Novel 3D Printed Resin Crowns for Primary Molars: In Vitro Study of Fracture Resistance, Biaxial Flexural Strength, and Dynamic Mechanical Analysis
Abstract
:1. Introduction
2. Materials and Methods
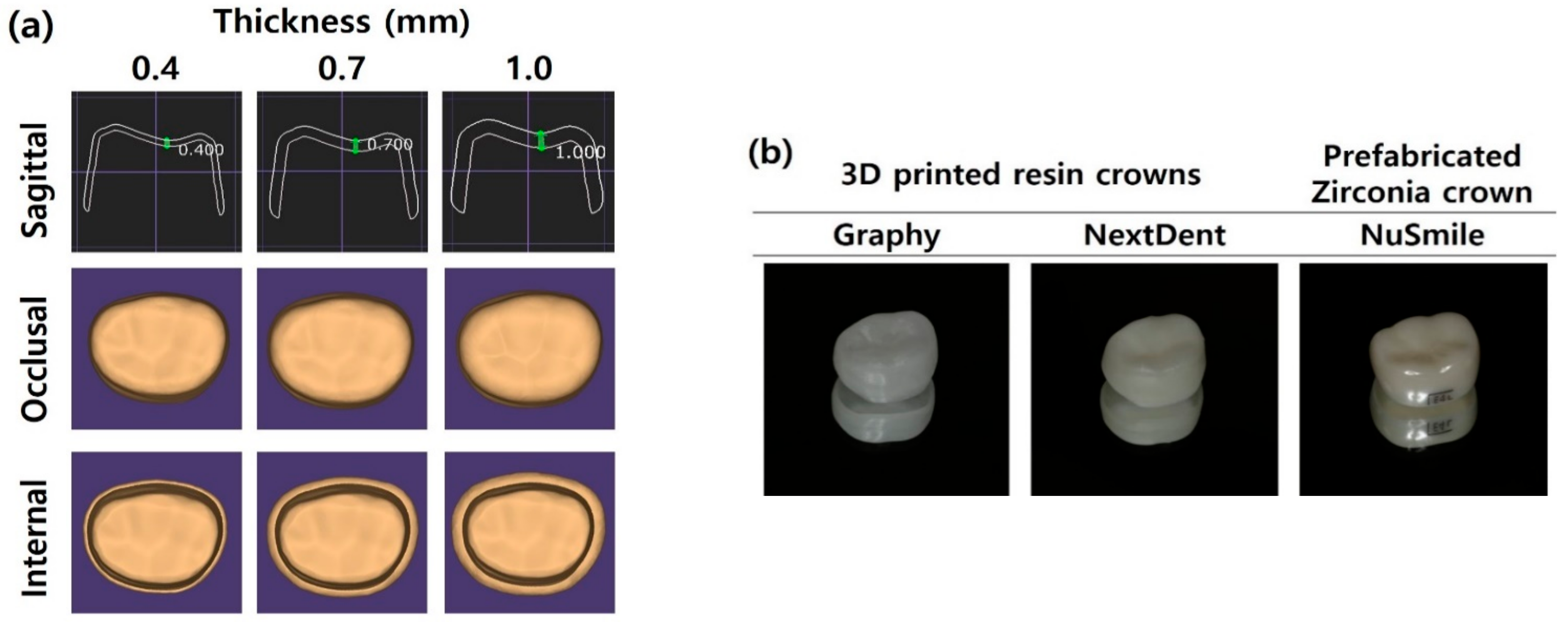
2.1. Fracture Resistance
2.1.1. Metal Die and Specimen Preparation
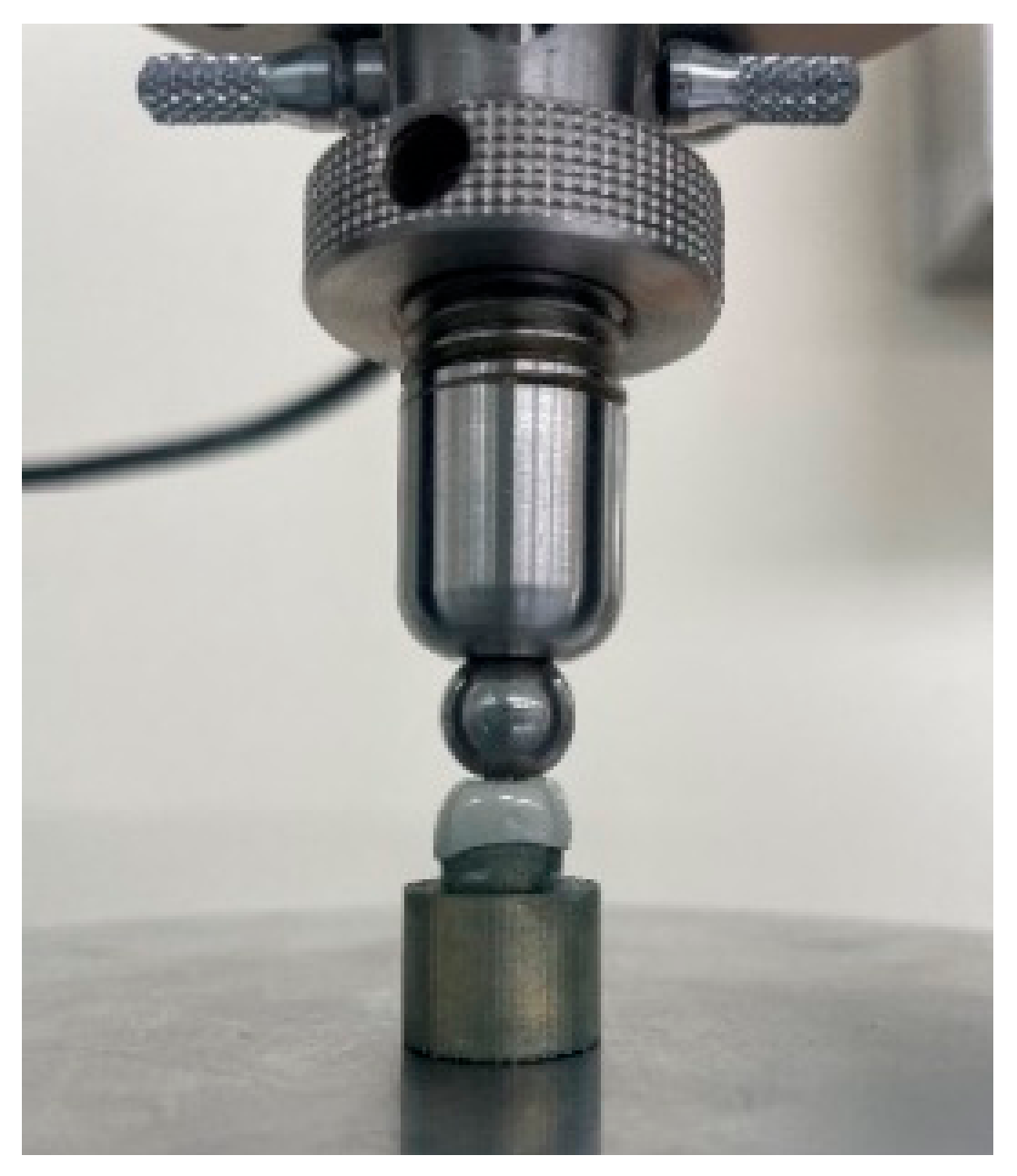
2.1.2. Fracture Resistance Measurements
2.2. Biaxial Flexural Strength (BFS)
2.2.1. Three-Dimensional Printed Resin Disc Preparation
2.2.2. Biaxial Flexural Strength Measurements
2.3. Dynamic Mechanical Analysis (DMA)
2.4. Statistical Analyses
3. Results
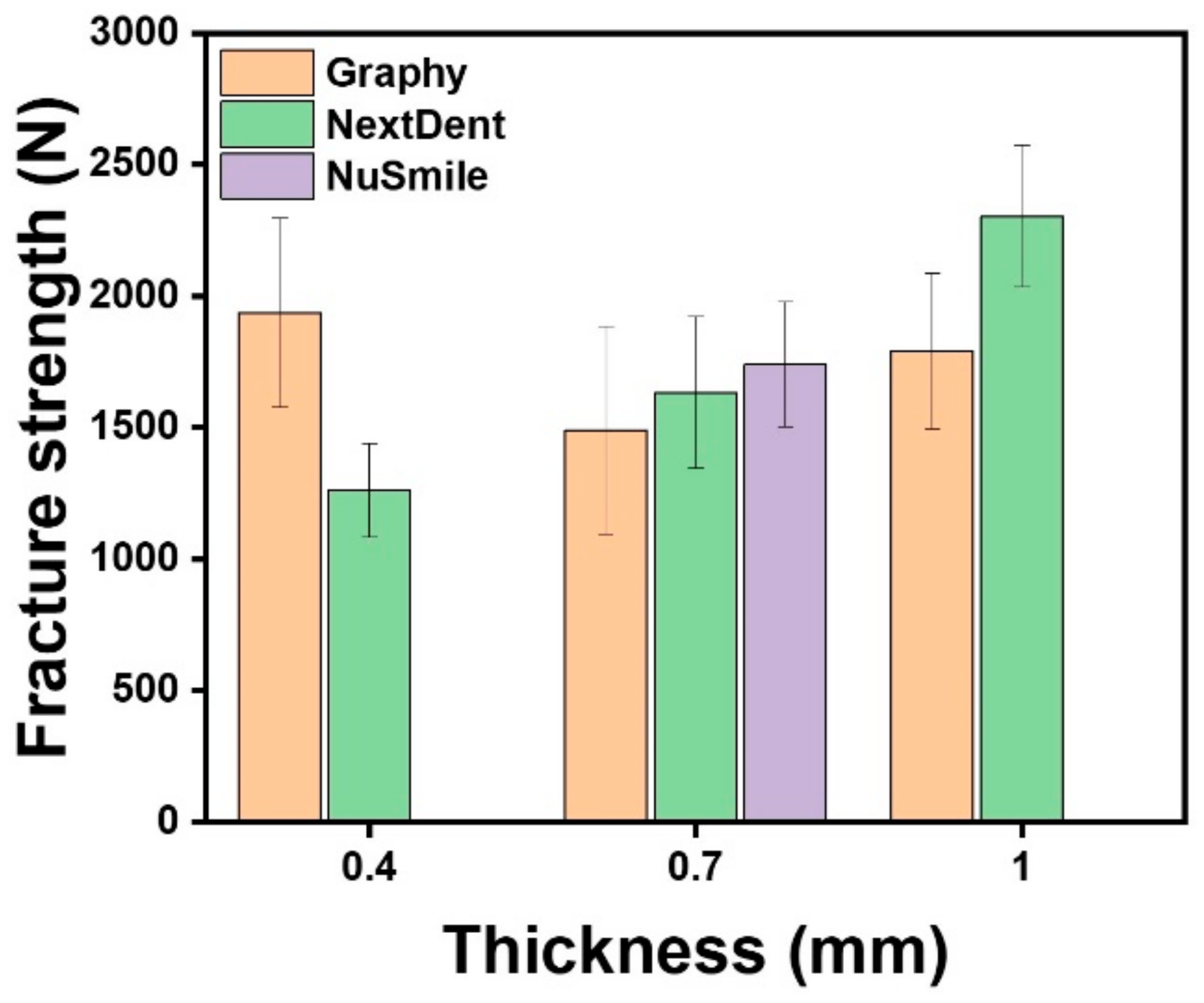
3.1. Fracture Resistance
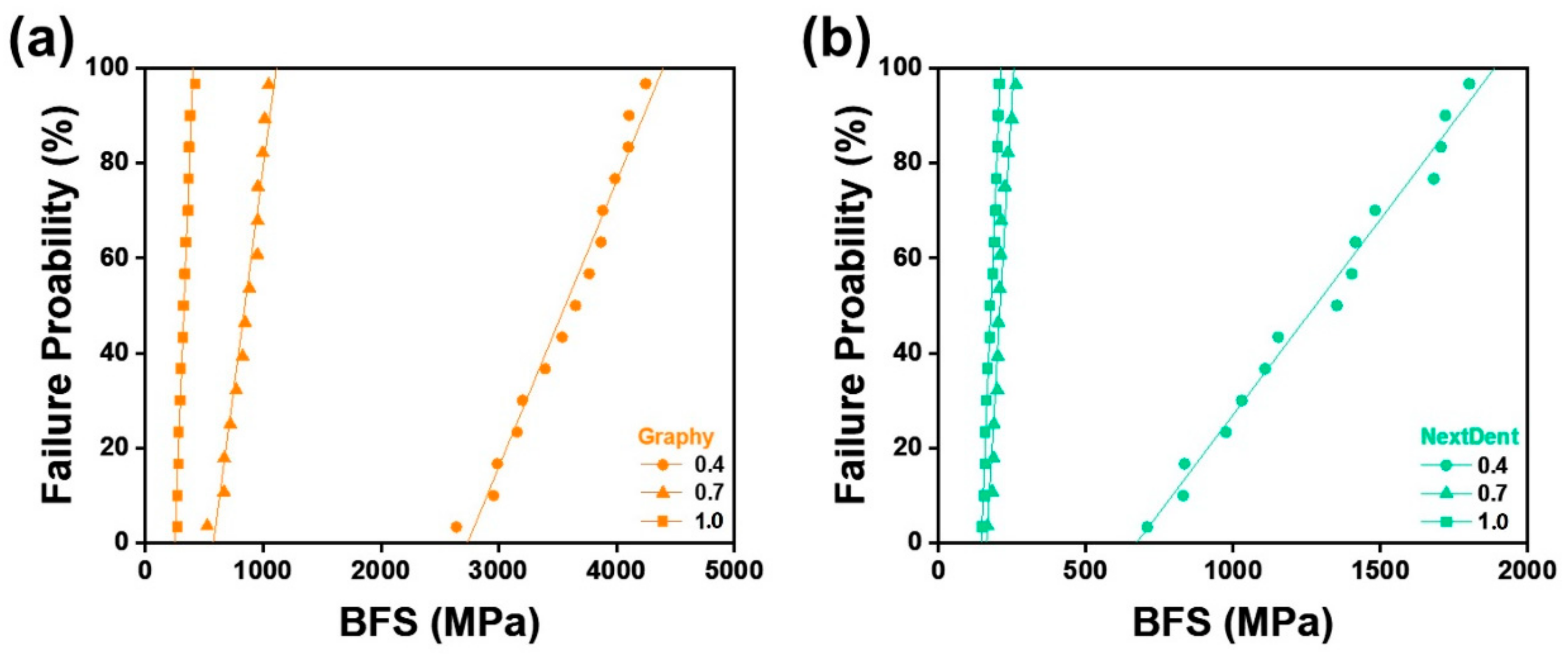
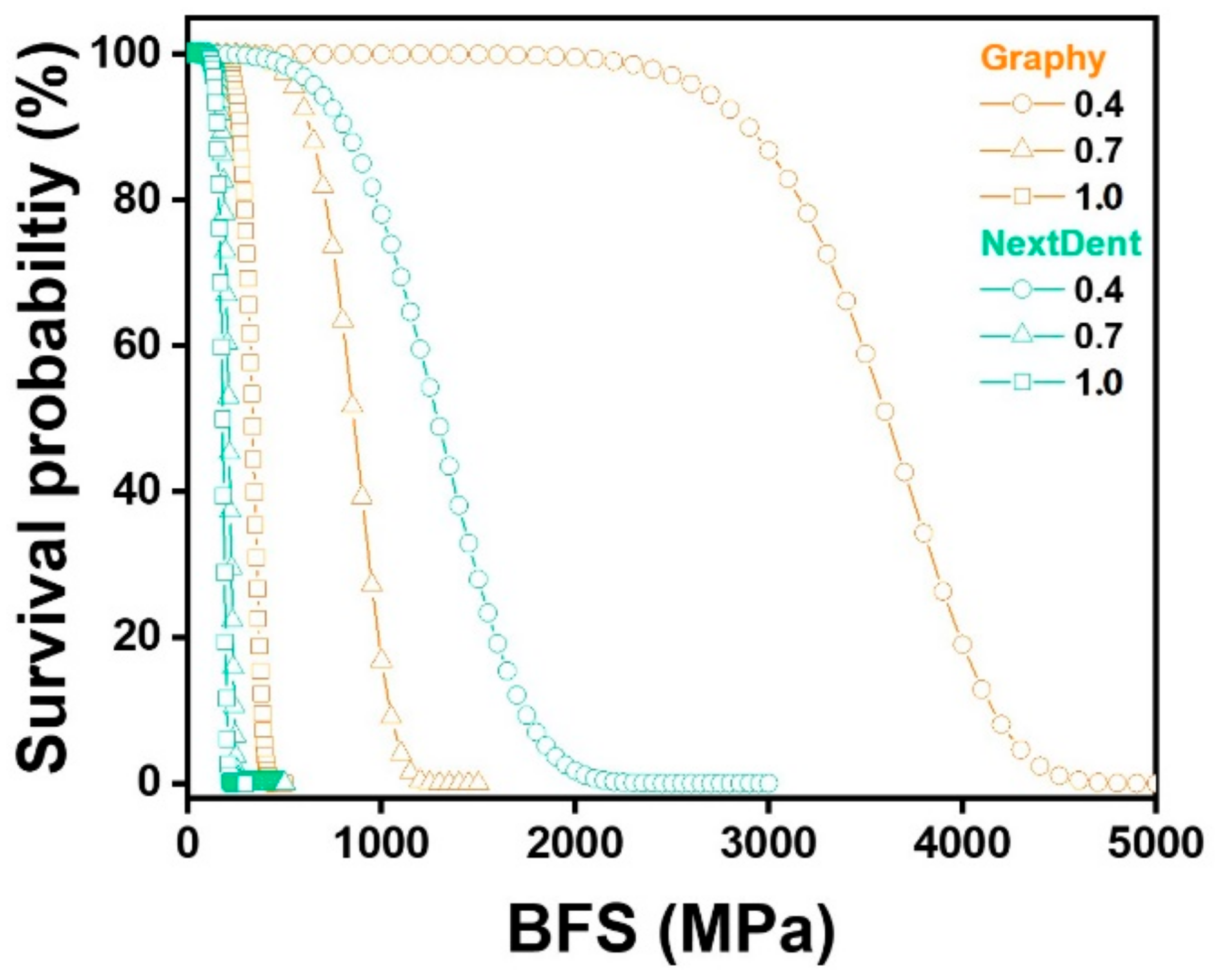
3.2. Biaxial Flexural Strength (BFS)
3.3. Dynamic Mechanical Analysis (DMA)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kapur, A.; Chawla, H.; Goyal, A.; Gaube, K. An esthetic point of view in very young children. J. Clin. Pediatr. Dent. 2005, 30, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Pani, S.C.; Saffan, A.A.; AlHobail, S.; Bin Salem, F.; AlFuraih, A.; AlTamimi, M. Esthetic concerns and acceptability of treatment modalities in primary teeth: A comparison between children and their parents. Int. J. Dent. 2016, 2016, 3163904. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.; Lee, J.; Wright, J. Clinical evaluation of and parental satisfaction with resin-faced stainless steel crowns. Pediatr. Dent. 2001, 23, 28–31. [Google Scholar] [PubMed]
- Yanover, L.; Waggoner, W.; Kupietzky, A.; Moskovitz, M.; Tickotsky, N. Parental and dentist satisfaction with primary anterior zirconia crowns: A case series analysis. Children 2021, 8, 451. [Google Scholar] [CrossRef]
- Mathew, M.G.; Roopa, K.B.; Soni, A.J.; Khan, M.M.; Kauser, A. Evaluation of clinical success, parental and child satisfaction of stainless steel crowns and zirconia crowns in primary molars. J. Family Med. Prim. Care 2020, 9, 1418. [Google Scholar] [CrossRef]
- Morley, J. The role of cosmetic dentistry in restoring a youthful appearance. J. Am. Dent. Assoc. 1999, 130, 1166–1172. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Pediatric Restorative Dentistry. Available online: https://www.aapd.org/globalassets/media/policies_guidelines/bp_restorativedent.pdf (accessed on 24 August 2022).
- Randall, R.C. Preformed metal crowns for primary and permanent molar teeth: Review of the literature. Pediatr. Dent. 2002, 24, 489–500. [Google Scholar]
- Mittal, G.K.; Verma, A.; Pahuja, H.; Agarwal, S.; Tomar, H. Esthetic crowns in pediatric dentistry: A review. Int. J. Contemp. Med. Res. 2016, 3, 1280–1282. [Google Scholar]
- Yilmaz, Y.; Gurbuz, T.; Eyuboglu, O.; Belduz, N. The repair of preveneered posterior stainless steel crowns. Pediatr. Dent. 2008, 30, 429–435. [Google Scholar] [CrossRef]
- Ajayakumar, L.P.; Chowdhary, N.; Reddy, V.R.; Chowdhary, R. Use of restorative full crowns made with zirconia in children: A systematic review. Int. J. Clin. Pediatr. Dent. 2020, 13, 551. [Google Scholar]
- Aiem, E.; Smaïl-Faugeron, V.; Muller-Bolla, M. Aesthetic preformed paediatric crowns: Systematic review. Int. J. Paediatr. Dent. 2017, 27, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Walia, T.; Salami, A.; Bashiri, R.; Hamoodi, O.; Rashid, F. A randomised controlled trial of three aesthetic full-coronal restorations in primary maxillary teeth. Eur. J. Paediatr. Dent. 2014, 15, 113–118. [Google Scholar] [PubMed]
- Park, S.-M.; Park, J.-M.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y. Flexural strength of 3d-printing resin materials for provisional fixed dental prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef] [PubMed]
- Anadioti, E.; Kane, B.; Soulas, E. Current and emerging applications of 3d printing in restorative dentistry. Curr. Oral. Health Rep. 2018, 5, 133–139. [Google Scholar] [CrossRef]
- Al-Halabi, M.N.; Bshara, N.; Comisi, J.C.; Abou Nassar, J. Evaluation of fracture resistance force in three types of primary molar crowns: Milled by cad\cam, 3d dental printed, and composite celluloid crowns. Eur. Dent. Res. Biomater. J. 2020, 1, 33–39. [Google Scholar] [CrossRef]
- Al-Halabi, M.N.; Bshara, N.; Abou Nassar, J.; Comisi, J.C.; Alawa, L. Comparative assessment of novel 3d printed resin crowns versus direct celluloid crowns in restoring pulp treated primary molars. J. Evid. Based Dent. Pract. 2022, 22, 101664. [Google Scholar] [CrossRef]
- Aati, S.; Akram, Z.; Ngo, H.; Fawzy, A.S. Development of 3d printed resin reinforced with modified zro2 nanoparticles for long-term provisional dental restorations. Dent. Mater. 2021, 37, e360–e374. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3d printing in digital prosthetic dentistry: An overview of recent developments in additive manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef]
- Nikzad, M.; Masood, S.H.; Sbarski, I. Thermo-mechanical properties of a highly filled polymeric composites for fused deposition modeling. Mater. Des. 2011, 32, 3448–3456. [Google Scholar] [CrossRef]
- Zhou, B.; Liu, Y.J.; Leng, J.S.; Li, T. Study on Thermo-Mechanical Behaviors of Shape Memory Polymer. Key Eng. Mater. 2009, 419–420, 497–500. [Google Scholar] [CrossRef]
- Lee, H.-J.; Park, H.-Y.; Kim, E.-H.; Choi, H.-H.; Jin, J.; Choi, J.; Yang, S.; Jung, Y.-G. Relationship between mechanical properties of ceramic green body and structures of photo-cured acrylate polymer for ceramic 3d printing based on photo polymerization. Ceram. Int. 2021, 47, 3867–3875. [Google Scholar] [CrossRef]
- ISO Standard No. 10477; Dentistry—Polymer-based crown and veneering materials. International Organization for Standardization: Geneva, Switzerland, 2020.
- Alrashdi, M.; Ardoin, J.; Liu, J.A. Zirconia crowns for children: A systematic review. Int. J. Paediatr. Dent. 2022, 32, 66–81. [Google Scholar] [CrossRef] [PubMed]
- Braun, S.; Hnat, W.P.; Freudenthaler, J.W.; Marcotte, M.R.; Hönigle, K.; Johnson, B.E. A study of maximum bite force during growth and development. Angle Orthod. 1996, 66, 261–264. [Google Scholar] [PubMed]
- Owais, A.I.; Shaweesh, M.; Abu Alhaija, E.S. Maximum occusal bite force for children in different dentition stages. Eur. J. Orthod. 2013, 35, 427–433. [Google Scholar] [CrossRef]
- Chong, M.X.; Khoo, C.D.; Goh, K.H.; Rahman, F.; Shoji, Y. Effect of age on bite force. J. Oral. Sci. 2016, 58, 361–363. [Google Scholar] [CrossRef]
- Abushanan, A.; Sharanesha, R.B.; Aljuaid, B.; Alfaifi, T.; Aldurayhim, A. Fracture resistance of primary zirconia crowns: An in vitro study. Children 2022, 9, 77. [Google Scholar] [CrossRef]
- Kist, S.; Stawarczyk, B.; Kollmuss, M.; Hickel, R.; Huth, K.C. Fracture load and chewing simulation of zirconia and stainless-steel crowns for primary molars. Eur. J. Oral Sci. 2019, 127, 369–375. [Google Scholar] [CrossRef]
- Souza, R.O.; Valandro, L.F.; Melo, R.M.; Machado, J.P.; Bottino, M.A.; Özcan, M. Air–particle abrasion on zirconia ceramic using different protocols: Effects on biaxial flexural strength after cyclic loading, phase transformation and surface topography. J. Mech Behav. Biomed. Mater. 2013, 26, 155–163. [Google Scholar] [CrossRef]
- Börger, A.; Supancic, P.; Danzer, R. The ball on three balls test for strength testing of brittle discs: Stress distribution in the disc. J. Eur. Ceram. Soc. 2002, 22, 1425–1436. [Google Scholar] [CrossRef]
- Yin, R.; Jang, Y.-S.; Lee, M.-H.; Bae, T.-S. Comparative evaluation of mechanical properties and wear ability of five cad/cam dental blocks. Materials 2019, 12, 2252. [Google Scholar] [CrossRef]
- Atria, P.J.; Bordin, D.; Marti, F.; Msci, V.V.N.; Conejo, J.; Jalkh, E.B.; Witek, L.; Sampaio, C.S.; Dds, M.P.J.A.; Dds, D.B.; et al. 3D -printed resins for provisional dental restorations: Comparison of mechanical and biological properties. J. Esthet. Restor. Dent. 2022, 34, 804–815. [Google Scholar] [CrossRef] [PubMed]



| Manufacturer | Product | Shade | Composition | Batch Number |
|---|---|---|---|---|
| Graphy (GP) | TC-80DP | A1 | Methacrylate oligomer based on polyurethane resin, phosphine oxides, pigment | 1-B1220K11-003 |
| NextDent (NXT) | C&B MFH | N1 | >90% methacrylic oligomers, methacrylate monomer, <3% phosphine oxides, pigment | WX151N01 |
| Printing Materials | Printer | Manufacturer | Printing Volume | Layer Thickness | Wavelength | Pixel Pitch |
|---|---|---|---|---|---|---|
| GP | Sprintray Pro95 | Graphy Inc. | 192 × 100 × 200 mm | 50–100 μm | 405 nm | 95 µm |
| NXT | NextDent 5100 | NextDent B.V. | 124.8 × 70.2 × 196 mm | 30–100 μm | 405 nm | 65 µm |
| Thickness (mm) | Materials | Force Required for Fracture (N) | ||||||
|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | Min | Max | 95% CI | p Value | ||
| 0.4 | GP | 15 | 1937.4 | 360.6 | 1326.0 | 2621.0 | 1737.7–2137.1 | 0.000 * |
| NXT | 15 | 1262.5 | 178.6 | 912.2 | 1526.4 | 1163.6–1361.4 | ||
| 0.7 | GP | 15 | 1491.6 | 394.6 | 924.0 | 2197.2 | 1273.1–1710.2 | 0.103 |
| NXT | 15 | 1634.4 | 289.3 | 1200.8 | 2025.8 | 1474.2–1794.7 | ||
| NS | 15 | 1742.3 | 237.5 | 1296.9 | 2151.0 | 1610.8–1873.9 | ||
| 1.0 | GP | 15 | 1792.2 | 297.5 | 1279.1 | 2163.9 | 1627.4–1956.9 | 0.000 * |
| NXT | 15 | 2303.7 | 269.6 | 1848.2 | 2657.1 | 2154.4–2453.0 | ||
| Thickness (mm) | Materials | N | Biaxial Flexural Strength (MPa) | m | σo | R2 | ||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | p Value | ||||||
| 0.4 | GP | 15 | 3564.6 | 489.1 | 0.000 * | 8.55 | 3770.3 | 0.97 |
| NXT | 15 | 1279.9 | 359.9 | 4.03 | 1412.7 | 0.95 | ||
| 0.7 | GP | 14 | 845.4 | 155.3 | 0.000 * | 6.12 | 910.07 | 0.98 |
| NXT | 14 | 209.3 | 26.58 | 9.47 | 220.35 | 0.92 | ||
| 1.0 | GP | 15 | 329.3 | 45.40 | 0.000 * | 8.55 | 348.48 | 0.89 |
| NXT | 15 | 177.8 | 19.46 | 10.7 | 186.23 | 0.92 | ||
| Thickness (mm) | Materials | 50 MPa | 150 MPa | 250 MPa |
|---|---|---|---|---|
| 0.4 | GP | 100.0000 | 100.0000 | 100.0000 |
| NXT | 99.9999 | 99.9999 | 99.9999 | |
| 0.7 | GP | 100.0000 | 99.9984 | 99.9632 |
| NXT | 99.9999 | 97.4110 | 3.6763 | |
| 1.0 | GP | 100.0000 | 99.9259 | 94.3227 |
| NXT | 99.9999 | 90.6396 | 0.0000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, N.; Kim, H.; Kim, I.-H.; Lee, J.; Lee, K.E.; Lee, H.-S.; Kim, J.-H.; Song, J.S.; Shin, Y. Novel 3D Printed Resin Crowns for Primary Molars: In Vitro Study of Fracture Resistance, Biaxial Flexural Strength, and Dynamic Mechanical Analysis. Children 2022, 9, 1445. https://doi.org/10.3390/children9101445
Kim N, Kim H, Kim I-H, Lee J, Lee KE, Lee H-S, Kim J-H, Song JS, Shin Y. Novel 3D Printed Resin Crowns for Primary Molars: In Vitro Study of Fracture Resistance, Biaxial Flexural Strength, and Dynamic Mechanical Analysis. Children. 2022; 9(10):1445. https://doi.org/10.3390/children9101445
Chicago/Turabian StyleKim, Nayoung, Hoon Kim, Ik-Hwan Kim, Jiho Lee, Ko Eun Lee, Hyo-Seol Lee, Jee-Hwan Kim, Je Seon Song, and Yooseok Shin. 2022. "Novel 3D Printed Resin Crowns for Primary Molars: In Vitro Study of Fracture Resistance, Biaxial Flexural Strength, and Dynamic Mechanical Analysis" Children 9, no. 10: 1445. https://doi.org/10.3390/children9101445








