A Case of Spontaneous Pneumomediastinum with Subcutaneous Emphysema in Children
Abstract
:1. Introduction
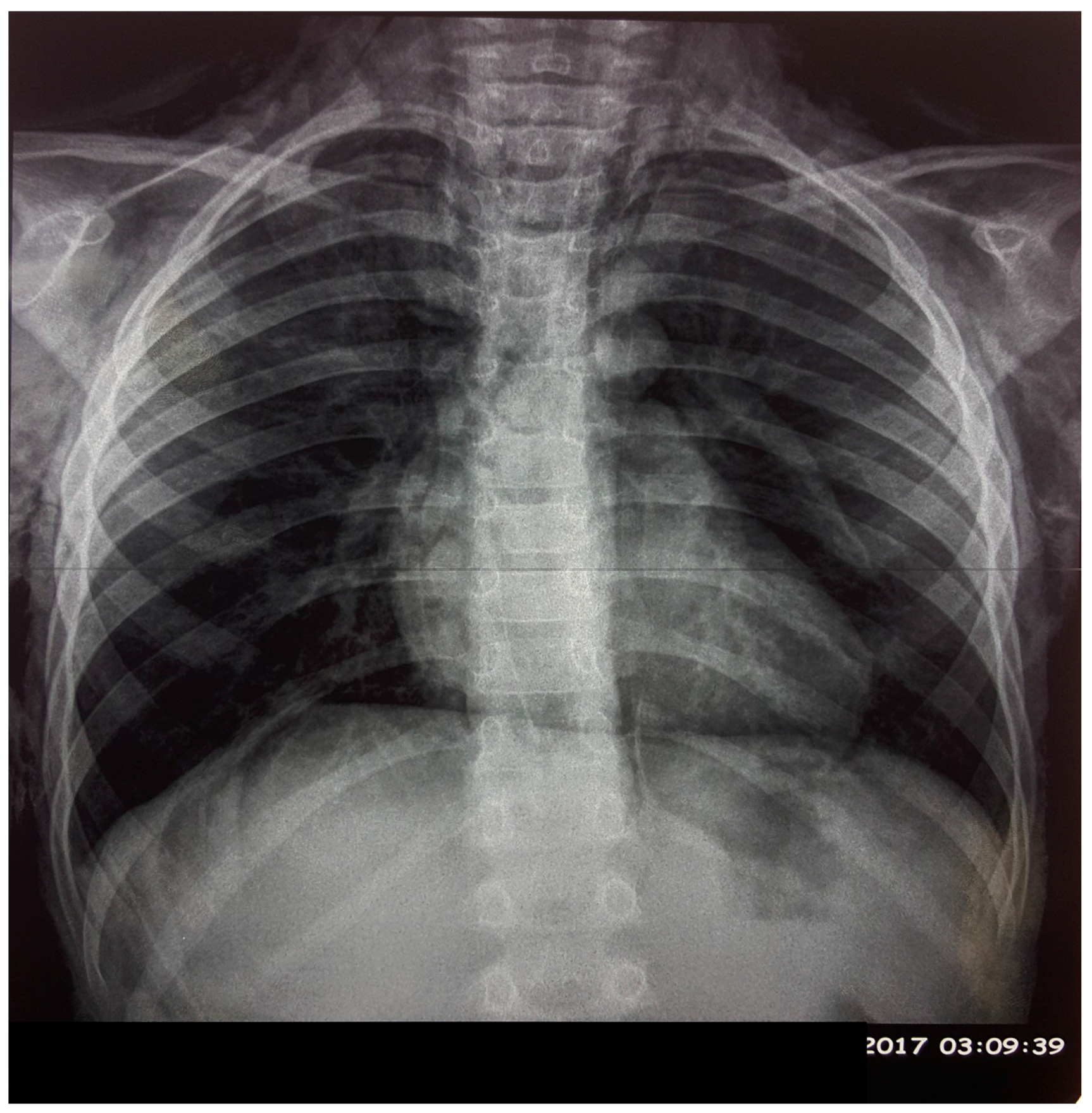
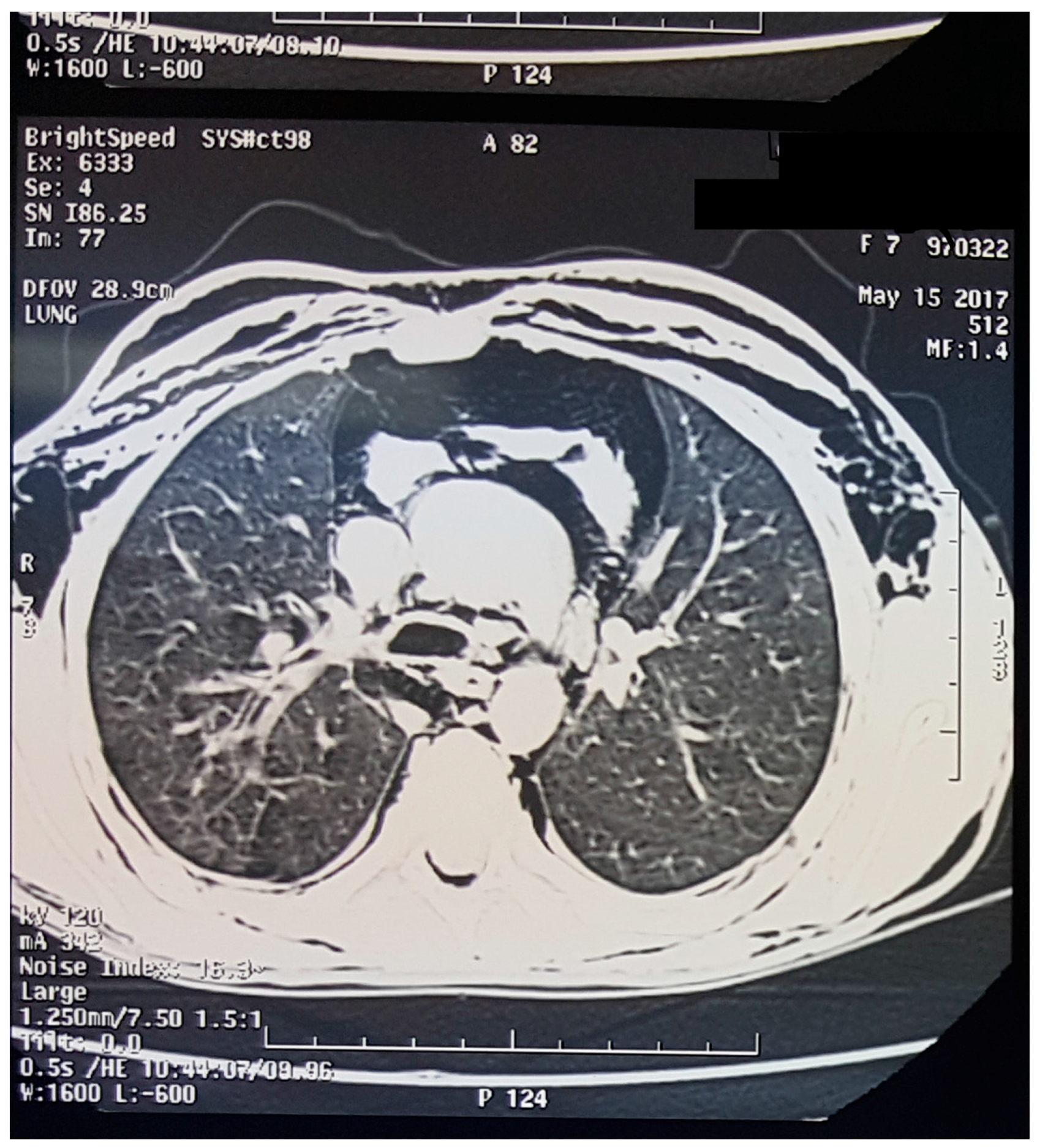
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Conflicts of Interest
References
- Kelly, S.; Hughes, S.; Nixon, S.; Paterson-Brown, S. Spontaneous pneumomediastinum (Hamman’s syndrome). Surgeon 2010, 8, 63–66. [Google Scholar] [CrossRef] [PubMed]
- McMahon, D. Spontaneous pneumomediastinum. Am. J. Surg. 1976, 131, 550–551. [Google Scholar] [CrossRef]
- Fitzwater, J.; Silva, N.; Knight, C.; Malvezzi, L.; Ramos-Irizarry, C.; Burnweit, C. Management of spontaneous pneumomediastinum in children. J. Pediatr. Surg. 2015, 50, 983–986. [Google Scholar] [CrossRef] [PubMed]
- Iyer, V.N.; Joshi, A.Y.; Ryu, J.H. Spontaneous pneumomediastinum: Analysis of 62 consecutive adult patients. Mayo Clin. Proc. 2009, 84, 417–421. [Google Scholar] [CrossRef]
- Al-Mufarrej, F.; Badar, J.; Gharagozloo, F.; Tempesta, B.; Strother, E.; Margolis, M. Spontaneous pneumomediastinum: Diagnostic and therapeutic interventions. J. Cardiothorac. Surg. 2008, 3, 59. [Google Scholar] [CrossRef] [PubMed]
- Caceres, M.; Ali, S.Z.; Braud, R.; Weiman, D.; Garrett, H.E., Jr. Spontaneous pneumomediastinum: A comparative study and review of the literature. Ann. Thorac. Surg. 2008, 86, 962–966. [Google Scholar] [CrossRef] [PubMed]
- Takada, K.; Matsumoto, S.; Hiramatsu, T.; Kojima, E.; Watanabe, H.; Sizu, M.; Okachi, S.; Ninomiya, K. Management of spontaneous pneumomediastinum based on clinical experience of 25 cases. Respir. Med. 2008, 102, 1329–1334. [Google Scholar] [CrossRef] [PubMed]
- Macia, I.; Moya, J.; Ramos, R.; Morera, R.; Escobar, I.; Saumench, J.; Perna, V.; Rivas, F. Spontaneous pneumomediastinum: 41 cases. Eur. J. Cardiothorac. Surg. 2007, 31, 1110–1114. [Google Scholar] [CrossRef] [PubMed]
- Mondello, B.; Pavia, R.; Ruggeri, P.; Barone, M.; Barresi, P.; Monaco, M. Spontaneous pneumomediastinum: Experience in 18 adult patients. Lung 2007, 185, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Newcomb, A.E.; Clarke, C.P. Spontaneous pneumomediastinum: A benign curiosity or a significant problem? Chest 2005, 128, 3298–3302. [Google Scholar] [CrossRef] [PubMed]
- Freixinet, J.; García, F.; Rodríguez, P.M.; Santana, N.B.; Quintero, C.O.; Hussein, M. Spontaneous pneumomediastinum long-term follow-up. Respir. Med. 2005, 99, 1160–1163. [Google Scholar] [CrossRef] [PubMed]
- Koullias, G.J.; Korkolis, D.P.; Wang, X.J.; Hammond, G.L. Current assessment and management of spontaneous pneumomediastinum: Experience in 24 adult patients. Eur. J. Cardiothorac. Surg. 2004, 25, 852–855. [Google Scholar] [CrossRef] [PubMed]
- Jougon, J.B.; Ballester, M.; Delcambre, F.; Mac Bride, T.; Dromer, C.E.; Velly, J.F. Assessment of spontaneous pneumomediastinum: Experience with 12 patients. Ann. Thorac. Surg. 2003, 75, 1711–1714. [Google Scholar] [CrossRef]
- Miura, H.; Taira, O.; Hiraguri, S.; Ohtani, K.; Kato, H. Clinical features of medical pneumomediastinum. Ann. Thorac. Cardiovasc. Surg. 2003, 9, 188–191. [Google Scholar] [PubMed]
- Gerazounis, M.; Athanassiadi, K.; Kalantzi, N.; Moustardas, M. Spontaneous pneumomediastinum: A rare benign entity. J. Thorac. Cardiovasc. Surg. 2003, 126, 774–776. [Google Scholar] [CrossRef]
- Kaneki, T.; Kubo, K.; Kawashima, A.; Koizumi, T.; Sekiguchi, M.; Sone, S. Spontaneous pneumomediastinum in 33 patients: Yield of chest computed tomography for the diagnosis of the mild type. Respiration 2000, 67, 408–411. [Google Scholar] [CrossRef] [PubMed]
- Panacek, E.A.; Singer, A.J.; Sherman, B.W.; Prescott, A.; Rutherford, W.F. Spontaneous pneumomediastinum: Clinical and natural history. Ann. Emerg. Med. 1992, 21, 1222–1227. [Google Scholar] [CrossRef]
- Lee, C.Y.; Wu, C.C.; Lin, C.Y. Etiologies of spontaneous pneumomediastinum in children of different ages. Pediatr. Neonatol. 2009, 50, 190–195. [Google Scholar] [CrossRef]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benlamkaddem, S.; Berdai, M.A.; Labib, S.; Harandou, M. A Case of Spontaneous Pneumomediastinum with Subcutaneous Emphysema in Children. Children 2018, 5, 22. https://doi.org/10.3390/children5020022
Benlamkaddem S, Berdai MA, Labib S, Harandou M. A Case of Spontaneous Pneumomediastinum with Subcutaneous Emphysema in Children. Children. 2018; 5(2):22. https://doi.org/10.3390/children5020022
Chicago/Turabian StyleBenlamkaddem, Said, Mohamed Adnane Berdai, Smael Labib, and Mustapha Harandou. 2018. "A Case of Spontaneous Pneumomediastinum with Subcutaneous Emphysema in Children" Children 5, no. 2: 22. https://doi.org/10.3390/children5020022
APA StyleBenlamkaddem, S., Berdai, M. A., Labib, S., & Harandou, M. (2018). A Case of Spontaneous Pneumomediastinum with Subcutaneous Emphysema in Children. Children, 5(2), 22. https://doi.org/10.3390/children5020022




