuss the research findings and how they might be used as the basis for an intervention to improve the nutritional status of local young women and their children. | |
| Southampton Initiative for Health as a formal partnership between research, policy and practice organisations was born. A programme of monthly meetings involving participating organisations was established. | |
| A focus group discussion was held with key SureStart Children’s Centres practitioners to discuss findings from discussions and survey work with women attending SureStart Children’s Centres, and to gather ideas for potential intervention points. | |
| 2009 | Research team observed a range of SureStart Children’s Centres sessions across Southampton. |
| Healthy Conversations Skills training was developed by the whole Southampton Initiative For Health team. Training manual was written. | |
| Research team held a pilot session of the training with SureStart Children’s Centre managers. Training manual was modified. | |
| SureStart Children’s Centres managers encouraged their staff to attend Healthy Conversation Skills training, to be delivered at the Centres. Southampton Initiative For Health and SureStart Children’s Centres worked together to recruit staff. | |
| Training began across the city. | |
| 2010–2011 | All Healthy Conversation Skills training sessions and follow-up completed early 2011. Research team monitored fidelity of their training delivery. |
| Research team attended a wide range of SureStart Children’s Centres sessions to observe trainees in action, evaluate competence in Healthy Conversation Skills and provide feedback. | |
| Evaluation data collected as part of trial analysed by research team. | |
| Local commissioners formally issued a contract to the regional health promotion team to deliver Healthy Conversation Skills training. | |
| Research team ‘handed over’ the intervention to be run by local services. Research team trained health promotion team in Healthy Conversation Skills. | |
| Health promotion team begins delivery of training to Primary Care Trust and city council staff in Southampton late 2010. | |
| Training sessions delivered by health promotion team observed by Southampton Initiative for Health research team to assess fidelity of intervention delivery. | |
| Evaluation data collected from health promotion team training analysed by research team. | |
| 2011 | Southampton Initiative for Health provided all trainees with an interactive Healthy Conversation Skills newsletter. |
| Research team conducted another round of observations of trainees in practice at SureStart Children’s Centres. | |
| 2012 | Research team conducted focus groups with trainees to gauge feasibility and acceptability of training programme. |
| Reports and papers produced by joint authorship representing all organisations participating in the Southampton Initiative for Health. | |
4.2. Agenda Matching
4.3. Changing Cultures
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Ethics
References
- Barker, D.; Barker, M.; Fleming, T.; Lampl, M. Developmental biology: Support mothers to secure future public health. Nature 2013, 504, 209–211. [Google Scholar] [CrossRef] [PubMed]
- Hanson, M.; Gluckman, P. Developmental origins of noncommunicable disease: Population and public health implications. Am. J. Clin. Nutr. 2011, 94, 1754S–1758S. [Google Scholar] [CrossRef] [PubMed]
- Backholer, K.; Spencer, E.; Gearon, E.; Magliano, D.J.; McNaughton, S.A.; Shaw, J.E.; Peeters, A. The association between socio-economic position and diet quality in Australian adults. Public Health Nutr. 2016, 19, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.M.; Crozier, S.R.; Borland, S.E.; Hammond, J.; Barker, D.J.P.; Inskip, H.M. Impact of educational attainment on the quality of young women’s diets. Eur. J. Clin. Nutr. 2004, 58, 1174–1180. [Google Scholar] [CrossRef] [PubMed]
- Snelgrove, J.W.; Murphy, K.E. Preterm birth and social inequality: Assessing the effects of material and psychosocial disadvantage in a UK birth cohort. Acta Obstet. Gynecol. Scandi. 2015, 94, 766–775. [Google Scholar] [CrossRef] [PubMed]
- Sebayang, S.K.; Dibley, M.J.; Kelly, P.J.; Shankar, A.V.; Shankar, A.H. Determinants of low birthweight, small-for-gestational-age and preterm birth in Lombok, Indonesia: Analyses of the birthweight cohort of the SUMMIT trial. Trop. Medi. Int. Health 2012, 17, 938–950. [Google Scholar] [CrossRef] [PubMed]
- Kraak, V.A.; Liverman, C.T.; Koplan, J.P. Preventing Childhood Obesity: Health in the Balance; National Academies Press: Washington, DC, USA, 2005. [Google Scholar]
- Booth, S.L.; Sallis, J.F.; Ritenbaugh, C.; Hill, J.O.; Birch, L.L.; Frank, L.D.; Glanz, K.; Himmelgreen, D.A.; Mudd, M.; Popkin, B.M.; et al. Environmental and societal factors affect food choice and physical activity: Rationale, influences, and leverage points. Nutr. Rev. 2001, 59. [Google Scholar] [CrossRef]
- Poulton, R.; Caspi, A.; Milne, B.J.; Thomson, W.M.; Taylor, A.; Sears, M.R.; Moffitt, T.E. Association between children’s experience of socioeconomic disadvantage and adult health: A life-course study. Lancet 2002, 360, 1640–1645. [Google Scholar] [CrossRef]
- Haider, B.A.; Bhutta, Z.A. Multiple-micronutrient Supplementation for Women during Pregnancy. Available online: http://www.cochrane.org/CD004905/PREG_multiple-micronutrient-supplementation-women-during-pregnancy (accessed on 1 November 2015).
- Pena-Rosas, J.P.; De-Regil, L.M.; Dowswell, T.; Viteri, F.E. Daily oral iron supplementation during pregnancy. Cochrane Database Syst. Rev. 2012, 12. [Google Scholar] [CrossRef]
- Michie, S.; West, R. Behaviour change theory and evidence: A presentation to Government. Health Psychol. Rev. 2013, 7, 1–22. [Google Scholar] [CrossRef]
- Strack, F.; Deutsch, R. Reflective and impulsive determinants of social behavior. Pers. Soc. Psychol. Rev. 2004, 8, 220–247. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Ashford, S.; Sniehotta, F.; Dombrowski, S.U.; Bishop, A.; French, D.P. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy. Psychol. Health 2011, 26, 1479–1498. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Abraham, C.; Whittington, C.; McAteer, J.; Gupta, S. Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychol. 2009, 28, 690–701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6. [Google Scholar] [CrossRef] [PubMed]
- Wight, D.; Wimbush, E.; Jepson, R.; Doi, L. Six steps in quality intervention development (6SQuID). J. Epidemiol. Community Health 2015. [Google Scholar] [CrossRef]
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The person-based approach to intervention development: Application to digital health-related behavior change interventions. J. Med. Internet Res. 2015, 17, e30. [Google Scholar] [CrossRef] [PubMed]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, J.; Johnson, M. Southampton Sure Start Children’s Centres Training Needs Assessment: Final Report; Southampton city PCT: Southampton, UK, 2008. [Google Scholar]
- Lawrence, W.; Keyte, J.; Tinati, T.; Haslam, C.; Baird, J.; Margetts, B.; Swift, J.; Cooper, C.; Barker, M. A mixed-methods investigation to explore how women living in disadvantaged areas might be supported to improve their diets. J. Health Psychol. 2012, 17, 785–798. [Google Scholar] [CrossRef] [PubMed]
- Butler, C.C.; Simpson, S.A.; Hood, K.; Cohen, D.; Pickles, T.; Spanou, C.; McCambridge, J.; Moore, L.; Randell, E.; Alam, M.F.; et al. Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: A cluster randomised trial. BMJ 2013, 346, f1191. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations Of Thought And Action: A Social Cognitive Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Bandura, A. Self-Efficacy: The Exercise of Control; Macmillan: London, UK, 1997. [Google Scholar]
- Steptoe, A.; Perkins-Porras, L.; Rink, E.; Hilton, S.; Cappucio, F.P. Psychological and social predictors of changes in fruit and vegetable consumption over 12 months following behavioural and nutrition education counseling. Health Psychol. 2004, 23, 574–581. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Barker, M.; Baird, J.; Lawrence, W.; Jarman, M.; Black, C.; Barnard, K.; Eccles, M.P.; Cane, J.; Wood, C.E. The Southampton Initiative for Health:a complex intervention to improve the diets and increase the physical activity levels of women from disadvantaged communities. J. Health Psychol. 2011, 16, 178–191. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, R.; Inskip, H. The Health and Wellbeing of Women in Southampton’s Communities: An Analysis of the Southampton Women’s Survey; Southampton City NHS Primary Care Trust: Southampton, UK, 2006. [Google Scholar]
- Black, C.; Lawrence, W.; Cradock, S.; Ntani, G.; Tinati, T.; Jarman, M.; Begum, R.; Inskip, H.; Cooper, C.; Barker, M.; et al. Healthy conversation skills: Increasing competence and confidence in front-line staff. Public Health Nutr. 2014, 17, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, W.; Black, C.; Tinati, T.; Cradock, S.; Begum, R.; Jarman, M.; Pease, A.; Margetts, B.; Davies, J.; Inskip, H.; et al. ‘Making every contact count’: Longitudinal evaluation of the impact of training in behaviour change on the work of health and social care practitioners. J. Health Psychol. 2016, 21, 138–151. [Google Scholar] [CrossRef] [PubMed]
- Baird, J.; Jarman, M.; Lawrence, W.; Black, C.; Davies, J.; Tinati, T.; Begum, R.; Mortimore, A.; Robinson, S.; Margetts, B.; et al. The effect of a behaviour change intervention on the diets and physical activity levels of women attending Sure Start Children’s Centres: Results from a complex public health intervention. BMJ Open 2014, 4, e005290. [Google Scholar] [CrossRef] [PubMed]
- Barker, M.; Lawrence, W.T.; Skinner, T.C.; Haslam, C.O.; Robinson, S.M.; Inskip, H.M.; Margetts, B.M.; Jackson, A.A.; Barker, D.J.; Cooper, C. Constraints on the food choices of women with lower educational attainment. Pubic Health Nutr. 2008, 11, 1229–1237. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, W.; Skinner, C.; Haslam, C.; Robinson, S.; Inskip, H.; Barker, D.; Cooper, C.; Jackson, A.; Barker, M. Why women of lower educational attainment struggle to make healthier food choices: The importance of psychological and social factors. Psychol. Health 2009, 24, 1003–1020. [Google Scholar] [CrossRef] [PubMed]
- Rycroft-Malone, J.; Seers, K.; Chandler, J.; Hawkes, C.; Crichton, N.; Allen, C.; Bullock, I.; Strunin, L. The role of evidence, context, and facilitation in an implementation trial: Implications for the development of the PARIHS framework. Implement. Sci. 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Rychetnik, L.; Bauman, A.; Laws, R.; King, L.; Rissel, C.; Nutbeam, D.; Colagiuri, S.; Caterson, I. Translating research for evidence-based public health: key concepts and future directions. J. epidemiol. Community Health 2012, 66, 1187–1192. [Google Scholar] [CrossRef] [PubMed]
- Belsky, J.; Melhuish, E.; Barnes, J.; Leyland, A.H.; Romaniuk, H. Effects of sure start local programmes on children and families: Early findings from a quasi-experimental, cross-sectional study. BMJ 2006, 332. [Google Scholar] [CrossRef] [PubMed]
- May, C. Agency and implementation: Understanding the embedding of healthcare innovations in practice. Soc. Sci. Med. 2012, 78, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Spoth, R.; Greenberg, M. Impact challenges in community science-with-practice: Lessons from prosper on transformative practitioner-scientist partnerships and prevention infrastructure development. Am. J. Community Psychol. 2011, 48, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Edwards, R.W.; Jumper-Thurman, P.; Plested, B.A.; Oetting, E.R.; Swanson, L. Community readiness: Research to practice. J. Community Psychol. 2000, 28, 291–307. [Google Scholar] [CrossRef]
- Kok, M.O.; Vaandrager, L.; Bal, R.; Schuit, J. Practitioner opinions on health promotion interventions that work: Opening the ‘black box’ of a linear evidence-based approach. Soc. Sci. Med. 2012, 74, 715–723. [Google Scholar] [CrossRef] [PubMed]
| BCT Group No. | BCT Group Name | BCT No. | BCT | Example of Activity Component in HCS Training |
|---|---|---|---|---|
| 1 | Goals & planning | 1.2 | Problem-solving | Prompt trainees to generate/select strategies to overcome barriers & increase facilitators to using HCS in routine practice; includes “relapse prevention” & “coping planning”. |
| 1.6 | Discrepancy between current behaviour & goal | Draw trainee’s attention to discrepancies between current practice and plans/goals to incorporate HCS into practice. | ||
| 3 | Social support | 3.2 | Social support (practical) | Group training & pair work provides practical support (listening & sharing tips) for practising HCS in the training & later in the workplace. |
| 3.3 | Social support (emotional) | Group training & pair work provides emotional support (encouragement/praise) for practising HCS in a safe/comfortable environment. | ||
| 4 | Shaping knowledge | 4.1 | Instruction on how to perform the behaviour | Skills training, including exploration & agreement on how to develop questions, support SMARTER planning etc. |
| 4.2 | Information on antecedents | Review with trainees what predicts behaviour (& possible relapse to old behaviour patterns), e.g., when under time pressure might revert to telling or suggesting. | ||
| 6 | Comparison of behaviour | 6.1 | Demonstration of the behaviour | Trainees growing awareness that HCS is being modelled by the trainer in all activities, & increasingly by other trainees in real/role play activities. |
| 7 | Associations | 7.1 | Prompts & cues | Resources provided in the training room to prompt use of the skills throughout the training; hand-outs to be used by trainees in their workplace to remind to use HCS. |
| 8 | Repetition & substitution | 8.1 | Behavioural practice/rehearsal | Prompt practice of HCS in training room by providing numerous opportunities. |
| 8.3 | Habit formation | Prompt practice of HCS in real world, by encouraging action-planning and problem-solving. | ||
| 8.6 | Generalisation of a target behaviour | If trainee has used HCS with friend/relative, encourage to try out skills in workplace. | ||
| 6 | Comparison of behaviour | 6.2 | Social comparison | Opportunities to compare own practice & experiences with others, including pre-training behaviour and then increasing use of HCS. |
| 13 | Identity | 13.3 | Incompatible beliefs | Draw attention to discrepancy between current/past practice and view of self as effective health practitioner. Embedding HCS is one way to reduce these incompatible beliefs & discrepancies. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barker, M.; Baird, J.; Tinati, T.; Vogel, C.; Strömmer, S.; Rose, T.; Begum, R.; Jarman, M.; Davies, J.; Thompson, S.; et al. Translating Developmental Origins: Improving the Health of Women and Their Children Using a Sustainable Approach to Behaviour Change. Healthcare 2017, 5, 17. https://doi.org/10.3390/healthcare5010017
Barker M, Baird J, Tinati T, Vogel C, Strömmer S, Rose T, Begum R, Jarman M, Davies J, Thompson S, et al. Translating Developmental Origins: Improving the Health of Women and Their Children Using a Sustainable Approach to Behaviour Change. Healthcare. 2017; 5(1):17. https://doi.org/10.3390/healthcare5010017
Chicago/Turabian StyleBarker, Mary, Janis Baird, Tannaze Tinati, Christina Vogel, Sofia Strömmer, Taylor Rose, Rufia Begum, Megan Jarman, Jenny Davies, Sue Thompson, and et al. 2017. "Translating Developmental Origins: Improving the Health of Women and Their Children Using a Sustainable Approach to Behaviour Change" Healthcare 5, no. 1: 17. https://doi.org/10.3390/healthcare5010017






