Three-Dimensional Printed Tooth Model with Root Canal Ledge: A Novel Educational Tool for Endodontic Training
Abstract
:1. Introduction
2. Materials and Methods
2.1. Model Fabrication
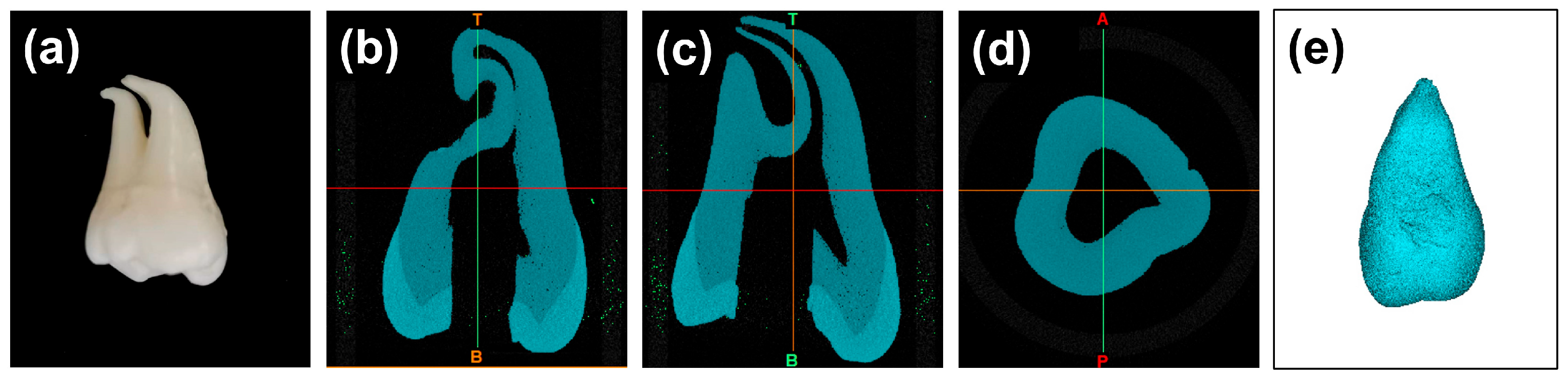
2.1.1. Tooth Preparation
2.1.2. Micro-Computed Tomography (μCT) Scanning
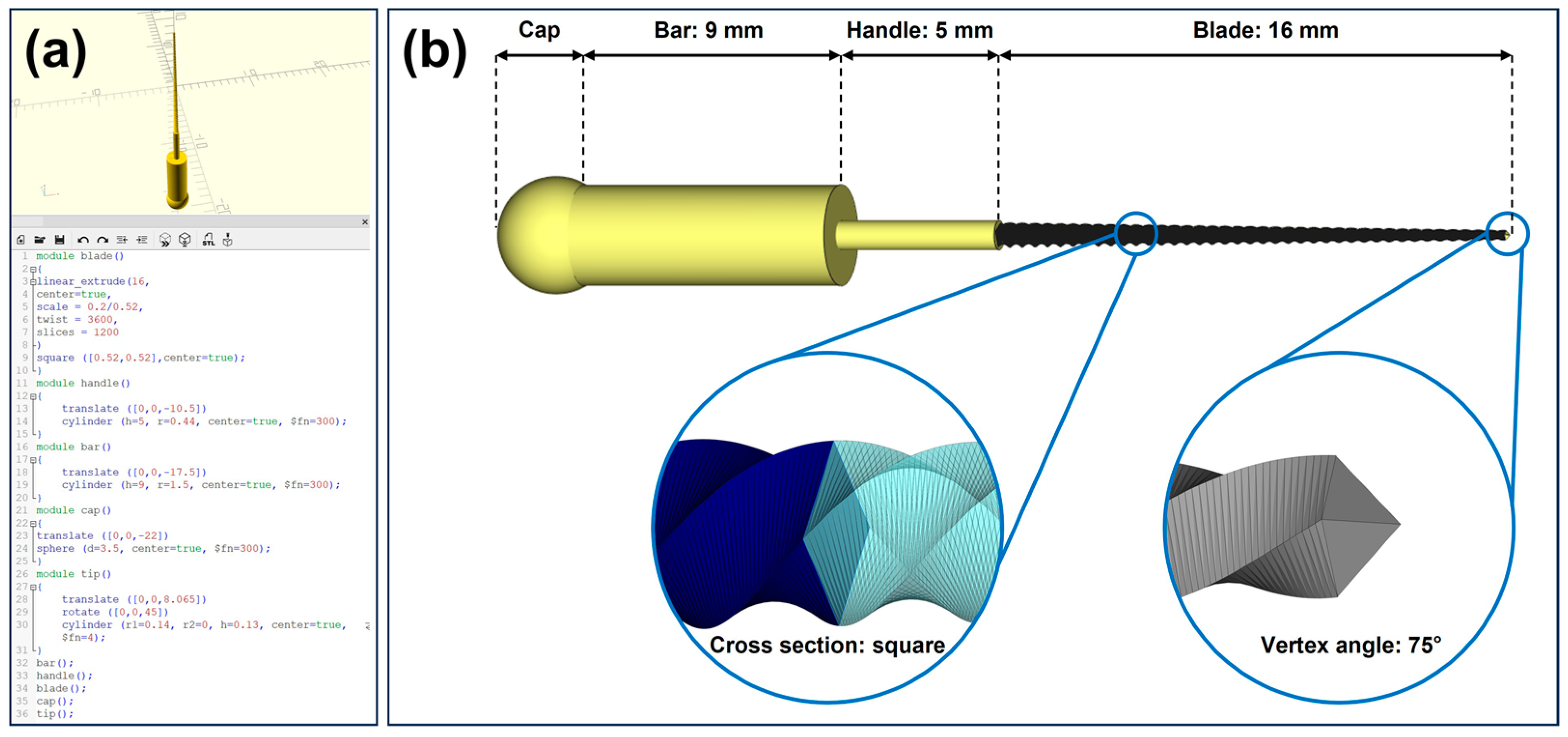
2.1.3. Computer-Aided Design (CAD) of K-File
2.1.4. CAD of the Tooth Model with Root Canal Ledge
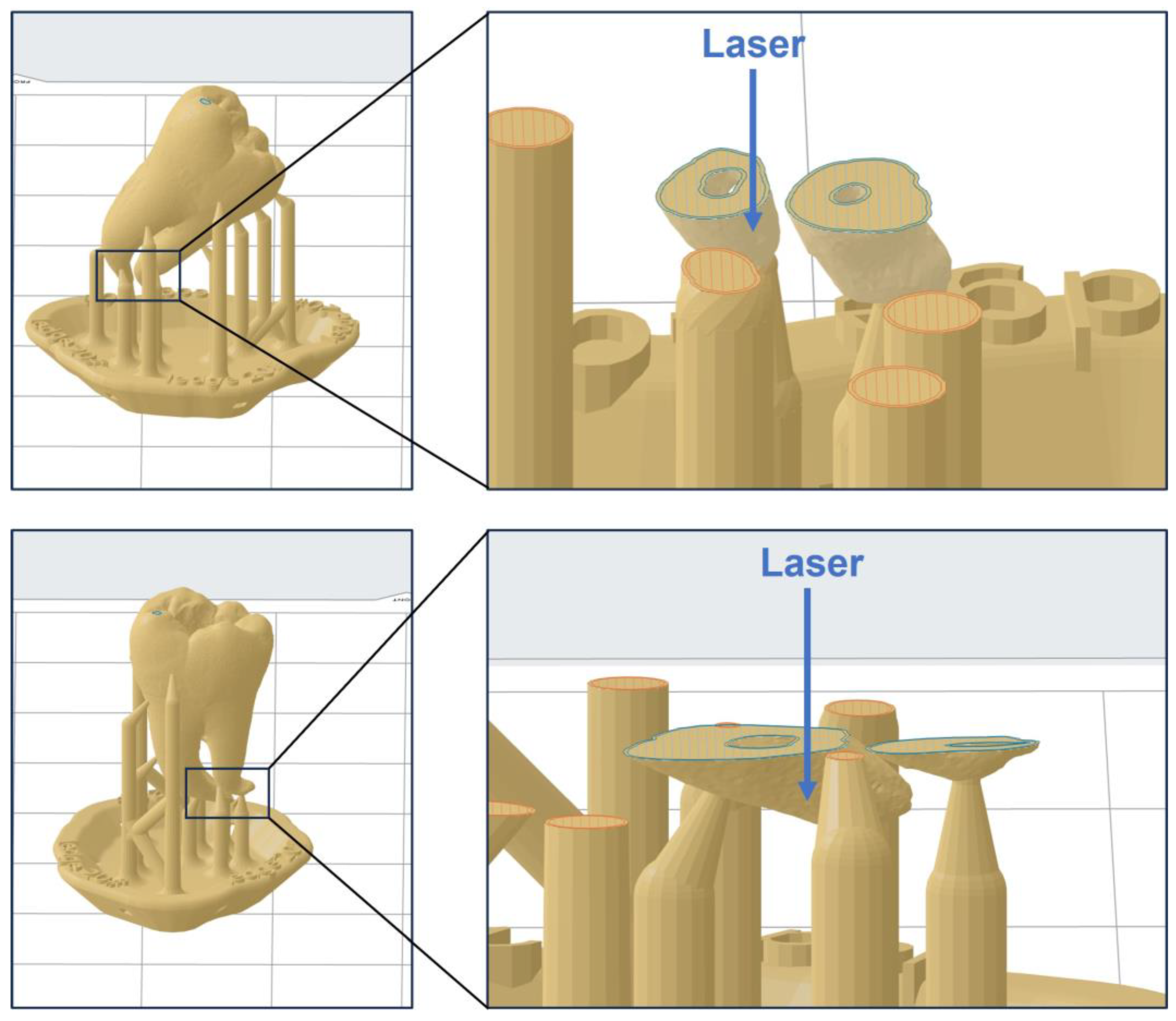
2.1.5. Additive Manufacturing
2.2. Model Evaluation
2.3. Statistical Analysis
3. Results
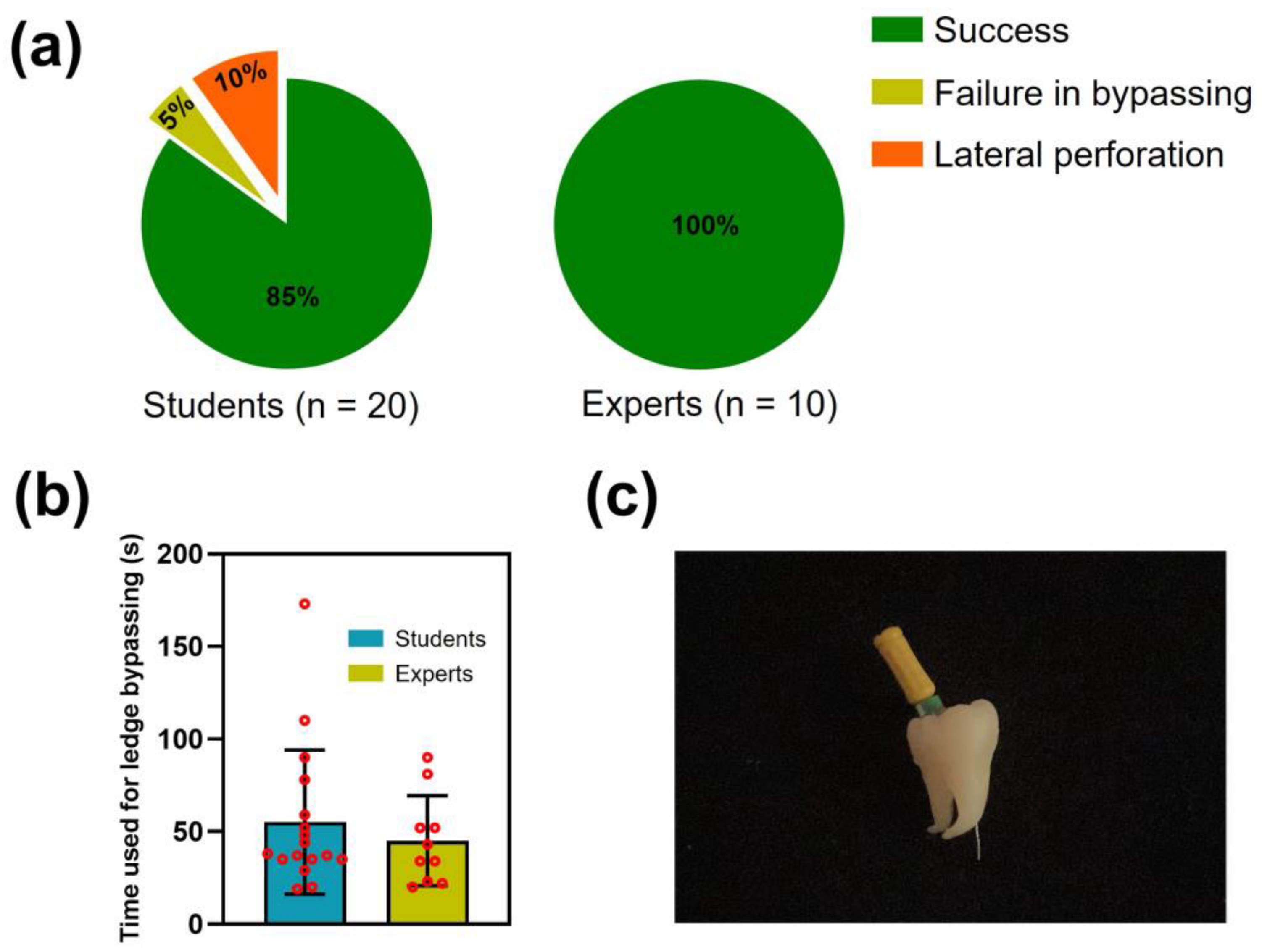
3.1. Three-Dimensional Printed Model for Endodontic Training
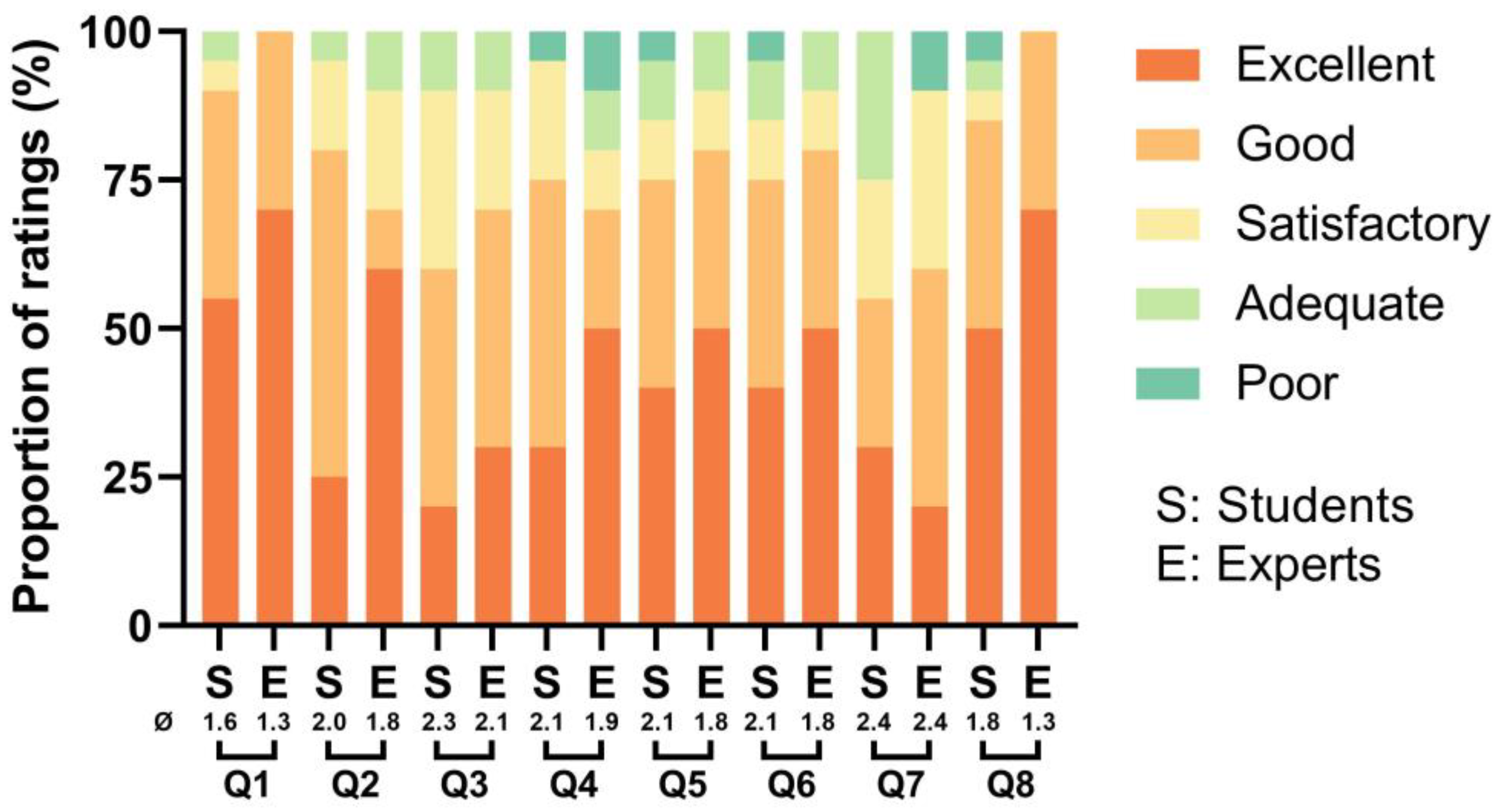
3.2. Evaluation of the Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Programming Code of a No. 20 K-File in OpenSCAD Software
module blade()
{
linear_extrude(16,
center=true,
scale=0.2/0.52,
twist=3600,
slices=1200
)
square ([0.52,0.52], center=true);
}
module handle()
{
translate ([0,0,-10.5])
cylinder (h=5, r=0.44, center=true, $fn=300);
}
module bar()
{
translate ([0,0,-17.5])
cylinder (h=9, r=1.5, center=true, $fn=300);
}
module cap()
{
translate ([0,0,-22])
sphere (d=3.5, center=true, $fn=300);
}
module tip()
{
translate ([0,0,8.065])
rotate ([0,0,45])
cylinder (r1=0.14, r2=0, h=0.13, center=true, $fn=4);
}
bar();
handle();
blade();
cap();
tip();
References
- Çelik, G.; Özdemir Kısacık, F.; Yılmaz, E.F.; Mersinlioğlu, A.; Ertuğrul, İ.F.; Orhan, H. A Comparative Study of Root Canal Shaping Using Protaper Universal and Protaper next Rotary Files in Preclinical Dental Education. PeerJ 2019, 7, e7419. [Google Scholar] [CrossRef] [PubMed]
- Hamid, H.R.; Gluskin, A.H.; Peters, O.A.; Peters, C.I. Rotary Versus Reciprocation Root Canal Preparation: Initial Clinical Quality Assessment in a Novice Clinician Cohort. J. Endod. 2018, 44, 1257–1262. [Google Scholar] [CrossRef] [PubMed]
- Jafarzadeh, H.; Abbott, P.V. Ledge Formation: Review of a Great Challenge in Endodontics. J. Endod. 2007, 33, 1155–1162. [Google Scholar] [CrossRef]
- Berutti, E.; Alovisi, M.; Moccia, E.; Carossa, M.; De Caro, G.; Roccuzzo, A.; Pasqualini, D.; Scotti, N. Micro-Computed Tomographic Evaluation of Endodontic Ledge Position in Relation to Canal Curvatures. BMC Oral Health 2022, 22, 1–6. [Google Scholar] [CrossRef]
- Greene, K.J.; Krell, K.V. Clinical Factors Associated with Ledged Canals in Maxillary and Mandibular Molars. Oral Surg. Oral Med. Oral Pathol. 1990, 70, 490–497. [Google Scholar] [CrossRef]
- Friedman, S.; Abitbol, S.; Lawrence, H.P. Treatment Outcome in Endodontics: The Toronto Study. Phase 1: Initial Treatment. J. Endod. 2003, 29, 787–793. [Google Scholar] [CrossRef]
- de Chevigny, C.; Dao, T.T.; Basrani, B.R.; Marquis, V.; Farzaneh, M.; Abitbol, S.; Friedman, S. Treatment Outcome in Endodontics: The Toronto Study--Phase 4: Initial Treatment. J. Endod. 2008, 34, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Hargreaves, K.M.; Cohen, S.; Berman, L.H. (Eds.) Cohen’s Pathways of the Pulp, 10th ed.; Elsevier: St. Louis, Mo, USA, 2011; pp. 733–737. [Google Scholar]
- Kapalas, A.; Lambrianidis, T. Factors Associated with Root Canal Ledging during Instrumentation. Dent. Traumatol. 2000, 16, 229–231. [Google Scholar] [CrossRef]
- van Noort, R. The Future of Dental Devices Is Digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Xu, Y.; Xepapadeas, A.B.; Koos, B.; Geis-Gerstorfer, J.; Li, P.; Spintzyk, S. Effect of Post-Rinsing Time on the Mechanical Strength and Cytotoxicity of a 3D Printed Orthodontic Splint Material. Dent. Mater. 2021, 37, e314–e327. [Google Scholar] [CrossRef]
- Xu, Y.; Huang, H.; Wu, M.; Tian, Y.; Wan, Q.; Shi, B.; Hu, T.; Spintzyk, S. Rapid Additive Manufacturing of a Superlight Obturator for Large Oronasal Fistula in Pediatric Patient. Laryngoscope 2022, 133, 1507–1512. [Google Scholar] [CrossRef] [PubMed]
- Hanisch, M.; Kroeger, E.; Dekiff, M.; Timme, M.; Kleinheinz, J.; Dirksen, D. 3D-Printed Surgical Training Model Based on Real Patient Situations for Dental Education. Int J. Environ. Res. Public Health 2020, 17, 2901. [Google Scholar] [CrossRef] [PubMed]
- Höhne, C.; Schwarzbauer, R.; Schmitter, M. 3D Printed Teeth with Enamel and Dentin Layer for Educating Dental Students in Crown Preparation. J. Dent. Educ 2019, 83, 1457–1463. [Google Scholar] [CrossRef] [PubMed]
- Höhne, C.; Schmitter, M. 3D Printed Teeth for the Preclinical Education of Dental Students. J. Dent. Educ 2019, 83, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Louangrath, P. Minimum Sample Size Method Based on Survey Scales. Int. J. Res. Methodol. Soc. Sci 2017, 3, 44–52. [Google Scholar] [CrossRef]
- Decurcio, D.A.; Lim, E.; Chaves, G.S.; Nagendrababu, V.; Estrela, C.; Rossi-Fedele, G. Pre-Clinical Endodontic Education Outcomes between Artificial versus Extracted Natural Teeth: A Systematic Review. Int. Endod. J. 2019, 52, 1153–1161. [Google Scholar] [CrossRef]
- Tchorz, J.P.; Brandl, M.; Ganter, P.A.; Karygianni, L.; Polydorou, O.; Vach, K.; Hellwig, E.; Altenburger, M.J. Pre-clinical endodontic training with artificial instead of extracted human teeth: does the type of exercise have an influence on clinical endodontic outcomes? Int. Endod. 2014, 48, 888–893. [Google Scholar] [CrossRef]
- Pouhaër, M.; Picart, G.; Baya, D.; Michelutti, P.; Dautel, A.; Pérard, M.; Le Clerc, J. Design of 3D-printed Macro-models for Undergraduates’ Preclinical Practice of Endodontic Access Cavities. Eur. J. Dent. Educ. 2022, 26, 347–353. [Google Scholar] [CrossRef]
- Ballester, B.; Pilliol, V.; Allaerd, P.; Jacquot, B.; Guivarc’h, M. Evaluation of a New 3D-Printed Tooth Model Allowing Preoperative ICDAS Assessment and Caries Removal. Eur. J. Dent. Educ 2023. [Google Scholar] [CrossRef]
- Reymus, M.; Fotiadou, C.; Kessler, A.; Heck, K.; Hickel, R.; Diegritz, C. 3D Printed Replicas for Endodontic Education. Int. Endod. J. 2019, 52, 123–130. [Google Scholar] [CrossRef]
- Anderson, J.; Wealleans, J.; Ray, J. Endodontic Applications of 3D Printing. Int. Endod. J. 2018, 51, 1005–1018. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Németh, A.; Vitai, V.; Czumbel, M.L.; Szabó, B.; Varga, G.; Kerémi, B.; Hegyi, P.; Hermann, P.; Borbély, J. Clear Guidance to Select the Most Accurate Technologies for 3D Printing Dental Models—A Network Meta-Analysis. J. Dent. 2023, 134, 104532. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.S. Novel Method for Structured Light System Calibration. Opt. Eng. 2006, 45, 083601. [Google Scholar] [CrossRef]
- Wyant, J.C. White Light Interferometry. In Proceedings of the SPIE, Orlando, FL, USA, 9 July 2002. [Google Scholar] [CrossRef]
- Dizon, J.R.C.; Espera, A.H.; Chen, Q.; Advincula, R.C. Mechanical Characterization of 3D-Printed Polymers. Addit. Manuf. 2018, 20, 44–67. [Google Scholar] [CrossRef]




| Category | Item Number | Content |
|---|---|---|
| Model quality | Q1 | The realism of the 3D printed model in simulating the anatomical structure of natural teeth. |
| Q2 | The realism of the 3D printed model in simulating root canal ledges. | |
| Q3 | The realism of the 3D printed model in simulating the material texture of natural teeth. | |
| Educational effect | Q4 | The extent to which practicing with the 3D printed model aids in recognizing root canal ledges. |
| Q5 | The extent to which practicing with the 3D printed model aids in bypassing root canal ledges. | |
| Q6 | The extent to which practicing with the 3D printed model aids in correcting root canal ledges. | |
| Q7 | The extent to which practicing with the 3D printed model aids in managing ledges to avoid lateral perforation. | |
| Q8 | The degree of potential educational effect of applying the 3D printed model in future endodontic training. |
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | |
|---|---|---|---|---|---|---|---|---|
| p-value 1 | 0.40 | 0.36 | 0.57 | 0.64 | 0.64 | 0.64 | 0.99 | 0.26 |
| S/E 2 | 328/137 | 330/135 | 323/142 | 321/144 | 321.5/143.5 | 321.5/143.5 | 311/154 | 334.5/130.5 |
| U statistic | 82 | 80 | 87 | 89 | 88.5 | 88.5 | 99 | 75.5 |
| Manufacturer | City/Country | Product No. | Model Type | Training Purpose |
|---|---|---|---|---|
| VDW GmbH | Munich/Germany | V040247000000 | Resin teeth and resin blocks | Root canal preparation and electronic length determination |
| Navadha | Mumbai/India | ADC07-3 | Resin teeth | Access cavity preparation, root canal preparation, and root canal filling |
| NISSIN DENTAL PRODUCTS INC. | Kyoto/Japan | S/E/B Series | Resin teeth and resin blocks | Access cavity preparation, root canal length measurement, root canal preparation, and root canal filling |
| Rogin Medical Co., Ltd. | Shenzhen/China | R38-0896 | Resin blocks | Root canal preparation and root canal irrigation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, R.; Tang, R.; Spintzyk, S.; Tian, Y.; Xiang, Y.; Xu, Y.; Hu, T. Three-Dimensional Printed Tooth Model with Root Canal Ledge: A Novel Educational Tool for Endodontic Training. Dent. J. 2023, 11, 213. https://doi.org/10.3390/dj11090213
Zhang R, Tang R, Spintzyk S, Tian Y, Xiang Y, Xu Y, Hu T. Three-Dimensional Printed Tooth Model with Root Canal Ledge: A Novel Educational Tool for Endodontic Training. Dentistry Journal. 2023; 11(9):213. https://doi.org/10.3390/dj11090213
Chicago/Turabian StyleZhang, Rui, Renjie Tang, Sebastian Spintzyk, Yuting Tian, Yong Xiang, Yichen Xu, and Tao Hu. 2023. "Three-Dimensional Printed Tooth Model with Root Canal Ledge: A Novel Educational Tool for Endodontic Training" Dentistry Journal 11, no. 9: 213. https://doi.org/10.3390/dj11090213







