Assessment of Occlusal Vertical Dimension Change in Mechanical and Virtual Articulation: A Pilot Study
Abstract
:1. Introduction
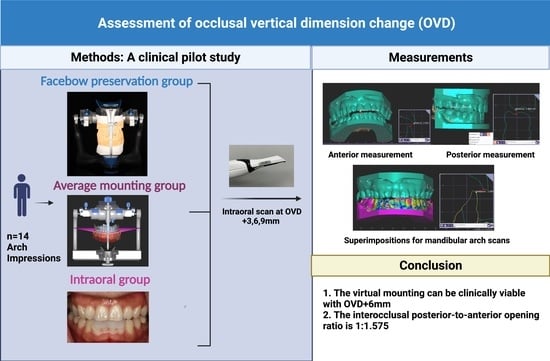
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- The mounting techniques of the average axis facebow record and the average values using the Bonwill triangle and the Balkwill angle in a virtual articulator (AMG) can be clinically viable with an increase in OVD up to 6 mm in dental Class 1 patients.
- The interocclusal posterior-to-anterior opening ratio observed clinically was 1:1.575, measured at the mandibular first molars and the central incisors. The coefficient of determination was 0.773, which showed a high correlation of anterior opening and posterior openings.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schopper, A.F. Loss of vertical dimension: Causes and effects: Diagnosis and various recommended treatments. J. Prosthet. Dent. 1959, 9, 428–431. [Google Scholar] [CrossRef]
- Turner, K.A.; Missirlian, D.M. Restoration of the extremely worn dentition. J. Prosthet. Dent. 1984, 52, 467–474. [Google Scholar] [CrossRef]
- Abduo, J.; Lyons, K. Clinical considerations for increasing occlusal vertical dimension: A review. Aust. Dent. J. 2012, 57, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J. Safety of increasing vertical dimension of occlusion: A systematic review. Quintessence Int. 2012, 43, 369–380. [Google Scholar] [PubMed]
- Calamita, M.; Coachman, C.; Sesma, N.; Kois, J. Occlusal vertical dimension: Treatment planning decisions and management considerations. Int. J. Esthet. Dent. 2019, 14, 166–181. [Google Scholar]
- The Glossary of Prosthodontic Terms: Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105. [CrossRef] [Green Version]
- Weinberg, L.A. An evaluation of the face-bow mounting. J. Prosthet. Dent. 1961, 11, 32–42. [Google Scholar] [CrossRef]
- Preston, J.D. A reassessment of the mandibular transverse horizontal axis theory. J. Prosthet. Dent. 1979, 41, 605–613. [Google Scholar] [CrossRef]
- Craddock, F.W.; Symmons, H.F. Evaluation of the face-bow. J. Prosthet. Dent. 1952, 2, 633–642. [Google Scholar] [CrossRef]
- Wieckiewicz, M.; Zietek, M.; Nowakowska, D.; Wieckiewicz, W. Comparison of selected kinematic facebows applied to mandibular tracing. BioMed. Res. Int. 2014, 2014, 818694. [Google Scholar] [CrossRef]
- Franklin, P.; McLelland, R.; Brunton, P. An investigation of the ability of computerized axiography to reproduce occlusal contacts. Eur. J. Prosthodont. Restor. Dent. 2010, 18, 17–22. [Google Scholar] [PubMed]
- Schallhorn, R.G. A study of the arbitrary center and the kinematic center of rotation for face-bow mountings. J. Prosthet. Dent. 1957, 3, 162–169. [Google Scholar] [CrossRef]
- Ahlers, M.O.; Edelhoff, D.; Jakstat, H.A. Reproduction accuracy of articulator mounting with an arbitrary face-bow vs. average values—A controlled, randomized, blinded patient simulator study. Clin. Oral Investig. 2019, 23, 1007–1014. [Google Scholar] [CrossRef] [PubMed]
- Att, W.; Witkowski, S.; Strub, J.R. Digital workflow in reconstructive dentistry. Quintessence Int. 2021, 6, 105–124. [Google Scholar]
- Lepidi, L.; Galli, M.; Mastrangelo, F.; Venezia, P.; Joda, T.; Wang, H.L.; Li, J. Virtual articulators and virtual mounting procedures: Where do we stand? J. Prosthodont. 2020, 30, 24–35. [Google Scholar] [CrossRef]
- Inoue, N.; Scialabba, R.; Lee, J.D.; Lee, S.J. A comparison of virtually mounted dental casts from traditional facebow records, average values, and 3D facial scans. J. Prosthet. Dent. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Olthoff, L.W.; Van Der Glas, H.W.; Van Der Bilt, A. Influence of occlusal vertical dimension on the masticatory performance during chewing with maxillary splints. J. Oral Rehabil. 2007, 34, 560–565. [Google Scholar] [CrossRef]
- Hsu, M.R.; Driscoll, C.F.; Romberg, E.; Masri, R. Accuracy of dynamic virtual articulation: Trueness and precision. J. Prosthodont. 2019, 28, 436–443. [Google Scholar] [CrossRef]
- Rebibo, M.; Darmouni, L.; Jouvin, J.; Orthlieb, J.D. Vertical dimension of occlusion: The keys to decision. J. Stomat. Occ. Med. 2009, 2, 147–159. [Google Scholar] [CrossRef]
- Kaiser, D.A.; Schelb, E. Geometric study of incisal guide pin opening. J. Prosthet. Dent. 1985, 53, 495. [Google Scholar] [CrossRef]
- Sharon, E.; Beyth, N.; Smidt, A.; Lipovetsky-Adler, M.; Zilberberg, N. Influence of jaw opening on occlusal vertical dimension between incisors and molars. J. Prosthet. Dent. 2019, 122, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Carossa, M.; Cavagnetto, D.; Ceruti, P.; Mussano, F.; Carossa, S. Individual mandibular movement registration and reproduction using an optoeletronic jaw movement analyzer and a dedicated robot: A dental technique. BMC Oral Health 2020, 20, 271. [Google Scholar] [CrossRef] [PubMed]






| Incisal Pin Opening (mm) | FPG | AMG | IOG | p Values |
|---|---|---|---|---|
| 3 | 1.949 ± 0.477 | 1.773 ± 0.381 | 2.180 ± 0.845 | 0.728 |
| 6 | 3.333 ± 0.483 | 2.913 ± 0.578 | 3.354 ± 0.829 | 0.101 |
| 9 | 4.263 ± 0.636 | 4.080 ± 0.690 | 4.844 ± 0.898 | 0.048 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, Y.-C.; Scialabba, R.; Lee, J.D.; Sun, J.; Lee, S.J. Assessment of Occlusal Vertical Dimension Change in Mechanical and Virtual Articulation: A Pilot Study. Dent. J. 2022, 10, 212. https://doi.org/10.3390/dj10110212
Lin Y-C, Scialabba R, Lee JD, Sun J, Lee SJ. Assessment of Occlusal Vertical Dimension Change in Mechanical and Virtual Articulation: A Pilot Study. Dentistry Journal. 2022; 10(11):212. https://doi.org/10.3390/dj10110212
Chicago/Turabian StyleLin, Yu-Chun, Rebecca Scialabba, Jason D. Lee, Jie Sun, and Sang J. Lee. 2022. "Assessment of Occlusal Vertical Dimension Change in Mechanical and Virtual Articulation: A Pilot Study" Dentistry Journal 10, no. 11: 212. https://doi.org/10.3390/dj10110212