Quality Improvement Project to Improve Hand Hygiene Compliance in a Level III Neonatal Intensive Care Unit
Abstract
:1. Introduction
2. Materials and Methods
2.1. Interventions
2.1.1. PDSA Cycle 1 and First Intervention
2.1.2. PDSA Cycle 2 and Second Intervention
2.1.3. PDSA Cycle 3 and Third Intervention
2.2. Key Measures
2.2.1. Outcome Measures
- The overall compliance with HH in the unit, which is calculated as the percentage of times HH was performed out of the total number of observed opportunities for HH in a day.
- Compliance rates for each of the nine HH opportunities observed. This was calculated as the percentage of times HH was performed for a specific HH opportunity out of the total number of observed opportunities for that HH opportunity in a day.
2.2.2. Process Measures
- PDSA 1 and 2 cycles: Number of educational interventions, including presentations and flyers given.
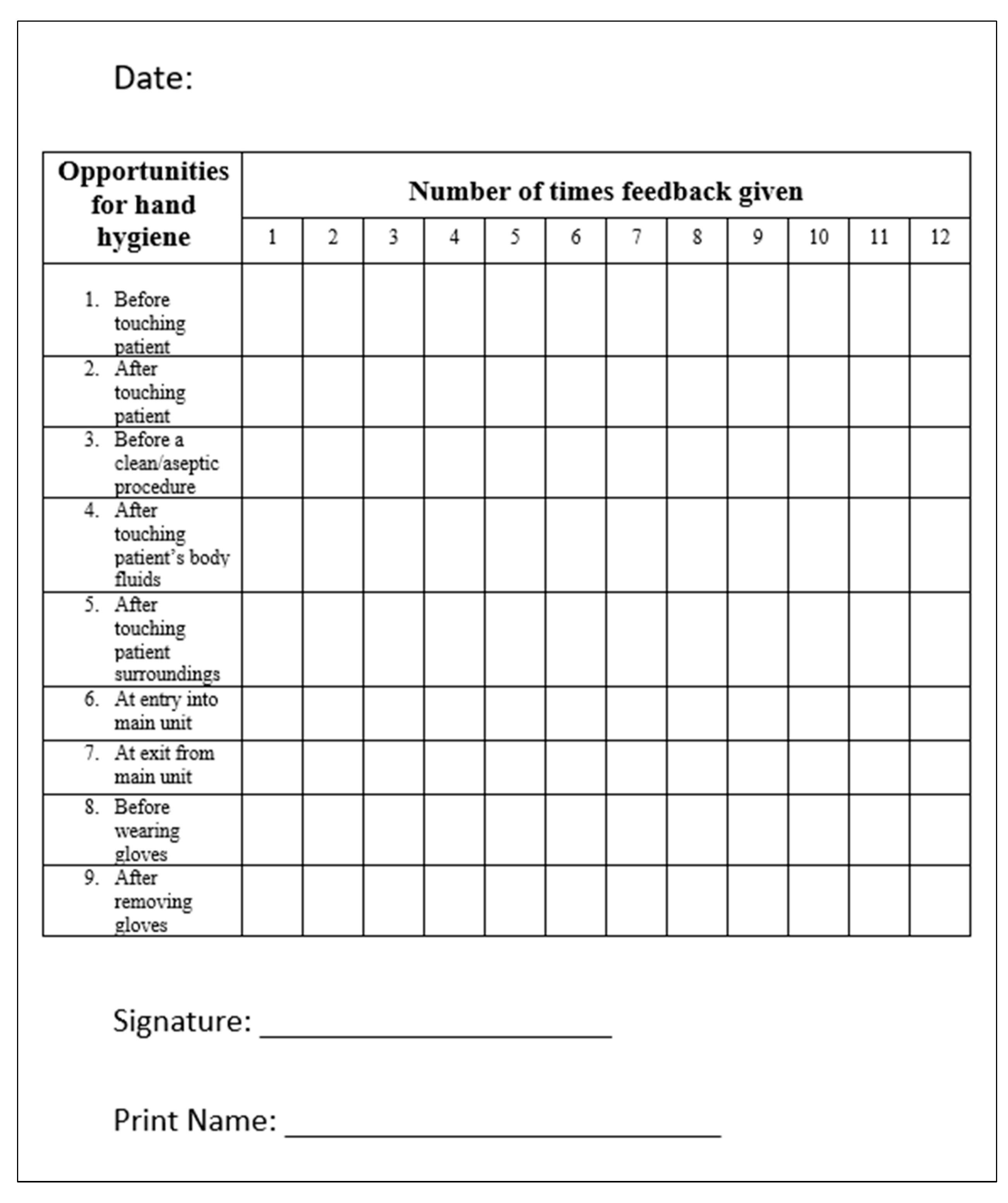
- PDSA 3 cycle: Number of times immediate feedback was given in a day.
2.2.3. Balancing Measures
- Perceived increase in work burden and interference with patient care by HCWs. This was assessed using individual surveys conducted among the HCWs during PDSA cycles 2 and 3.
2.3. Statistical Considerations
2.3.1. Sample Size
2.3.2. Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Healthcare Associated Infections. 2018. Available online: https://cdc.gov/hai/data/index.html (accessed on 27 August 2022).
- Pittet, D.; Hugonnet, S.; Harbarth, S.; Mourouga, P.; Sauvan, V.; Touveneau, S.; Perneger, T.V. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet 2000, 356, 1307–1312, Erratum in Lancet 2000, 356, 2196. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.D.; Robbins, G.; Quinn, J.; Arbogast, J.W. The impact of COVID-19 pandemic on hand hygiene performance in hospitals. Am. J. Infect. Control 2021, 49, 30–33. [Google Scholar] [CrossRef]
- Musu, M.; Lai, A.; Mereu, N.; Galletta, M.; Campagna, M.; Tidore, M.; Piazza, M.; Spada, L.; Massidda, M.; Colombo, S.; et al. Assessing hand hygiene compliance among healthcare workers in six Intensive Care Units. J. Prev. Med. Hyg. 2017, 58, E231–E237. [Google Scholar] [PubMed]
- Sax, H.; Allegranzi, B.; Uçkay, I.; Larson, E.; Boyce, J.; Pittet, D. ‘My five moments for hand hygiene’: A user-centred design approach to understand, train, monitor and report hand hygiene. J. Hosp. Infect. 2007, 67, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Gopalakrishnan, S.; Chaurasia, S.; Sankar, M.J.; Paul, V.K.; Deorari, A.K.; Joshi, M.; Agarwal, R. Stepwise interventions for improving hand hygiene compliance in a level 3 academic neonatal intensive care unit in north India. J. Perinatol. 2021, 41, 2834–2839. [Google Scholar] [CrossRef]
- Brotfain, E.; Livshiz-Riven, I.; Gushansky, A.; Erblat, A.; Koyfman, L.; Ziv, T.; Saidel-Odes, L.; Klein, M.; Borer, A. Monitoring the hand hygiene compliance of health care workers in a general intensive care unit: Use of continuous closed circle television versus overt observation. Am. J. Infect. Control 2017, 45, 849–854. [Google Scholar] [CrossRef]
- Barroso, V.; Caceres, W.; Loftus, P.; Evans, K.H.; Shieh, L. Hand hygiene of medical students and resident physicians: Predictors of attitudes and behaviour. Postgrad. Med. J. 2016, 92, 497–500. [Google Scholar] [CrossRef]
- Sax, H.; Allegranzi, B.; Chraïti, M.-N.; Boyce, J.; Larson, E.; Pittet, D. The World Health Organization hand hygiene observation method. Am. J. Infect. Control 2009, 37, 827–834. [Google Scholar] [CrossRef]
- WHO. Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Available online: https://www.cdc.gov/handhygiene/campaign/provider-infographic-6.html (accessed on 27 August 2022).
- Baloh, J.; Thom, K.A.; Perencevich, E.; Rock, C.; Robinson, G.; Ward, M.; Herwaldt, L.; Reisinger, H.S. Hand hygiene before donning nonsterile gloves: Healthcare workers’ beliefs and practices. Am. J. Infect. Control 2019, 47, 492–497. [Google Scholar] [CrossRef]
- Wałaszek, M.; Kołpa, M.; Różańska, A.; Wolak, Z.; Bulanda, M.; Wójkowska-Mach, J. Practice of hand hygiene and use of protective gloves: Differences in the perception between patients and medical staff. Am. J. Infect. Control 2018, 46, 1074–1076. [Google Scholar] [CrossRef]
- Kurtz, S.L. Identification of low, high, and super gelers and barriers to hand hygiene among intensive care unit nurses. Am. J. Infect. Control 2017, 45, 839–843. [Google Scholar] [CrossRef] [PubMed]
- Boudjema, S.; Tarantini, C.; Peretti-Watel, P.; Brouqui, P. Merging video coaching and an anthropologic approach to understand health care provider behavior toward hand hygiene protocols. Am. J. Infect. Control 2017, 45, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Menon, V.; Shukla, U. Hand hygiene compliance among healthcare workers in an accredited tertiary care hospital. Indian J. Crit. Care Med. 2014, 18, 689–693. [Google Scholar] [CrossRef]
- Graveto, J.M.G.D.N.; Rebola, R.I.F.; Fernandes, E.A.; Costa, P.J.D.S. Hand hygiene: Nurses’ adherence after training. Rev. Bras. Enferm. 2018, 71, 1189–1193. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.L.; Sistrunk, W.W.; Higginbotham, M.A.; Burks, K.; Halford, L.; Goddard, L.; Thombs, L.A.; Austin, C.; Finley, P.J. Hospital hand hygiene compliance improves with increased monitoring and immediate feedback. Am. J. Infect. Control 2014, 42, 1074–1078. [Google Scholar] [CrossRef]
- Lehotsky, Á.; Szilágyi, L.; Ferenci, T.; Kovács, L.; Pethes, R.; Wéber, G.; Haidegger, T. Quantitative impact of direct, personal feedback on hand hygiene technique. J. Hosp. Infect. 2015, 91, 81–84. [Google Scholar] [CrossRef]
- Livshiz-Riven, I.; Azulay, H.; Koyfman, L.; Gushanski, A.; Askira, S.; Abar, V.I.; Gruenbaum, B.F.; Ivanov, E.; Klein, M.; Danziger, A.; et al. The long-term impact of immediate verbal feedback of hand hygiene compliance after overt observation sessions, as assessed by continuous closed-circuit television monitoring in an intensive care setting. Arch. Public Health 2021, 80, 141. [Google Scholar] [CrossRef]
- Deshommes, T.; Nagel, C.; Tucker, R.; Dorcélus, L.; Gautier, J.; Koster, M.P.; E Lechner, B. A Quality Improvement Initiative to Increase Hand Hygiene Awareness and Compliance in a Neonatal Intensive Care Unit in Haiti. J. Trop. Pediatr. 2020, 67, fmaa029. [Google Scholar] [CrossRef]
- Fouad, M.; Eltaher, S. Hand hygiene initiative: Comparative study of pre- and postintervention outcomes. East. Mediterr. Health J. 2020, 26, 198–205. [Google Scholar] [CrossRef]
- Sansam, S.; Yamamoto, E.; Srun, S.; Sinath, Y.; Moniborin, M.; Sim, K.B.; A Reyer, J.; Yoshida, Y.; Hamajima, N. Assessment of hand hygiene compliance after hand hygiene education among health care workers in Cambodia. Nagoya J. Med Sci. 2016, 78, 151–162. [Google Scholar]
- Higgins, A.; Hannan, M. Improved hand hygiene technique and compliance in healthcare workers using gaming technology. J. Hosp. Infect. 2013, 84, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Phan, H.T.; Tran, H.T.T.; Tran, H.T.M.; Dinh, A.P.P.; Ngo, H.T.; Theorell-Haglow, J.; Gordon, C.J. An educational intervention to improve hand hygiene compliance in Vietnam. BMC Infect. Dis. 2018, 18, 116. [Google Scholar] [CrossRef] [PubMed]
- Doron, S.I.; Kifuji, K.; Hynes, B.T.; Dunlop, D.; Lemon, T.; Hansjosten, K.; Cheng, T.; Curley, B.; Snydman, D.R.; Fairchild, D.G. A Multifaceted Approach to Education, Observation, and Feedback in a Successful Hand Hygiene Campaign. Jt. Comm. J. Qual. Patient Saf. 2011, 37, AP1–AP3. [Google Scholar] [CrossRef] [PubMed]
- Lydon, S.; Power, M.; McSharry, J.; Byrne, M.; Madden, C.; Squires, J.E.; O’connor, P. Interventions to Improve Hand Hygiene Compliance in the ICU: A Systematic Review. Crit. Care Med. 2017, 45, e1165–e1172. [Google Scholar] [CrossRef] [PubMed]
- Identifying Motivators for Hand Hygiene: External and Internal Factors. Available online: https://www.cdc.gov/infectioncontrol/pdf/strive/HH103-508.pdf (accessed on 8 August 2023).

| Opportunities for Hand Hygiene | Baseline Compliance | Compliance after 1st PDSA Cycle | Compliance after 2nd PDSA Cycle | Compliance after 3rd PDSA Cycle |
|---|---|---|---|---|
| 1—Before touching patient without gloves | 36/71 (50.7%) | 7/30 (56.66%) | 11/19 (57.89%) | 21/29 (72.4%) |
| 2—After touching patient without gloves | 18/33 (54.54%) | 22/33 (66.66%) | 13/25 (52.0%) | 21/27 (77.77%) |
| 3—Before a clean/aseptic procedure | 9/10 (90%) | 5/5 (100%) | N/A | N/A |
| 4—After touching patient’s body fluids | 8/10 (80%) | 4/4 (100%) | 2/3 (66.67%) | 3/3 (100%) |
| 5—After touching patient surroundings | 11/62 (17.74%) | 15/61 (24.59%) | 5/41 (12.19%) | 10/27 (37.03%) |
| 6—At entry into main unit | 15/71 (21.12%) | 19/59 (32.2%) | 15/49 (30.61%) | 38/79 (48.10%) |
| 7—At exit from main unit | 3/47 (6.38%) | 10/45 (22.22%) | 6/41 (14.63%) | 13/62 (20.96%) |
| 8—Before wearing gloves | 7/28 (25%) | 6/26 (23.07%) | 10/22 (45.45%) | 11/28 (39.28%) |
| 9—After removing gloves | 12/45 (26.66%) | 22/56 (39.28%) | 19/39 (48.71%) | 22/43 (51.16%) |
| Overall compliance | 119/377 (31.56%) | 120/319 (37.61%) | 81/239 (33.89%) | 139/298 (46.64%) |
| p-value * | - | 0.09 | 0.54 | <0.01 |
| Opportunities for Hand Hygiene | Baseline Compliance | Compliance after 3rd PDSA Cycle | p-Value |
|---|---|---|---|
| 1—Before touching patient without gloves | 36/71 (50.7%) | 21/29 (72.4%) | 0.04 |
| 2—After touching patient without gloves | 18/33 (54.54%) | 21/27 (77.77%) | 0.06 |
| 3—Before a clean/aseptic procedure | 9/10 (90%) | N/A | N/A |
| 4—After touching patient’s body fluids | 8/10 (80%) | 3/3 (100%) | 0.42 |
| 5—After touching patient surroundings | 11/62 (17.74%) | 10/27 (37.03%) | 0.05 |
| 6—At entry into main unit | 15/71 (21.12%) | 38/79 (48.10%) | <0.01 |
| 7—At exit from main unit | 3/47 (6.38%) | 13/62 (20.96%) | 0.03 |
| 8—Before wearing gloves | 7/28 (25%) | 11/28 (39.28%) | 0.25 |
| 9—After removing gloves | 12/45 (26.66%) | 22/43 (51.16%) | 0.02 |
| Overall compliance | 119/377 (31.56%) | 139/298 (46.64%) | <0.01 |
| Role of HCW | Baseline Compliance | Compliance after 1st PDSA Cycle | Compliance after 2nd PDSA Cycle | Compliance after 3rd PDSA Cycle | p-Value |
|---|---|---|---|---|---|
| Attending MD | 17/34 (50%) | 12/21 (57.1%) | 3/6 (50%) | 7/13 (53.8%) | 0.96 |
| 1st Year Resident | 15/40 (37.5%) | 8/21 (38%) | 4/10 (40%) | 24/34 (70.5%) | 0.02 |
| 2nd Year Resident | 14/46 (30.4%) | 11/33 (33.3%) | 8/16 (50%) | 10/16 (62.5%) | 0.09 |
| Neonatal Fellow | 10/39 (25.6%) | 6/16 (37.5%) | 3/7 (42.8%) | 8/20 (40%) | 0.6 |
| RN | 63/218 (28.8%) | 83/228 (36.4%) | 63/200 (31.5%) | 90/215 (41.8%) | 0.03 |
| p-value | 0.11 | 0.43 | 0.48 | 0.016 |
| Role of HCW | Baseline Compliance | Compliance after 3rd PDSA Cycle | p-Value |
|---|---|---|---|
| Attending MD | 17/34 (50%) | 7/13 (53.8%) | 0.82 |
| 1st Year Resident | 15/40 (37.5%) | 24/34 (70.5%) | <0.01 |
| 2nd Year Resident | 14/46 (30.4%) | 10/16 (62.5%) | 0.02 |
| Neonatal Fellow | 10/39 (25.6%) | 8/20 (40%) | 0.26 |
| RN | 63/218 (28.8%) | 90/215 (41.8%) | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chitamanni, P.; Allana, A.; Hand, I. Quality Improvement Project to Improve Hand Hygiene Compliance in a Level III Neonatal Intensive Care Unit. Children 2023, 10, 1484. https://doi.org/10.3390/children10091484
Chitamanni P, Allana A, Hand I. Quality Improvement Project to Improve Hand Hygiene Compliance in a Level III Neonatal Intensive Care Unit. Children. 2023; 10(9):1484. https://doi.org/10.3390/children10091484
Chicago/Turabian StyleChitamanni, Pavani, Ahreen Allana, and Ivan Hand. 2023. "Quality Improvement Project to Improve Hand Hygiene Compliance in a Level III Neonatal Intensive Care Unit" Children 10, no. 9: 1484. https://doi.org/10.3390/children10091484





