3D Surface Topographic Optical Scans Yield Highly Reliable Global Spine Range of Motion Measurements in Scoliotic and Non-Scoliotic Adolescents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Surface Topographic Scanner
2.3. Scan Protocol
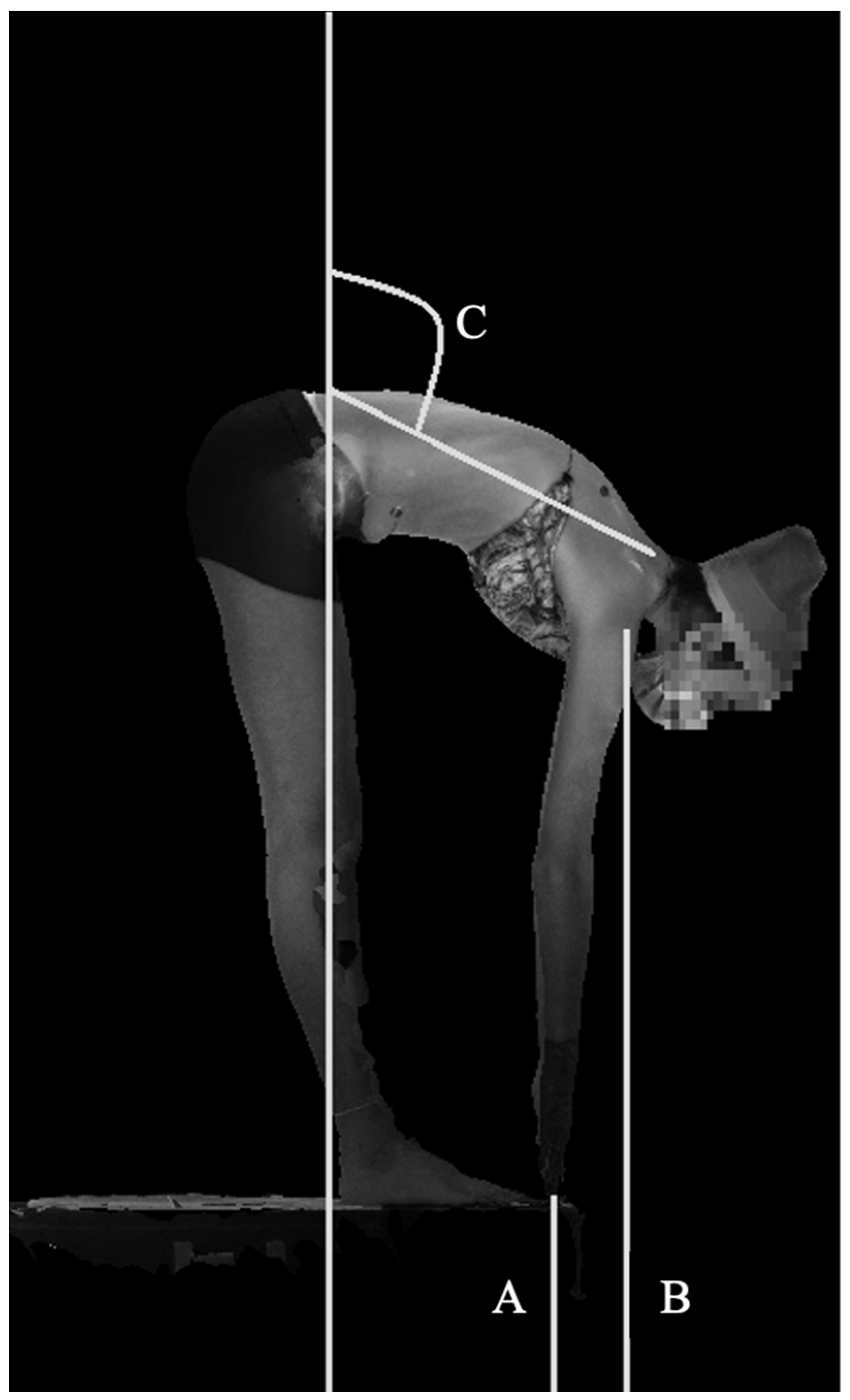
2.4. Automated Analysis
2.5. Reliability
2.6. Measurements
2.7. Statistical Analysis
3. Results
3.1. Reliability
3.2. Scoliosis Patients Versus Controls
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wiggins, G.C.; Shaffrey, C.I.; Abel, M.F.; Menezes, A.H. Pediatric spinal deformities. Neurosurg. Focus 2003, 14, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banton, R.A. Biomechanics of the spine. J. Spinal Res. Found. 2012, 7, 12–20. [Google Scholar]
- Bible, J.E.; Biswas, D.; Miller, C.P.; Whang, P.G.; Grauer, J.N. Normal functional range of motion of the lumbar spine during 15 activities of daily living. J. Spinal Disord. Tech. 2010, 23, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Eyvazov, K.; Samartzis, D.; Cheung, J.P.Y. The association of lumbar curve magnitude and spinal range of motion in adolescent idiopathic scoliosis: A cross-sectional study. BMC Musculoskelet. Disord. 2017, 18, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, P.S.; Park, M.S. Lumbar spine coordination during axial trunk rotation in adolescents with and without right thoracic idiopathic scoliosis. Hum. Mov. Sci. 2020, 73, 102680. [Google Scholar] [CrossRef]
- Perret, C.; Poiraudeau, S.; Fermanian, J.; Colau, M.M.L.; Benhamou, M.A.M.; Revel, M. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch. Phys. Med. Rehabil. 2010, 82, 1566–1570. [Google Scholar] [CrossRef]
- Macrae, I.F.; Wright, V. Measurement of back movement. Ann. Rheum. Dis. 1969, 28, 584–589. [Google Scholar] [CrossRef] [Green Version]
- Kelemen, J.; Eichhorn, M.; Ovenhausen, K.; Lorensen, W.; Müller, W. Reliability and validity studies with the triflexometer, a new method for assessing form and flexibility of the spine. Die Rehabil. 1998, 37, 78–84. [Google Scholar]
- Hresko, M.T.; Mesiha, M.; Richards, K.; Zurakowski, D. A Comparison of Methods for Measuring Spinal Motion in Female Patients with Adolescent Idiopathic Scoliosis. J. Pediatr. Orthop. 2006, 26, 758–763. [Google Scholar] [CrossRef]
- Aartun, E.; Degerfalk, A.; Kentsdotter, L.; Hestbaek, L. Screening of the spine in adolescents: Inter- and intra-rater reliability and measurement error of commonly used clinical tests. BMC Musculoskelet. Disord. 2014, 15, 37. [Google Scholar] [CrossRef]
- Merritt, J.L.; Mclean, T.J.; Erickson, R.P.; Offord, K.P. Measurement of trunk flexibility in normal subjects: Reproducibility of three clinical methods. Mayo Clin. Proc. 1986, 61, 192–197. [Google Scholar] [CrossRef]
- Gauvin, M.G.; Riddle, D.L.; Rothstein, J.M. Reliability of clinical measurements of forward bending using the modified fingertip-to-floor method. Phys. Ther. 1990, 70, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Kippers, V.; Parker, A.W. Toe-touch test: A measure of its validity. Phys. Ther. 1987, 67, 1680–1684. [Google Scholar] [CrossRef] [PubMed]
- Hyytiäinen, K.; Salminen, J.J.; Suvitie, T.; Wickström, G.; Pentti, J. Reproducibility of nine tests to measure spinal mobility and trunk muscle strength. Scand. J. Rehabil. Med. 1991, 23, 3–10. [Google Scholar] [PubMed]
- Lübbers, H.-T.; Medinger, L.; Kruse, A.; Grätz, K.W.; Matthews, F. Precision and accuracy of the 3dMD photogrammetric system in craniomaxillofacial application. J. Craniofacial Surg. 2010, 21, 763–767. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glaser, D.A.; Doan, J.; Newton, P.O. Comparison of 3-dimensional spinal reconstruction accuracy. Spine 2012, 37, 1391–1397. [Google Scholar] [CrossRef] [PubMed]
- Baksi, S.; Freezer, S.; Matsumoto, T.; Dreyer, C. Accuracy of an automated method of 3D soft tissue landmark detection. Eur. J. Orthod. 2021, 43, 622–630. [Google Scholar] [CrossRef] [PubMed]
- Knott, P.; Sturm, P.; Lonner, B.; Cahill, P.; Betsch, M.; McCarthy, R.; Kelly, M.; Lenke, L.; Betz, R. Multicenter comparison of 3D spinal measurements using surface topography with those from conventional radiography. Spine Deform. 2016, 4, 98–103. [Google Scholar] [CrossRef]
- Groisser, B.N.; Hillstrom, H.J.; Thakur, A.; Morse, K.W.; Cunningham, M.; Hresko, M.T.; Kimmel, R.; Wolf, A.; Widmann, R.F. Reliability of automated topographic measurements for spine deformity. Spine Deform. 2022, 10, 1035–1045. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Rezvani, A.; Ergin, O.; Karacan, I.; Oncu, M. Validity and reliability of the metric measurements in the assessment of lumbar spine motion in patients with ankylosing spondylitis. Spine 2012, 37, E1189–E1196. [Google Scholar] [CrossRef] [PubMed]
- Mayer, T.G.; Kondraske, G.; Beals, S.B.; Gatchel, R.J. Spinal range of motion. Accuracy and sources of error with inclinometric measurement. Spine 1997, 22, 1976–1984. [Google Scholar] [CrossRef] [PubMed]
- Ekedahl, H.; Jönsson, B.; Frobell, R.B. Fingertip-to-floor test and straight leg raising test: Validity, responsiveness, and predictive value in patients with acute/subacute low back pain. Arch. Phys. Med. Rehabil. 2012, 93, 2210–2215. [Google Scholar] [CrossRef] [PubMed]



| Lateral Bending Measurements | Description | Calculation |
| Lateral Bend Fingertip Asymmetry | Asymmetry of left vs. right bend fingertips to floor | 200 × |(finger tips right − finger tips left)|/(finger tips right + finger tips left) |
| Lateral Bend Acromia Asymmetry | Asymmetry of left vs. right bend acromia to floor | 200 × |(Right AC height right − left AC height left)|/(Right AC height right + left AC height left) |
| Coronal Angle Asymmetry | Asymmetry of left vs. right coronal angle (angle between C7 to PSIS midpoint and line between PSIS) | 200 × |(coronal angle right − coronal angle left)|/(coronal angle right + coronal angle left) |
| Coronal Angle ROM | Left + right coronal angle (summation of angles from C7 to PSIS midpoint and line between PSIS in left and right bends) | (coronal angle right + coronal angle left) |
| Forward Bending Measurements | Description | Calculation |
| Forward Bend Finger to Floor | Finger to floor distance in maximum forward flexion. Normalized to patient height. | (finger to floor distance)/(patient height) |
| Forward Bend Acromia to Floor | Average of acromioclavicular joint distance to floor in maximum forward flexion. Normalized to height. | (average distance from right AC joint to floor and left AC joint to floor)/(height) |
| Sagittal Angle | Maximum forward bend angle measured from C7 to PSIS midpoint, referenced to the line perpendicular to the floor. | (maximum forward bend angle) |
| Sagittal Angle Normalized | Maximum forward bend angle measured from C7 to PSIS midpoint, subtracting reference angle in A-pose. | (Sagittal angle forward − sagittal angle A pose) |
| Reliability | Controls, n = 20 | Patients, n = 26 |
|---|---|---|
| Sex | ||
| Males, n (%) | 11 (55) | 12 (46.2) |
| Age, mean (range, SD), years | 14.6 (11–20, 2.4) | 14.5 (11–21, 2.7) |
| BMI, mean (range, SD), kg/m2 | 21.7 (16.8–28.7, 3.8) | 20.6 (15.9–35.9, 4.3) |
| Measurements | Intra-Rater Reliability, ICC (95%CI) | Inter-Rater Reliability, ICC (95%CI) | |
|---|---|---|---|
| Test–Retest | Remove-Replace | ||
| Lateral Bending | |||
| LBFA | 0.448, 0.481 (0.165–0.677) | 0.233, 0.457 (−0.069–0.682) | 0.496 (0.236–0.689) |
| LBAA | 0.509, 0.564 (0.254–0.736) | 0.176, 0.588 (−0.128–0.752) | 0.433 (0.155–0.649) |
| CAA | 0.576, 0.769 (0.339–0.867) | 0.601, 0.738 (0.372–0.848) | 0.756 (0.594–0.859) |
| CAR | 0.910, 0.965 (0.842–0.981) | 0.795, 0.819 (0.655–0.897) | 0.783 (0.636–0.876) |
| Forward Bending | |||
| FBFF | 0.984, 0.990 (0.971–0.995) | 0.985. 0.985 (0.968–0.993) | 0.984 (0.970–0.991) |
| FBAF | 0.939, 0.958 (0.891–0.977) | 0.799, 0.836 (0.660–0.907) | 0.746 (0.580–0.852) |
| SA | 0.666, 0.750 (0.458–0.859) | 0.413, 0.995 (0.132–0.995) | 0.994 (0.988–0.996) |
| SAN | 0.973, 0.973 (0.950–0.986) | 0.957, 0.981 (0.921–0.990) | 0.977 (0.957–0.987) |
| Scoliosis Patients vs. Controls | Controls, n = 37 | Patients, n = 58 |
|---|---|---|
| Sex | ||
| Males, n (%) | 23 (62.2) | 21 (36.2) |
| Age, mean (range, SD), years | 14.3 (11–20, 2.4) | 14.6 (11–21, 2.2) |
| BMI, mean (range, SD), kg/m2 | 21.9 (16.8–29.7, 3.9) | 21.1 (15.3–35.9, 4.6) |
| Thoracic Cobb angle, average (range, SD), degrees | N/A | 49.5 (15.2–83.1, 17.1) |
| Lumbar Cobb angle, average (range, SD), degrees | N/A | 42.1 (25.1–86.3, 13.4) |
| Patients, n = 58 | Controls, n = 37 | ||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p-Value | |
| Lateral Bending Measurements | |||||
| LBFA | 10.80 | 9.01 | 6.35 | 6.40 | 0.011 |
| LBAA | 3.56 | 2.81 | 1.83 | 1.74 | 0.001 |
| CAA | 22.73 | 17.40 | 9.34 | 6.62 | ≤0.001 |
| CAR (degrees) | 68.91 | 18.99 | 73.68 | 12.15 | 0.18 |
| Forward Bending Measurements * | |||||
| FBFF | 0.076 | 0.062 | 0.07 | 0.054 | 0.63 |
| FBAF | 0.45 | 0.07 | 0.41 | 0.07 | 0.018 |
| SA (degrees) | 65.56 | 13.36 | 60.07 | 16.22 | 0.086 |
| SAN (degrees) | 59.14 | 13.13 | 54.19 | 16.27 | 0.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Page, K.; Gmelich, C.; Thakur, A.; Heyer, J.H.; Hillstrom, H.J.; Groisser, B.; Morse, K.W.; Li, D.; Cunningham, M.E.; Hresko, M.T.; et al. 3D Surface Topographic Optical Scans Yield Highly Reliable Global Spine Range of Motion Measurements in Scoliotic and Non-Scoliotic Adolescents. Children 2022, 9, 1756. https://doi.org/10.3390/children9111756
Page K, Gmelich C, Thakur A, Heyer JH, Hillstrom HJ, Groisser B, Morse KW, Li D, Cunningham ME, Hresko MT, et al. 3D Surface Topographic Optical Scans Yield Highly Reliable Global Spine Range of Motion Measurements in Scoliotic and Non-Scoliotic Adolescents. Children. 2022; 9(11):1756. https://doi.org/10.3390/children9111756
Chicago/Turabian StylePage, Kira, Caroline Gmelich, Ankush Thakur, Jessica H. Heyer, Howard J. Hillstrom, Benjamin Groisser, Kyle W. Morse, Don Li, Matthew E. Cunningham, M. Timothy Hresko, and et al. 2022. "3D Surface Topographic Optical Scans Yield Highly Reliable Global Spine Range of Motion Measurements in Scoliotic and Non-Scoliotic Adolescents" Children 9, no. 11: 1756. https://doi.org/10.3390/children9111756





