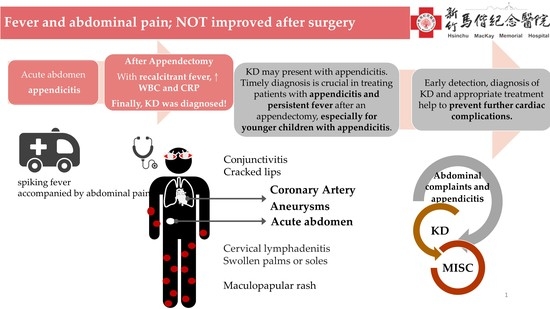
Appendicitis as a Leading Manifestation of Kawasaki Disease in Older Children
Abstract
:1. Introduction
2. Case Report
3. Discussion and Literature Review
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rife, E.; Gedalia, A. Kawasaki disease: An update. Curr. Rheumatol. Rep. 2020, 22, 75. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.L.; Kuo, H.C. Public health interventions for COVID-19 reduce kawasaki disease in Taiwan. Children 2021, 8, 623. [Google Scholar] [CrossRef] [PubMed]
- Garnett, G.M.; Kimball, S.; Melish, M.E.; Thompson, K.S.; Puapong, D.P.; Johnson, S.M.; Woo, R.K. Appendicitis as the presenting manifestation of kawasaki disease. Pediatr. Surg. Int. 2014, 30, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Zulian, F.; Falcini, F.; Zancan, L.; Martini, G.; Secchieri, S.; Luzzatto, C.; Zacchello, F. Acute surgical abdomen as presenting manifestation of kawasaki disease. J. Pediatr. 2003, 142, 731–735. [Google Scholar] [CrossRef] [PubMed]
- Yasukawa, K.; Terai, M.; Shulman, S.T.; Toyozaki, T.; Yajima, S.; Kohno, Y.; Rowley, A.H. Systemic production of vascular endothelial growth factor and fms-like tyrosine kinase-1 receptor in acute kawasaki disease. Circulation 2002, 105, 766–769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miyamoto, K.; Yamazaki, Y.; Okamoto, K.; Tsuboi, T.; Hirao, J.; Arisaka, O. Kawasaki disease: Relationship between acute surgical abdomen and cytokine profiles. Pediatr. Infect. Dis. J. 2013, 32, 1299. [Google Scholar] [CrossRef] [PubMed]
- Chiba, T. Two cases of appendicitis in kawasaki disease. Nihon Geka Hokan Arch. Fur Jpn. Chir. 1998, 67, 69–71. [Google Scholar]
- Ulloa-Gutierrez, R.; Gutierrez-Alvarez, R.; Avila-Aguero, M.L. Kawasaki disease mimicking an acute appendicitis. J. Pediatr. 2004, 144, 691. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.C.; Liotta, A.; Vitaliti, S.M.; Corsello, G. A case of kawasaki disease mimicking acute appendicitis. Med. J. Aust. 2007, 187, 316–317. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, A.H.; Dishop, M.K.; Baker, C.J. An unusual cause of appendicitis in a child. Semin. Pediatr. Infect. Dis. 2006, 17, 111–112. [Google Scholar] [CrossRef] [PubMed]
- Velez-Tirado, N.; Ridaura-Sanz, C.; Venegas-Montoya, E.; Scheffler-Mendoza, S.; Camacho-Moreno, R.; Otero-Mendoza, F.; Medina-Vega, F.A.; Garrido-García, L.M.; Rivas-Larrauri, F.; Nakashimada, M.A.Y. Acute abdomen in kawasaki disease. Indian J. Pediatr. 2019, 86, 1151–1152. [Google Scholar] [CrossRef] [PubMed]
- Thors, V.S.; Vastert, S.J.; Wulffraat, N.; van Royen, A.; Frenkel, J.; de Sain-van der Velden, M.; de Koning, T.J. Periodic fever in mvk deficiency: A patient initially diagnosed with incomplete kawasaki disease. Pediatrics 2014, 133, e461–e465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiu, N.-C.; Chi, H.; Tu, Y.-K.; Huang, Y.-N.; Tai, Y.-L.; Weng, S.-L.; Chang, L.; Huang, D.T.-N.; Huang, F.-Y.; Lin, C.-Y. To mix or not to mix? A rapid systematic review of heterologous prime–boost COVID-19 vaccination. Expert Rev. Vaccines 2021, 20, 1211–1220. [Google Scholar] [CrossRef] [PubMed]
- Lien, C.H.; Lee, M.D.; Weng, S.L.; Lin, C.H.; Liu, L.Y.; Tai, Y.L.; Lei, W.T.; Liu, J.M.; Huang, Y.N.; Chi, H.; et al. Repurposing colchicine in treating patients with COVID-19: A systematic review and meta-analysis. Life 2021, 11, 864. [Google Scholar] [CrossRef] [PubMed]
- Dufort, E.M.; Koumans, E.H.; Chow, E.J.; Rosenthal, E.M.; Muse, A.; Rowlands, J.; Barranco, M.A.; Maxted, A.M.; Rosenberg, E.S.; Easton, D.; et al. Multisystem inflammatory syndrome in children in new york state. N. Engl. J. Med. 2020, 383, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.J.; Chavarria, H.D.; Hacking, S.M. A case of multisystem inflammatory syndrome in children mimicking acute appendicitis in a COVID-19 pandemic area. Cureus 2020, 12, e10722. [Google Scholar] [CrossRef] [PubMed]

| Reference | Demographic Profile | Clinical Presentation | Treatment | Outcome | |||||
|---|---|---|---|---|---|---|---|---|---|
| Study (Publication Year) | AGE (Years Old), GENDER | Completed KD | WBC (103/uL) /CRP (mg/dL) | Sonography | Computed Tomography | Histological Findings | Surgery | IVIG | Coronary Artery Aneurysms |
| Our patient Chiba et al. (1998) [7] Zulian et al. (2003) [4] Ulloa-Gutierrez et al. (2004) [8] Bartlett et al. (2006) [10] Maggio et al. (2007) [9] Miyamoto et al. (2013) [6] Garnett et al. (2014) [3] Velez-Tirado et al. (2019) [11] | 5, M 6, M 4.6, M 5.4, M 4, M 7, M 3, M 5, M 3, M 7, F Three cases | + + + + + + + - + + 3/3 + | 10.3/11.8 21.3/11 12.6/7 21.6/6.9 24.2/14.9 23.2/16.7 Both elevated 15.9/15.5 Both elevated Both elevated NA | - NA - Appendicitis - - Appendicitis NA - NA NA | Appendicitis NA NA NA NA Post-operation NA Appendicitis Pelvic ascites All pelvic ascites 1/3 Perforation 2/3 Appendicitis | Appendicular vasculitis Acute phlegmonous appendicitis Inflammatory change with edema Acute transmural inflammation, arteritis Mesenteric adenitis NA Appendicular vasculitis Mesenteric adenitis Acute appendicitis Perforated suppurative appendicitis 2/3: Appendicitis 1/3: Serositis | + + + + + + + + + + All + | + + + + + + + + + + All + | Normal Normal Normal Normal Fusiform LCA Normal Saccular form -, pericardial effusion +, follow up normal LCA, persisted aneurysm All Normal |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.-N.; Liu, L.-H.; Chen, J.-J.; Tai, Y.-L.; Duh, Y.-C.; Lin, C.-Y. Appendicitis as a Leading Manifestation of Kawasaki Disease in Older Children. Children 2022, 9, 193. https://doi.org/10.3390/children9020193
Huang Y-N, Liu L-H, Chen J-J, Tai Y-L, Duh Y-C, Lin C-Y. Appendicitis as a Leading Manifestation of Kawasaki Disease in Older Children. Children. 2022; 9(2):193. https://doi.org/10.3390/children9020193
Chicago/Turabian StyleHuang, Ya-Ning, Lu-Hang Liu, Jeng-Jung Chen, Yu-Lin Tai, Yih-Cherng Duh, and Chien-Yu Lin. 2022. "Appendicitis as a Leading Manifestation of Kawasaki Disease in Older Children" Children 9, no. 2: 193. https://doi.org/10.3390/children9020193