Pragmatic Carbohydrate Quality Metrics in Relation to Glycemic Index, Glycemic Load, and Front-of-Pack Warning Labels in Grain Foods
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population and Setting
2.2. Dietary Assessment
2.3. Carbohydrate Metrics
- At least 1 g of fiber (10:1)—First proposed metric, recommended by the American Heart Association based on the naturally occurring carbohydrate-to-fiber ratio found in the whole wheat flour, and aiming to capture the relative balance between the contents of refined starch and added sugar vs. whole grain and bran [12,14].
- At least 1 g of fiber and less than 1 g of free sugars (10:1:1)—Follows the same rationale of the 10:1 metric, with further incorporation of the recommendation of less than 5% of energy from free sugars [10,13,14]. According to the recommendations, a usual diet (e.g., 2000 kcal) should contain 50% of total calories from carbohydrates (e.g., 1000 kcal or 250 g), 25 g of dietary fiber, and less than 5% of total calories from free sugar (e.g., 100 kcal). Altogether, these recommendations are the 10:1:1 metric basis.
- At least 1 g of fiber, and less than 2 g of free sugars per each 1 g of fiber (10:1|1:2)—Follows the same rationale of the 10:1 and further limits the amount of free sugars depending on the fiber content [10,13,14]. This is particularly relevant to investigate whether the balance between fiber and free sugar would favorably affect cardiometabolic health considering differences in glycemic response.
2.4. Glycemic Index and Glycemic Load
2.5. Warning Label Systems
2.6. Statistical Analysis
3. Results
3.1. Grain Foods Meeting Each Carbohydrate Quality Metric
3.2. Association of Carbohydrate Quality Metrics with Glycemic Index and Glycemic Load
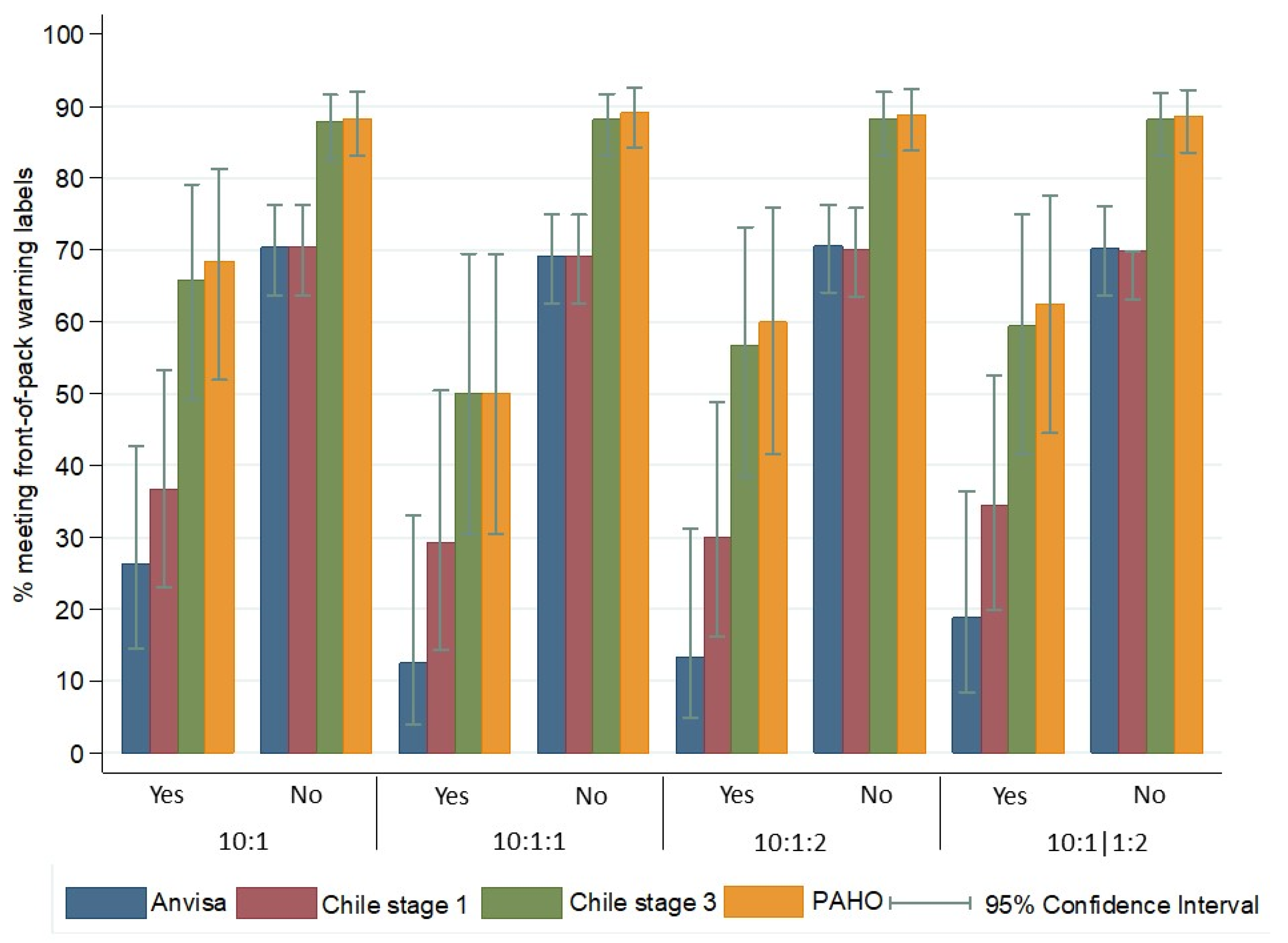
3.3. Association between Carbohydrate Quality Metrics and Warning Labels
3.4. Association between Carbohydrate Quality Metrics and Nutrients from the Warning Labels
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Herforth, A.; Arimond, M.; Alvarez-Sanchez, C.; Coates, J.; Christianson, K.; Muehlhoff, E. A global review of food-based dietary guidelines. Adv. Nutr. 2019, 10, 590–605. [Google Scholar] [CrossRef]
- Willett, W.; Rockstrom, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- World Health Organization. Carbohydrate Intake for Adults and Children: WHO Guideline; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Campos, V.; Tappy, L.; Bally, L.; Sievenpiper, J.L.; Lê, K.A. Importance of carbohydrate quality: What does it mean and how to measure it? J. Nutr. 2022, 152, 1200–1206. [Google Scholar] [CrossRef] [PubMed]
- Seal, C.J.; Courtin, C.M.; Venema, K.; de Vries, J. Health benefits of whole grain: Effects on dietary carbohydrate quality, the gut microbiome, and consequences of processing. Compr. Rev. Food Sci. Food Saf. 2021, 20, 2742–2768. [Google Scholar] [CrossRef]
- Reynolds, A.; Mann, J.; Cummings, J.; Winter, N.; Mete, E.; Te Morenga, L. Carbohydrate quality and human health: A series of systematic reviews and meta-analyses. Lancet 2019, 393, 434–445. [Google Scholar] [CrossRef]
- Mozaffarian, R.S.; Lee, R.M.; Kennedy, M.A.; Ludwig, D.S.; Mozaffarian, D.; Gortmaker, S.L. Identifying whole grain foods: A comparison of different approaches for selecting more healthful whole grain products. Public Health Nutr. 2013, 16, 2255–2264. [Google Scholar] [CrossRef]
- Mathews, R.; Chu, Y. Global review of whole grain definitions and health claims. Nutr. Rev. 2020, 78, 98–106. [Google Scholar] [CrossRef]
- Kissock, K.R.; Neale, E.P.; Beck, E.J. The relevance of whole grain food definitions in estimation of whole grain intake: A secondary analysis of the National Nutrition and Physical Activity Survey 2011–2012. Public Health Nutr. 2020, 23, 1307–1319. [Google Scholar] [CrossRef]
- Liu, J.; Rehm, C.D.; Shi, P.; McKeown, N.M.; Mozaffarian, D.; Micha, R. A comparison of different practical indices for assessing carbohydrate quality among carbohydrate-rich processed products in the US. PLoS ONE 2020, 15, e0231572. [Google Scholar] [CrossRef]
- Tan, D.; Olden, A.N.; Orengo, A.; Francey, C.; Campos, V.C.; Fayet-Moore, F.; Kim, J.E.; Lê, K.A. An assessment of three carbohydrate metrics of nutritional quality for packaged foods and beverages in Australia and Southeast Asia. Nutrients 2020, 12, 2771. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sugars Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Scientific Advisory Committee on Nutrition. Carbohydrates and Health; TSO (The Stationery Office): London, UK, 2015. [Google Scholar]
- Fontanelli, M.D.M.; Micha, R.; Sales, C.H.; Liu, J.; Mozaffarian, D.; Fisberg, R.M. Application of the ≤10:1 carbohydrate to fiber ratio to identify healthy grain foods and its association with cardiometabolic risk factors. Eur. J. Nutr. 2020, 59, 3269–3279. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, F.S.; Brand-Miller, J.C.; Foster-Powell, K.; Buyken, A.E.; Goletzke, J. International tables of glycemic index and glycemic load values 2021: A systematic review. Am. J. Clin. Nutr. 2021, 114, 1625–1632. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Aronne, L.J.; Astrup, A.; de Cabo, R.; Cantley, L.C.; Friedman, M.I.; Heymsfield, S.B.; Johnson, J.D.; King, J.C.; Krauss, R.M. The carbohydrate-insulin model: A physiological perspective on the obesity pandemic. Am. J. Clin. Nutr. 2021, 114, 1873–1885. [Google Scholar] [CrossRef] [PubMed]
- Srichaikul, K.; Jenkins, D.J.A. The glycemic index, rate of digestion of carbohydrate foods, and their potential link with cardiovascular disease. J. Nutr. 2022, 152, 920–921. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization. Front-of-Package Labeling as a Policy Tool for the Prevention of Noncommunicable Diseases in the Americas; PAHO: Washington, DC, USA, 2020. [Google Scholar]
- Crosbie, E.; Gomes, F.S.; Olvera, J.; Rincón-Gallardo Patiño, S.; Hoeper, S.; Carriedo, A. A policy study on front-of-pack nutrition labeling in the Americas: Emerging developments and outcomes. Lancet Reg. Health Am. 2022, 18, 100400. [Google Scholar] [CrossRef] [PubMed]
- Kanter, R.; Vanderlee, L.; Vandevijvere, S. Front-of-package nutrition labelling policy: Global progress and future directions. Public Health Nutr. 2018, 21, 1399–1408. [Google Scholar] [CrossRef]
- Duran, A.C.; Ricardo, C.Z.; Mais, L.A.; Bortoletto Martins, A.P. Role of different nutrient profiling models in identifying targeted foods for front-of-package food labelling in Brazil. Public Health Nutr. 2021, 24, 1514–1525. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.; Escuder, M.M.L.; Goldbaum, M.; Barros, M.B.A.; Fisberg, R.M.; Cesar, C.L.G. Sampling plan in health surveys, city of Sao Paulo, Brazil, 2015. Rev. Saude Publica 2018, 52, 81. [Google Scholar] [CrossRef]
- Brazilian Institute for Geography and Statistics. Brasil/São Paulo/São Paulo 2023. Available online: https://cidades.ibge.gov.br/brasil/sp/sao-paulo/panorama (accessed on 15 March 2023). (In Portuguese)
- Fisberg, R.M.; Sales, C.H.; Fontanelli, M.M.; Pereira, J.L.; Alves, M.C.G.P.; Escuder, M.M.L.; César, C.L.G.; Goldbaum, M. 2015 Health Survey of Sao Paulo with Focus in Nutrition: Rationale, design, and procedures. Nutrients 2018, 10, 169. [Google Scholar] [CrossRef]
- Moshfegh, A.J.; Rhodes, D.G.; Baer, D.J.; Murayi, T.; Clemens, J.C.; Rumpler, W.V.; Paul, D.R.; Sebastian, R.S.; Kuczynski, K.J.; Ingwersen, L.A.; et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am. J. Clin. Nutr. 2008, 88, 324–332. [Google Scholar] [CrossRef] [PubMed]
- University of São Paulo—Food Research Center (FoRC). Brazilian Food Composition Table (Tabela Brasileira de Composição de Alimentos—TBCA). Version 7.2. Sao Paulo 2023. Available online: http://www.fcf.usp.br/tbca (accessed on 20 January 2023). (In Portuguese).
- U.S. Department of Agriculture, Agricultural Research Service. 2019–2020 Food and Nutrient Database for Dietary Studies Documentation. Beltsville, USA, 2022. Available online: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/fndds/2019_2020_FNDDS_Doc.pdf (accessed on 21 April 2024).
- Swan, G.E.; Powell, N.A.; Knowles, B.L.; Bush, M.T.; Levy, L.B. A definition of free sugars for the UK. Public Health Nutr. 2018, 21, 1636–1638. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization. Pan American Health Organization Nutrient Profile Model; PAHO: Washington, DC, USA, 2016. [Google Scholar]
- Brazil Ministry of Health; National Health Surveillance Agency (ANVISA). Resolution of the Collegiate Board 18, March 24, 2008. Technical Regulation Authorizing the Use of Sweetening Additives in Foods, with Their Respective Maximum Limits; Official Diary of the Union: Brasilia, Brazil, 2008. (In Portuguese) [Google Scholar]
- Flood, A.; Subar, A.F.; Hull, S.G.; Zimmerman, T.P.; Jenkins, D.J.; Schatzkin, A. Methodology for adding glycemic load values to the National Cancer Institute Diet History Questionnaire database. J. Am. Diet. Assoc. 2006, 106, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Brazil Ministry of Health; National Health Surveillance Agency (ANVISA). Resolution of the Collegiate Board 429, October 08, 2020. Establishes Nutritional Labeling of Packaged Foods; Official Diary of the Union: Brasilia, Brazil, 2020. (In Portuguese) [Google Scholar]
- Reyes, M.; Garmendia, M.L.; Olivares, S.; Aqueveque, C.; Zacarías, I.; Corvalán, C. Development of the Chilean front-of-package food warning label. BMC Public Health 2019, 19, 906. [Google Scholar] [CrossRef]
- Chilean Ministry of Health. Food Law: Nutrition Labeling Manual. 2019. Available online: https://www.minsal.cl/ley-de-alimentos-manual-etiquetado-nutricional/ (accessed on 11 April 2023). (In Spanish).
- Brazilian Ministry of Health. Food Guide for the Brazilian Population, 2nd ed.; Ministry of Health: Brasilia, Brazil, 2014. (In Portuguese) [Google Scholar]
- Cohen, J.A. Coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- Blaak, E.E.; Antoine, J.M.; Benton, D.; Björck, I.; Bozzetto, L.; Brouns, F.; Diamant, M.; Dye, L.; Hulshof, T.; Holst, J.J.; et al. Impact of postprandial glycemia on health and prevention of disease. Obes. Rev. 2012, 13, 923–984. [Google Scholar] [CrossRef] [PubMed]
- Zeevi, D.; Korem, T.; Zmora, N.; Israeli, D.; Rothschild, D.; Weinberger, A.; Ben-Yacov, O.; Lador, D.; Avnit-Sagi, T.; Lotan-Pompan, M.; et al. Personalized nutrition by prediction of glycemic responses. Cell 2015, 63, 1079–1094. [Google Scholar] [CrossRef] [PubMed]
- Berry, S.E.; Valdes, A.M.; Drew, D.A.; Asnicar, F.; Mazidi, M.; Wolf, J.; Capdevila, J.; Hadjigeorgiou, G.; Davies, R.; Al Khatib, H.; et al. Human postprandial responses to food and potential for precision nutrition. Nat. Med. 2020, 26, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, N.Q.; Mufarrih, S.H.; Bloomfield, G.S.; Tariq, W.; Almas, A.; Mokdad, A.H.; Bartlett, J.; Nisar, I.; Siddiqi, S.; Bhutta, Z.; et al. Disparities in cardiovascular research output and disease outcomes among high-, middle- and low-income countries—An analysis of global cardiovascular publications over the last decade (2008–2017). Glob. Heart 2021, 16, 4. [Google Scholar] [CrossRef]
- Miller, V.; Micha, R.; Choi, E.; Karageorgou, D.; Webb, P.; Mozaffarian, D. Evaluation of the quality of evidence of the association of foods and nutrients with cardiovascular disease and diabetes. JAMA Netw. Open 2022, 5, e2146705. [Google Scholar] [CrossRef]
- Chiavaroli, L.; Lee, D.; Ahmed, A.; Cheung, A.; Khan, T.A.; Blanco, S.M.; Mirrahimi, A.; Jenkins, D.J.A.; Livesey, G.; Wolever, T.M.S.; et al. Effect of low glycaemic index or load dietary patterns on glycaemic control and cardiometabolic risk factors in diabetes: Systematic review and meta-analysis of randomized controlled trials. BMJ 2021, 374, n1651. [Google Scholar] [CrossRef] [PubMed]
- Fisberg, R.M.; Fontanelli, M.M.; Kowalskys, I.; Gómez, G.; Rigotti, A.; Cortés, L.Y.; García, M.Y.; Pareja, R.G.; Herrera-Cuenca, M.; Fisberg, M.; et al. Total and whole grain intake in Latin America: Findings from the multicenter cross-sectional Latin American Study of Health and Nutrition (ELANS). Eur. J. Nutr. 2022, 61, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Fretes, G.; Corvalán, C.; Reyes, M.; Taillie, L.S.; Economos, C.D.; Wilson, N.L.W.; Cash, S.B. Changes in children’s and adolescents’ dietary intake after the implementation of Chile’s law of food labeling, advertising and sales in schools: A longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 40. [Google Scholar] [CrossRef] [PubMed]
- Ricardo, C.Z.; Corvalán, C.; Taillie, L.S.; Quitral, V.; Reyes, M. Changes in the use of non-nutritive sweeteners in the Chilean food and beverage supply after the implementation of the food labeling and advertising law. Front. Nutr. 2021, 8, 773450. [Google Scholar] [CrossRef] [PubMed]
- von Hippel, P.T.; Fliman, F.B. Did child obesity decline after 2016 food regulations in Chile? Rev. Panam. Salud Publica 2024, 48, e16. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Diabetes Endocrinology. Food nutritional information: Transparency and public health. Lancet Diabetes Endocrinol. 2018, 6, 515. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Hao, T.; Rimm, E.B.; Willett, W.C.; Hu, F.B. Changes in diet and lifestyle and long-term weight gain in women and men. N. Engl. J. Med. 2011, 364, 2392–2404. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Hu, F.B.; Tappy, L.; Brand-Miller, J. Dietary carbohydrates: Role of quality and quantity in chronic disease. BMJ 2018, 361, k2340. [Google Scholar] [CrossRef]
- Ljubičić, M.; Sarić, M.M.; Rumbak, I.; Barić, I.C.; Sarić, A.; Komes, D.; Šatalić, Z.; Dželalija, B.; Guiné, R.P.F. Is better knowledge about health benefits of dietary fiber related to food labels reading habits? A Croatian overview. Foods 2022, 11, 2347. [Google Scholar] [CrossRef]
- Moreira, M.J.; García-Díez, J.; de Almeida, J.M.M.M.; Saraiva, C. Consumer knowledge about food labeling and fraud. Foods 2021, 10, 1095. [Google Scholar] [CrossRef]
- Zhang, J.; Zhai, L.; Osewe, M.; Liu, A. Analysis of factors influencing food nutritional labels use in Nanjing, China. Foods 2020, 9, 1796. [Google Scholar] [CrossRef] [PubMed]

| Grain Food Categories 1 | # 2 | % (95% CI) | Percent Meeting Each Metric 3 | Kappa | |||
|---|---|---|---|---|---|---|---|
| 10:1 | 10:1:1 | 10:1:2 | 10:1|1:2 | ||||
| % (95%CI) | % (95%CI) | % (95%CI) | % (95%CI) | ||||
| Flour and dry mixes | 9 | 3.8 (1.9–7.0) | 55.6 (23.5–83.5) | 55.6 (23.5–83.5) | 55.6 (23.5–83.5) | 55.6 (23.5–83.5) | 1.00 |
| Yeast breads, rolls | 50 | 20.5 (15.9–26.1) | 18.0 (9.5–31.3) | 10.0 (4.2–22.1) | 18.0 (9.5–31.3) | 18.0 (9.5–31.3) | 0.85 |
| Quick breads | 5 | 2.0 (0.9–4.9) | 0.0 (-) | 0.0 (-) | 0.0 (-) | 0.0 (-) | 0.00 |
| Cakes, cookies, pies, pastries, bars | 110 | 45.1 (38.9–51.4) | 4.5 (1.9–10.6) | 0.0 (-) | 0.0 (-) | 0.0 (-) | −0.01 |
| Crackers and salty snacks from grain products | 27 | 11.1 (7.7–15.7) | 18.5 (7.8–38.1) | 14.8 (5.5–34.0) | 18.5 (7.8–38.1) | 18.5 (7.7–38.1) | 0.94 |
| Pancakes, waffles, French toast, other grain products | 5 | 2.0 (0.9–4.9) | 0.0 (-) | 0.0 (-) | 0.0 (-) | 0.0 (-) | 0.00 |
| Pastas, cooked cereals, rice | 24 | 9.8 (6.7–14.3) | 25.0 (11.4–46.3) | 25.0 (11.4–46.2) | 25.0 (11.4–46.2) | 25.0 (11.4–46.2) | 1.00 |
| Cereals, not cooked or NS as to cooked | 14 | 5.7 (3.4–9.5) | 57.1 (30.7–80.1) | 28.6 (10.7–57.3) | 35.7 (15.1–63.5) | 50.0 (25.1–74.9) | 0.66 |
| Overall | 244 | 100.0 (-) | 15.6 (11.5–20.7) | 9.8 (6.7–14.3) | 12.3 (8.7–17.1) | 13.1 (9.4–18.0) | 0.86 |
| Carbohydrate Metrics 1 | Glycemic Index | Glycemic Load | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean (SE) | Median (IQR) | Diff. (SE) 2 | p-Value | Mean (SE) | Median (IQR) | Diff. (SE) | p-Value | |
| 10:1 | ||||||||
| Yes 3 | 57.0 (2.5) | 61.4 (25.0) | −9.0 (1.9) | <0.001 | 11.2 (1.2) | 10.9 (10.5) | −10.3 (1.7) | <0.001 |
| No 4 | 66.0 (0.7) | 66.8 (4.3) | 21.5 (1.2) | 17.4 (14.7) | ||||
| 10:1:1 | ||||||||
| Yes | 53.0 (3.5) | 50.8 (30.4) | −12.8 (2.2) | <0.001 | 8.6 (1.5) | 7.7 (9.6) | −12.5 (1.8) | <0.001 |
| No | 65.8 (0.6) | 66.7 (4.6) | 21.1 (1.1) | 17.1 (13.9) | ||||
| 10:1:2 | ||||||||
| Yes | 56.5 (3.1) | 62.9 (30.0) | −9.2 (2.1) | <0.001 | 10.3 (1.4) | 9.1 (9.6) | −10.9 (1.8) | <0.001 |
| No | 65.7 (0.7) | 66.6 (4.4) | 21.2 (1.1) | 17.1 (14.2) | ||||
| 10:1|1:2 | ||||||||
| Yes | 56.2 (3.0) | 57.8 (28.4) | −9.7 (2.0) | <0.001 | 10.6 (1.4) | 9.1 (10.9) | −10.7 (1.8) | <0.001 |
| No | 65.8 (0.7) | 66.7 (4.4) | 21.3 (1.1) | 17.1 (14.2) | ||||
| Overall | 64.6 (0.7) | 66.6 (5.4) | 19.9 (1.0) | 16.1 (14.1) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fontanelli, M.d.M.; Batista, L.D.; Martinez-Arroyo, A.; Mozaffarian, D.; Micha, R.; Rogero, M.M.; Fisberg, R.M.; Sarti, F.M. Pragmatic Carbohydrate Quality Metrics in Relation to Glycemic Index, Glycemic Load, and Front-of-Pack Warning Labels in Grain Foods. Foods 2024, 13, 1299. https://doi.org/10.3390/foods13091299
Fontanelli MdM, Batista LD, Martinez-Arroyo A, Mozaffarian D, Micha R, Rogero MM, Fisberg RM, Sarti FM. Pragmatic Carbohydrate Quality Metrics in Relation to Glycemic Index, Glycemic Load, and Front-of-Pack Warning Labels in Grain Foods. Foods. 2024; 13(9):1299. https://doi.org/10.3390/foods13091299
Chicago/Turabian StyleFontanelli, Mariane de Mello, Lais Duarte Batista, Angela Martinez-Arroyo, Dariush Mozaffarian, Renata Micha, Marcelo Macedo Rogero, Regina Mara Fisberg, and Flavia Mori Sarti. 2024. "Pragmatic Carbohydrate Quality Metrics in Relation to Glycemic Index, Glycemic Load, and Front-of-Pack Warning Labels in Grain Foods" Foods 13, no. 9: 1299. https://doi.org/10.3390/foods13091299






