Goal Pursuit in Youth with Chronic Pain
Abstract
:1. Introduction and Purpose of Review
2. An Overview of Goals, Goal Achievement, and Goal Frustration
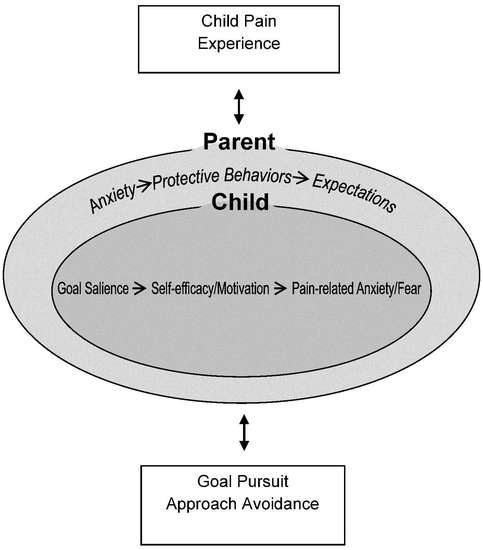
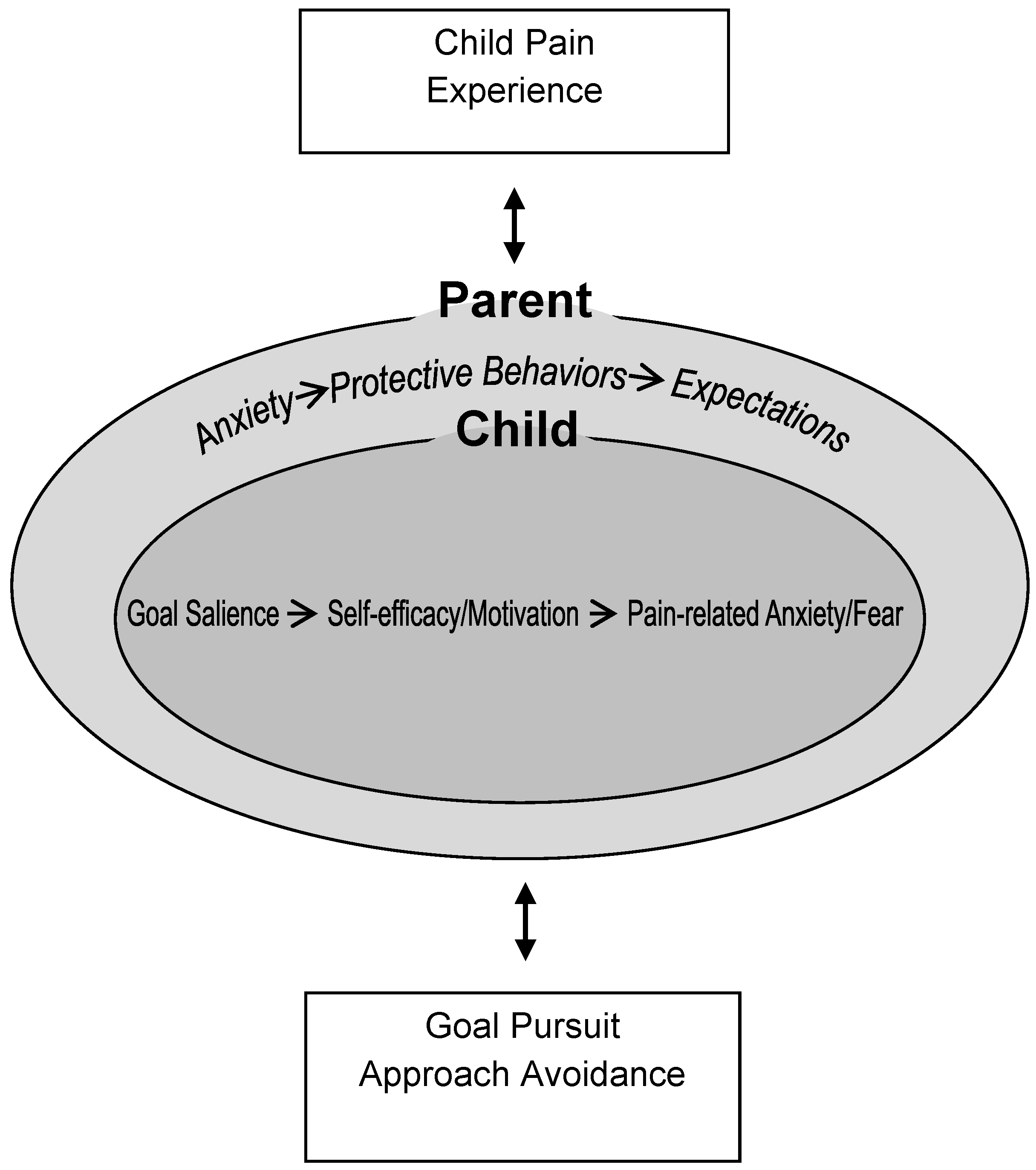
3. Description of a New Goal Pursuit Model for Pediatric Chronic Pain
3.1. Child’s Pain Experience
3.2. Child Factors
3.3. Parent Factors
3.4. Goal Pursuit
4. Future Directions
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef] [PubMed]
- Merskey, H.; Bogduk, N. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms; IASP Press: Seattle, WA, USA, 1994. [Google Scholar]
- Huguet, A.; Miró, J. The severity of chronic pediatric pain: An epidemiological study. J. Pain 2008, 9, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Dengler-Crish, C.M.; Rippel, S.; Bruehl, S. Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain 2010, 150, 568–572. [Google Scholar] [CrossRef] [PubMed]
- Kashikar-Zuck, S.; Cunningham, N.; Sil, S.; Bromberg, M.H.; Lynch-Jordan, A.M.; Strotman, D.; Peugh, J.; Noll, J.; Ting, T.V.; Powers, S.W.; et al. Long-term outcomes of adolescents with juvenile-onset fibromyalgia in early adulthood. Pediatrics 2014, 133, e592–e600. [Google Scholar] [CrossRef] [PubMed]
- Forgeron, P.A.; Evans, J.; McGrath, P.J.; Stevens, B.; Finley, G.A. Living with difference: Exploring the social self of adolescents with chronic pain. Pain Res. Manag. 2013, 18, e115–e123. [Google Scholar] [CrossRef] [PubMed]
- Gauntlett-Gilbert, J.; Eccleston, C. Disability in adolescents with chronic pain: Patterns and predictors across different domains of functioning. Pain 2007, 131, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Logan, D.E.; Simons, L.E.; Stein, M.J.; Chastain, L. School impairment in adolescents with chronic pain. J. Pain 2008, 9, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Kaczynski, K.J.; Simons, L.E.; Claar, R.L. Anxiety, coping, and disability: A test of mediation in a pediatric chronic pain sample. J. Pediatr. Psychol. 2011, 36, 932–941. [Google Scholar] [CrossRef] [PubMed]
- Cohen, L.L.; Vowles, K.E.; Eccleston, C. The impact of adolescent chronic pain on functioning: Disentangling the complex role of anxiety. J. Pain 2010, 11, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Kashikar-Zuck, S.; Parkins, I.S.; Graham, T.B.; Lynch, A.M.; Passo, M.; Johnston, M.; Schikler, K.N.; Hashkes, P.J.; Banez, G.; Richards, M.M. Anxiety, mood, and behavioral disorders among pediatric patients with juvenile fibromyalgia syndrome. Clin. J. Pain 2008, 24, 620–626. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Smith, C.A.; Garber, J.; Claar, R.L. Appraisal and coping with daily stressors by pediatric patients with chronic abdominal pain. J. Pediatr. Psychol. 2007, 32, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Simons, L.E.; Kaczynski, K.J. The fear avoidance model of chronic pain: Examination for pediatric application. J. Pain 2012, 13, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.S.; Linton, S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000, 85, 317–332. [Google Scholar] [CrossRef]
- Caes, L.; Fisher, E.; Clinch, J.; Tobias, J.H.; Eccleston, C. The role of pain-related anxiety in adolescents’ disability and social impairment: Alspac data. Eur. J. Pain 2015, 19, 842–851. [Google Scholar] [CrossRef] [PubMed]
- Perquin, C.W.; Hazebroek-Kampschreur, A.A.J.M.; Hunfeld, J.A.; Bohnen, A.M.; van Suijlekom-Smit, L.W.A.; Passchier, J.; van der Wouden, J.C. Pain in children and adolescents: A common experience. Pain 2000, 87, 51–58. [Google Scholar] [CrossRef]
- Austin, J.T.; Vancouver, J.B. Goal constructs in psychology: Structure, process, and content. Psychol. Bull. 1996, 120, 338–375. [Google Scholar] [CrossRef]
- Wrosch, C.; Miller, G.E.; Scheier, M.F.; De Pontet, S.B. Giving up on unattainable goals: Benefits for health? Personal. Soc. Psychol. Bull. 2007, 33, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Massey, E.K.; Garnefski, N.; Gebhardt, W.A. Goal frustration, coping and well-being in the context of adolescent headache: A self-regulation approach. Eur. J. Pain 2009, 13, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Stommen, N.C.; Verbunt, J.A.; Goossens, M.E. Future goals of adolescents and young adults with chronic musculoskeletal pain. Eur. J. Pain 2016, 20, 564–572. [Google Scholar] [CrossRef] [PubMed]
- Fisher, E.; Keogh, E.; Eccleston, C. Adolescents’ approach-avoidance behaviour in the context of pain. Pain 2016, 157, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; Valrie, C.R.; Karlson, C.W. Family and parent influences on pediatric chronic pain: A developmental perspective. Am. Psychol. 2014, 69, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; Chambers, C.T. Parent and family factors in pediatric chronic pain and disability: An integrative approach. Pain 2005, 119, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.L.; Eccleston, C.; Osborn, M. Being a parent of the adolescent with complex chronic pain: An interpretative phenomenological analysis. Eur. J. Pain 2007, 11, 49. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Williams, S.E.; Smith, C.A.; Garber, J.; Van Slyke, D.A.; Lipani, T.A. Parent attention versus distraction: Impact on symptom complaints by children with and without chronic functional abdominal pain. Pain 2006, 122, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Caes, L.; Vervoort, T.; Eccleston, C.; Vandenhende, M.; Goubert, L. Parental catastrophizing about child’s pain and its relationship with activity restriction: The mediating role of parental distress. Pain 2011, 152, 212–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claar, R.L.; Simons, L.E.; Logan, D.E. Parental response to children’s pain: The moderating impact of children’s emotional distress on symptoms and disability. Pain 2008, 138, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Grey, M.; Davidson, M.; Boland, E.A.; Tamborlane, W.V. Clinical and psychosocial factors associated with achievement of treatment goals in adolescents with diabetes mellitus. J. Adolesc. Health 2001, 28, 377–385. [Google Scholar] [CrossRef]
- Fisher, E.; Bromberg, M.; Tai, G.; Palermo, T.M. Adolescent and parent treatment goals in an internet delivered chronic pain self-management program: Does agreement of treatment goals matter? J. Pediatr. Psychol. 2016, in press. [Google Scholar]
- Karoly, P.; Ruehlman, L.S. Psychosocial aspects of pain-related life task interference: An exploratory analysis in a general population sample. Pain Med. 2007, 8, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Karoly, P.; Okun, M.A.; Ruehlman, L.S.; Pugliese, J.A. The impact of goal cognition and pain severity on disability and depression in adults with chronic pain: An examination of direct effects and mediated effects via pain-induced fear. Cogn. Ther. Res. 2008, 32, 418–433. [Google Scholar] [CrossRef]
- Eccleston, C.; Crombez, G. Worry and chronic pain: A misdirected problem solving model. Pain 2007, 132, 233–236. [Google Scholar] [CrossRef] [PubMed]
- Crombez, G.; Eccleston, C.; Van Damme, S.; Vlaeyen, J.W.S.; Karoly, P. Fear-avoidance model of chronic pain: The next generation. Clin. J. Pain 2012, 28, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, S.; Crombez, G.; Eccleston, C. Coping with pain: A motivational perspective. Pain 2008, 139, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, S.; Kindermans, H. A self-regulation perspective on avoidance and persistence behavior in chronic pain: New theories, new challenges? Clin. J. Pain 2015, 31, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.S.; Crombez, G.; Linton, S.J. The fear-avoidance model of pain. Pain 2016, 157, 1588–1589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schrooten, M.G.S.; Wiech, K.; Vlaeyen, J.W.S. When pain meets… Pain-related choice behavior and pain perception in different goal conflict situations. J. Pain 2014, 15, 1166–1178. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, S.; Van Ryckeghem, D.M.; Wyffels, F.; Van Hulle, L.; Crombez, G. No pain no gain? Pursuing a competing goal inhibits avoidance behavior. Pain 2012, 153, 800–804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maes, S.; Karoly, P. Self-regulation assessment and intervention in physical health and illness: A review. Appl. Psychol. 2005, 54, 267–299. [Google Scholar] [CrossRef]
- Schwarzer, R.; Lippke, S.; Luszczynska, A. Mechanisms of health behavior change in persons with chronic illness or disability: The health action process approach (HAPA). Rehabil. Psychol. 2011, 56, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Fisher, E.; Caes, L.; Clinch, J.; Tobias, J.H.; Eccleston, C. Anxiety at 13 and its effect on pain, pain-related anxiety, and pain-related disability at 17: An ALSPAC cohort longitudinal analysis. Psychol. Health Med. 2016, 21, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jackson, T.; Wang, Y.; Wang, Y.; Fan, H. Self-efficacy and chronic pain outcomes: A meta-analytic review. J. Pain 2014, 15, 800–814. [Google Scholar] [CrossRef] [PubMed]
- Carpino, E.; Segal, S.; Logan, D.; Lebel, A.; Simons, L.E. The interplay of pain-related self-efficacy and fear on functional outcomes among youth with headache. J. Pain 2014, 15, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Kalapurakkel, S.; Carpino, E.A.; Lebel, A.; Simons, L.E. “Pain can’t stop me”: Examining pain self-efficacy and acceptance as resilience processes among youth with chronic headache. J. Pediatr. Psychol. 2015, 40, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Tran, S.T.; Jastrowski Mano, K.E.; Hainsworth, K.R.; Medrano, G.R.; Anderson Khan, K.; Weisman, S.J.; Davies, W.H. Distinct influences of anxiety and pain catastrophizing on functional outcomes in children and adolescents with chronic pain. J. Pediatr. Psychol. 2015, 40, 744–755. [Google Scholar] [CrossRef] [PubMed]
- Vervoort, T.; Eccleston, C.; Goubert, L.; Buysse, A.; Crombez, G. Children’s catastrophic thinking about their pain predicts pain and disability 6 months later. Eur. J. Pain 2010, 14, 90–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vervoort, T.; Goubert, L.; Eccleston, C.; Bijttebier, P.; Crombez, G. Catastrophic thinking about pain is independently associated with pain severity, disability, and somatic complaints in school children and children with chronic pain. J. Pediatr. Psychol. 2006, 31, 674–683. [Google Scholar] [CrossRef] [PubMed]
- Caes, L.; Vervoort, T.; Devos, P.; Verlooy, J.; Benoit, Y.; Goubert, L. Parental distress and catastrophic thoughts about child pain: Implications for parental protective behavior in the context of child leukemia-related medical procedures. Clin. J. Pain 2014, 30, 787–799. [Google Scholar] [CrossRef] [PubMed]
- Sieberg, C.B.; Williams, S.; Simons, L.E. Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? J. Pediatr. Psychol. 2011, 36, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Guite, J.W.; McCue, R.L.; Sherker, J.L.; Sherry, D.D.; Rose, J.B. Relationships among pain, protective parental responses, and disability for adolescents with chronic musculoskeletal pain: The mediating role of pain catastrophizing. Clin. J. Pain 2011, 27, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, N.R.; Lynch-Jordan, A.; Barnett, K.; Peugh, J.; Sil, S.; Goldschneider, K.; Kashikar-Zuck, S. Child pain catastrophizing mediates the relation between parent responses to pain and disability in youth with functional abdominal pain. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Lipani, T.A.; Walker, L.S. Children’s appraisal and coping with pain: Relation to maternal ratings of worry and restriction in family activities. J. Pediatr. Psychol. 2006, 31, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Hasenbring, M.I.; Hallner, D.; Klasen, B.; Streitlein-Bohme, I.; Willburger, R.; Rusche, H. Pain-related avoidance versus endurance in primary care patients with subacute back pain: Psychological characteristics and outcome at a 6-month follow-up. Pain 2012, 153, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Claes, N.; Crombez, G.; Vlaeyen, J.W.S. Pain-avoidance versus reward-seeking: An experimental investigation. Pain 2015, 156, 1449–1457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- James, A.C.; James, G.; Cowdrey, F.A.; Soler, A.; Choke, A. Cognitive behavioural therapy for anxiety disorders in children and adolescents. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2015. [Google Scholar]
- Palermo, T.M.; Law, E.F.; Fales, J.; Bromberg, M.H.; Jessen-Fiddick, T.; Tai, G. Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: A randomized controlled multicenter trial. Pain 2016, 157, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; Law, E.F.; Essner, B.; Jessen-Fiddick, T.; Eccleston, C. Adaptation of problem-solving skills training (PSST) for parent caregivers of youth with chronic pain. Clin. Pract. Pediatr. Psychol. 2014, 2, 212–223. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fisher, E.; Palermo, T.M. Goal Pursuit in Youth with Chronic Pain. Children 2016, 3, 36. https://doi.org/10.3390/children3040036
Fisher E, Palermo TM. Goal Pursuit in Youth with Chronic Pain. Children. 2016; 3(4):36. https://doi.org/10.3390/children3040036
Chicago/Turabian StyleFisher, Emma, and Tonya M. Palermo. 2016. "Goal Pursuit in Youth with Chronic Pain" Children 3, no. 4: 36. https://doi.org/10.3390/children3040036