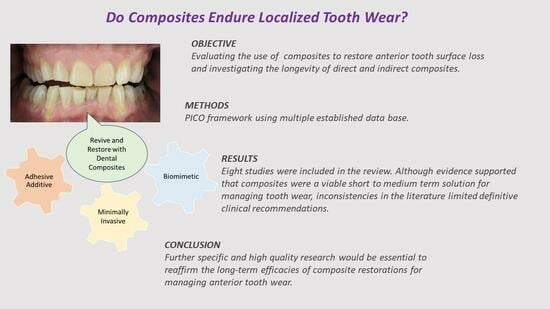
Longevity of Anterior Composite Restorations for Localized Tooth Wear: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Primary Aim and Null Hypothesis
2.2. Protocol Development
2.3. Search Strategy
2.4. Study Selection and Data Extraction
2.5. Analysis
| Author | Title |
|---|---|
| Crins et al. (2021) [27] | Randomized controlled trial on the performance of direct and indirect composite restorations in patients with severe tooth wear |
| Mehta et al. (2021) [25] | Clinical performance of direct composite resin restorations in a full mouth rehabilitation for patients with severe tooth wear: 5.5-year results |
| A. Milosevic and G. Burnside (2016) [26] | The survival of direct composite restorations for the management of severe tooth wear including attrition and erosion: a prospective 8-year study |
| A. Aljawad and J. S. Rees (2016) [24] | Retrospective study on survival and patient satisfaction with composite Dahl restorations in the management of localized anterior tooth wear |
| Al-Khayatt et al. (2013) [28] | Direct composite restorations for the worn mandibular anterior dentition: a 7-year follow-up of a prospective randomized controlled split-mouth clinical trial |
| Poyser et al. (2007) [12] | The evaluation of direct composite restorations for the worn mandibular anterior dentition—clinical performance and patient satisfaction |
| A. M. Gow and K. W. Hemmings (2002) [29] | The treatment of localized anterior tooth wear with indirect Artglass restorations at an increased occlusal vertical dimension. Results were presented after 2 years |
| Hemmings et al. (2000) [30] | Tooth wear treated with direct composite restorations at an increased vertical dimension: results were provided at 30 months |
2.6. Quality Assessment
2.7. Assessment of Risk of Bias in Included Studies
3. Results
Study Characteristics
| Author Study and Follow Up Period | Direct or Indirect | Type of Composite | No. of Patients | No. of Restorations | Outcome | Conclusion |
|---|---|---|---|---|---|---|
| Crins et al. (2021) RCT 3 years [27] | Direct and Indirect |
| 41 | 132 Direct maxilla palatal veneer 112 Indirect palatal veneer | Direct
|
|
| Mehta et al. (2021) Prospective 5.5 years [25] | Direct | Clearfil AP-X) | 34 |
| 77 failures (level 1 + level 2 failures) Survival 88.6% |
|
| Milosevic and Burnside (2016) Prospective 8 years [26] | Direct | Hybrid composite—spectrum | 164 | 903
| 67 (6.9%) of the direct composites failed. Failure was defined as a total debond or chip. Survival 92.5% |
|
| Aljawad and Rees (2016) Retrospective 25.4 months [24] | Direct | CeramX Duo) | 41 | 296 | Major failure 13 bulk fractures (4.4%) Minor failure
|
|
| Al-Khayatt et al. (2013) Prospective 7 years [28] | Direct | Micro-hybrid–Herculite XRV composite and Optibond dentine bonding agent | 15 | 85 | Survival of 85/89 at the 7-year (85%) | For the majority of patients, direct composite restorations worked well, provided high levels of patient satisfaction, and required minimal maintenance. |
| Poyser et al. (2007) Prospective 2.5 years [12] | Direct | Micro-hybrid–Herculite XRV composite and Optibond dentine bonding agent | 14 | 73 | Survival of 72/77 at 2.5 years. (94%)
|
|
| Gow and Hemmings 2002 Prospective 2 years [29] | Indirect | Artglass restoration | 12 | 75 | 100% survival 10 restorations had minor failures requiring chairside repairs. | Artglass indirect palatal restorations are an effective short-term treatment for localized anterior teeth wear. |
| Hemmings et al. (2000) Prospective 30 months [30] | Direct |
| 16 | 104 | 93% Survival
| For the treatment of localized anterior tooth wear, direct composite restorations could be an option. |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van’t Spijker, A.; Rodriguez, J.M.; Kreulen, C.M.; Bronkhorst, E.M.; Bartlett, D.W.; Creugers, N.H. Prevalence of tooth wear in adults. Int. J. Prosthodont. 2009, 22, 35–42. [Google Scholar] [PubMed]
- Mehta, S.B.; Banerji, S.; Millar, B.J.; Suarez-Feito, J.M. Current concepts on the management of tooth wear: Part 1. Assessment, treatment planning and strategies for the prevention and the passive management of tooth wear. Br. Dent. J. 2012, 212, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Hattab, F.N.; Yassin, O.M. Etiology and diagnosis of tooth wear: A literature review and presentation of selected cases. Int. J. Prosthodont. 2000, 13, 101–107. [Google Scholar] [PubMed]
- Wang, R.; Zhu, Y.; Chen, C.; Han, Y.; Zhou, H. Tooth Wear and Tribological Investigations in Dentistry. Appl. Bionics Biomech. 2022, 2022, 2861197. [Google Scholar] [CrossRef] [PubMed]
- Grippo, J.O.; Simring, M.; Schreiner, S. Attrition, abrasion, corrosion and abfraction revisited: A new perspective on tooth surface lesions. J. Am. Dent. Assoc. 2004, 135, 1109–1118. [Google Scholar] [CrossRef]
- Magne, P.; Magne, M.; Belser, U.C. Adhesive restorations, centric relation, and the Dahl principle: Minimally invasive approaches to localized anterior tooth erosion. Eur. J. Esthet. Dent. 2007, 2, 260–273. [Google Scholar] [PubMed]
- Smith, B.G.; Knight, J.K. An index for measuring the wear of teeth. Br. Dent. J. 1984, 156, 435–438. [Google Scholar] [CrossRef]
- Bartlett, D. A proposed system for screening tooth wear. Br. Dent. J. 2010, 208, 207–209. [Google Scholar] [CrossRef]
- Vailati, F.; Belser, U.C. Classification and treatment of the anterior maxillary dentition affected by dental erosion: The ACE classification. Int. J. Periodontics Restor. Dent. 2010, 30, 559–571. [Google Scholar]
- Al-Omiri, M.K.; Lamey, P.J.; Clifford, T. Impact of tooth wear on daily living. Int. J. Prosthodont. 2006, 19, 601–605. [Google Scholar]
- Muts, E.J.; van Pelt, H.; Edelhoff, D.; Krejci, I.; Cune, M. Tooth wear: A systematic review of treatment options. J. Prosthet. Dent. 2014, 112, 752–759. [Google Scholar] [CrossRef] [PubMed]
- Poyser, N.J.; Briggs, P.F.; Chana, H.S.; Kelleher, M.G.; Porter, R.W.; Patel, M.M. The evaluation of direct composite restorations for the worn mandibular anterior dentition—Clinical performance and patient satisfaction. J. Oral. Rehabil. 2007, 34, 361–376. [Google Scholar] [CrossRef] [PubMed]
- Magne, P. Composite resins and bonded porcelain: The postamalgam era? J. Calif. Dent. Assoc. 2006, 34, 135–147. [Google Scholar] [CrossRef]
- Mehta, S.B.; Banerji, S.; Millar, B.J.; Suarez-Feito, J.M. Current concepts on the management of tooth wear: Part 4. An overview of the restorative techniques and dental materials commonly applied for the management of tooth wear. Br. Dent. J. 2012, 212, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Tirlet, G.; Crescenzo, H.; Crescenzo, D.; Bazos, P. Ceramic adhesive restorations and biomimetic dentistry: Tissue preservation and adhesion. Int. J. Esthet. Dent. 2014, 9, 354–369. [Google Scholar] [PubMed]
- Bayne, S.C.; Heymann, H.O.; Swift, E.J., Jr. Update on dental composite restorations. J. Am. Dent. Assoc. 1994, 125, 687–701. [Google Scholar] [CrossRef] [PubMed]
- Labella, R.; Lambrechts, P.; Van Meerbeek, B.; Vanherle, G. Polymerization shrinkage and elasticity of flowable composites and filled adhesives. Dent. Mater. 1999, 15, 128–137. [Google Scholar] [CrossRef]
- Braga, R.R.; Ballester, R.Y.; Ferracane, J.L. Factors involved in the development of polymerization shrinkage stress in resin-composites: A systematic review. Dent. Mater. 2005, 21, 962–970. [Google Scholar] [CrossRef]
- Azeem, R.A.; Sureshbabu, N.M. Clinical performance of direct versus indirect composite restorations in posterior teeth: A systematic review. J. Conserv. Dent. 2018, 21, 2–9. [Google Scholar]
- Samran, A.; Al-Ammari, A.; El Bahra, S.; Halboub, E.; Wille, S.; Kern, M. Bond strength durability of self-adhesive resin cements to zirconia ceramic: An in vitro study. J. Prosthet. Dent. 2019, 121, 477–484. [Google Scholar] [CrossRef]
- Miao, C.; Yang, X.; Wong, M.C.; Zou, J.; Zhou, X.; Li, C.; Wang, Y. Rubber dam isolation for restorative treatment in dental patients. Cochrane Database Syst. Rev. 2021, 5, CD009858. [Google Scholar] [CrossRef]
- Bevenius, J.; Evans, S.; L’Estrange, P. Conservative management of erosion-abrasion: A system for the general practitioner. Aust. Dent. J. 1994, 39, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Lucarotti, P.S.; Holder, R.L.; Burke, F.J. Outcome of direct restorations placed within the general dental services in England and Wales (Part 3): Variation by dentist factors. J. Dent. 2005, 33, 827–835. [Google Scholar] [CrossRef]
- Aljawad, A.; Rees, J.S. Retrospective Study of the Survival and Patient Satisfaction with Composite Dahl Restorations in the Management of Localised Anterior Tooth Wear. Eur. J. Prosthodont. Restor. Dent. 2016, 24, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.B.; Lima, V.P.; Bronkhorst, E.M.; Crins, L.; Bronkhorst, H.; Opdam, N.J.M.; Huysmans, M.; Loomans, B.A.C. Clinical performance of direct composite resin restorations in a full mouth rehabilitation for patients with severe tooth wear: 5.5-year results. J. Dent. 2021, 112, 103743. [Google Scholar] [CrossRef]
- Milosevic, A.; Burnside, G. The survival of direct composite restorations in the management of severe tooth wear including attrition and erosion: A prospective 8-year study. J. Dent. 2016, 44, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Crins, L.A.M.J.; Opdam, N.J.M.; Kreulen, C.M.; Bronkhorst, E.M.; Sterenborg, B.A.M.M.; Huysmans, M.C.D.N.J.M.; Loomans, B.A.C. Randomized controlled trial on the performance of direct and indirect composite restorations in patients with severe tooth wear. Dent. Mater. 2021, 37, 1645–1654. [Google Scholar] [CrossRef] [PubMed]
- Al-Khayatt, A.S.; Ray-Chaudhuri, A.; Poyser, N.J.; Briggs, P.F.; Porter, R.W.; Kelleher, M.G.; Eliyas, S. Direct composite restorations for the worn mandibular anterior dentition: A 7-year follow-up of a prospective randomised controlled split-mouth clinical trial. J. Oral. Rehabil. 2013, 40, 389–401. [Google Scholar] [CrossRef]
- Gow, A.M.; Hemmings, K.W. The treatment of localised anterior tooth wear with indirect Artglass restorations at an increased occlusal vertical dimension. Results after two years. Eur. J. Prosthodont. Restor. Dent. 2002, 10, 101–105. [Google Scholar]
- Hemmings, K.W.; Darbar, U.R.; Vaughan, S. Tooth wear treated with direct composite restorations at an increased vertical dimension: Results at 30 months. J. Prosthet. Dent. 2000, 83, 287–293. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Gulamali, A.B.; Hemmings, K.W.; Tredwin, C.J.; Petrie, A. Survival analysis of composite Dahl restorations provided to manage localised anterior tooth wear (ten year follow-up). Br. Dent. J. 2011, 211, E9. [Google Scholar] [CrossRef] [PubMed]
- Mesko, M.E.; Sarkis-Onofre, R.; Cenci, M.S.; Opdam, N.J.; Loomans, B.; Pereira-Cenci, T. Rehabilitation of severely worn teeth: A systematic review. J. Dent. 2016, 48, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, K.E.; Murbay, S. Survival rates of anterior composites in managing tooth wear: Systematic review. J. Oral. Rehabil. 2016, 43, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; Bronkhorst, E.M.; Cenci, M.S.; Huysmans, M.C.; Wilson, N.H. Age of failed restorations: A deceptive longevity parameter. J. Dent. 2011, 39, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Milosevic, A. Clinical guidance and an evidence-based approach for restoration of the worn dentition by direct composite resin. Br. Dent. J. 2018, 224, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.; Sundaram, G. An up to 3-year randomized clinical study comparing indirect and direct resin composites used to restore worn posterior teeth. Int. J. Prosthodont. 2006, 19, 613–617. [Google Scholar] [PubMed]
- Loomans, B.; Bougatsias, L.; Sterenborg, B.; Bronkhorst, E.; Opdam, N.J.M. Survival of direct and indirect composites restorations in toothwear patients. J. Dent. Res. 2018, 97. [Google Scholar]
- Barghi, N.; Knight, G.T.; Berry, T.G. Comparing two methods of moisture control in bonding to enamel: A clinical study. Oper. Dent. 1991, 16, 130–135. [Google Scholar]
- Manhart, J.; Mehl, A.; Schroeter, R.; Obster, B.; Hickel, R. Bond strength of composite to dentin treated by air abrasion. Oper. Dent. 1999, 24, 223–232. [Google Scholar]
- De Munck, J.; Mine, A.; Poitevin, A.; Van Ende, A.; Cardoso, M.V.; Van Landuyt, K.L.; Peumans, M.; Van Meerbeek, B. Meta-analytical review of parameters involved in dentin bonding. J. Dent. Res. 2012, 91, 351–357. [Google Scholar] [CrossRef]
- Vailati, F.; Vaglio, G.; Belser, U.C. Full-mouth minimally invasive adhesive rehabilitation to treat severe dental erosion: A case report. J. Adhes. Dent. 2012, 14, 83–92. [Google Scholar] [CrossRef]
- Akar, G.C.; Dundar, M. Treatment of localized anterior tooth wear with a glass-fiber-reinforced composite resin: A clinical report. J. Prosthet. Dent. 2007, 97, 133–136. [Google Scholar] [CrossRef]



| Population | Patients with Anterior Tooth Surface Loss |
| Intervention | Restoration of worn teeth with direct anterior composite resin |
| Comparison | Restoration of worn teeth with indirect anterior composite resin |
| Outcome | Survival of direct and indirect anterior composite used in tooth surface loss |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Electronic databases and search terms | Ovid MEDLINE, Embase Classic + EMBASE, The Cochrane Library, Web of Science tooth wear OR dental wear OR tooth attrition OR dental abrasion OR dental erosion AND composite resin OR composite AND Dental restoration failure OR Dental Stress Analysis OR survival OR Longevity OR Fracture OR Chipping (Tooth or teeth or dental) near/3 (wear* or attrition or erosion or abrasion) (Topic) and “composite resin*” or “direct composite*” or “indirect composite*” or “dental restoration*” (Topic) and survival or “success rate*” or longevity or fracture* or chip* or “survival analysis” or “dental restoration failure” or “dental stress analysis” (Topic) |
| Other strategies used to find specific research | Additional articles were found by hand searching reference lists of pertinent papers and reviews. |
| Journals hand-searched | British Dental Journal, Journal of Aesthetic Dentistry, Journal of Adhesive Dentistry, Journal of prosthetic dentistry, Journal of Oral Rehabilitation would be searched manually |
| Author | Isolation | Splint | Assessment Criteria |
|---|---|---|---|
| Crins et al. (2021) [27] | Rubber dam or cotton roll | Not soon after the treatment 3 patients had a 1-year recall, as several fractures were seen | “(F1) severe deficiencies that were replaced or in case of loss of the tooth; (F2) Restorations with localized deficiencies repaired; (F3) Restorations with small material chippings that needed refurbishment by polishing” |
| Mehta et al. (2021) [25] | Rubber dam | Acrylic splints were not initially recommended, but when failure was later observed owing to fracture or wear from bruxist tendencies, a night guard was then indicated. | “Level 1 failure’ = a restoration with a severe deficiency, that required restoration replacement (to include the need for endodontic treatment, or a dental extraction); ‘Level 2 failure’ = a restoration with localized deficiencies, that was repaired, and ‘Level 3 failure’ = a restoration with small material chips” |
| Milosevic and Burnside (2016) [26] | No rubber dam | Not mentioned | Defined “failure as total debond or chip” |
| Aljawad and Rees (2016) [24] | Rubber dam not used | Not mentioned | Modified USPHS |
| Al-Khayatt et al. (2013) [28] | Rubber dam used | Not given | Modified USPHS |
| Poyser et al. (2007) [12] | Rubber dam used | Not given | Modified USPHS |
| Gow and Hemmings (2002) [29] | Not mentioned | Not mentioned | Modified USPHS (United States Public Health Services) |
| Hemmings et al. (2000) [30] | Rubber dam | Not given | Fracture, marginal discoloration, loss of marginal integrity, obvious wear, discomfort or sensitivity, endodontic failure, and cosmetic failure were all indications of failure. |
| I Squared % (N Studies) | p-Value | |
|---|---|---|
| Method | ||
| Direct [12,24,25,26,27,28,30] | 84.4% (7) | <0.001 |
| Indirect [27,29] | 78% (2) | <0.001 |
| Both [27] | N/A (1) | N/A |
| DIRECT ONLY | ||
| Design | ||
| Prospective [12,25,26,27,28,30] | 85.9(6) | 0.012 |
| Retrospective [24] | N/A (1) | N/A |
| Follow-up | ||
| Less than 3 years [12,24,27,30] | 87.5 (4) | <0.001 |
| More than 3 years [25,26,28] | 79.4 (3) | <0.001 |
| Occlusal Splint | ||
| Used [25,27] | 96.5 (2) | <0.001 |
| Not used [12,24,26,28,30] | 61.4 (5) | 0.035 |
| Rubber Dam | ||
| Used [12,25,27,28,30] | 88.6 (5) | <0.001 |
| Not used [24,26] | 70.5 (2) | 0.066 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rajarajan, S.; Nathwani, N.; Nejatian, T.; Fine, P.; Leung, A. Longevity of Anterior Composite Restorations for Localized Tooth Wear: A Scoping Review. Dent. J. 2023, 11, 255. https://doi.org/10.3390/dj11110255
Rajarajan S, Nathwani N, Nejatian T, Fine P, Leung A. Longevity of Anterior Composite Restorations for Localized Tooth Wear: A Scoping Review. Dentistry Journal. 2023; 11(11):255. https://doi.org/10.3390/dj11110255
Chicago/Turabian StyleRajarajan, Sindhu, Neil Nathwani, Touraj Nejatian, Peter Fine, and Albert Leung. 2023. "Longevity of Anterior Composite Restorations for Localized Tooth Wear: A Scoping Review" Dentistry Journal 11, no. 11: 255. https://doi.org/10.3390/dj11110255