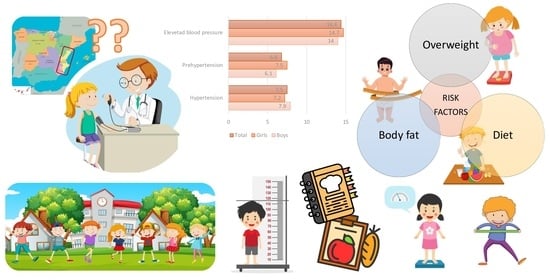
Cardiovascular Risk Assessment of Elevated Blood Pressure for Screening and Early Detection in Children 6 to 9 Years of Age in the Valencian Community: ANIVA Study
Abstract
:1. Introduction
2. Methods
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N. Heart Disease and Stroke statistics—2020 Update: A Report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Hypertension. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 15 May 2023).
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting Adult Obesity from Childhood Obesity: A Systematic Review and Meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wang, Y. Tracking of Blood Pressure from Childhood to Adulthood: A Systematic Review and Meta–regression Analysis. Circulation 2008, 117, 3171–3180. [Google Scholar] [CrossRef] [PubMed]
- Berenson, G.S.; Bogalusa Heart Study Research Group. Childhood Risk Factors Predict Adult Risk Associated with Subclinical Cardiovascular Disease: The Bogalusa Heart Study. Am. J. Cardiol. 2002, 90, L3–L7. [Google Scholar] [CrossRef] [PubMed]
- Franks, P.W.; Hanson, R.L.; Knowler, W.C.; Sievers, M.L.; Bennett, P.H.; Looker, H.C. Childhood Obesity, Other Cardiovascular Risk Factors, and Premature Death. N. Engl. J. Med. 2010, 362, 485–493. [Google Scholar] [CrossRef]
- Abrignani, M.G.; Luca, F.; Favilli, S.; Benvenuto, M.; Rao, C.M.; Di Fusco, S.A.; Gabrielli, D.; Gulizia, M.M.; Cardiovascular Prevention Area, Young Cardiologists Area, and Paediatric Cardiology Task Force of the Associazione Nazionale Medici Cardiologi Ospedalieri (ANMCO), and Heart Care Foundation. Lifestyles and Cardiovascular Prevention in Childhood and Adolescence. Pediatr. Cardiol. 2019, 40, 1113–1125. [Google Scholar] [CrossRef] [PubMed]
- Haseler, E.; Sinha, M.D. Hypertension in Children and Young Adults. Pediatr. Clin. 2022, 69, 1165–1180. [Google Scholar] [CrossRef]
- Song, P.; Zhang, Y.; Yu, J.; Zha, M.; Zhu, Y.; Rahimi, K.; Rudan, I. Global Prevalence of Hypertension in Children: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2019, 173, 1154–1163. [Google Scholar] [CrossRef]
- Sun, J.; Steffen, L.M.; Ma, C.; Liang, Y.; Xi, B. Definition of Pediatric Hypertension: Are Blood Pressure Measurements on Three Separate Occasions Necessary? Hypertens. Res. 2017, 40, 496–503. [Google Scholar] [CrossRef]
- Lurbe, E.; Torro, I.; Alvarez, J.; Aguilar, F.; Mancia, G.; Redon, J.; Redon, P. Impact of ESH and AAP Hypertension Guidelines for Children and Adolescents on Office and Ambulatory Blood Pressure-Based Classifications. J. Hypertens. 2019, 37, 2414–2421. [Google Scholar] [CrossRef]
- De Simone, G.; Mancusi, C.; Hanssen, H.; Genovesi, S.; Lurbe, E.; Parati, G.; Sendzikaite, S.; Valerio, G.; Di Bonito, P.; Di Salvo, G. Hypertension in Children and Adolescents: A Consensus Document from ESC Council on Hypertension, European Association of Preventive Cardiology, European Association of Cardiovascular Imaging, Association of Cardiovascular Nursing & Allied Professions, ESC Council for Cardiology Practice and Association for European Paediatric and Congenital Cardiology. Eur. Heart J. 2022, 43, 3290–3301. [Google Scholar] [PubMed]
- De Ferranti, S.D.; Steinberger, J.; Ameduri, R.; Baker, A.; Gooding, H.; Kelly, A.S.; Mietus-Snyder, M.; Mitsnefes, M.M.; Peterson, A.L.; St-Pierre, J. Cardiovascular Risk Reduction in High-Risk Pediatric Patients: A Scientific Statement from the American Heart Association. Circulation 2019, 139, e603–e634. [Google Scholar] [CrossRef] [PubMed]
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A. Worldwide Trends in Body-Mass Index, Underweight, Overweight, and Obesity from 1975 to 2016: A Pooled Analysis of 2416 Population-Based Measurement Studies in 128· 9 Million Children, Adolescents, and Adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- Skinner, A.C.; Perrin, E.M.; Moss, L.A.; Skelton, J.A. Cardiometabolic Risks and Severity of Obesity in Children and Young Adults. N. Engl. J. Med. 2015, 373, 1307–1317. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.S.; Barlow, S.E.; Rao, G.; Inge, T.H.; Hayman, L.L.; Steinberger, J.; Urbina, E.M.; Ewing, L.J.; Daniels, S.R. Severe Obesity in Children and Adolescents: Identification, Associated Health Risks, and Treatment Approaches: A Scientific Statement from the American Heart Association. Circulation 2013, 128, 1689–1712. [Google Scholar] [CrossRef] [PubMed]
- Sorof, J.M.; Lai, D.; Turner, J.; Poffenbarger, T.; Portman, R.J. Overweight, Ethnicity, and the Prevalence of Hypertension in School-Aged Children. Pediatrics 2004, 113, 475–482. [Google Scholar] [CrossRef]
- World Health Organization. WHO Child Growth Standards: Length/Height for Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age, Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- de la Cerda Ojeda, F.; Herrero Hernando, C. Hipertensión Arterial En Niños Y Adolescentes. Protoc. Diagnósticos Ter. Pediatría 2014, 1, 171–189. [Google Scholar]
- American Academy of Pediatrics. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. Pediatrics 2004, 114, 555–576. [Google Scholar]
- Flynn, J.T.; Kaelber, D.C.; Baker-Smith, C.M.; Blowey, D.; Carroll, A.E.; Daniels, S.R.; de Ferranti, S.D.; Dionne, J.M.; Falkner, B.; Flinn, S.K. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017, 140, e20171904. [Google Scholar] [CrossRef]
- Barrett-Connor, E. Nutrition Epidemiology: How do we Know what they Ate? Am. J. Clin. Nutr. 1991, 54, 182S–187S. [Google Scholar] [CrossRef] [PubMed]
- Federación Española de Sociedades de Nutrición, Alimentación y Dietética (FESNAD). Ingestas Dietéticas De Referencia (IDR) Para La Población Española, 2010. Act. Dietética 2010, 14, 196–197. [Google Scholar] [CrossRef]
- Kass, G.V. An Exploratory Technique for Investigating Large Quantities of Categorical Data. J. R. Stat. Soc. Ser. C (Appl. Stat. ) 1980, 29, 119–127. [Google Scholar] [CrossRef]
- Beckett, L.A.; Rosner, B.; Roche, A.F.; Guo, S. Serial Changes in Blood Pressure from Adolescence into Adulthood. Am. J. Epidemiol. 1992, 135, 1166–1177. [Google Scholar] [CrossRef] [PubMed]
- Sorof, J.; Daniels, S. Obesity Hypertension in Children: A Problem of Epidemic Proportions. Hypertension 2002, 40, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Li, H. Waist Circumference as an Indicator of High Blood Pressure in Preschool Obese Children. Asia Pac. J. Clin. Nutr. 2011, 20, 557–562. [Google Scholar] [PubMed]
- Crispim, P.A.A.; Peixoto, M.d.R.G.; Jardim, P.C.B.V. Risk Factors Associated with High Blood Pressure in Two-to Five-Year-Old Children. Arq. Bras. Cardiol. 2014, 102, 39–46. [Google Scholar] [CrossRef]
- Chiolero, A.; Madeleine, G.; Gabriel, A.; Burnier, M.; Paccaud, F.; Bovet, P. Prevalence of Elevated Blood Pressure and Association with Overweight in Children of a Rapidly Developing Country. J. Hum. Hypertens. 2007, 21, 120. [Google Scholar] [CrossRef]
- Lo, J.C.; Sinaiko, A.; Chandra, M.; Daley, M.F.; Greenspan, L.C.; Parker, E.D.; Kharbanda, E.O.; Margolis, K.L.; Adams, K.; Prineas, R.; et al. Prehypertension and Hypertension in Community-Based Pediatric Practice. Pediatrics 2013, 131, 415. [Google Scholar] [CrossRef]
- Martín-Espinosa, N.; Díez-Fernández, A.; Sánchez-López, M.; Rivero-Merino, I.; Lucas-De La Cruz, L.; Solera-Martínez, M.; Martínez-Vizcaíno, V. Prevalence of High Blood Pressure and Association with Obesity in Spanish Schoolchildren Aged 4–6 Years Old. PLoS ONE 2017, 12, e0170926. [Google Scholar] [CrossRef]
- Morales-Suárez-Varela, M.; Mohino-Chocano, M.; Soler, C.; Llopis-Morales, A.; Peraita-Costa, I.; Llopis-González, A. Prevalencia De Hipertensión Arterial Y Su Asociación Con Antropometría Y Dieta En Niños (De Seis a Nueve Años): Estudio ANIVA. Nutr. Hosp. 2019, 36, 133–141. [Google Scholar] [PubMed]
- Serra Majem, L.; Ribas Barba, L.; Aranceta Bartrina, J.; Pérez Rodrigo, C.; Saavedra Santana, P.; Peña Quintana, L. Obesidad Infantil Y Juvenil En España. Resultados Del Estudio enKid (1998–2000). Med. Clínica 2003, 121, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Eisenmann, J.C.; Wrede, J.; Heelan, K.A. Associations between Adiposity, Family History of CHD and Blood Pressure in 3–8 Year-Old Children. J. Hum. Hypertens. 2005, 19, 675. [Google Scholar] [CrossRef] [PubMed]
- Drozdz, D.; Kwinta, P.; Korohoda, P.; Pietrzyk, J.A.; Drozdz, M.; Sancewicz-Pach, K. Correlation between Fat Mass and Blood Pressure in Healthy Children. Pediatr. Nephrol. 2009, 24, 1735–1740. [Google Scholar] [CrossRef]
- Plachta-Danielzik, S.; Landsberg, B.; Johannsen, M.; Lange, D.; Müller, M.J. Association of Different Obesity Indices with Blood Pressure and Blood Lipids in Children and Adolescents. Br. J. Nutr. 2008, 100, 208–218. [Google Scholar] [CrossRef]
- Larsson, B.; Svardsudd, K.; Welin, L.; Wilhemsen, L.; Björntorp, P.; Tibblin, G. Abdominal Adipose Tissue Distribution, Obesity, and Risk of Cardiovascular Disease and Death: 13 Year Follow Up of Participants in the Study of Men Born in 1913. BMJ (Clin. Res. Ed.) 1984, 288, 1401–1404. [Google Scholar] [CrossRef]
- Santos-Beneit, G.; Sotos-Prieto, M.; Pocock, S.; Redondo, J.; Fuster, V.; Peñalvo, J.L. Asociación Entre Antropometría Y Presión Arterial Alta En Una Muestra Representativa De Preescolares De Madrid. Rev. Española De Cardiol. 2015, 68, 477–484. [Google Scholar] [CrossRef]
- Martínez-Vizcaíno, V.; Martínez, M.S.; Pacheco, B.N.; López, M.S.; García-Prieto, J.C.; Nino, C.T.; Palencia, N.A.; Aguilar, F.S.; Rodríguez-Artalejo, F. Trends in Excess of Weight, Underweight and Adiposity among Spanish Children from 2004 to 2010: The Cuenca Study. Public Health Nutr. 2012, 15, 2170–2174. [Google Scholar] [CrossRef]
- Abdulle, A.M.; Nagelkerke, N.J.; Abouchacra, S.; Pathan, J.Y.; Adem, A.; Obineche, E.N. Under-Treatment and Under Diagnosis of Hypertension: A Serious Problem in the United Arab Emirates. BMC Cardiovasc. Disord. 2006, 6, 24. [Google Scholar] [CrossRef]
- Hansen, M.L.; Gunn, P.W.; Kaelber, D.C. Underdiagnosis of Hypertension in Children and Adolescents. JAMA 2007, 298, 874–879. [Google Scholar] [CrossRef]




| Total (N = 1142) | Boys (n = 543) | Girls (n = 599) | p Value * | |
|---|---|---|---|---|
| Age (years) | 7.21 ± 1.00 | 7.24 ± 0.98 | 7.19 ± 1.02 | 0.422 |
| Height (cm) | 1.39 ± 3.75 | 1.29 ± 0.15 | 1.48 ± 5.17 | 0.391 |
| Height for age Z-score | 0.43 ± 1.03 | 0.51 ± 0.98 | 0.36 ± 108 | 0.012 |
| Weight (kg) | 28.51 ± 7.08 | 28.96 ± 7.14 | 28.10 ± 7.01 | 0.039 |
| Weight for age Z-score | 0.74 ± 1.75 | 0.87 ± 2.17 | 0.62 ± 1.25 | 0.018 |
| BMI (kg/m2) | 17.14 ± 2.82 | 17.21 ± 2.89 | 17.08 ± 2.75 | 0.426 |
| BMI | 0.062 | |||
| Underweight | 108 (9.5%) | 42 (7.7%) | 66 (11.0%) | 0.057 |
| Normal weight | 796 (69.7%) | 390 (71.8%) | 406 (67.8%) | 0.142 |
| Overweight | 194 (17.0%) | 85 (15.7%) | 109 (18.2%) | 0.262 |
| Obesity | 44 (3.9%) | 26 (4.8%) | 18 (3.0%) | 0.115 |
| BMI for age Z-score | 0.59 ± 1.23 | 0.67 ± 1.32 | 0.51 ± 1.13 | 0.028 |
| % lean body mass | 34.12 ± 51.39 | 32.65 ± 48.71 | 35.46 ± 53.70 | 0.357 |
| Waist circunference (cm) | 60.16 ± 15.22 | 60.46 ± 7.12 | 59.89 ± 19.89 | 0.525 |
| Hip circunference (cm) | 68.13 ± 7.47 | 68.39 ± 7.64 | 67.89 ± 7.31 | 0.261 |
| Waist-hip index (cm/cm) | 0.96 ± 2.61 | 1.05 ± 3.78 | 0.88 ± 0.32 | 0.280 |
| Triceps skinfold (mm) | 23.61 ± 38.89 | 23.54 ± 39.86 | 23.67 ± 38.02 | 0.955 |
| Biceps skinfold (mm) | 14.35 ± 24.44 | 14.28 ± 25.45 | 14.42 ± 23.50 | 0.922 |
| Abdominal skinfold (mm) | 22.81 ± 39.82 | 22.59 ± 41.41 | 23.01 ± 38.35 | 0.858 |
| Suprailiac skinfold (mm) | 19.52 ± 40.81 | 19.84 ± 44.24 | 19.23 ± 37.47 | 0.801 |
| SBP (mm Hg) | 99.76 ± 13.02 | 100.57 ± 13.07 | 99.02 ± 12.94 | 0.044 |
| DBP (mmHg) | 67.78 ± 29.57 | 67.66 ± 32.17 | 67.89 ± 27.03 | 0.897 |
| Blood pressure category | 0.580 | |||
| Normal | 978 (85.6%) | 468 (86.0%) | 510 (85.3%) | 0.736 |
| Prehypertension | 78 (6.8%) | 33 (6.1%) | 45 (7.5%) | 0.349 |
| Hypertension | 86 (7.5%) | 43 (7.9%) | 43 (7.2%) | 0.655 |
| Heart rate (ppm) | 87.76 ± 14.44 | 86.13 ± 13.92 | 89.23 ± 1474 | 0.001 |
| MBP (mmHg) ** | 78.33 ± 21.23 | 78.52 ± 22.95 | 78.16 ± 19.55 | 0.775 |
| PP (mmHg) *** | 31.97 ± 29.41 | 32.91 ± 31.76 | 31.13 ± 27.09 | 0.308 |
| KIDMED score | 7.00 ± 2.04 | 7.02 ± 2.05 | 6.97 ± 2.04 | 0.674 |
| KIDMED classification | 0.661 | |||
| Optimal | 464 (40.6%) | 228 (42.0%) | 236 (39.4%) | 0.372 |
| Needs improvement | 632 (55.3%) | 293 (54.0%) | 339 (56.6%) | 0.378 |
| Bad | 46 (4.0%) | 22 (4.1%) | 24 (4.0%) | 0.932 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morales-Suarez-Varela, M.; Peraita-Costa, I.; Llopis-Morales, A.; Navarro Perez, J. Cardiovascular Risk Assessment of Elevated Blood Pressure for Screening and Early Detection in Children 6 to 9 Years of Age in the Valencian Community: ANIVA Study. Children 2023, 10, 1928. https://doi.org/10.3390/children10121928
Morales-Suarez-Varela M, Peraita-Costa I, Llopis-Morales A, Navarro Perez J. Cardiovascular Risk Assessment of Elevated Blood Pressure for Screening and Early Detection in Children 6 to 9 Years of Age in the Valencian Community: ANIVA Study. Children. 2023; 10(12):1928. https://doi.org/10.3390/children10121928
Chicago/Turabian StyleMorales-Suarez-Varela, Maria, Isabel Peraita-Costa, Agustin Llopis-Morales, and Jorge Navarro Perez. 2023. "Cardiovascular Risk Assessment of Elevated Blood Pressure for Screening and Early Detection in Children 6 to 9 Years of Age in the Valencian Community: ANIVA Study" Children 10, no. 12: 1928. https://doi.org/10.3390/children10121928