Comparison between Shear Bond Strength of Er:YAG and Er,Cr:YSGG Lasers-Assisted Dentinal Adhesion of Self-Adhering Resin Composite: An Ex Vivo Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Teeth Collection and Storage
2.2. Specimen Preparation
2.3. Mechanical Shear Stress
- Score 1: All of the adhesives remained on the tooth.
- Score 2: More than 90% of the adhesives remained on the tooth.
- Score 3: 10–90% of the adhesives remained on the tooth.
- Score 4: Less than 10% of the adhesives remained on the tooth.
- Score 5: No adhesive remained on the tooth.
2.4. Statistical Analysis
3. Results
3.1. Shear Bond Strength Test
3.2. Stereomicroscopic Analysis
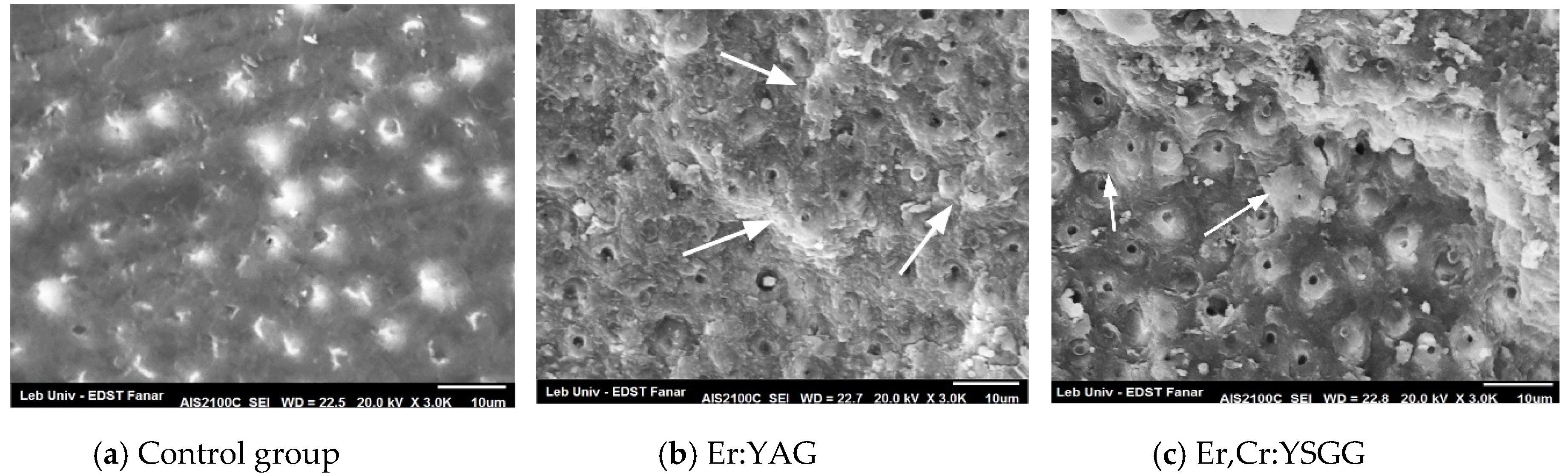
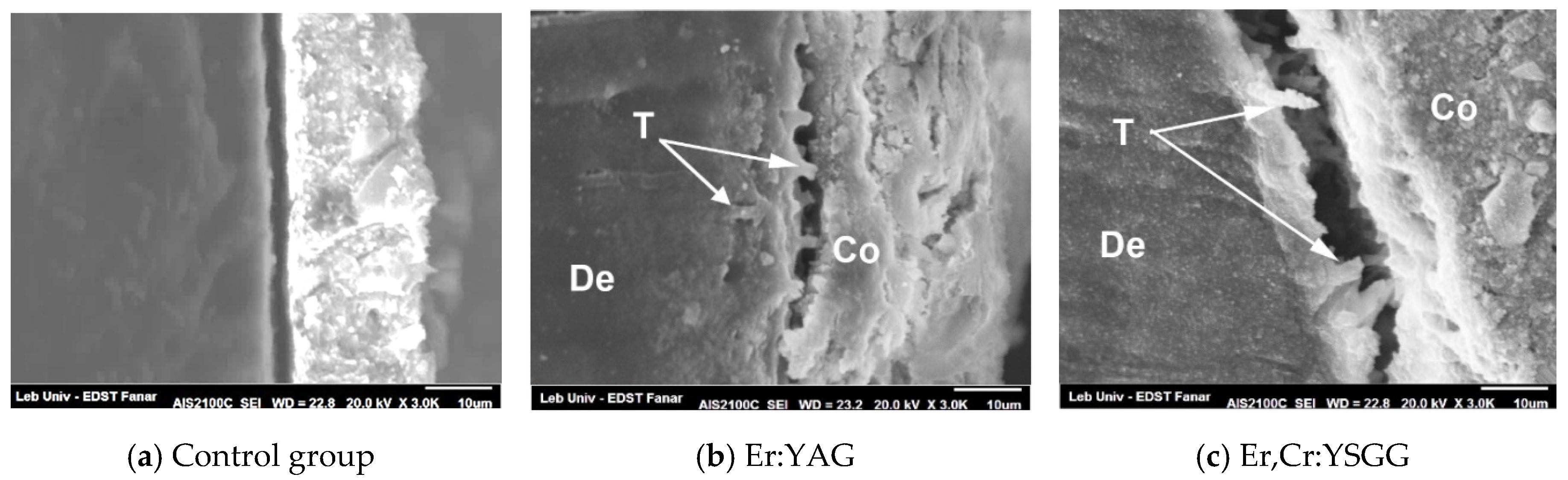
3.3. SEM Topographical Observation
4. Discussion
4.1. Stereomicroscopic Observation
4.2. SEM Observation
4.3. Perspective
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Peumans, M.; De Munck, J.; Van Landuyt, K.L.; Poitevin, A.; Lambrechts, P.; Van Meerbeek, B. A 13-year clinical evaluation of two three-step etch-and-rinse adhesives in non-carious class-V lesions. Clin. Oral Investig. 2012, 16, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Memarpour, M.; Shafiei, F.; Razmjoei, F.; Kianimanesh, N. Effect of laser preparation on adhesion of a self-adhesive flowable composite resin to primary teeth. Microsc. Res. Tech. 2016, 79, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Rahimian-Imam, S.; Ramazani, N.; Fayazi, M.R. Marginal Microleakage of Conventional Fissure Sealants and Self-Adhering Flowable Composite as Fissure Sealant in Permanent Teeth. J. Dent. 2015, 12, 430–435. [Google Scholar]
- Sachdeva, P.; Goswami, M.; Singh, D. Comparative evaluation of shear bond strength and nanoleakage of conventional and self-adhering flowable composites to primary teeth dentin. Contemp. Clin. Dent. 2016, 7, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Tuloglu, N.; Sen Tunc, E.; Ozer, S.; Bayrak, S. Shear bond strength of self-adhering flowable composite on dentin with and without application of an adhesive system. J. Appl. Biomater. Funct. Mater. 2014, 12, 97–101. [Google Scholar] [CrossRef]
- Koliniotou-Koumpia, E.; Kouros, P.; Zafiriadis, L.; Koumpia, E.; Dionysopoulos, P.; Karagiannis, V. Bonding of adhesives to Er:YAG laser-treated dentin. Eur. J. Dent. 2012, 6, 16–23. [Google Scholar] [CrossRef] [Green Version]
- Ayar, M.K.; Yildirim, T.; Yesilyurt, C. Effects of Er,Cr:YSGG laser parameters on dentin bond strength and interface morphology. Microsc. Res. Tech. 2015, 78, 1104–1111. [Google Scholar] [CrossRef]
- Altunsoy, M.; Botsali, M.S.; Sari, T.; Onat, H. Effect of different surface treatments on the microtensile bond strength of two self-adhesive flowable composites. Lasers Med. Sci. 2015, 30, 1667–1673. [Google Scholar] [CrossRef]
- Ozel Bektas, O.; Eren, D.; Herguner Siso, S.; Akin, G.E. Effect of thermocycling on the bond strength of composite resin to bur and laser treated composite resin. Lasers Med. Sci. 2012, 27, 723–728. [Google Scholar] [CrossRef]
- Eren, D.; Dogan, C.A.; Bektas, O.O. Effect of Different Surface Treatments and Roughness on the Repair Bond Strength of Aged Nanohybrid Composite. Photobiomodulation Photomed. Laser Surg. 2019, 37, 473–482. [Google Scholar] [CrossRef]
- Karadas, M.; Caglar, I. The effect of Er:YAG laser irradiation on the bond stability of self-etch adhesives at different dentin depths. Lasers Med. Sci. 2017, 32, 967–974. [Google Scholar] [CrossRef] [Green Version]
- Erdemir, U.; Sancakli, H.S.; Sancakli, E.; Eren, M.M.; Ozel, S.; Yucel, T.; Yildiz, E. Shear bond strength of a new self-adhering flowable composite resin for lithium disilicate-reinforced CAD/CAM ceramic material. J. Adv. Prosthodont. 2014, 6, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Park, K.J.; Schneider, H.; Haak, R. Assessment of defects at tooth/self-adhering flowable composite interface using swept-source optical coherence tomography (SS-OCT). Dent. Mater. Off. Publ. Acad. Dent. Mater. 2015, 31, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Veli, I.; Akin, M.; Kucukyilmaz, E.; Uysal, T. Shear bond strength of a self-adhering flowable composite when used for lingual retainer bonding. J. Orofac. Orthop. Fortschritte der Kieferorthopadie Organ/Official Journal Deutsche Gesellschaft fur Kieferorthopadie 2014, 75, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Li, M.; Guo, B.; Gao, Y.; Liu, H.; Li, J. Evaluation of Microtensile Bond Strength and Microleakage of a Self-adhering Flowable Composite. J. Adhes. Dent. 2015, 17, 535–543. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Margvelashvili, M.; Goracci, C.; Papacchini, F.; Ferrari, M. Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorations. Clin. Oral Investig. 2013, 17, 1497–1506. [Google Scholar] [CrossRef] [PubMed]
- Shafiei, F.; Saadat, M. Micromorphology and bond strength evaluation of adhesive interface of a self-adhering flowable composite resin-dentin: Effect of surface treatment. Microsc. Res. Tech. 2016, 79, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Chou, J.C.; Ding, S.J.; Chen, C.C. Dentin surface modification using the Er,Cr:YSGG laser and a meshwork mask: Light and SEM microscopic observations. Photomed. Laser Surg. 2011, 29, 433–435. [Google Scholar] [CrossRef]
- Lin, S.; Pan, D.; Lin, Q.; Yin, S.; Chen, D.; Liu, Q.; Yu, L.; Lin, Z. Evaluation of phase, microstructure and composition of human dentine after Er,Cr:YSGG laser irradiation. J. Nanosci. Nanotechnol. 2011, 11, 2421–2426. [Google Scholar] [CrossRef]
- Nahas, P.; Zeinoun, T.; Majzoub, Z.; Corbani, K.; Nammour, S. The Effect of Energy Densities on the Shear Bond Strength of Self-Adhering Flowable Composite to Er:YAG Pretreated Dentin. BioMed Res. Int. 2016, 2016, 6507924. [Google Scholar] [CrossRef] [Green Version]
- Shahabi, S.; Chiniforush, N.; Bahramian, H.; Monzavi, A.; Baghalian, A.; Kharazifard, M.J. The effect of erbium family laser on tensile bond strength of composite to dentin in comparison with conventional method. Lasers Med. Sci. 2013, 28, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Ayar, M.K.; Erdermir, F. Bonding strength of universal adhesives to Er,Cr:YSGG Laser-Irradiated Dentin. Niger. J. Clin. Pract. 2018, 21, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Ostby, A.W.; Bishara, S.E.; Denehy, G.E.; Laffoon, J.F.; Warren, J.J. Effect of self-etchant pH on the shear bond strength of orthodontic brackets. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2008, 134, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Poitevin, A.; De Munck, J.; Van Ende, A.; Suyama, Y.; Mine, A.; Peumans, M.; Van Meerbeek, B. Bonding effectiveness of self-adhesive composites to dentin and enamel. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2013, 29, 221–230. [Google Scholar] [CrossRef]
- Jordehi, A.Y.; Shahabi, M.S.; Akbari, A. Comparison of self-adhering flowable composite microleakage with several types of bonding agent in class V cavity restoration. Dent. Res. J. 2019, 16, 257–263. [Google Scholar]
- Fu, J.; Kakuda, S.; Pan, F.; Hoshika, S.; Ting, S.; Fukuoka, A.; Bao, Y.; Ikeda, T.; Nakaoki, Y.; Selimovic, D.; et al. Bonding performance of a newly developed step-less all-in-one system on dentin. Dent. Mater. J. 2013, 32, 203–211. [Google Scholar] [CrossRef] [Green Version]
- Van Landuyt, K.L.; Mine, A.; De Munck, J.; Jaecques, S.; Peumans, M.; Lambrechts, P.; Van Meerbeek, B. Are one-step adhesives easier to use and better performing? Multifactorial assessment of contemporary one-step self-etching adhesives. J. Adhes. Dent. 2009, 11, 175–190. [Google Scholar] [PubMed]
- Ribeiro, C.F.; Goncalves, S.E.; Yui, K.C.; Borges, A.B.; Barcellos, D.C.; Brayner, R. Dentin bond strength: Influence of Er:YAG and Nd:YAG lasers. Int. J. Periodontics Restor. Dent. 2013, 33, 373–377. [Google Scholar] [CrossRef] [Green Version]
- Yazici, A.R.; Agarwal, I.; Campillo-Funollet, M.; Munoz-Viveros, C.; Antonson, S.A.; Antonson, D.E.; Mang, T. Effect of laser preparation on bond strength of a self-adhesive flowable resin. Lasers Med. Sci. 2013, 28, 343–347. [Google Scholar] [CrossRef]
- Moretto, S.G.; Azambuja, N., Jr.; Arana-Chavez, V.E.; Reis, A.F.; Giannini, M.; Eduardo Cde, P.; De Freitas, P.M. Effects of ultramorphological changes on adhesion to lased dentin-Scanning electron microscopy and transmission electron microscopy analysis. Microsc. Res. Tech. 2011, 74, 720–726. [Google Scholar] [CrossRef] [PubMed]
- El-Araby, A.M.; Talic, Y.F. The effect of thermocycling on the adhesion of self-etching adhesives on dental enamel and dentin. J. Contemp. Dent. Pract. 2007, 8, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.S.; Li, M.T.; Huang, F.M.; Ding, S.J. The effect of thermocycling and dentine pre-treatment on the durability of the bond between composite resin and dentine. J. Oral Rehabil. 2004, 31, 492–499. [Google Scholar] [CrossRef]
- Kawazu, M.; Takamizawa, T. Comparison of dentin bond durability of a universal adhesive and two etch-and-rinse adhesive systems. Clin. Oral Investig. 2019. [Google Scholar] [CrossRef] [PubMed]
- Delme, K.I.; Deman, P.J.; De Moor, R.J. Microleakage of class V resin composite restorations after conventional and Er:YAG laser preparation. J. Oral Rehabil. 2005, 32, 676–685. [Google Scholar] [CrossRef] [PubMed]
- Saraceni, C.H.; Liberti, E.; Navarro, R.S.; Cassoni, A.; Kodama, R.; Oda, M. Er:YAG-laser and sodium hypochlorite influence on bond to dentin. Microsc. Res. Tech. 2013, 76, 72–78. [Google Scholar] [CrossRef]
- Juloski, J.; Goracci, C.; Rengo, C.; Giovannetti, A.; Vichi, A.; Vulicevic, Z.R.; Ferrari, M. Enamel and dentin bond strength of new simplified adhesive materials with and without preliminary phosphoric acid-etching. Am. J. Dent. 2012, 25, 239–243. [Google Scholar]
- Saberi, S.; Seyed Jabbari Doshanlo, S.; Bagheri, H.; Mir Mohammad Rezaei, S.; Shahabi, S. Evaluation of Tooth Surface Irradiated With Erbium: Yttrium Aluminum Garnet and Carbon Dioxide Lasers by Atomic Force Microscopy. J. Lasers Med. Sci. 2018, 9, 188–193. [Google Scholar] [CrossRef]
- Sharafeddin, F.; Salehi, R.; Feizi, N. Effect of Dimethyl Sulfoxide on Bond Strength of a Self-Etch Primer and an Etch and Rinse Adhesive to Surface and Deep Dentin. J. Dent. 2016, 17, 242–249. [Google Scholar]
- Matsumoto, K.; Hossain, M.; Tsuzuki, N.; Yamada, Y. Morphological and compositional changes of human dentin after Er:YAG laser irradiation. J. Oral Laser Appl. 2003, 3, 15–19. [Google Scholar]
- Ekworapoj, P.; Sidhu, S.K.; McCabe, J.F. Effect of different power parameters of Er,Cr:YSGG laser on human dentine. Lasers Med. Sci. 2007, 22, 175–182. [Google Scholar] [CrossRef]
- Sarr, M.; Kane, A.W.; Vreven, J.; Mine, A.; Van Landuyt, K.L.; Peumans, M.; Lambrechts, P.; Van Meerbeek, B.; De Munck, J. Microtensile bond strength and interfacial characterization of 11 contemporary adhesives bonded to bur-cut dentin. Oper. Dent. 2010, 35, 94–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ritter, A.V.; Swift, E.J., Jr.; Heymann, H.O.; Sturdevant, J.R.; Wilder, A.D., Jr. An eight-year clinical evaluation of filled and unfilled one-bottle dental adhesives. J. Am. Dent. Assoc. (1939) 2009, 140, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, M.V.; de Almeida Neves, A.; Mine, A.; Coutinho, E.; Van Landuyt, K.; De Munck, J.; Van Meerbeek, B. Current aspects on bonding effectiveness and stability in adhesive dentistry. Aust. Dent. J. 2011, 56 (Suppl. 1), 31–44. [Google Scholar] [CrossRef]
- Taşar, S.; Ulusoy, M.M.; Merıç, G. Microshear bond strength according to dentin cleansing methods before recementation. J. Adv. Prosthodont. 2014, 6, 79–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Storage Mode | Studied Groups | Mean ± SD | Std. Errors of Mean |
|---|---|---|---|
| WS | Group 1 | 8.355 ± 2.297 A | 0.6926 |
| Group 2 | 13.10 ± 1.291 B | 0.3727 | |
| Group 3 | 14.04 ± 5.233 B | 1.511 | |
| TC | Group 1 | 2.75 ± 1.583 C | 0.4570 |
| Group 2 | 10.03 ± 1.503 A | 0.4339 | |
| Group 3 | 10.53 ± 2.631 A | 0.7595 |
| Studied Groups | Storage Mode | Failure Mode | ||||
|---|---|---|---|---|---|---|
| Score 1 (%) | Score 2 (%) | Score 3 (%) | Score 4 (%) | Score 5 (%) | ||
| Group 1 | WS 24 h | 0 (0%) | 0 (0%) | 2 (12.16%) | 4 (33.34%) | 6 (54.5%) |
| TC | 0 (0%) | 0 (0%) | 0 (0%) | 2 (16.67%) | 10 (83.33%) | |
| Group 2 | WS 24 h | 0 (0%) | 0 (0%) | 4 (32.19%) | 5 (41.66%) | 3 (26.15%) |
| TC | 0 (0%) | 0 (0%) | 2 (25.66%) | 4 (32.34%) | 6 (42%) | |
| Group 3 | WS 24 h | 0 (0%) | 0 (0%) | 4 (33.84%) | 5 (40.06%) | 3 (26.10%) |
| TC | 0 (0%) | 0 (0%) | 3 (24.96%) | 4 (31.34%) | 5 (43.70%) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nahas, P.; Nammour, S.; Gerges, E.; Zeinoun, T. Comparison between Shear Bond Strength of Er:YAG and Er,Cr:YSGG Lasers-Assisted Dentinal Adhesion of Self-Adhering Resin Composite: An Ex Vivo Study. Dent. J. 2020, 8, 66. https://doi.org/10.3390/dj8030066
Nahas P, Nammour S, Gerges E, Zeinoun T. Comparison between Shear Bond Strength of Er:YAG and Er,Cr:YSGG Lasers-Assisted Dentinal Adhesion of Self-Adhering Resin Composite: An Ex Vivo Study. Dentistry Journal. 2020; 8(3):66. https://doi.org/10.3390/dj8030066
Chicago/Turabian StyleNahas, Paul, Samir Nammour, Elie Gerges, and Toni Zeinoun. 2020. "Comparison between Shear Bond Strength of Er:YAG and Er,Cr:YSGG Lasers-Assisted Dentinal Adhesion of Self-Adhering Resin Composite: An Ex Vivo Study" Dentistry Journal 8, no. 3: 66. https://doi.org/10.3390/dj8030066






