Abstract
The evolution of Internet from static Web “publishing” to the highly participative, and data-driven, innovations of Web 2.0 has been influencing how people search for health-related information. This review included studies indexed in the PubMed electronic database that focused on social media analysis, examining relationships between participants (patients and healthcare consumers) through social media usage. The obtained results showed that previous research regarding social media’s impact on patients and healthcare consumers aimed at a combination of platforms, but there is a penury of information about niche topics or its usage for retrieving medical information. Nevertheless, social media proved to be to be a promising tool in research mainly for recruitment purposes. The review has outlined that eHealth literacy is an attribute for populations that are female and relatively young and educated. Blogs share personal experiences, YouTube contains unregulated, high- and low-quality information that can mislead individuals, Facebook contains more marketing than health-related information, while Wikipedia is recommended for providing high-quality information. Despite healthcare practitioners’ and healthcare public institutions’ reluctance about the use of social media, this review demonstrates the usefulness of social media for patients and healthcare consumers in retrieving health-related information based on content availability and usage implications, and highlights gaps in knowledge that further research needs to fill.
1. Introduction
1.1. Background
The evolution of Internet from the static Web “publishing” to the highly participative, and data-driven, innovations of Web 2.0 is influencing the communication channels for healthcare knowledge [1]. There is a wealth of healthcare information and communication technologies that transform how providers and patients think about access, and act upon, digitally supplied healthcare information. The transformation has an impact upon the clinical encounters, rendering the traditional face-to-face patient encounters as one of many options, and often not the preferred one. Social media facilitates instantaneous information sharing and patients seem to be way ahead of healthcare professionals when using digital technology to access health information [2].
Health 2.0/Medicine 2.0 have been developing concepts with no consensus of their definition. A systematic review published in 2010 provides 46 unique definitions of Health 2.0 and Medicine 2.0 with seven recurrent topics: Web 2.0/technology, patients, professionals, social networking, health information/content, collaboration, and change of health care [3].
The participative and collaborative social media platforms facilitate information creation, sharing and retrieval, creating new bridges for reaching patients or other health care consumers [4].
The unstructured language of patients has been explored through several dimensions including linguistic, sociocultural, and medical informatics studies, but findings suggest that patients have not directly contributed to health information systems; rather, physicians and information systems serve as mediators [5].
1.2. State-of-the Art & Aim
The concept of patient’s rights and responsibilities has been changing proportionally with the increase use of technologies to deliver healthcare, from a traditional passive role to one of ascribed labels such as “informed,” “expert,” “self-managing,” “having responsibilities,” “feeling supported,” “relationships with others,” “experiencing health services,” or “affecting behavior,” affecting the management of patient–health professional relationships [6,7]. Patients’ participation to the creation of health content, through blogging and social networking, is affecting their experiences and has implications upon healthcare management and the retrieving and sharing of health information [8]. Not all patients are likely to support the adoption of Web 2.0 platforms in their care delivery. Patients who are skeptical of its value might hesitate to engage in rehabilitation and health promotion programs that involve social media [9]. For example, a review on the use of social media in child health shows evidence of utility, but further research shows no significant effect [10].
Websites such as Facebook allow individuals to post messages, photos, and videos and to share them with an online group of friends. Such tools can be used to reach professionally a wider range of people than the traditional marketing tools allow [11].
Street et al. show that the development of communities of bloggers with shared experience can “help explain” the experience of living with different diseases [12]. In some topics, the perspectives gathered from web blogs are similar to those sourced from reports and literature reviews, but in other areas, web blogs provide insight that is not available in the published literature. This raises ethical issues like the blurring of public–private boundaries [12]. On the other hand, Wikipedia is evolving into an important medical resource for the public and is attracting a sizable number of experts that are expanding its medical content [13]. Furthermore, Leithner et al. showed that the quality of medical information found on Wikipedia is reliable [14].
The aim of this research was to understand the influence of social media and the importance of patient’s social media usage context in retrieving medical information. Firstly, the evidence was synthesized based on network characteristics and how social networks influenced health consumer’s behavior. Secondly, the relationship between social networks and medical information was examined.
2. Materials and Methods
This review followed the Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA) guidelines [15]. Studies describing social media analysis, or those examining relationships between participants through social media usage indexed in PubMed were included in this review.
2.1. Criteria for Considering the Studies
Studies were included if they reported primary or secondary research, with quantitative analytical designs for answering whether social media is effective for patients’ or healthcare consumers’ use, and to provide context to attributes that may contribute to the effectiveness or lack of effectiveness of its use. Both interventional/experimental (e.g., engaging the consumers via social media platforms) or observational (e.g., data observing patients’ social media behaviors) designs were eligible for our study.
Social media was defined according to Kaplan’s and Haenlein’s classification scheme [16], and was divided into categories as follows: collaborative projects, blogs or microblogs, content communities, social networking sites, and virtual worlds.
Studies that investigated patients or healthcare consumers, regardless of gender, age group, race, ethnic, cultural, or religious group, or location, were evaluated. Based primarily on the need to address the research questions, our main outcome was peer selection and the influence of social media usage.
Studies that examined mobile health applications (e.g., tracking or medical reference apps), and real-time exchanges of medical information mediated by technology (e.g., Skype, chat rooms) [17] were excluded. Furthermore, studies published in a language other than English were also excluded from the analysis.
2.2. Search Strategy
The PubMed database was searched for relevant articles using the research query presented in Figure 1. The PubMed database was chosen because it comprises a large amount of biomedical literature (over 22 million abstracts in 2013) reviewed based on clear scientific criteria [18]. The search was undertaken by December 2015 and included papers published up to then.

Figure 1.
PubMed search strategy.
2.3. Selection of the Studies
Data was extracted using a standardized form developed based on PRISMA guideline [15]. The data extraction form ensured the extraction of pertinent data to provide a comprehensive synthesis of the literature regarding social media analysis of medical information usage. As per the PRISMA guidelines, data was extracted from each article that met the inclusion criteria regarding participants, interventions, results, and social media analysis methodology [15].
Titles and abstracts were screened for inclusion in the first round of screening. The studies identified as eligible in the first screening round were included in the second round of full-text screening. The resources available at the Iuliu Haţieganu University of Medicine and Pharmacy Cluj-Napoca (assured by the Romanian Ministry of Education through AnelisPlus program) were used to retrieve the full-text of the articles that passed the title and abstract screening. If no university access to the full text was available, an e-mail request to the corresponding author was sent by presenting the researchers and their research and asking for a copy of the full text.
Data was extracted independently by two reviewers in both screening steps. The discrepancies regarding data categorization were discussed as a group at each step, and the articles were included in the analysis whenever a consensus existed.
2.4. Analysis
Qualitative, quantitative, and mixed-method data that met the inclusion criteria for the review, including methodological rigor, credibility, and quality standards as outlined, were described and synthesized using narrative synthesis [19]. This approach was used to synthesize the evidence relevant to the research questions, summarizing and explaining the findings of included studies. Results were presented as a percentage and associated 95% confidence intervals using an exact method [20] for qualitative variables. Comparisons between groups on qualitative variables were done using Z-test for proportions at a significance level of 5%. The sample sizes were summarized as the median and interquartile range (IQR = (Q1 − Q3), where Q1 = first quartile and Q3 = third quartile), as the data proved was not normally distributed (Shapiro–Wilk test). The comparison of the sample sizes used in interventional and observational studies was tested using the Mann–Whitney test. The significance level of 5% was used in the statistical analysis, and any p-value less than 0.05 was considered statistically significant.
Preliminary synthesis results in an initial description of the included study, incorporating outcome statistics against research question. As patterns across the study results emerged from the preliminary synthesis, reviewers interrogated the data to identify and gain an understanding about any factors that may explain differences in direction and/or effect. The narrative synthesis of evidence was reported, highlighting the key outcomes. In order to avoid potential biases, key points of difference between studies were identified.
3. Results
3.1. Eligible Studies
Three hundred fifty studies involving social media, medical information, and patient/healthcare consumer-related subjects were identified by applying the aforementioned search strategy. Two hundred fifteen studies passed the title and abstract screening (Figure 2).
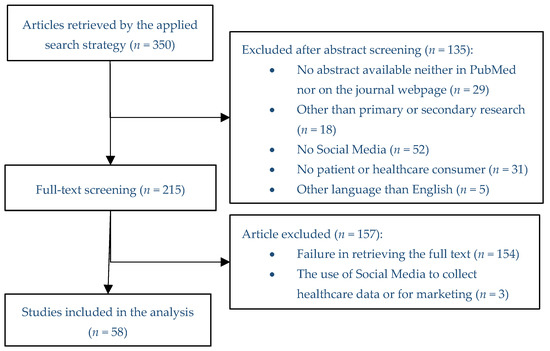
Figure 2.
Flowchart diagram of the selection procedure.
Most of the studies were excluded because they proved not to be social media-related (~39%). The abstract was unavailable for almost 21% of the identified titles, neither in PubMed nor on the webpage of the journal, so these were excluded in the first screening. Almost 13% of the identified titles were excluded as they did not present any primary or secondary research (e.g., 12 narrative reviews, 5 editorials and points of view, and 1 interview). Several titles (~23%) were discarded at the title and abstract screening, as they presented the use of social media as tools in education of healthcare professionals, thus not dealing with patients or healthcare consumers. The majority of the titles discarded related with the language of the article were written in Spanish.
Fifty-eight out of the 215 articles that passed the title and abstract screening were included in the analysis, the main reason of exclusion being the failure in retrieving the full-text (no full text available on the university network and low response rate to full-text e-mail requests).
3.2. Analysis of Eligible Studies
Majority of the included manuscripts had a secondary research design (59%) and 86% of the eligible studies were observational. There is a statistical difference between the percentage of interventional and observational studies (Z = 13.208, p < 0.0001). Most observational studies had a secondary design through web crawling (60.42%, 95% CI [45.877–74.957]). The distribution of design by study is presented in Figure 3.
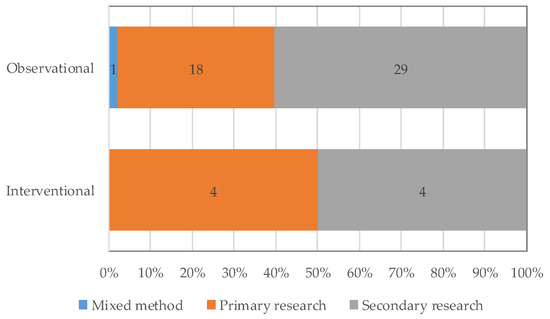
Figure 3.
Design of the eligible studies.
The majority of papers included in the study were aimed at patients (31.03%, 95% CI [18.995–44.798]), the majority of them being diagnosed with different types of cancer and investigating their survival (38.88%, 95% CI [16.98–66.36]).
The investigated statistical unit was questionnaires, posts, pages, and conditions, categories and posts with sample sizes ranging from 11 to 36,042, and as expected with the highest sample on secondary research designs. The manuscript included in the analysis were published in 2007, with the highest number published in 2014 (39.66%, 95% CI [27.616–53.419]) (Figure 4).
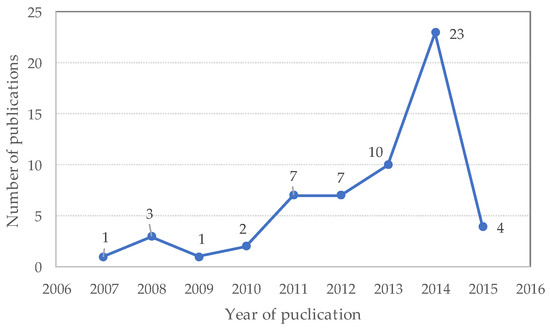
Figure 4.
Number of studies meeting criteria for review, by year (studies published through December 2015).
Mixed social media platforms (comprised of a mixture between Facebook, YouTube, Twitter, and other platforms) (22.41%, 95% CI [12.099–34.453]) were most frequently analyzed. The platforms analyzed independently were as follows: YouTube (15.52%, 95% CI [6.926–27.556]), Facebook (13.79%, 95% CI [5.202–25.832]), blogs (10.34%, 95% CI [3.478–20.66]), Wikipedia (10.34%, 95% CI [3.478–20.66]), and PatientsLikeMe (10.34%, 95% CI [3.478–20.66]), Netwellness (3.45%, 95% CI [0.03–12.039]), and Twitter (3.45%, 95% CI [0.03–12.039]). The remaining research was directed to niche social media platforms.
The top three instruments used by the studies included in the analysis were web crawling, questionnaires or surveys (either online, mailed, or telephone), and interviews (face-to-face, focus group, or by telephone).
Fifty out of 58 studies included in the analysis (86.21% (95% CI [74.168–94.798]) were published in journals indexed also in Web of Science (WOS), most of them classified in Health Care Science & Services as first domain, follow by Oncology and Public, Environmental & Occupational Health (Figure 5). Half of the WOS articles were published in journal classified in the first 25% journals in their domains. Most of the studies included in the analysis were published in the Journal of Medical Internet Research (25.86%, 95% CI [15.547–39.625]).
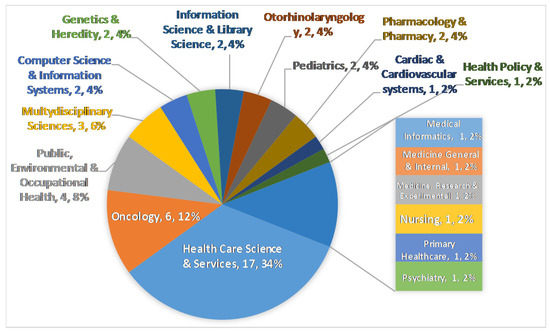
Figure 5.
Main domain of articles published in journals also indexed in the Web of Science.
4. Discussion
4.1. Network Characteristics
Our results showed that the research on social media for patients and healthcare consumers are mainly secondary research papers that analyzed mixed social media platforms such as Facebook, YouTube, and/or Twitter, not going for a one-platform / narrowed investigation.
As shown in previous research [1,2,4], Web 2.0 applications were increasingly used in the health sector with the aim of creating more user-friendly, interactive, and efficient health care systems [21], blogs being an integrating part of this stage of the online healthcare development [22]. Despite the high use of social media, the amount of information available on niche topics and the usage of social media by patients and consumers for retrieving medical information is limited [23].
4.2. Influence Behavior
When referring to online customer engagement, social media showed to be a promising tool for empowering research [24,25]. Social media could be a potential solution to recruitment challenges consumer health IT researchers confront. The study conducted by Pant et al. [26] as well as the one conducted by Biggs et al. [27] suggested that leveraging Facebook is currently a viable means of recruitment for qualitative but not large-scale quantitative research and generally the participants gave positive feedback to the use of Facebook in research [28,29].
Lower age and more education predicted higher eHealth literacy, and more education and being a female was associated with a high usage of Web 2.0 for retrieving health information [30,31,32]. Women [32] and teenagers [33] with a chronic disease were more active in engaging and participating in health-enhancing behaviors online than the general population. Young people extensively used Facebook privacy settings and intentionally disclosed only a few pieces of personal health information to all of their Facebook friends [34].
4.3. Medical Information
Blogs were used more frequently to share emotional support and personal stories than medical knowledge [35,36], thus agreeing with Street et al. [12], who suggested that the use of blogs can lead cancer patients and their companions to engage in meaningful conversation. Furthermore, they suggested that sharing personal experiences via blogs might help patients to better cope with their cancer-related conditions [12].
YouTube hosted a significant number of health-related videos. Several studies showed that the information on this platform was not regulated and contains both high- and low-quality health information. This resulted in misinformation or disinformation for individuals seeking online healthcare information [37,38,39,40,41,42,43].
Not in line with previous published results [10], the Facebook search for common health conditions provided a large number of irrelevant pages, most pages containing marketing/promotion information, while relatively few pages were dedicated to social support [24].
Sustaining previous results [13,14], based on its position among search engine results for health-related queries, Wikipedia is considered a prominent health information website [44]. The participatory model, having majority health specialists [45] but also laypeople of varying editorial skills contributing to the health-related content [46], generates high-quality information. Wikipedia was recommended as an appropriate source of information [22,47].
4.4. Study Limitations
The strengths of our paper lie in the comprehensive and systematic approach of the literature review. Nevertheless, there are limitations that warrant considering. First, it is possible that, despite the attempts to capture all pertinent articles using carefully selected search terms, some relevant studies may have unintentionally been excluded. Consequently, it is possible that pertinent studies have been missed as a result of the keywords used in the article selection process. Secondly, another limitation of the study is the deliberate and detailed approach of reviewing only full-text articles. The limited restriction of available scientific databases in the home institution is a reality that needs to be faced. Due to limited financial support in our study, we sent e-mails to the corresponding authors of those articles without full-text access in the university network. Several articles were included as the authors provided the full-text of their articles. Accordingly, a large number of eligible articles were not considered in this review and the information on these articles could be significant for the research topic. Despite of this limitation, our study identified trends for use of social media within patients and healthcare consumers. Thirdly, there is a potential language bias, as the review was restricted to English-language publications and social media is an internationally recognized and validated tool, potentially relevant publications in other languages were not taken into account.
4.5. Future Research Directions
Understanding how patients and healthcare consumers use social media in identification of healthcare related information can enable the development of new online-friendly engaging tools and social media channels. Further exploration and development of these strategies to build effective information/knowledge platforms that can positively influence the sharing process are needed. One of the greatest challenges in harnessing social media is the constant and rapid evolution, including the continuous development of new technologies and the ever-changing popularity as well as adoption of specific platforms among different user demographics. In order to stay on top of this rapidly evolving landscape, ongoing monitoring of the social media usage for identification of healthcare information is needed.
5. Conclusions
Although healthcare practitioners and healthcare public institutions remain reluctant about the use of social media, this review demonstrates the usefulness of social media in retrieving the healthcare information by the patients and healthcare consumers. The majority of the research conducted to date have been observational, investigating the content of social media and the resulting implications of its use by patients and/or healthcare consumers. Most studies identified in this review investigated the use of social media by patients with cancer indicating a lack of insight about healthcare consumers’ use of social media. Since no study reported any experience on the Romanian population, a further research will aim to investigate the use of social media by patients and consumers to retrieve medical information in a Romanian population.
Acknowledgments
This research was supported by University of Medicine and Pharmacy, Cluj-Napoca, Romania through PCD No. 7690/30/15.04.2016. No funds were received for covering the costs to publish in open access.
Author Contributions
Ariana-Anamaria Cordoş and Sorana Daniela Bolboacă conceived and designed the study, applied the search, and performed the screening; Sorana Daniela Bolboacă and Cristina Drugan analyzed the data; Ariana-Anamaria Cordoş wrote the paper; Sorana Daniela Bolboacă and Cristina Drugan critically reviewed the final version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hesse, B.; O’Connell, M.; Augustson, E.; Chou, W.; Shaikh, A.; Rutten, L. Realizing the promise of Web 2.0: Engaging community intelligence. J. Health Commun. 2011, 16, 10–31. [Google Scholar] [CrossRef] [PubMed]
- Reis, S.; Visser, A.; Frankel, R. Health information and communication technology in healthcare communication: The good, the bad, and the transformative. Patient Educ. Couns. 2013, 93, 359–362. [Google Scholar] [CrossRef] [PubMed]
- Van De Belt, T.; Engelen, L.; Berben, S.; Schoonhoven, L. Definition of Health 2.0 and Medicine 2.0: A systematic review. J. Med. Internet Res. 2010, 12, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Adams, S. Revisiting the online health information reliability debate in the wake of “web 2.0”: An inter-disciplinary literature and website review. Int. J. Med. Inform. 2010, 79, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Smith, C. Consumer language, patient language, and thesauri: A review of the literature. J. Med. Libr. Assoc. 2011, 99, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Finch, T.; Mort, M.; May, C.; Mair, F. Telecare: Perspectives on the changing role of patients and citizens. J. Telemed. Telecare 2005, 11, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Kelly, L.; Jenkinson, C.; Ziebland, S. Measuring the effects of online health information for patients: Item generation for an e-health impact questionnaire. Patient Educ. Couns. 2013, 93, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Ziebland, S.; Wyke, S. Health and illness in a connected world: How might sharing experiences on the internet affect people’s health? Milbank Q. 2012, 90, 219–249. [Google Scholar] [CrossRef] [PubMed]
- Knight, E.; Werstine, R.; Rasmussen-Pennington, D.; Fitzsimmons, D.; Petrella, R. Physical therapy 2.0: Leveraging social media to engage patients in rehabilitation and health promotion. Phys. Ther. 2015, 95, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Hamm, M.; Shulhan, J.; Williams, G.; Milne, A.; Scott, S.; Hartling, L. A systematic review of the use and effectiveness of social media in child health. BMC Pediatr. 2014, 14, 138. [Google Scholar] [CrossRef] [PubMed]
- Devi, S. Facebook friend request from a patient? Lancet 2011, 377, 1141–1142. [Google Scholar]
- Street, J.; Braunack-Mayer, A.; Facey, K.; Ashcroft, R.; Hiller, J. Virtual community consultation? Using the literature and weblogs to link community perspectives and health technology assessment. Health Expect. 2008, 11, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Heilman, J.; Kemmann, E.; Bonert, M.; Chatterjee, A.; Ragar, B.; Beards, G.; Iberri, D.; Harvey, M.; Grover, S.; Lodge, D. Wikipedia: A key tool for global public health promotion. J. Med. Internet Res. 2011, 13, e14. [Google Scholar] [CrossRef] [PubMed]
- Leithner, A.; Maurer-Ertl, W.; Glehr, M.; Friesenbichler, J.; Leithner, K.; Windhager, R. Wikipedia and osteosarcoma: A trustworthy patients’ information? J. Am. Med. Inform. Assoc. 2010, 17, 373–374. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.; The Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 7, e1000097. [Google Scholar]
- Kaplan, A.M.; Haenlein, M. Users of the world, unite! The challenges and opportunities of Social Media. Bus. Horiz. 2010, 53, 59–68. [Google Scholar] [CrossRef]
- Hamm, M.; Chisholm, A.; Shulhan, J.; Milne, A.; Scott, S.; Given, L.; Hartling, L. Social media use among patients and caregivers: A scoping review. BMJ Open 2013, 3, e002819. [Google Scholar] [CrossRef] [PubMed]
- Canese, K.; Weis, S. PubMed: The Bibliographic Database. In The NCBI Handbook [Internet], 2nd ed.; National Center for Biotechnology Information (US): Bethesda, MD, USA, 2013. [Google Scholar]
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N.; Roen, K.; Duffy, S. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC Methods Programme Version. Prod. ESRC Method Program. Version 2006, 1, 1–92. [Google Scholar]
- Jäntschi, L.; Bolboacă, S. Exact Probabilities and Confidence Limits for Binomial Samples: Applied to the Difference between Two Proportions. Sci. World J. 2010, 10, 865–878. [Google Scholar] [CrossRef] [PubMed]
- Hale, T.; Pathipati, A.; Zan, S.; Jethwani, K. Representation of health conditions on Facebook: Content analysis and evaluation of user engagement. J. Med. Internet Res. 2014, 16, e182. [Google Scholar] [CrossRef] [PubMed]
- Laurent, M.R.; Vickers, T. Seeking health information online: Does Wikipedia matter? J. Am. Med. Inform. Assoc. 2009, 16, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Seltzer, E.; Stolley, M.; Mensah, E.; Sharp, L. Social networking site usage among childhood cancer survivors—A potential tool for research recruitment? J. Cancer Surviv. 2014, 8, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Chung, D. Characteristics of cancer blog users. J. Med. Libr. Assoc. 2007, 95, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Neal, D.; McKenzie, P. Putting the pieces together: Endometriosis blogs, cognitive authority, and collaborative information behavior. J. Med. Libr. Assoc. 2011, 99, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Pant, S.; Deshmukh, A.; Murugiah, K.; Kumar, G.; Sachdeva, R.; Mehta, J. Assessing the credibility of the “YouTube approach” to health information on acute myocardial infarction. Clin. Cardiol. 2012, 35, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Biggs, T.; Bird, J.; Harries, P.; Salib, R. YouTube as a source of information on rhinosinusitis: The good, the bad and the ugly. J. Laryngol. Otol. 2013, 127, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Stamelou, M.; Edwards, M.; Espay, A.; Fung, V.; Hallett, M.; Lang, A.; Hallett, M. Movement disorders on YouTube—Caveat spectator. N. Engl. J. Med. 2011, 365, 1160–1161. [Google Scholar] [CrossRef] [PubMed]
- Dubey, D.; Amritphale, A.; Sawhney, A.; Dubey, D.; Srivastav, N. Analysis of YouTube as a source of information for West Nile Virus infection. Clin. Med. Res. 2014, 12, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Mazanderani, F.; O’Neill, B.; Powell, J. “People power” or “pester power”? YouTube as a forum for the generation of evidence and patient advocacy. Patient Educ. Couns. 2013, 93, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Miller, E.; Pole, A. Diagnosis blog: Checking up on health blogs in the blogosphere. Am. J. Public Health 2010, 100, 1514–1519. [Google Scholar] [CrossRef] [PubMed]
- De Viron, S.; Suggs, L.; Brand, A.; Van Oyen, H. Communicating genetics and smoking through social media: Are we there yet? J. Med. Internet Res. 2013, 15, e198. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, K.; Stringer, K.; Donohue, J.; Yu, S.; Shaver, A.; Caruthers, R.; Zikmund-Fisher, B.; Fifer, C.; Goldberg, C.; Russell, M. Social media methods for studying rare diseases. Pediatrics 2014, 133, e1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Van Der Velden, M.; El Emam, K. “Not all my friends need to know”: A qualitative study of teenage patients, privacy, and social media. J. Am. Med. Inform. Assoc. 2013, 20, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Heilman, J.; West, A. Wikipedia and medicine: Quantifying readership, editors, and the significance of natural language. J. Med. Internet Res. 2015, 17, e62. [Google Scholar] [CrossRef] [PubMed]
- Farič, N.; Potts, H. Motivations for contributing to health-related articles on Wikipedia: an interview study. J. Med. Internet Res. 2014, 16, e260. [Google Scholar] [CrossRef] [PubMed]
- Valdez, R.; Guterbock, T.; Thompson, M.; Reilly, J.; Menefee, H.; Bennici, M.; Williams, I.; Rexrode, D. Beyond traditional advertisements: Leveraging Facebook’s social structures for research recruitment. J. Med. Internet Res. 2014, 16, e243. [Google Scholar] [CrossRef] [PubMed]
- De Vries, N.; Carlson, J.; Moscato, P. A data-driven approach to reverse engineering customer engagement models: Towards functional constructs. PLoS ONE 2014, 9, e102768. [Google Scholar]
- Moreno, M.; Grant, A.; Kacvinsky, L.; Moreno, P.; Fleming, M. Older adolescents’ views regarding participation in Facebook research. J. Adolesc. Health 2012, 51, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Kontos, E.; Blake, K.; Chou, W.; Prestin, A. Predictors of eHealth usage: Insights on the digital divide from the Health Information National Trends Survey 2012. J. Med. Internet Res. 2014, 16, e172. [Google Scholar] [CrossRef] [PubMed]
- Tennant, B.; Stellefson, M.; Dodd, V.; Chaney, B.; Chaney, D.; Paige, S.; Alber, J. eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers and older adults. J. Med. Internet Res. 2015, 17, e70. [Google Scholar] [CrossRef] [PubMed]
- Connolly, K.; Crosby, M. Examining e-Health literacy and the digital divide in an underserved population in Hawaii. Hawaii J. Med. Public Health 2014, 73, 44–48. [Google Scholar] [PubMed]
- Blackstock, O.; Haughton, L.; Garner, R.; Horvath, K.; Norwood, C.; Cunningham, C. General and health-related Internet use among an urban, community-based sample of HIV-positive women: Implications for intervention development. AIDS Care 2015, 27, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.; Kok, K.; Ganesh, V.; Thomas, S. Patient information on breast reconstruction in the era of the world wide web. A snapshot analysis of information available on youtube.com. Breast 2014, 23, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Bezner, S.; Hodgman, E.; Diesen, D.; Clayton, J.; Minkes, R.; Langer, J.; Chen, L. Pediatric surgery on YouTube™: Is the truth out there? J. Pediatr. Surg. 2014, 49, 586–589. [Google Scholar] [CrossRef] [PubMed]
- Yaylaci, S.; Serinken, M.; Eken, C.; Karcioglu, O.; Yilmaz, A.; Elicabuk, H.; Dal, O. Are YouTube videos accurate and reliable on basic life support and cardiopulmonary resuscitation? Emerg. Med. Australas. 2014, 26, 474–477. [Google Scholar] [CrossRef] [PubMed]
- Reavley, N.; Mackinnon, A.; Morgan, A.; Alvarez-Jimenez, M.; Hetrick, S.; Killackey, E.; Nelson, B.; Purcell, R.; Yap, M.B.H.; Jorm, A. Quality of information sources about mental disorders: A comparison of Wikipedia with centrally controlled web and printed sources. Psychol. Med. 2012, 42, 1753–1762. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).