Osteoconductivity of Bovine Xenograft Granules of Different Sizes in Sinus Lift: A Histomorphometric Study in Rabbits
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animal Sample
2.2. Randomization and Allocation Concealment
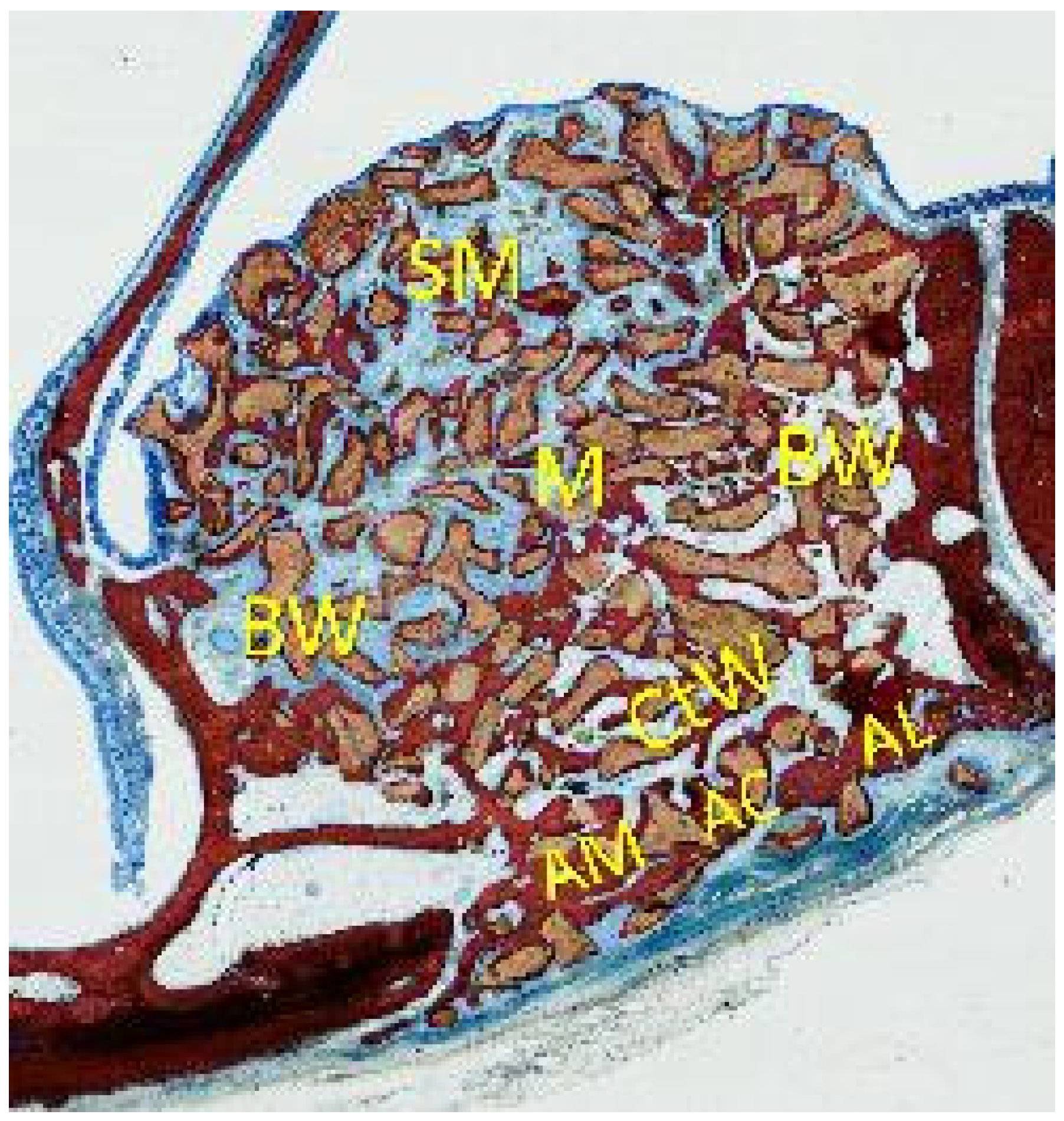
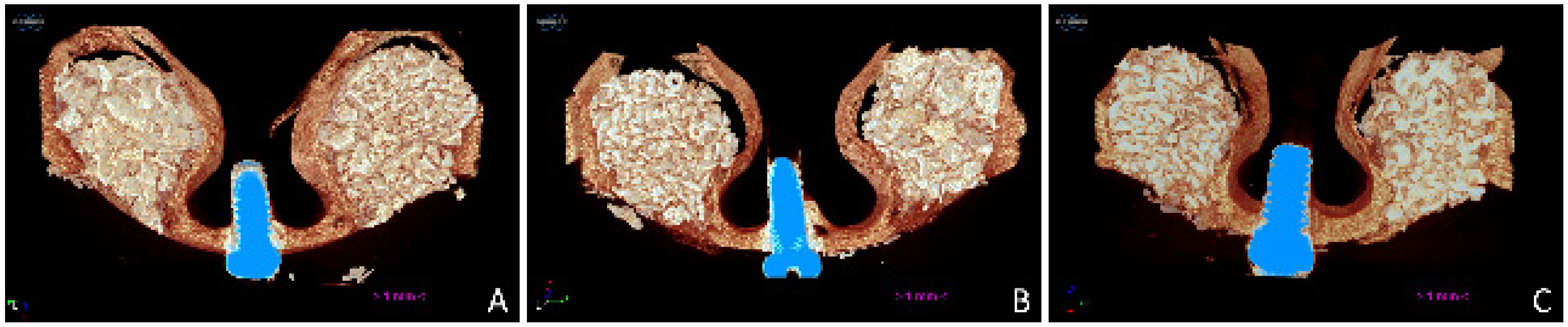
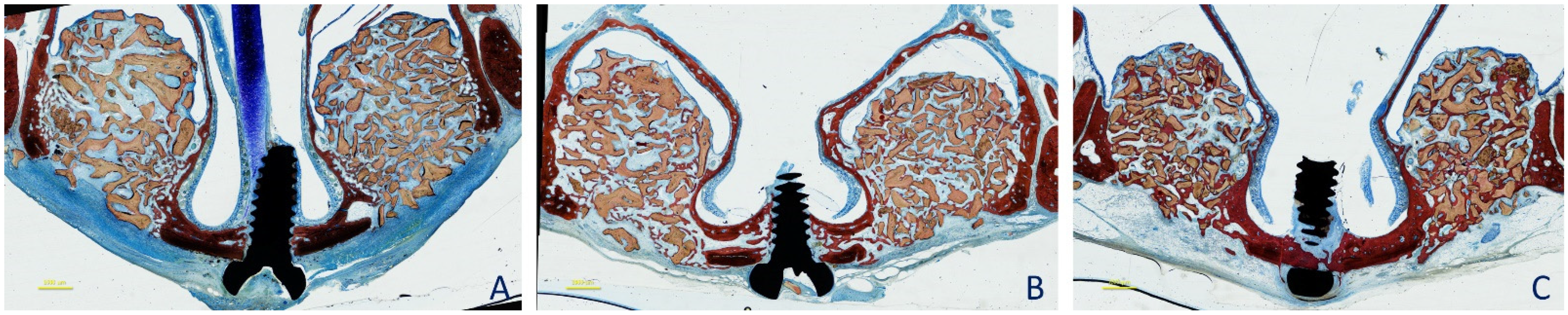
2.3. Surgical Procedures
2.4. Maintenance Care and Euthanasia
2.5. MicroCT Evaluations
2.6. Histological Preparation
2.7. Calibration for Histomorphometric Evaluations
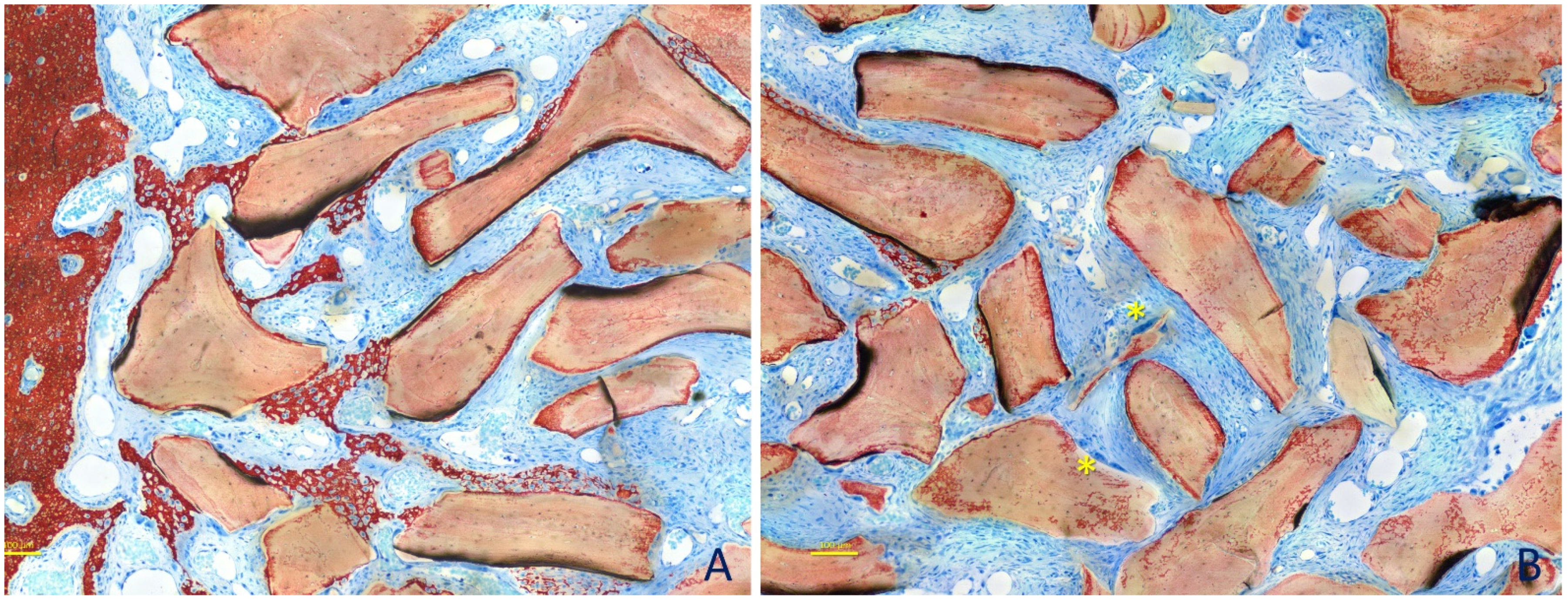
2.8. Histomorphometric Evaluations
2.9. Data Analysis
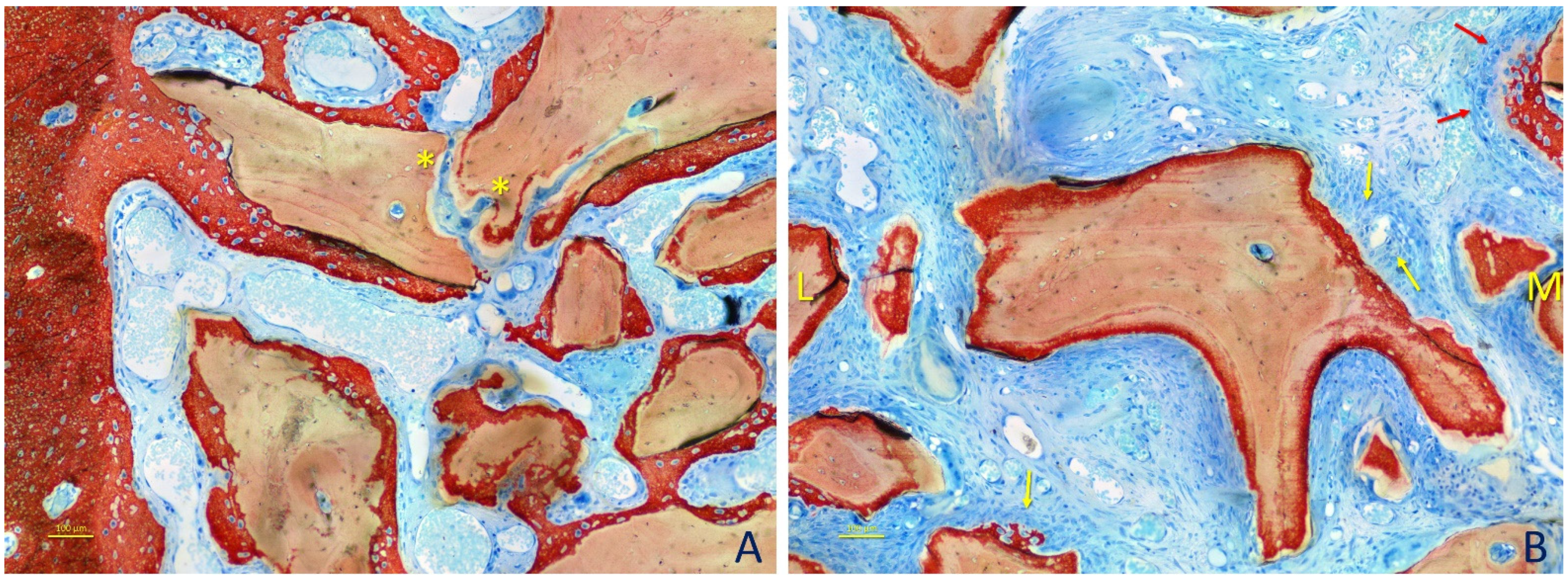
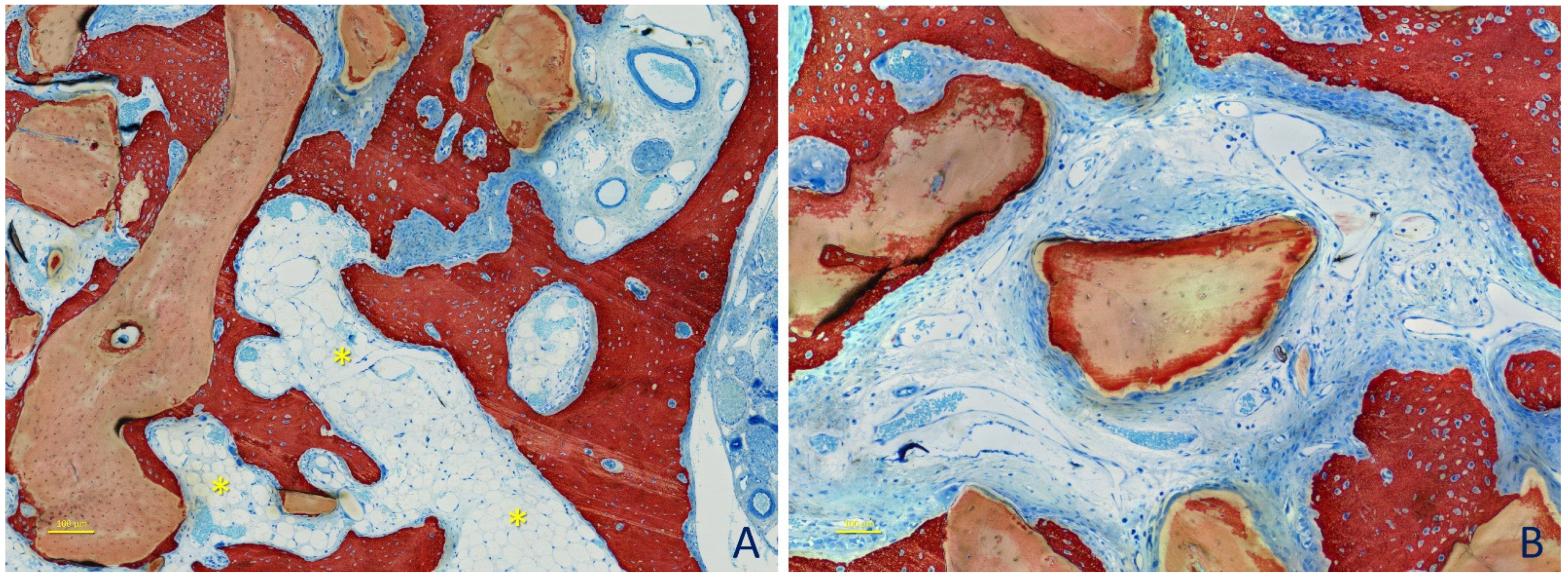
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Asai, S.; Shimizu, Y.; Ooya, K. Maxillary sinus augmentation model in rabbits: Effect of occluded nasal ostium on new bone formation. Clin. Oral Implant. Res. 2002, 13, 405–409. [Google Scholar] [CrossRef]
- Xu, H.; Shimizu, Y.; Asai, S.; Ooya, K. Grafting of deproteinized bone particles inhibits bone resorption after maxillary sinus floor elevation. Clin. Oral Implant. Res. 2004, 15, 126–133. [Google Scholar] [CrossRef]
- Xu, H.; Shimizu, Y.; Ooya, K. Histomorphometric study of the stability of newly formed bone after elevation of the floor of the maxillary sinus. Br. J. Oral Maxillofac. Surg. 2005, 43, 493–499. [Google Scholar] [CrossRef]
- Scala, A.; Botticelli, D.; Rangel, I.G., Jr.; de Oliveira, J.A.; Okamoto, R.; Lang, N.P. Early healing after elevation of the maxillary sinus floor applying a lateral access: A histological study in monkeys. Clin. Oral Implant. Res. 2010, 21, 1320–1326. [Google Scholar] [CrossRef] [PubMed]
- Scala, A.; Botticelli, D.; Faeda, R.S.; Garcia Rangel, I., Jr.; de Oliveira, J.A.; Lang, N.P. Lack of influence of the Schneiderian membrane in forming new bone apical to implants simultaneously installed with sinus floor elevation: An experimental study in monkeys. Clin. Oral Implant. Res. 2012, 23, 175–181. [Google Scholar] [CrossRef]
- Corbella, S.; Taschieri, S.; Weinstein, R.; Del Fabbro, M. Histomorphometric outcomes after lateral sinus floor elevation procedure: A systematic review of the literature and meta-analysis. Clin. Oral Implant. Res. 2016, 27, 1106–1122. [Google Scholar] [CrossRef] [PubMed]
- Cordaro, L.; Bosshardt, D.D.; Palattella, P.; Rao, W.; Serino, G.; Chiapasco, M. Maxillary sinus grafting with Bio-Oss or Straumann Bone Ceramic: Histomorphometric results from a randomized controlled multicenter clinical trial. Clin. Oral Implant. Res. 2008, 19, 796–803. [Google Scholar] [CrossRef]
- Testori, T.; Wallace, S.S.; Trisi, P.; Capelli, M.; Zuffetti, F.; Del Fabbro, M. Effect of xenograft (ABBM) particle size on vital bone formation following maxillary sinus augmentation: A multicenter, randomized, controlled, clinical histomorphometric trial. Int. J. Periodontics Restor. Dent. 2013, 33, 467–475. [Google Scholar] [CrossRef] [Green Version]
- Kawakami, S.; Lang, N.P.; Iida, T.; Ferri, M.; Apaza Alccayhuaman, K.A.; Botticelli, D. Influence of the position of the antrostomy in sinus floor elevation assessed with cone-beam computed tomography: A randomized clinical trial. J. Investig. Clin. Dent. 2018, 9, e12362. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, S.; Lang, N.P.; Ferri, M.; Apaza Alccayhuaman, K.A.; Botticelli, D. Influence of the height of the antrostomy in sinus floor elevation assessed by cone beam computed tomography—A randomized clinical trial. Int. J. Oral Maxillofac. Implant. 2019, 34, 223–232. [Google Scholar] [CrossRef]
- Caneva, M.; Lang, N.P.; Garcia Rangel, I.J.; Ferreira, S.; Caneva, M.; De Santis, E.; Botticelli, D. Sinus mucosa elevation using Bio-Oss® or Gingistat® collagen sponge: An experimental study in rabbits. Clin. Oral Implant. Res. 2017, 28, e21–e30. [Google Scholar] [CrossRef]
- Iida, T.; Carneiro Martins Neto, E.; Botticelli, D.; Apaza Alccayhuaman, K.A.; Lang, N.P.; Xavier, S.P. Influence of a collagen membrane positioned subjacent the sinus mucosa following the elevation of the maxillary sinus. A histomorphometric study in rabbits. Clin. Oral Implant. Res. 2017, 28, 1567–1576. [Google Scholar] [CrossRef] [PubMed]
- Omori, Y.; Ricardo Silva, E.; Botticelli, D.; Apaza Alccayhuaman, K.A.; Lang, N.P.; Xavier, S.P. Reposition of the bone plate over the antrostomy in maxillary sinus augmentation: A histomorphometric study in rabbits. Clin. Oral Implant. Res. 2018, 29, 821–834. [Google Scholar] [CrossRef] [PubMed]
- Masuda, K.; Silva, E.R.; Botticelli, D.; Apaza Alccayhuaman, K.A.; Xavier, S.P. Antrostomy preparation for maxillary sinus floor augmentation using drills or a sonic instrument: A microcomputed tomography and histomorphometric study in rabbits. Int. J. Oral Maxillofac. Implant. 2019, 34, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Shin, H.K.; Yun, J.H.; Cho, K.S. Randomized Clinical Trial of Maxillary Sinus Grafting using Deproteinized Porcine and Bovine Bone Mineral. Clin. Implant. Dent. Relat. Res. 2017, 19, 140–150. [Google Scholar] [CrossRef] [PubMed]
- De Molon, R.S.; Magalhaes-Tunes, F.S.; Semedo, C.V.; Furlan, R.G.; de Souza, L.G.L.; de Souza Faloni, A.P.; Marcantonio, E., Jr.; Faeda, R.S. A randomized clinical trial evaluating maxillary sinus augmentation with different particle sizes of demineralized bovine bone mineral: Histological and immunohistochemical analysis. Int. J. Oral Maxillofac. Surg. 2019, 48, 810–823. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.S.; Aaboe, M.; Janner, S.F.; Saulacic, N.; Bornstein, M.M.; Bosshardt, D.D.; Buser, D. Influence of particle size of deproteinized bovine bone mineral on new bone formation and implant stability after simultaneous sinus floor elevation: A histomorphometric study in minipigs. Clin. Implant. Dent. Relat. Res. 2015, 17, 274–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Santis, E.; Lang, N.P.; Ferreira, S.; Rangel Garcia, I., Jr.; Caneva, M.; Botticelli, D. Healing at implants installed concurrently to maxillary sinus floor elevation with Bio-Oss® or autologous bone grafts. A histo-morphometric study in rabbits. Clin. Oral Implant. Res. 2017, 28, 503–511. [Google Scholar] [CrossRef]
- Masuda, K.; Silva, E.R.; Apaza Alccayhuaman, K.A.; Botticelli, D.; Xavier, S.P. Histologic and micro-ct analyses at implants placed immediately after maxillary sinus elevation using large or small xenograft granules: An experimental study in rabbits. Int. J. Oral Maxillofac. Implant. 2020, 35, 739–748. [Google Scholar] [CrossRef]
- Hoang, T.N.; Mealey, B.L. Histologic comparison of healing after ridge preservation using human demineralized bone matrix putty with one versus two different-sized bone particles. J. Periodontol. 2012, 83, 174–181. [Google Scholar] [CrossRef]
- Dos Anjos, T.L.; de Molon, R.S.; Paim, P.R.; Marcantonio, E.; Marcantonio, E., Jr.; Faeda, R.S. Implant stability after sinus floor augmentation with deproteinized bovine bone mineral particles of different sizes: A prospective, randomized and controlled split-mouth clinical trial. Int. J. Oral Maxillofac. Surg. 2016, 45, 1556–1563. [Google Scholar] [CrossRef] [Green Version]
- Chackartchi, T.; Iezzi, G.; Goldstein, M.; Klinger, A.; Soskolne, A.; Piattelli, A.; Shapira, L. Sinus floor augmentation using large (1–2 mm) or small (0.25–1 mm) bovine bone mineral particles: A prospective, intra-individual controlled clinical, micro-computerized tomography and histomorphometric study. Clin. Oral Implant. Res. 2011, 22, 473–480. [Google Scholar] [CrossRef]
- Schroeder, H.E.; Münzel-Pedrazzoli, S. Correlated morphometric and biochemical analysis of gingival tissue. Morphometric model, tissue sampling and test of stereologic procedures. J. Microsc. 1973, 99, 301–329. [Google Scholar] [CrossRef]
- Botticelli, D.; Lang, N.P. Dynamics of osseointegration in various human and animal models—A comparative analysis. Clin. Oral Implant. Res. 2017, 28, 742–748. [Google Scholar] [CrossRef]
- Iida, T.; Baba, S.; Botticelli, D.; Masuda, K.; Xavier, S.P. Comparison of histomorphometry and microCT after sinus augmentation using xenografts of different particle sizes in rabbits. Oral Maxillofac. Surg. 2020, 24, 57–64. [Google Scholar] [CrossRef]
- Busenlechner, D.; Huber, C.D.; Vasak, C.; Dobsak, A.; Gruber, R.; Watzek, G. Sinus augmentation analysis revised: The gradient of graft consolidation. Clin. Oral Implant. Res. 2009, 20, 1078–1083. [Google Scholar] [CrossRef] [PubMed]
- Aimetti, M.; Massei, G.; Morra, M.; Cardesi, E.; Romano, F. Correlation between gingival phenotype and Schneiderian membrane thickness. Int. J. Oral Maxillofac. Implant. 2008, 23, 1128–1132. [Google Scholar] [PubMed]
- Janner, S.F.; Caversaccio, M.D.; Dubach, P.; Sendi, P.; Buser, D.; Bornstein, M.M. Characteristics and dimensions of the Schneiderian membrane: A radiographic analysis using cone beam computed tomography in patients referred for dental implant surgery in the posterior maxilla. Clin. Oral Implant. Res. 2011, 22, 1446–1453. [Google Scholar] [CrossRef] [PubMed]
- Scharf, K.E.; Lawson, W.; Shapiro, J.M.; Gannon, P.J. Pressure measurements in the normal and occluded rabbit maxillary sinus. Laryngoscope 1995, 105, 570–574. [Google Scholar] [CrossRef]

| New Bone | Marrow Spaces | DBBM | Dense Tissue | Loose Tissue | Vessels | Other Tissues | ||
|---|---|---|---|---|---|---|---|---|
| 2 weeks | Small granules | 7.0 ± 4.5; 6.6 | 2.4 ± 2.9; 1.8 | 50.6 ± 6.4; 51.5 | 20.2 ± 3.6; 20.1 | 12.9 ± 5.2; 12.8 | 2.9 ± 2.1; 2.6 | 4.0 * ± 7.1; 1.2 |
| Large granules | 6.3 ± 3.4; 5.4 | 3.2 ± 1.8; 2.7 | 52.6 ± 7.9; 52.4 | 20.3 ± 2.5; 19.7 | 14.6 ± 4.9; 15.9 | 2.6 ± 2.1; 2.1 | 0.4 * ± 0.2; 0.3 | |
| 4 weeks | Small granules | 16.7 ± 3.4; 16.9 | 11.3 ± 9.8; 8.3 | 48.5 ± 4.7; 47.5 | 12.8 ± 7.8; 12.2 | 6.4 ± 3.6; 6.7 | 3.8 ± 1.4; 4.0 | 0.3 ± 0.4; 0.2 |
| Large granules | 18.4 ± 6.0; 18.4 | 11.1 ± 7.4; 9.5 | 43.5 ± 3.2; 42.1 | 12.9 ± 5.7; 11.6 | 8.3 ± 2.3; 8.3 | 5.4 ± 2.2; 4.4 | 0.3 ± 0.3; 0.2 | |
| 8 weeks | Small granules | 27.6 ± 4.6; 27.2 | 16.4 ± 5.0; 16.3 | 46.3 ± 3.4; 46.1 | 6.3 ± 4.4; 5.7 | 2.5 ± 2.0; 2.6 | 0.7 ± 0.5; 0.5 | 0.1 ± 0.3; 0.0 |
| Large granules | 27.6 ± 4.8; 27.0 | 19.2 ± 3.8; 18.6 | 44.3 ± 5.0; 43.8 | 4.2 ± 3.4; 5.1 | 3.1 ± 4.0; 1.2 | 1.3 ± 0.7; 1.3 | 0.3 ± 0.5; 0.0 | |
| New Bone | Marrow Spaces | Dense Tissue | Loose Tissue | Vessels | Osteoclasts | ||
|---|---|---|---|---|---|---|---|
| 2 weeks | Small granules | 10.9 ± 6.3; 12.5 | 1.0 ± 1.1; 0.9 | 70.9 ± 9.1; 73.3 | 12.6 ± 5.5; 14.1 | 0.1 ± 0.2; 0.0 | 4.6 ± 3.7; 3.5 |
| Large granules | 11.9 ± 5.9; 11.5 | 1.5 ± 0.9; 1.7 | 69.6 ± 7.4; 71.4 | 11.5 ± 5.1; 11.4 | 0.3 ± 0.5; 0.0 | 5.1 ± 3.4; 3.9 | |
| 4 weeks | Small granules | 48.6 ± 13.1; 46.3 | 11.7 ± 10.4; 8.3 | 35.0 ± 16.2; 34.4 | 2.6 ± 2.2; 2.1 | 0.0 ± 0.0; 0.0 | 2.2 ± 2.1; 1.6 |
| Large granules | 49.1 ± 18.2; 48.3 | 10.8 ± 9.1; 8.5 | 35.5 ± 19.7; 32.7 | 2.2 ± 2.2; 1.6 | 0.0 ± 0.0; 0.0 | 2.4 ± 2.3; 1.9 | |
| 8 weeks | Small granules | 65.0 ± 7.3; 65.9 | 16.9 ± 3.7; 17.7 | 15.0 ± 8.1; 13.8 | 2.2 ± 2.1; 1.9 | 0.0 ± 0.0; 0.0 | 0.9 ± 0.6; 0.9 |
| Large granules | 62.0 ± 8.7; 61.8 | 15.6 ± 5.8; 15.0 | 21.0 ± 10.0; 18.3 | 0.5 ± 0.6; 0.3 | 0.0 ± 0.0; 0.0 | 0.9 ± 0.6; 0.8 | |
| Small Granules | Large Granules | |||||
|---|---|---|---|---|---|---|
| 2 Weeks | 4 Weeks | 8 Weeks | 2 Weeks | 4 Weeks | 8 Weeks | |
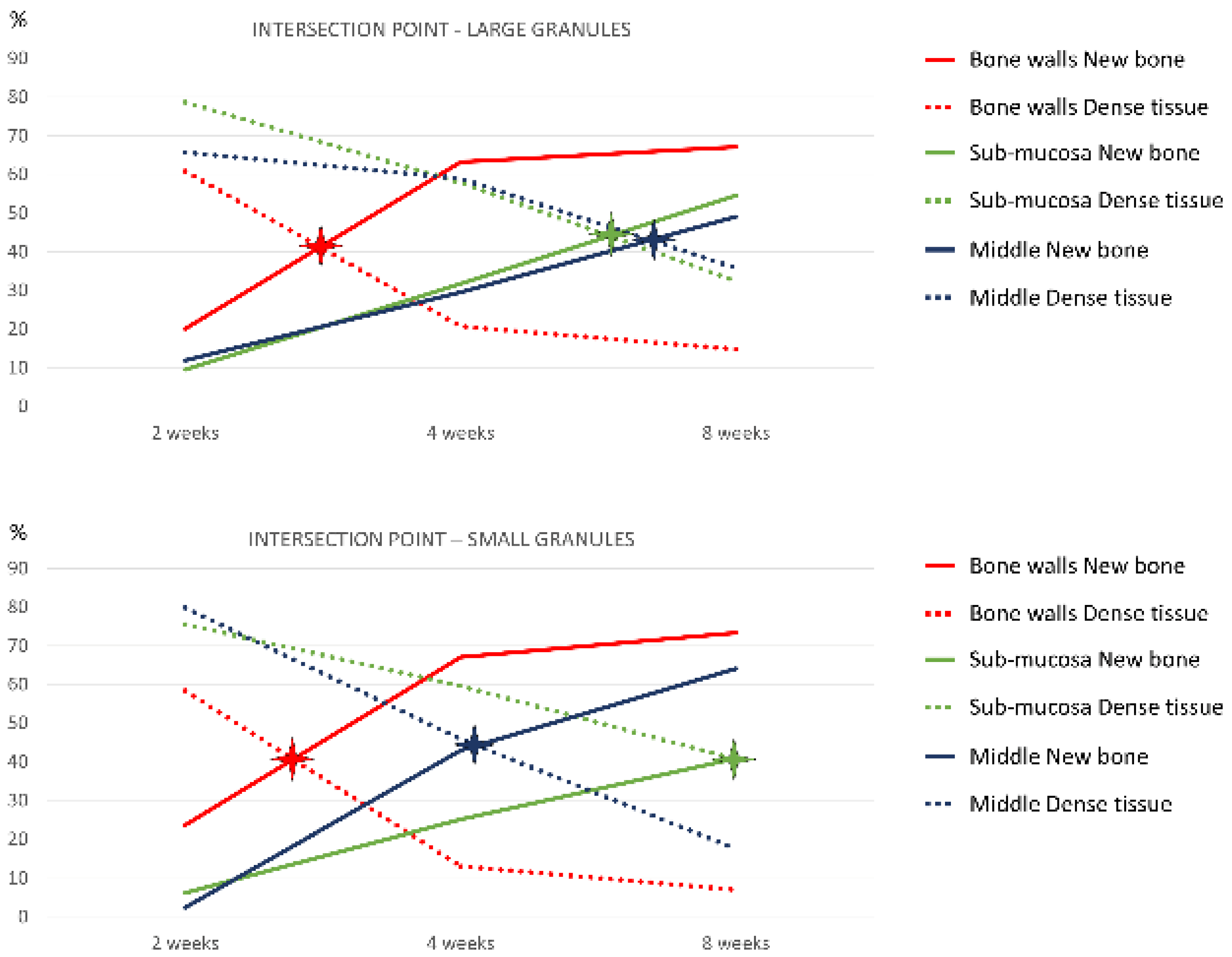
| Bone walls | 23.6 ± 14.2; 29.6 | 67.0 ± 8.2; 69.8 | 73.4 ± 6.2; 73.2 | 20.1 ± 7.7; 17.4 | 63.2 ± 19.2; 67.7 | 67.1 ± 8.1; 67.2 |
| Schneiderian | 6.2 ± 13.8; 0.0 | 25.1 ± 22.1; 25.4 | 40.8 ± 18.1; 45.0 | 9.5 ± 12.7; 4.3 | 31.7 ± 22.3; 32.9 | 54.5 ± 24.9; 57.6 |
| Middle zone | 2.4 ± 5.4; 0.0 | 42.9 ± 23.1; 39.6 | 64.0 ± 20.6; 70.0 | 11.9 ± 15.6; 4.8 | 29.6 ± 23.9; 24.1 | 49.1 ± 22.0; 53.1 |
| Close window | 3.1 ± 4.8; 0.0 | 47.2 ± 15.3; 52.8 | 74.8 ± 4.6; 76.9 | 0.0 ± 0.0; 0.0 | 52.0 ± 24.4; 60.4 | 71.9 ± 8.7; 74.5 |
| Full area | 10.9 ± 6.3; 12.5 | 48.6 ± 13.1; 46.3 | 65.0 ± 3.7; 65.9 | 11.9 ± 5.9; 11.5 | 49.1 ± 18.2; 48.3 | 62.0 ± 8.7; 61.8 |
| Bone Walls | Schneiderian | Middle Zone | Close Window | Full Area | |
|---|---|---|---|---|---|
| Small granules | 19.5; 40.6% | 55.9; 40.8% | 28.6; 44.5% | 26.1; 41.1% | 25.4; 41.6% |
| Large granules | 20.8; 41.2% | 43.2; 44.0% | 47.3; 43.0% | 24.6; 39.5% | 25.3; 42.0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Godoy, E.P.; Apaza Alccayhuaman, K.A.; Botticelli, D.; Amaroli, A.; Balan, V.F.; Silva, E.R.; Xavier, S.P. Osteoconductivity of Bovine Xenograft Granules of Different Sizes in Sinus Lift: A Histomorphometric Study in Rabbits. Dent. J. 2021, 9, 61. https://doi.org/10.3390/dj9060061
Godoy EP, Apaza Alccayhuaman KA, Botticelli D, Amaroli A, Balan VF, Silva ER, Xavier SP. Osteoconductivity of Bovine Xenograft Granules of Different Sizes in Sinus Lift: A Histomorphometric Study in Rabbits. Dentistry Journal. 2021; 9(6):61. https://doi.org/10.3390/dj9060061
Chicago/Turabian StyleGodoy, Eduardo Pires, Karol Alí Apaza Alccayhuaman, Daniele Botticelli, Andrea Amaroli, Vitor Ferreira Balan, Erick Ricardo Silva, and Samuel Porfirio Xavier. 2021. "Osteoconductivity of Bovine Xenograft Granules of Different Sizes in Sinus Lift: A Histomorphometric Study in Rabbits" Dentistry Journal 9, no. 6: 61. https://doi.org/10.3390/dj9060061








