Knowledge, Attitude, and Practice towards Chelating Agents in Endodontic Treatment among Dental Practitioners
Abstract
:1. Introduction
2. Materials and Methods
- z (z-score) = 1.96 (95% CI);
- p (standard deviation) = 0.5;
- e (a margin of error) = 0.05;
- N (a population size) = 5000.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chugal, N.; Mallya, S.M.; Kahler, B.; Lin, L.M. Endodontic Treatment Outcomes. Dent. Clin. N. Am. 2017, 61, 59–80. [Google Scholar] [CrossRef]
- McComb, D.; Smith, D.C. A Preliminary Scanning Electron Microscopic Study of Root Canals after Endodontic Procedures. J. Endod. 1975, 1, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Martinho, F.C.; Chiesa, W.M.M.; Marinho, A.C.S.; Zaia, A.A.; Ferraz, C.C.R.; Almeida, J.F.A.; Souza-Filho, F.J.; Gomes, B.P.F.A. Clinical Investigation of the Efficacy of Chemomechanical Preparation with Rotary Nickel-Titanium Files for Removal of Endotoxin from Primarily Infected Root Canals. J. Endod. 2010, 36, 1766–1769. [Google Scholar] [CrossRef]
- Aksel, H.; Küçükkaya Eren, S.; Puralı, N.; Serper, A.; Azim, A.A. Efficacy of Different Irrigant Protocols and Application Systems on Sealer Penetration Using a Stepwise CLSM Analysis. Microsc. Res. Tech. 2017, 80, 1323–1327. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.M.V.; Marins, F.C.; Belladonna, F.G.; Souza, E.M.; De-Deus, G.; Lopes, R.T.; Silva, E.J.N.L. Untouched Canal Areas and Debris Accumulation after Root Canal Preparation with Rotary and Adaptive Systems. Aust. Endod. J. 2018, 44, 260–266. [Google Scholar] [CrossRef]
- Wang, Z.; Shen, Y.; Haapasalo, M. Effect of Smear Layer against Disinfection Protocols on Enterococcus Faecalis-Infected Dentin. J. Endod. 2013, 39, 1395–1400. [Google Scholar] [CrossRef]
- Machado, R.; Garcia, L.d.F.R.; da Silva Neto, U.X.; Cruz Filho, A.d.M.d.; Silva, R.G.; Vansan, L.P. Evaluation of 17% EDTA and 10% Citric Acid in Smear Layer Removal and Tubular Dentin Sealer Penetration. Microsc. Res. Tech. 2018, 81, 275–282. [Google Scholar] [CrossRef]
- Kumar, P.; Prasad, N.; Darawade, A.; Bhagat, S.K.; Narayana, N.; Darawade, P. The Effect of Four Commonly Used Root Canal Irrigants on the Removal of Smear Layer: An In-Vitro Scanning Electron Microscope Study. J. Int. Oral. Health 2015, 7, 88. [Google Scholar]
- Vieira, A.R.; Siqueira, J.F.; Ricucci, D.; Lopes, W.S.P. Dentinal Tubule Infection as the Cause of Recurrent Disease and Late Endodontic Treatment Failure: A Case Report. J. Endod. 2012, 38, 250–254. [Google Scholar] [CrossRef]
- Shahravan, A.; Haghdoost, A.-A.; Adl, A.; Rahimi, H.; Shadifar, F. Effect of Smear Layer on Sealing Ability of Canal Obturation: A Systematic Review and Meta-Analysis. J. Endod. 2007, 33, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Morago, A.; Ordinola-Zapata, R.; Ferrer-Luque, C.M.; Baca, P.; Ruiz-Linares, M.; Arias-Moliz, M.T. Influence of Smear Layer on the Antimicrobial Activity of a Sodium Hypochlorite/Etidronic Acid Irrigating Solution in Infected Dentin. J. Endod. 2016, 42, 1647–1650. [Google Scholar] [CrossRef]
- Grossman, L.I.; Meiman, B.W. Solution of Pulp Tissue by Chemical Agents. J. Am. Dent. Assoc. 1941, 28, 223–225. [Google Scholar] [CrossRef]
- Willershausen, I.; Wolf, T.G.; Schmidtmann, I.; Berger, C.; Ehlers, V.; Willershausen, B.; Briseño, B. Survey of Root Canal Irrigating Solutions Used in Dental Practices within Germany. Int. Endod. J. 2015, 48, 654–660. [Google Scholar] [CrossRef]
- Savani, G.M.; Sabbah, W.; Sedgley, C.M.; Whitten, B. Current Trends in Endodontic Treatment by General Dental Practitioners: Report of a United States National Survey. J. Endod. 2014, 40, 618–624. [Google Scholar] [CrossRef]
- Natanasabapathy, V.; Durvasulu, A.; Krithikadatta, J.; Namasivayam, A.; Deivanayagam, K.; Manali, S.; Sureshbabu, N.M. Current Trends in the Use of Irrigant Activation Techniques among Endodontists & Post-Graduate Dental Students in India—A Knowledge, Attitude and Practice Based Survey. Eur. Endod. J. 2020, 5, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Zaugg, L.K.; Savic, A.; Amato, M.; Amato, J.; Weiger, R.; Connert, T. Endodontic Treatment in Switzerland. A National Survey. Swiss Dent. J. 2019, 130, 18–29. [Google Scholar]
- Gbadebo, S.O.; Ajayi, D.M. Endodontic Practice amongst Nigerian Dentists Undergoing Postgraduate Training. Pan Afr. Med. J. 2021, 39. [Google Scholar] [CrossRef]
- Haapasalo, M.; Shen, Y.; Qian, W.; Gao, Y. Irrigation in Endodontics. Dent. Clin. N. Am. 2010, 54, 291–312. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Bhosale, A.; Pawar, S.; Kakti, A.; Bichpuriya, A.; Agwan, M.A. Current Trends in Root Canal Irrigation. Cureus 2022, 14, e24833. [Google Scholar] [CrossRef]
- Zehnder, M. Root Canal Irrigants. J. Endod. 2006, 32, 389–398. [Google Scholar] [CrossRef]
- Violich, D.R.; Chandler, N.P. The Smear Layer in Endodontics—A Review. Int. Endod. J. 2010, 43, 2–15. [Google Scholar] [CrossRef] [PubMed]
- Mello, I.; Kammerer, B.A.; Yoshimoto, D.; Macedo, M.C.S.; Antoniazzi, J.H. Influence of Final Rinse Technique on Ability of Ethylenediaminetetraacetic Acid of Removing Smear Layer. J. Endod. 2010, 36, 512–514. [Google Scholar] [CrossRef] [PubMed]
- Goldman, M.; Goldman, L.B.; Cavaleri, R.; Bogis, J.; Sun Lin, P. The Efficacy of Several Endodontic Irrigating Solutions: A Scanning Electron Microscopic Study: Part 2. J. Endod. 1982, 8, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Yamada, R.S.; Armas, A.; Goldman, M.; Lin, P.S. A Scanning Electron Microscopic Comparison of a High Volume Final Flush with Several Irrigating Solutions: Part 3. J. Endod. 1983, 9, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Niu, W.; Yoshioka, T.; Kobayashi, C.; Suda, H. A Scanning Electron Microscopic Study of Dentinal Erosion by Final Irrigation with EDTA and NaOCl Solutions. Int. Endod. J. 2002, 35, 934–939. [Google Scholar] [CrossRef]
- Kovac, J.; Kovac, D. Effect of Irrigating Solutions in Endodontic Therapy. Bratisl. Lek. Listy 2011, 112, 410–415. [Google Scholar]
- Grawehr, M.; Sener, B.; Waltimo, T.; Zehnder, M. Interactions of Ethylenediamine Tetraacetic Acid with Sodium Hypochlorite in Aqueous Solutions. Int. Endod. J. 2003, 36, 411–417. [Google Scholar] [CrossRef]
- Dutner, J.; Mines, P.; Anderson, A. Irrigation Trends among American Association of Endodontists Members: A Web-Based Survey. J. Endod. 2012, 38, 37–40. [Google Scholar] [CrossRef]
- Calt, S.; Serper, A. Time-Dependent Effects of EDTA on Dentin Structures. J. Endod. 2002, 28, 17–19. [Google Scholar] [CrossRef] [PubMed]
- De-Deus, G.; Zehnder, M.; Reis, C.; Fidel, S.; Fidel, R.A.S.; Galan, J.J.; Paciornik, S. Longitudinal Co-Site Optical Microscopy Study on the Chelating Ability of Etidronate and EDTA Using a Comparative Single-Tooth Model. J. Endod. 2008, 34, 71–75. [Google Scholar] [CrossRef] [Green Version]
- Hülsmann, M.; Heckendorff, M.; Lennon, Á. Chelating Agents in Root Canal Treatment: Mode of Action and Indications for Their Use. Int. Endod. J. 2003, 36, 810–830. [Google Scholar] [CrossRef]
- Tiwari, S.; Nikhade, P.; Chandak, M.; Sudarshan, C.; Shetty, P.; Gupta, N.K. Impact of Various Irrigating Agents on Root Fracture: An In Vitro Study. J. Contemp. Dent. Pract. 2016, 17, 659–662. [Google Scholar] [CrossRef]
- Generali, L.; Prati, C.; Pirani, C.; Cavani, F.; Gatto, M.R.; Gandolfi, M.G. Double Dye Technique and Fluid Filtration Test to Evaluate Early Sealing Ability of an Endodontic Sealer. Clin. Oral. Investig. 2017, 21, 1267–1276. [Google Scholar] [CrossRef]
- Mandras, N.; Pasqualini, D.; Roana, J.; Tullio, V.; Banche, G.; Gianello, E.; Bonino, F.; Cuffini, A.M.; Berutti, E.; Alovisi, M. Influence of Photon-Induced Photoacoustic Streaming (PIPS) on Root Canal Disinfection and Post-Operative Pain: A Randomized Clinical Trial. J. Clin. Med. 2020, 9, 3915. [Google Scholar] [CrossRef]
- Gandolfi, M.G.; Taddei, P.; Pondrelli, A.; Zamparini, F.; Prati, C.; Spagnuolo, G. Demineralization, Collagen Modification and Remineralization Degree of Human Dentin after EDTA and Citric Acid Treatments. Materials 2019, 12, 25. [Google Scholar] [CrossRef] [Green Version]
- Matos, F.d.S.; da Silva, F.R.; Paranhos, L.R.; Moura, C.C.G.; Bresciani, E.; Valera, M.C. The Effect of 17% EDTA and QMiX Ultrasonic Activation on Smear Layer Removal and Sealer Penetration: Ex Vivo Study. Sci. Rep. 2020, 10, 10311. [Google Scholar] [CrossRef] [PubMed]
- Alakshar, A.; Saleh, A.R.M.; Gorduysus, M.O. Debris and Smear Layer Removal from Oval Root Canals Comparing XP-Endo Finisher, EndoActivator, and Manual Irrigation: A SEM Evaluation. Eur. J. Dent. 2020, 14, 626–633. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidi, E.; Psimma, Z.; Chávez de Paz, L.E.; Boutsioukis, C. Apical Negative Pressure Irrigation versus Syringe Irrigation: A Systematic Review of Cleaning and Disinfection of the Root Canal System. Int. Endod. J. 2017, 50, 1034–1054. [Google Scholar] [CrossRef] [Green Version]
- Badami, V.; Akarapu, S.; Kethineni, H.; Mittapalli, S.P.; Bala, K.R.; Fatima, S.F. Efficacy of Laser-Activated Irrigation Versus Ultrasonic-Activated Irrigation: A Systematic Review. Cureus 2023, 15, e36352. [Google Scholar] [CrossRef]
- Solakoğlu, E.; Topçuoğlu, H.S.; Düzgün, S. Effect of Different Final Irrigation Agitation Techniques on Root Canal Dentin Tubule Penetration of Nanoparticle Calcium Hydroxide Dressing. Aust. Endod. J. 2023. [Google Scholar] [CrossRef] [PubMed]
- Widbiller, M.; Rosendahl, A.; Schlichting, R.; Schuller, C.; Lingl, B.; Hiller, K.A.; Buchalla, W.; Galler, K.M. Impact of Endodontic Irrigant Activation on Smear Layer Removal and Surface Disintegration of Root Canal Dentine In Vitro. Healthcare 2023, 11, 376. [Google Scholar] [CrossRef]
- Arias-Moliz, M.T.; Ferrer-Luque, C.M.; Espigares-Rodríguez, E.; Liébana-Ureña, J.; Espigares-García, M. Bactericidal Activity of Phosphoric Acid, Citric Acid, and EDTA Solutions against Enterococcus Faecalis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, e84–e89. [Google Scholar] [CrossRef]
- Arias-Moliz, M.T.; Ferrer-Luque, C.M.; Espigares-García, M.; Baca, P. Enterococcus Faecalis Biofilms Eradication by Root Canal Irrigants. J. Endod. 2009, 35, 711–714. [Google Scholar] [CrossRef]
- Ordinola-Zapata, R.; Bramante, C.M.; Cavenago, B.; Graeff, M.S.Z.; Gomes de Moraes, I.; Marciano, M.; Duarte, M.A.H. Antimicrobial Effect of Endodontic Solutions Used as Final Irrigants on a Dentine Biofilm Model. Int. Endod. J. 2012, 45, 162–168. [Google Scholar] [CrossRef]
- Bryce, G.; O’Donnell, D.; Ready, D.; Ng, Y.-L.; Pratten, J.; Gulabivala, K. Contemporary Root Canal Irrigants Are Able to Disrupt and Eradicate Single- and Dual-Species Biofilms. J. Endod. 2009, 35, 1243–1248. [Google Scholar] [CrossRef] [PubMed]
- Busanello, F.H.; Petridis, X.; So, M.V.R.; Dijkstra, R.J.B.; Sharma, P.K.; van der Sluis, L.W.M. Chemical Biofilm Removal Capacity of Endodontic Irrigants as a Function of Biofilm Structure: Optical Coherence Tomography, Confocal Microscopy and Viscoelasticity Determination as Integrated Assessment Tools. Int. Endod. J. 2019, 52, 461–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zehnder, M.; Schmidlin, P.; Sener, B.; Waltimo, T. Chelation in Root Canal Therapy Reconsidered. J. Endod. 2005, 31, 817–820. [Google Scholar] [CrossRef]
- Boutsioukis, C.; Arias-Moliz, M.T. Present Status and Future Directions—Irrigants and Irrigation Methods. Int. Endod. J. 2022, 55, 588–612. [Google Scholar] [CrossRef] [PubMed]
- Viola, K.S.; Coaguila-Llerena, H.; Rodrigues, E.M.; Santos, C.S.; Chávez-Andrade, G.M.; Magro, M.G.; Tanomaru-Filho, M.; Guerreiro-Tanomaru, J.M.; Faria, G. Different Formulations of Peracetic Acid: Effects on Smear Layer Removal, Dentine Erosion, Cytotoxicity and Antibiofilm Activity. J. Appl. Oral. Sci. 2022, 30, e20210575. [Google Scholar] [CrossRef]
- Gawdat, S.I.; Bedier, M.M. Influence of Dual Rinse Irrigation on Dentinal Penetration of a Bioceramic Root Canal Sealer: A Conofocal Microscopic Analysis. Aust. Endod. J. 2022, 48, 481–486. [Google Scholar] [CrossRef]
- Barcellos, D.P.D.C.; Farina, A.P.; Barcellos, R.; Souza, M.A.; Borba, M.; Bedran-Russo, A.K.; Bello, Y.D.; Pimenta Vidal, C.D.M.; Cecchin, D. Effect of a New Irrigant Solution Containing Glycolic Acid on Smear Layer Removal and Chemical/Mechanical Properties of Dentin. Sci. Rep. 2020, 10, 7313. [Google Scholar] [CrossRef]
- Wayman, B.E.; Kopp, W.M.; Pinero, G.J.; Lazzari, E.P. Citric and Lactic Acids as Root Canal Irrigants in vitro. J. Endod. 1979, 5, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Heredia, M.; Ferrer-Luque, C.M.; González-Rodríguez, M.P. The Effectiveness of Different Acid Irrigating Solutions in Root Canal Cleaning after Hand and Rotary Instrumentation. J. Endod. 2006, 32, 993–997. [Google Scholar] [CrossRef]
- Prado, M.; Gusman, H.; Gomes, B.P.F.A.; Simão, R.A. Scanning Electron Microscopic Investigation of the Effectiveness of Phosphoric Acid in Smear Layer Removal When Compared with EDTA and Citric Acid. J. Endod. 2011, 37, 255–258. [Google Scholar] [CrossRef] [Green Version]
- Ballal, N.V.; Kandian, S.; Mala, K.; Bhat, K.S.; Acharya, S. Comparison of the Efficacy of Maleic Acid and Ethylenediaminetetraacetic Acid in Smear Layer Removal from Instrumented Human Root Canal: A Scanning Electron Microscopic Study. J. Endod. 2009, 35, 1573–1576. [Google Scholar] [CrossRef]
- Ballal, N.V.; Jain, I.; Tay, F.R. Evaluation of the Smear Layer Removal and Decalcification Effect of QMix, Maleic Acid and EDTA on Root Canal Dentine. J. Dent. 2016, 51, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Kaushal, R.; Bansal, R.; Malhan, S. A Comparative Evaluation of Smear Layer Removal by Using Ethylenediamine Tetraacetic Acid, Citric Acid, and Maleic Acid as Root Canal Irrigants: An in vitro Scanning Electron Microscopic Study. J. Conserv. Dent. 2020, 23, 71–78. [Google Scholar] [CrossRef]
- Ferrer-Luque, C.M.; Arias-Moliz, M.T.; González-Rodríguez, M.P.; Baca, P. Antimicrobial Activity of Maleic Acid and Combinations of Cetrimide with Chelating Agents against Enterococcus Faecalis Biofilm. J. Endod. 2010, 36, 1673–1675. [Google Scholar] [CrossRef] [PubMed]
- Sceiza, M.F.; Daniel, R.L.; Santos, E.M.; Jaeger, M.M. Cytotoxic Effects of 10% Citric Acid and EDTA-T Used as Root Canal Irrigants: An In Vitro Analysis. J. Endod. 2001, 27, 741–743. [Google Scholar] [CrossRef] [PubMed]
- Ballal, N.V.; Moorkoth, S.; Mala, K.; Bhat, K.S.; Hussen, S.S.; Pathak, S. Evaluation of Chemical Interactions of Maleic Acid with Sodium Hypochlorite and Chlorhexidine Gluconate. J. Endod. 2011, 37, 1402–1405. [Google Scholar] [CrossRef]
- Wright, P.P.; Cooper, C.; Kahler, B.; Walsh, L.J. From an Assessment of Multiple Chelators, Clodronate Has Potential for Use in Continuous Chelation. Int. Endod. J. 2020, 53, 122–134. [Google Scholar] [CrossRef]
- Biel, P.; Mohn, D.; Attin, T.; Zehnder, M. Interactions between the Tetrasodium Salts of EDTA and 1-Hydroxyethane 1,1-Diphosphonic Acid with Sodium Hypochlorite Irrigants. J. Endod. 2017, 43, 657–661. [Google Scholar] [CrossRef] [Green Version]
- Solana, C.; Ruiz-Linares, M.; Baca, P.; Valderrama, M.J.; Arias-Moliz, M.T.; Ferrer-Luque, C.M. Antibiofilm Activity of Sodium Hypochlorite and Alkaline Tetrasodium EDTA Solutions. J. Endod. 2017, 43, 2093–2096. [Google Scholar] [CrossRef]
- Tartari, T.; Oda, D.F.; Zancan, R.F.; da Silva, T.L.; de Moraes, I.G.; Duarte, M.A.H.; Bramante, C.M. Mixture of Alkaline Tetrasodium EDTA with Sodium Hypochlorite Promotes In Vitro Smear Layer Removal and Organic Matter Dissolution during Biomechanical Preparation. Int. Endod. J. 2017, 50, 106–114. [Google Scholar] [CrossRef]
- Arias-Moliz, M.T.; Ordinola-Zapata, R.; Baca, P.; Ruiz-Linares, M.; Ferrer-Luque, C.M. Antimicrobial Activity of a Sodium Hypochlorite/Etidronic Acid Irrigant Solution. J. Endod. 2014, 40, 1999–2002. [Google Scholar] [CrossRef]
- Tartari, T.; Guimarães, B.M.; Amoras, L.S.; Duarte, M.A.H.; Silva e Souza, P.A.R.; Bramante, C.M. Etidronate Causes Minimal Changes in the Ability of Sodium Hypochlorite to Dissolve Organic Matter. Int. Endod. J. 2015, 48, 399–404. [Google Scholar] [CrossRef]
- Alzamzami, Z.T.; Alqurashi, A.A.; Almansour, L.A.; Ashi, H.M.; Abulhamael, A.M.; Alghamdi, F.T.; Albahiti, M.T. Current Trends in Irrigation Solution and Adjunct Use During Endodontic Therapy Among Dental Professionals in Jeddah, Saudi Arabia: A Cross-Sectional Study. Cureus 2022, 14, e32168. [Google Scholar] [CrossRef]
- Gopikrishna, V.; Pare, S.; Pradeep Kumar, A.; Lakshmi Narayanan, L. Irrigation Protocol among Endodontic Faculty and Post-Graduate Students in Dental Colleges of India: A Survey. J. Conserv. Dent. 2013, 16, 394–398. [Google Scholar] [CrossRef] [Green Version]
- Mohammadi, Z.; Shalavi, S.; Yaripour, S.; Kinoshita, J.-I.; Manabe, A.; Kobayashi, M.; Giardino, L.; Palazzi, F.; Sharifi, F.; Jafarzadeh, H. Smear Layer Removing Ability of Root Canal Irrigation Solutions: A Review. J. Contemp. Dent. Pract. 2019, 20, 395–402. [Google Scholar] [CrossRef]
- Basrani, B.; Haapasalo, M. Update on Endodontic Irrigating Solutions. Endod. Topics 2012, 27, 74–102. [Google Scholar] [CrossRef]
- Albahiti, M.H. Knowledge and Practices of Decontamination during Root Canal Treatment by Dentists in Jeddah. Saudi Dent. J. 2020, 32, 213–218. [Google Scholar] [CrossRef]
- Dogra, M.; Sawai, D.; Ganapathy, S.; Sharma, U.; Singh, I.; Gupta, P. Knowledge, Attitude, and Practice of General Dental Practitioners toward Following Proper Standards of Endodontic Practice and Use of Latest Technology in Dehradun: A Cross-Sectional Study. J. Fam. Med. Prim. Care 2020, 9, 282. [Google Scholar] [CrossRef]
- Bansal, N.; Dogra, M.; Mehta, P.; Khan, S.; Jhunjhunwala, N.; Gupta, P. Perception, Knowledge, and Practice of Endodontists and General Dental Practitioners toward Evidence-Based Practice and Factors Associated with It—A Cross-Sectional Study. J. Fam. Med. Prim. Care 2020, 9, 2958. [Google Scholar] [CrossRef]
- Al-Omari, W.M. Survey of Attitudes, Materials and Methods Employed in Endodontic Treatment by General Dental Practitioners in North Jordan. BMC Oral Health 2004, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Drake, D.R.; Wiemann, A.H.; Rivera, E.M.; Walton, R.E. Bacterial Retention in Canal Walls In Vitro: Effect of Smear Layer. J. Endod. 1994, 20, 78–82. [Google Scholar] [CrossRef]
- Pashley, D.H. Dentin-Predentin Complex and Its Permeability: Physiologic Overview. J. Dent. Res. 1985, 64, 613–620. [Google Scholar] [CrossRef]
- Williams, S.; Goldman, M. Penetrability of the Smeared Layer by a Strain of Proteus Vulgaris. J. Endod. 1985, 11, 385–388. [Google Scholar] [CrossRef]
- Meryon, S.D.; Brook, A.M. Penetration of Dentine by Three Oral Bacteria In Vitro and Their Associated Cytotoxicity. Int. Endod. J. 1990, 23, 196–202. [Google Scholar] [CrossRef]
- Virdee, S.S.; Ravaghi, V.; Camilleri, J.; Cooper, P.; Tomson, P. Current Trends in Endodontic Irrigation amongst General Dental Practitioners and Dental Schools within the United Kingdom and Ireland: A Cross-Sectional Survey. Br. Dent. J. 2020, 1–7. [Google Scholar] [CrossRef]
- White, R.R.; Goldman, M.; Lin, P.S. The Influence of the Smeared Layer upon Dentinal Tubule Penetration by Plastic Filling Materials. J. Endod. 1984, 10, 558–562. [Google Scholar] [CrossRef]
- Baumgartner, J.C.; Mader, C.L. A Scanning Electron Microscopic Evaluation of Four Root Canal Irrigation Regimens. J. Endod. 1987, 13, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Cengiz, T.; Aktener, B.O.; Piskin, B. Effect of Dentinal Tubule Orientation on the Removal of Smear Layer by Root Canal Irrigants. A Scanning Electron Microscopic Study. Int. Endod. J. 1990, 23, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Tošić, G.; Miladinović, M.; Kovačević, M.; Stojanović, M. Choice of Root Canal Irrigants by Serbian Dental Practitioners. Vojnosanit. Pregl. 2016, 73, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Al-Fouzan, K.S. A Survey of Root Canal Treatment of Molar Teeth by General Dental Practitioners in Private Practice in Saudi Arabia. Saudi Dent. J. 2010, 22, 113–117. [Google Scholar] [CrossRef] [Green Version]
- Ravanshad, S.; Sahraei, S.; Khayat, A. Survey of Endodontic Practice amongst Iranian Dentists Participating Restorative Dentistry Congress in Shiraz, November 2007. Iran. Endod. J. 2008, 2, 135–142. [Google Scholar] [PubMed]
- Tsotsis, P.; Dunlap, C.; Scott, R.; Arias, A.; Peters, O.A. A Survey of Current Trends in Root Canal Treatment: Access Cavity Design and Cleaning and Shaping Practices. Aust. Endod. J. 2021, 47, 27–33. [Google Scholar] [CrossRef]
- De Gregorio, C.; Arias, A.; Navarrete, N.; Cisneros, R.; Cohenca, N. Differences in Disinfection Protocols for Root Canal Treatments between General Dentists and Endodontists: A Web-Based Survey. J. Am. Dent. Assoc. 2015, 146, 536–543. [Google Scholar] [CrossRef]
- Moss, H.D.; Allemang, J.D.; Johnson, J.D. Philosophies and Practices Regarding the Management of the Endodontic Smear Layer: Results from Two Surveys. J. Endod. 2001, 27, 537–539. [Google Scholar] [CrossRef]
- Vasundhara, V.; Kumar, A.; Kamal Badiyani, B. Assessment of Irrigation Practice among Dentists in South India. Int. J. Med. Oral Res. 2020, 5, 1–3. [Google Scholar]
- Unal, G.C.; Kaya, B.U.; Tac, A.G.; Kececi, A.D. Survey of Attitudes, Materials and Methods Preferred in Root Canal Therapy by General Dental Practice in Turkey: Part 1. Eur. J. Dent. 2012, 6, 376–384. [Google Scholar] [CrossRef] [Green Version]





| Sociodemographic Data | Count, n | Percentage, % |
|---|---|---|
| Gender | ||
| Male | 115 | 30.6 |
| Female | 261 | 69.4 |
| Specialty | ||
| Endodontist | 47 | 12.5 |
| General practitioner | 329 | 87.5 |
| Years of clinical experience | ||
| <5 | 160 | 42.6 |
| 5–10 | 97 | 25.8 |
| 11–20 | 75 | 19.9 |
| >20 | 44 | 14.9 |
| Clinic | ||
| Private | 85 | 22.6 |
| Government-funded | 291 | 77.4 |
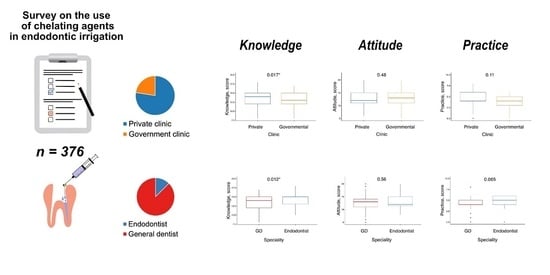
| Knowledge | Total | Specialty | Clinic | ||
|---|---|---|---|---|---|
| Endodontists | General Practitioners | Private | Government-Funded | ||
| Score, points | |||||
| Mean (sd) | 13.5 (2.4) | 14.3 (1.7) | 13.4 (2.1) | 13.7 (2.0) | 13.0 (2.2) |
| Median (Q1; Q3) | 14 (12; 15) | 15 (13; 15) | 14 (12; 15) | 13 (12; 15) | 14 (13; 15) |
| Min, Max | 8, 18 | 10, 28 | 8, 17 | 8, 18 | 8, 17 |
| p-value 1 | 0.01185 | 0.01742 | |||
| Level, n (%) | |||||
| Poor | 62 (16.5) | 2 (4.3) | 60 (18.2) | 42 (14.4) | 20 (23.5) |
| Fair | 314 (83.5) | 45 (95.7) | 269 (81.8) | 249 (85.6) | 65 (76.5) |
| Good | - | - | - | - | - |
| p-value 2 | 0.01157 | 0.06625 | |||
| Question | Total | Specialty | Clinic | ||
|---|---|---|---|---|---|
| Endodontists | General Practitioners | Private | Government-Funded | ||
| EDTA properties | |||||
| Correct | 313 (83.2) | 44 (93.6) | 269 (81.8) | 248 (85.2) | 65 (76.5) |
| Incorrect | 63 (16.8) | 3 (6.4) | 60 (18.2) | 43 (14.8) | 20 (23.5) |
| p-value 1 | 0.05744 | 0.06907 | |||
| EDTA concentration | |||||
| Correct | 295 (78.5) | 44 (93.6) | 251 (76.4) | 235 (80.8) | 60 (70.6) |
| Incorrect | 81 (21.5) | 3 (6.4) | 78 (23.6) | 56 (19.2) | 25 (29.4) |
| p-value 1 | 0.004399 | 0.05161 | |||
| Chelating solutions used for root canal irrigation | |||||
| Correct 2 | 34 (9.0) | 7 (14.9) | 27 (8.3) | 30 (10.3) | 4 (4.7) |
| Incorrect | 342 (81.0) | 40 (85.1) | 302 (91.8) | 261 (89.7) | 81 (95.3) |
| p-value 1 | 0.1683 | 0.1346 | |||
| Interaction between EDTA and NaOCl | |||||
| Correct | 87 (23.1) | 14 (29.8) | 73 (22.2) | 71 (24.4) | 16 (18.8) |
| Incorrect | 289 (76.9) | 33 (70.2) | 256 (77.8) | 220 (75.6) | 69 (81.2) |
| p-value 1 | 0.2682 | 0.3096 | |||
| Interaction between EDTA and CHX | |||||
| Correct | 20 (5.3) | 4 (8.5) | 16 (4.9) | 14 (4.8) | 6 (7.1) |
| Incorrect | 309 (94.7) | 43 (91.5) | 313 (95.1) | 277 (95.2) | 79 (92.9) |
| p-value 1 | 0.295 | 0.4148 | |||
| Attitude | Total | Specialty | Clinic | ||
|---|---|---|---|---|---|
| Endodontists | General Practitioners | Private | Government-Funded | ||
| Score | |||||
| Mean (sd) | 12.8 (2.6) | 13.1 (2.8) | 12.8 (2.5) | 12.8 (2.5) | 13.0 (2.8) |
| Median (Q1; Q3) | 13 (11; 15) | 12 (11.5; 15) | 13 (11; 14) | 12 (11; 15) | 13 (11; 15) |
| Min, Max | 5, 20 | 8, 20 | 5, 20 | 6, 20 | 5, 20 |
| p-value 1 | W = 8139, p-value = 0.5555 | W = 12980, p-value = 0.4837 | |||
| Level, n (%) | |||||
| Negative | 64 (17.0) | 10 (21.3) | 54 (16.4) | 50 (17.2) | 14 (16.5) |
| Positive | 312 (83.0) | 37 (78.7) | 275 (83.6) | 241 (82.8) | 71 (83.5) |
| p-value 2 | 0.4089 | 1.0 | |||
| Item | Respondents’ Answers n (%) | ||||
|---|---|---|---|---|---|
| SA | A | N | D | SD | |
| NaOCl should be combined with CAs | 125 (33.2) | 86 (22.9) | 84 (22.3) | 49 (13.1) | 32 (8.5) |
| CAs weaken dentin structure | 56 (14.9) | 83 (22.1) | 98 (26.1) | 72 (19.1) | 67 (17.8) |
| CAs should be used only in sclerotized root canals | 40 (10.6) | 60 (16.0) | 66 (17.6) | 82 (21.8) | 128 (34.0) |
| CAs decrease the effect of NaOCl | 94 (25.0) | 76 (20.2) | 104 (27.6) | 42 (11.2) | 60 (16.0) |
| Practice | Total | Specialty | Clinic | ||
|---|---|---|---|---|---|
| Endodontists | General Practitioners | Private | Government-Funded | ||
| Mean (sd) | 5.1 (1.7) | 4.8 (1.2) | 4.3 (1.5) | 4.5 (1.4) | 4.0 (1.7) |
| Median (Q1; Q3) | 5 (5; 6) | 5 (4; 6) | 4 (4; 5) | 6 (4; 8) | 4 (3; 5) |
| Min, Max | 0, 8 | 0, 6 | 0, 8 | 0, 8 | 0, 6 |
| p-value 1 | 0.06536 | 0.1104 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mikheikina, A.; Novozhilova, N.; Polyakova, M.; Sokhova, I.; Mun, A.; Zaytsev, A.; Babina, K.; Makeeva, I. Knowledge, Attitude, and Practice towards Chelating Agents in Endodontic Treatment among Dental Practitioners. Dent. J. 2023, 11, 156. https://doi.org/10.3390/dj11070156
Mikheikina A, Novozhilova N, Polyakova M, Sokhova I, Mun A, Zaytsev A, Babina K, Makeeva I. Knowledge, Attitude, and Practice towards Chelating Agents in Endodontic Treatment among Dental Practitioners. Dentistry Journal. 2023; 11(7):156. https://doi.org/10.3390/dj11070156
Chicago/Turabian StyleMikheikina, Anna, Nina Novozhilova, Maria Polyakova, Inna Sokhova, Anastasia Mun, Alexandr Zaytsev, Ksenia Babina, and Irina Makeeva. 2023. "Knowledge, Attitude, and Practice towards Chelating Agents in Endodontic Treatment among Dental Practitioners" Dentistry Journal 11, no. 7: 156. https://doi.org/10.3390/dj11070156