Effects of Prolonged Serum Calcium Suppression during Extracorporeal Cardiopulmonary Resuscitation in Pigs
Abstract
:1. Introduction
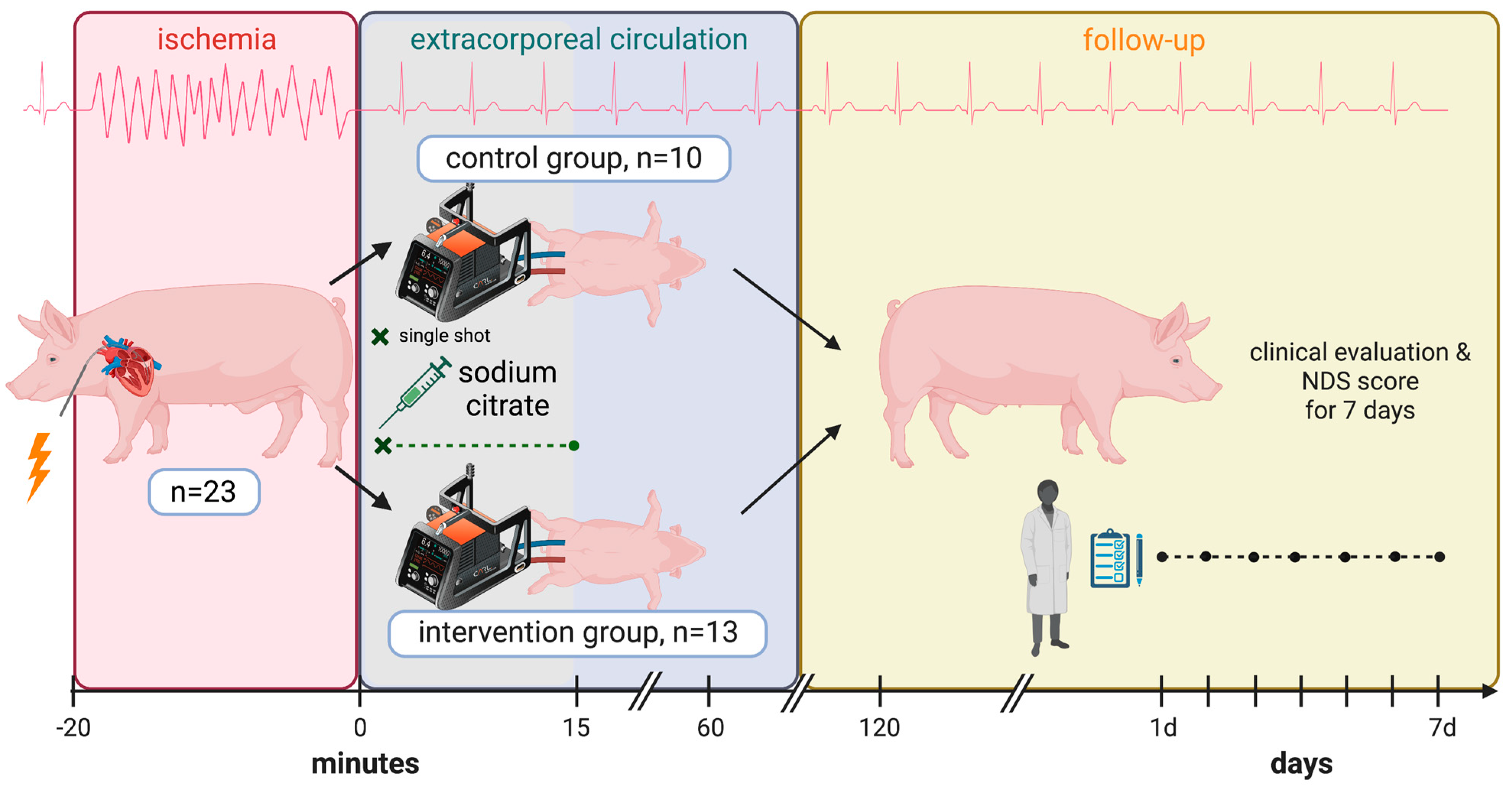
2. Materials and Methods
2.1. Preoperative Management and Anesthesia
2.2. Blood Sampling and Induction of Cardiac Arrest
2.3. Controlled Reperfusion (CARL Protocol) and Citrate Addition
2.4. Postoperative Care and Clinical Assessment
2.5. Statistical Analysis
3. Results
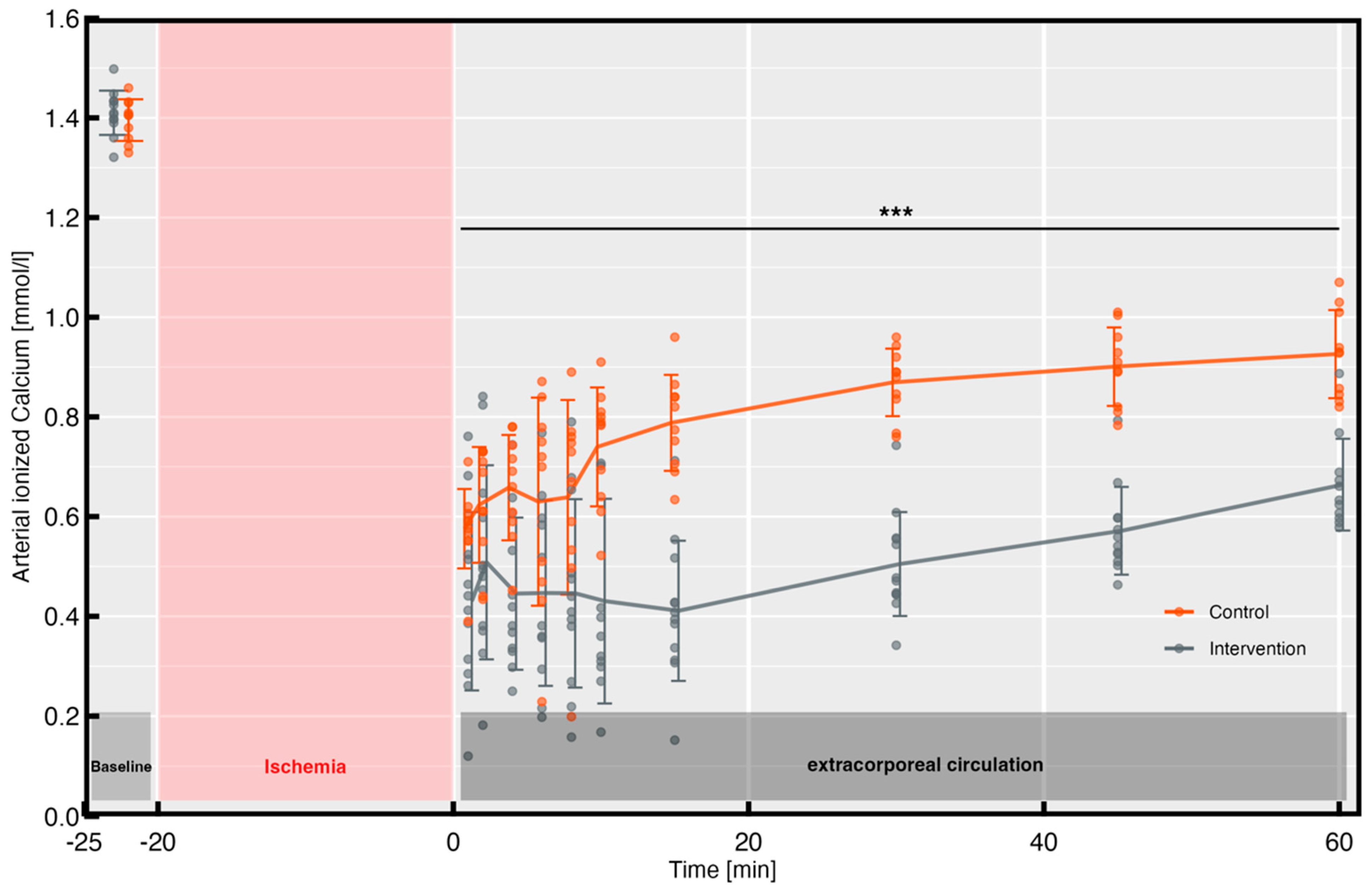
3.1. Ionized Arterial Calcium Levels
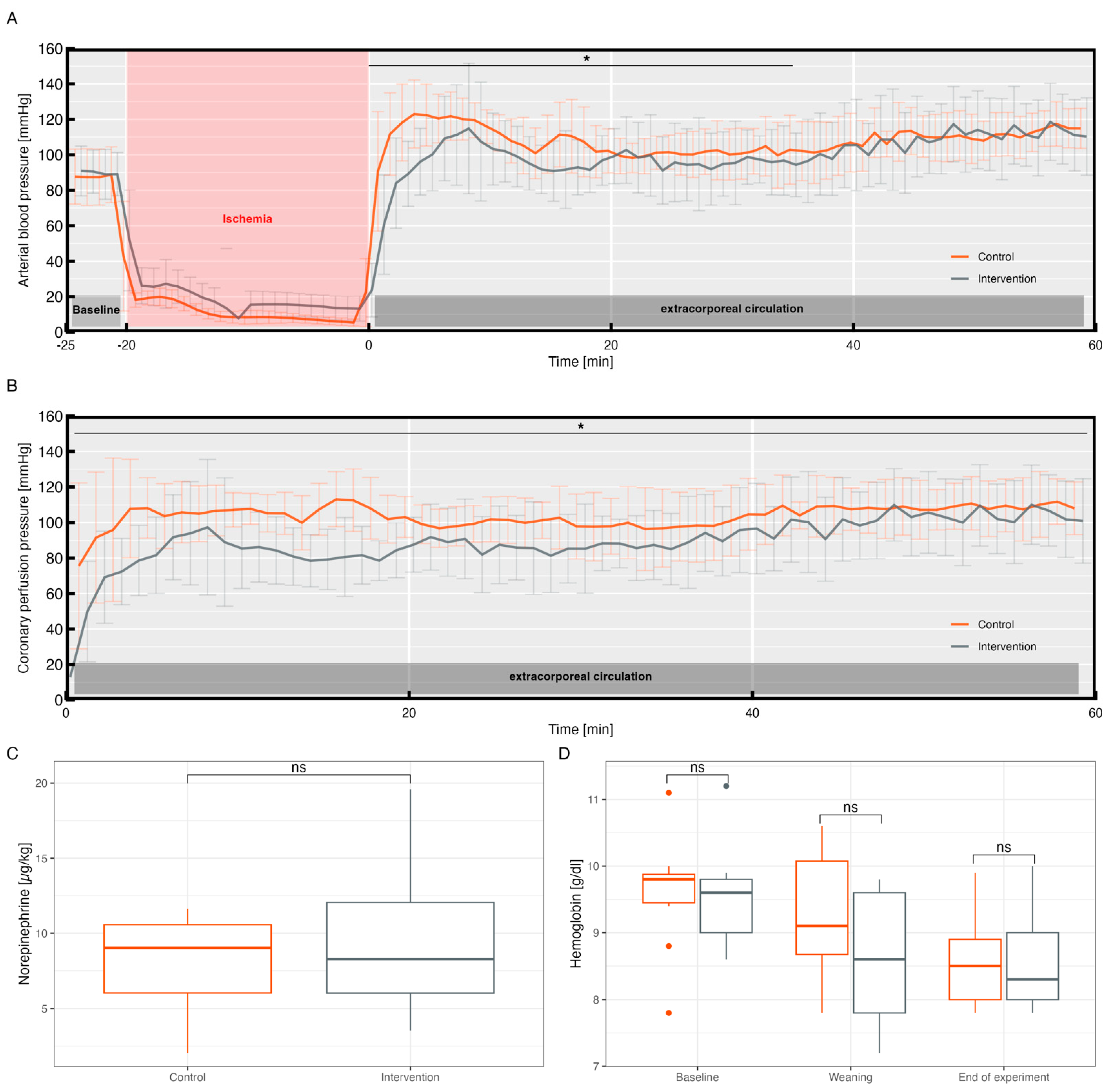
3.2. Hemodynamics and Norepinephrine Requirement
3.3. Cardiac Arrhythmias and Bleeding
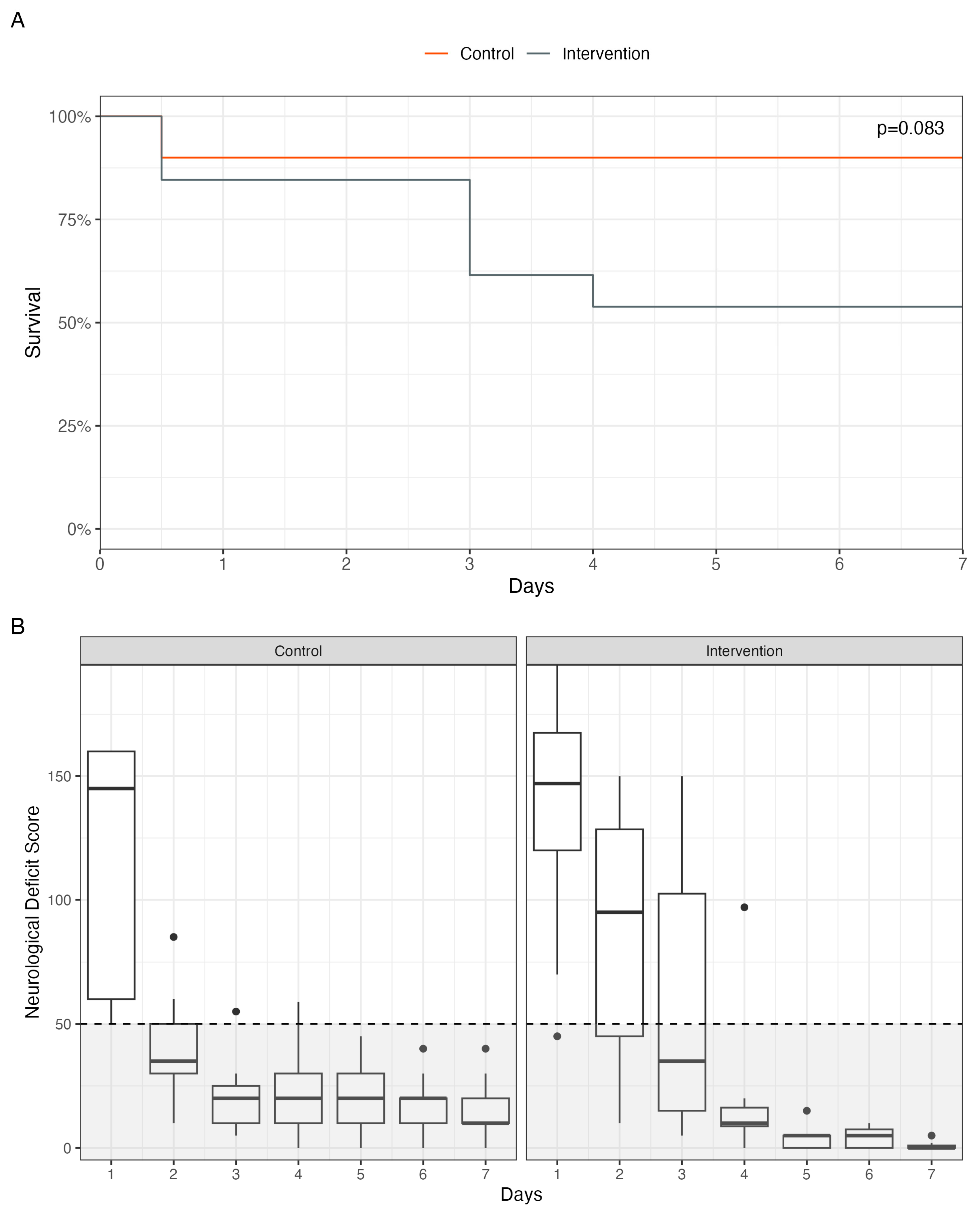
3.4. Survival and Neurological Deficit
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reynolds, J.C.; Grunau, B.E.; Rittenberger, J.C.; Sawyer, K.N.; Kurz, M.C.; Callaway, C.W. Association Between Duration of Resuscitation and Favorable Outcome After Out-of-Hospital Cardiac Arrest. Circulation 2016, 134, 2084–2094. [Google Scholar] [CrossRef] [PubMed]
- Guy, A.; Kawano, T.; Besserer, F.; Scheuermeyer, F.; Kanji, H.D.; Christenson, J.; Grunau, B. The relationship between no-flow interval and survival with favourable neurological outcome in out-of-hospital cardiac arrest: Implications for outcomes and ECPR eligibility. Resuscitation 2020, 155, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Gräsner, J.-T.; Herlitz, J.; Tjelmeland, I.B.M.; Wnent, J.; Masterson, S.; Lilja, G.; Bein, B.; Bottiger, B.W.; Rosell-Ortiz, F.; Nolan, J.P.; et al. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe. Resuscitation 2021, 161, 61–79. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.; et al. Heart Disease and Stroke Statistics-2020 Update: A Report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- Moulaert, V.R.M.P.; Verbunt, J.A.; van Heugten, C.M.; Wade, D.T. Cognitive impairments in survivors of out-of-hospital cardiac arrest: A systematic review. Resuscitation 2009, 80, 297–305. [Google Scholar] [CrossRef]
- Daniele, S.G.; Trummer, G.; Hossmann, K.A.; Vrselja, Z.; Benk, C.; Gobeske, K.T.; Damjanovic, D.; Andrijevic, D.; Pooth, J.-S.; Dellal, D.; et al. Brain vulnerability and viability after ischaemia. Nat. Rev. Neurosci. 2021, 22, 553–572. [Google Scholar] [CrossRef]
- Kalogeris, T.; Baines, C.P.; Krenz, M.; Korthuis, R.J. Chapter Six—Cell Biology of Ischemia/Reperfusion Injury. In International Review of Cell and Molecular Biology; Jeon, K.W., Ed.; Academic Press: Cambridge, MA, USA, 2012; Volume 298, pp. 229–317. [Google Scholar] [CrossRef]
- Taunyane, I.C.; Benk, C.; Beyersdorf, F.; Foerster, K.; Cristina Schmitz, H.; Wittmann, K.; Mader, I.; Doostkam, S.; Heilmann, C.; Trummer, G. Preserved brain morphology after controlled automated reperfusion of the whole body following normothermic circulatory arrest time of up to 20 minutes. Eur. J. Cardio-Thorac. Surg. 2016, 50, 1025–1034. [Google Scholar] [CrossRef]
- Beyersdorf, F.; Trummer, G.; Benk, C.; Pooth, J.-S. Application of cardiac surgery techniques to improve the results of cardiopulmonary resuscitation after cardiac arrest: Controlled automated reperfusion of the whole body. JTCVS Open 2021, 8, 47–52. [Google Scholar] [CrossRef]
- Pooth, J.-S.; Brixius, S.J.; Scherer, C.; Diel, P.; Liu, Y.; Taunyane, I.C.; Damjanovic, D.; Wolkewitz, M.; Haberstroh, J.; Benk, C.; et al. Limiting calcium overload after cardiac arrest: The role of human albumin in controlled automated reperfusion of the whole body. Perfusion 2023, 38, 622–630. [Google Scholar] [CrossRef]
- Choi, D.W. Calcium-mediated neurotoxicity: Relationship to specific channel types and role in ischemic damage. Trends Neurosci. 1988, 11, 465–469. [Google Scholar] [CrossRef]
- Szydlowska, K.; Tymianski, M. Calcium, ischemia and excitotoxicity. Cell Calcium 2010, 47, 122–129. [Google Scholar] [CrossRef]
- Orrenius, S.; Zhivotovsky, B.; Nicotera, P. Regulation of cell death: The calcium–apoptosis link. Nat. Rev. Mol. Cell. Biol. 2003, 4, 552–565. [Google Scholar] [CrossRef]
- Sanada, S.; Komuro, I.; Kitakaze, M. Pathophysiology of myocardial reperfusion injury: Preconditioning, postconditioning, and translational aspects of protective measures. Am. J. Physiol. Heart Circ. Physiol. 2011, 301, H1723–H1741. [Google Scholar] [CrossRef]
- Murphy, E.; Steenbergen, C. Ion Transport and Energetics During Cell Death and Protection. Physiology 2008, 23, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Baines, C.P. The mitochondrial permeability transition pore and ischemia-reperfusion injury. Basic Res. Cardiol. 2009, 104, 181–188. [Google Scholar] [CrossRef]
- Blaustein, M.P.; Lederer, W.J. Sodium/Calcium Exchange: Its Physiological Implications. Physiol. Rev. 1999, 79, 763–854. [Google Scholar] [CrossRef] [PubMed]
- White, C.; Ambrose, E.; Müller, A.; Hatami, S.; Li, Y.; Le, H.; Thilveris, J.; Arora, R.; Lee, T.; Dixon, I.; et al. Impact of Reperfusion Calcium and pH on the Resuscitation of Hearts Donated After Circulatory Death. Ann. Thorac. Surg. 2017, 103, 122–130. [Google Scholar] [CrossRef]
- Schäfer, C. Role of the reverse mode of the Na+/Ca2+ exchanger in reoxygenation-induced cardiomyocyte injury. Cardiovasc. Res. 2001, 51, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Talukder, M.A.H.; Zweier, J.L.; Periasamy, M. Targeting calcium transport in ischaemic heart disease. Cardiovasc. Res. 2009, 84, 345–352. [Google Scholar] [CrossRef]
- Iijima, T.; Bauer, R.; Hossmann, K.-A. Brain resuscitation by extracorporeal circulation after prolonged cardiac arrest in cats. Intensive Care Med. 1993, 19, 82–88. [Google Scholar] [CrossRef]
- Lee, G.; Arepally, G.M. Anticoagulation techniques in apheresis: From heparin to citrate and beyond. J. Clin. Apher. 2012, 27, 117–125. [Google Scholar] [CrossRef]
- Fukuhiro, Y.; Wowk, M.; Ou, R.; Rosenfeldt, F.; Pepe, S. Cardioplegic Strategies for Calcium Control. Circulation 2000, 102, 319–325. [Google Scholar] [CrossRef]
- Richardson, A.C.; Tonna, J.E.; Nanjayya, V.; Nixon, P.; Abrams, D.C.; Raman, L.; Bernard, S.; Finney, S.; Grunau, B.; Youngquist, S.; et al. Extracorporeal Cardiopulmonary Resuscitation in Adults. Interim Guideline Consensus Statement from the Extracorporeal Life Support Organization. ASAIO J. 2021, 67, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Brixius, S.J.; Pooth, J.-S.; Haberstroh, J.; Damjanovic, D.; Scherer, C.; Greiner, P.; Benk, C.; Beyersdorf, F.; Trummer, G. Beneficial Effects of Adjusted Perfusion and Defibrillation Strategies on Rhythm Control within Controlled Automated Reperfusion of the Whole Body (CARL) for Refractory Out-of-Hospital Cardiac Arrest. J. Clin. Med. 2022, 11, 2111. [Google Scholar] [CrossRef] [PubMed]
- Forbess, J.M.; Ibla, J.C.; Lidov, H.G.; Cioffi, M.A.; Hiramatsu, T.; Laussen, P.; Miura, T.; Jonas, R.A. University of Wisconsin cerebroplegia in a piglet survival model of circulatory arrest. Ann. Thorac. Surg. 1995, 60, S494–S500. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Garcia-Dorado, D.; Piper, H.M. Postconditioning: Reperfusion of “reperfusion injury” after hibernation. Cardiovasc. Res. 2006, 69, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Eisner, D.A.; Caldwell, J.L.; Kistamás, K.; Trafford, A.W. Calcium and Excitation-Contraction Coupling in the Heart. Circ. Res. 2017, 121, 181–195. [Google Scholar] [CrossRef]
- Spronk, H.M.H.; Govers-Riemslag, J.W.P.; ten Cate, H. The blood coagulation system as a molecular machine. Bioessays 2003, 25, 1220–1228. [Google Scholar] [CrossRef]
- Borah, M.; Dhar, S.; Gogoi, D.M.; Ruram, A.A. Association of Serum Calcium Levels with Infarct Size in Acute Ischemic Stroke: Observations from Northeast India. J. Neurosci. Rural Pract. 2016, 7, S041–S045. [Google Scholar] [CrossRef]
- Chung, J.-W.; Ryu, W.-S.; Kim, B.J.; Yoon, B.-W. Elevated Calcium after Acute Ischemic Stroke: Association with a Poor Short-Term Outcome and Long-Term Mortality. J. Stroke 2015, 17, 54–59. [Google Scholar] [CrossRef]
- Feingold, P.; Mina, M.J.; Burke, R.M.; Hashimoto, B.; Gregg, S.; Martin, G.S.; Leeper, K.; Buchman, T. Long-term survival following in-hospital cardiac arrest: A matched cohort study. Resuscitation 2016, 99, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Schluep, M.; Gravesteijn, B.Y.; Stolker, R.J.; Endeman, H.; Hoeks, S.E. One-year survival after in-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation 2018, 132, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Philipp, A.; Pooth, J.-S.; Benk, C.; Mueller, T.; Lunz, D. Enabling the control of reperfusion parameters in out-of-hospital cardiac arrest: First applications of the CARL system. Perfusion 2023, 38, 436–439. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.; Hossmann, K.-A. No-reflow after cardiac arrest. Intensive Care Med. 1995, 21, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Fischer, E.G.; Ames, A.; Lorenzo, A.V. Cerebral blood flow immediately following brief circulatory stasis. Stroke 1979, 10, 423–427. [Google Scholar] [CrossRef]
- Reynolds, J.C.; Salcido, D.D.; Menegazzi, J.J. Conceptual models of coronary perfusion pressure and their relationship to defibrillation success in a porcine model of prolonged out-of-hospital cardiac arrest. Resuscitation 2012, 83, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Bhate, T.D.; McDonald, B.; Sekhon, M.S.; Griesdale, D.E.G. Association between blood pressure and outcomes in patients after cardiac arrest: A systematic review. Resuscitation 2015, 97, 1–6. [Google Scholar] [CrossRef]
- Leunissen, K.M.; van den Berg, B.W.; van Hooff, J.P. Ionized calcium plays a pivotal role in controlling blood pressure during haemodialysis. Blood Purif. 1989, 7, 233–239. [Google Scholar] [CrossRef]
- Bělohlávek, J.; Mlček, M.; Huptych, M.; Svoboda, T.; Havránek, Š.; Ošt’ádal, P.; Bouček, T.; Kovárník, T.; Mlejnský, F.; Mrázek, V.; et al. Coronary versus carotid blood flow and coronary perfusion pressure in a pig model of prolonged cardiac arrest treated by different modes of venoarterial ECMO and intraaortic balloon counterpulsation. Crit. Care 2012, 16, R50. [Google Scholar] [CrossRef]
- Hutin, A.; Lamhaut, L.; Lidouren, F.; Kohlhauer, M.; Mongardon, N.; Carli, P.; Berdeaux, A.; Ghaleh, B.; Tissier, R. Early Coronary Reperfusion Facilitates Return of Spontaneous Circulation and Improves Cardiovascular Outcomes After Ischemic Cardiac Arrest and Extracorporeal Resuscitation in Pigs. J. Am. Heart Assoc. 2016, 5, e004588. [Google Scholar] [CrossRef]
- Hutin, A.; Abu-Habsa, M.; Burns, B.; Bernard, S.; Bellezzo, J.; Shinar, Z.; Torres, E.C.; Gueugniaud, P.-Y.; Carli, P.; Lamhaut, L. Early ECPR for out-of-hospital cardiac arrest: Best practice in 2018. Resuscitation 2018, 130, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Sardu, C.; Santulli, G.; Guerra, G.; Trotta, M.C.; Santamaria, M.; Sacra, C.; Testa, N.; Ducceschi, V.; Gatta, G.; D’Amico, M.; et al. Modulation of SERCA in Patients with Persistent Atrial Fibrillation Treated by Epicardial Thoracoscopic Ablation: The CAMAF Study. J. Clin. Med. 2020, 9, 544. [Google Scholar] [CrossRef] [PubMed]

| Group | Arrhythmias During ECC | Postoperative Arrhythmias | ||
|---|---|---|---|---|
| N | p-Value | N | p-Value | |
| Control, N = 10 | 4/10 | 0.10 | 2/10 | 0.66 |
| Intervention, N = 13 | 10/13 | 4/13 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pooth, J.-S.; Liu, Y.; Petzold, R.; Scherer, C.; Benning, L.; Kreibich, M.; Czerny, M.; Beyersdorf, F.; Benk, C.; Trummer, G.; et al. Effects of Prolonged Serum Calcium Suppression during Extracorporeal Cardiopulmonary Resuscitation in Pigs. Biomedicines 2023, 11, 2612. https://doi.org/10.3390/biomedicines11102612
Pooth J-S, Liu Y, Petzold R, Scherer C, Benning L, Kreibich M, Czerny M, Beyersdorf F, Benk C, Trummer G, et al. Effects of Prolonged Serum Calcium Suppression during Extracorporeal Cardiopulmonary Resuscitation in Pigs. Biomedicines. 2023; 11(10):2612. https://doi.org/10.3390/biomedicines11102612
Chicago/Turabian StylePooth, Jan-Steffen, Yechi Liu, Ralf Petzold, Christian Scherer, Leo Benning, Maximilian Kreibich, Martin Czerny, Friedhelm Beyersdorf, Christoph Benk, Georg Trummer, and et al. 2023. "Effects of Prolonged Serum Calcium Suppression during Extracorporeal Cardiopulmonary Resuscitation in Pigs" Biomedicines 11, no. 10: 2612. https://doi.org/10.3390/biomedicines11102612







