A One-Year Randomized Controlled Clinical Trial of Three Types of Narrow-Diameter Implants for Fixed Partial Implant-Supported Prosthesis in the Mandibular Incisor Area
Abstract
1. Introduction
2. Materials and Methods
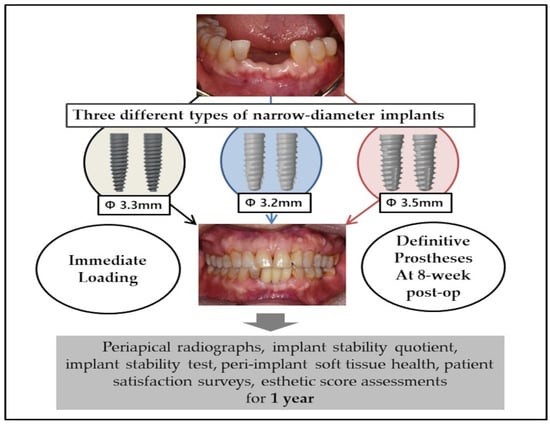
2.1. Clinical Study Design
2.2. Study Populations and Inclusion/Exclusion Criteria
- 19 years of age or older
- Extractions and implant placement of at least two mandibular incisors required
- Healthy adjacent teeth periodontium
- Inter-implant distance ≥ 3 mm; teeth-implant distance ≥ 1.5 mm
- Sufficient amount of bone to obtain primary stability.
- Presence of acute infection in surgical sites
- Extraction of adjacent teeth required due to extensive periodontal disease
- Pregnancy or nursing
- Uncontrolled metabolic systemic diseases (hypertension, diabetes)
- Severe cardiovascular diseases, respiratory diseases, renal or liver diseases, digestive system diseases, blood system diseases, and neuropsychiatric diseases
- Hyperthyroidism or hypothyroidism
- Known history of drug allergy
- Severe depression or anxiety disorder
- History, or current abuse of, drug or alcohol abuse within a year
- Bisphosphonate medication within 4 months
- Heavy smoker
- Lack of occlusal stop.
2.3. Treatment Procedures
2.3.1. Virtual Planning, 3D Surgical Templates, Provisional prostheses
2.3.2. Surgical Procedure
2.3.3. Prosthetic Procedure
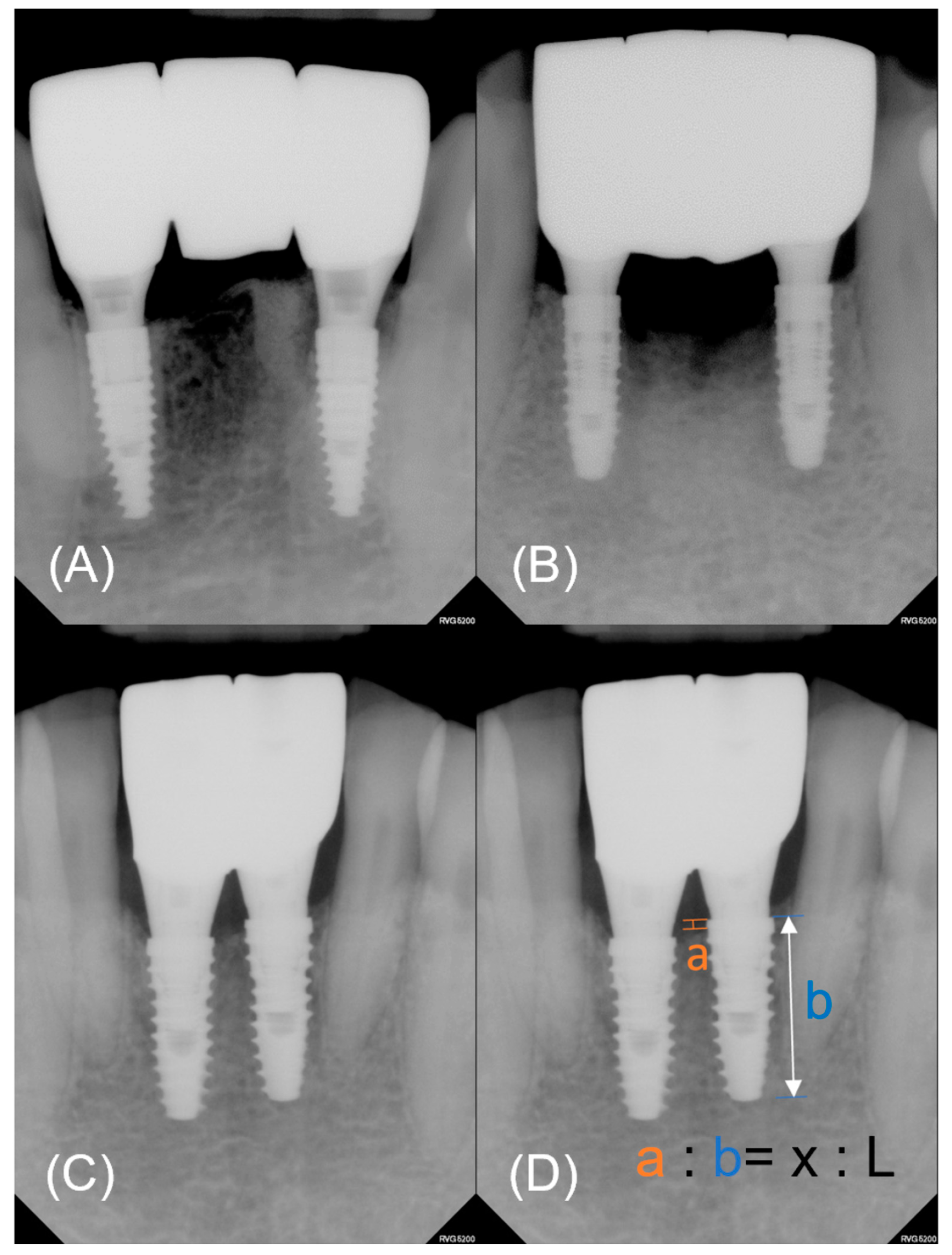
2.3.4. Marginal Bone Loss Evaluation
2.3.5. Peri-Implant Soft Tissue Health, Patient Satisfaction, and Esthetic Score
2.3.6. Follow-Up Visits and Implant Survival and Success
2.4. Statistical Analysis
3. Results
3.1. Demographics
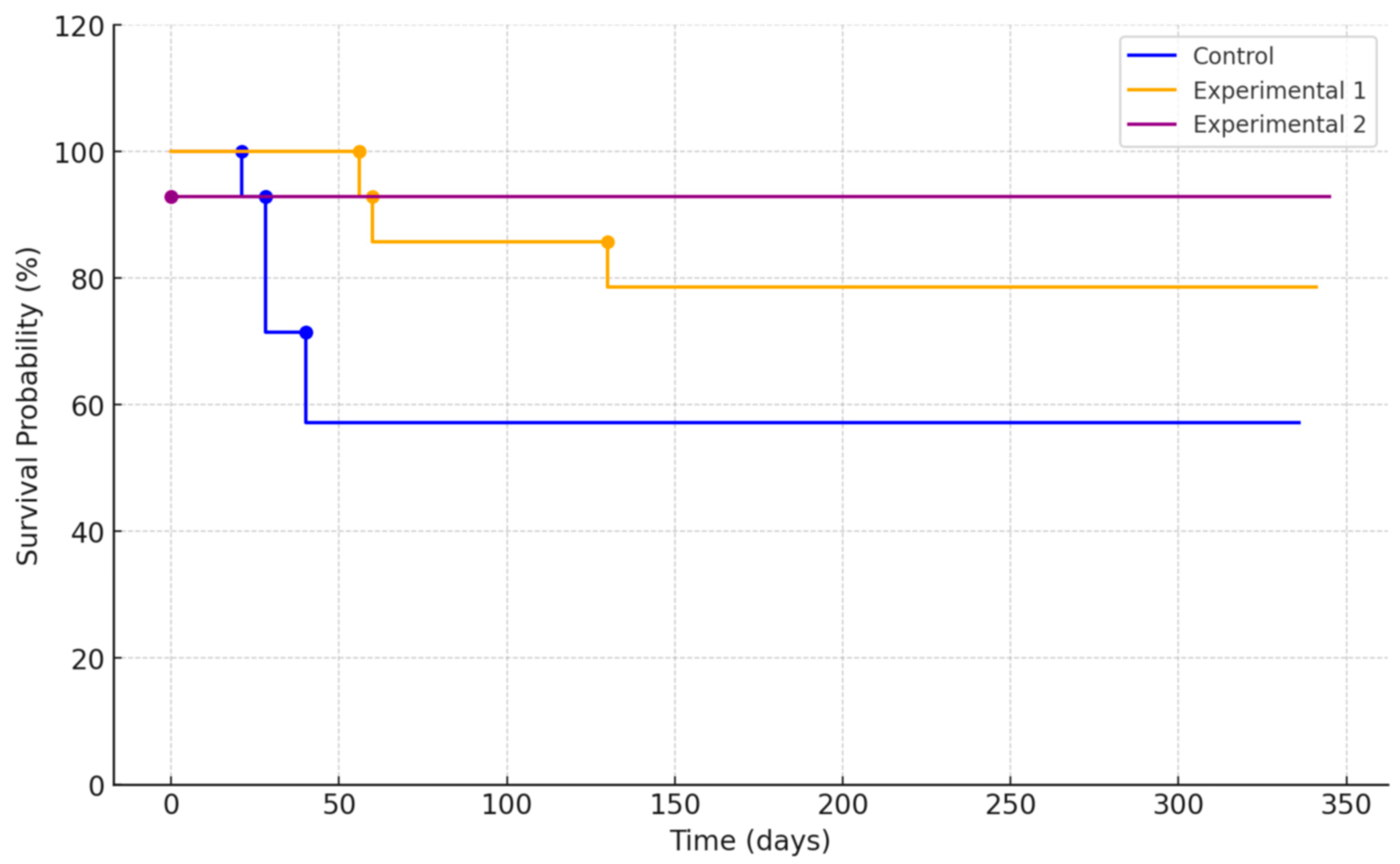
3.2. Survival Rate and Success Rate
3.3. Marginal Bone Loss
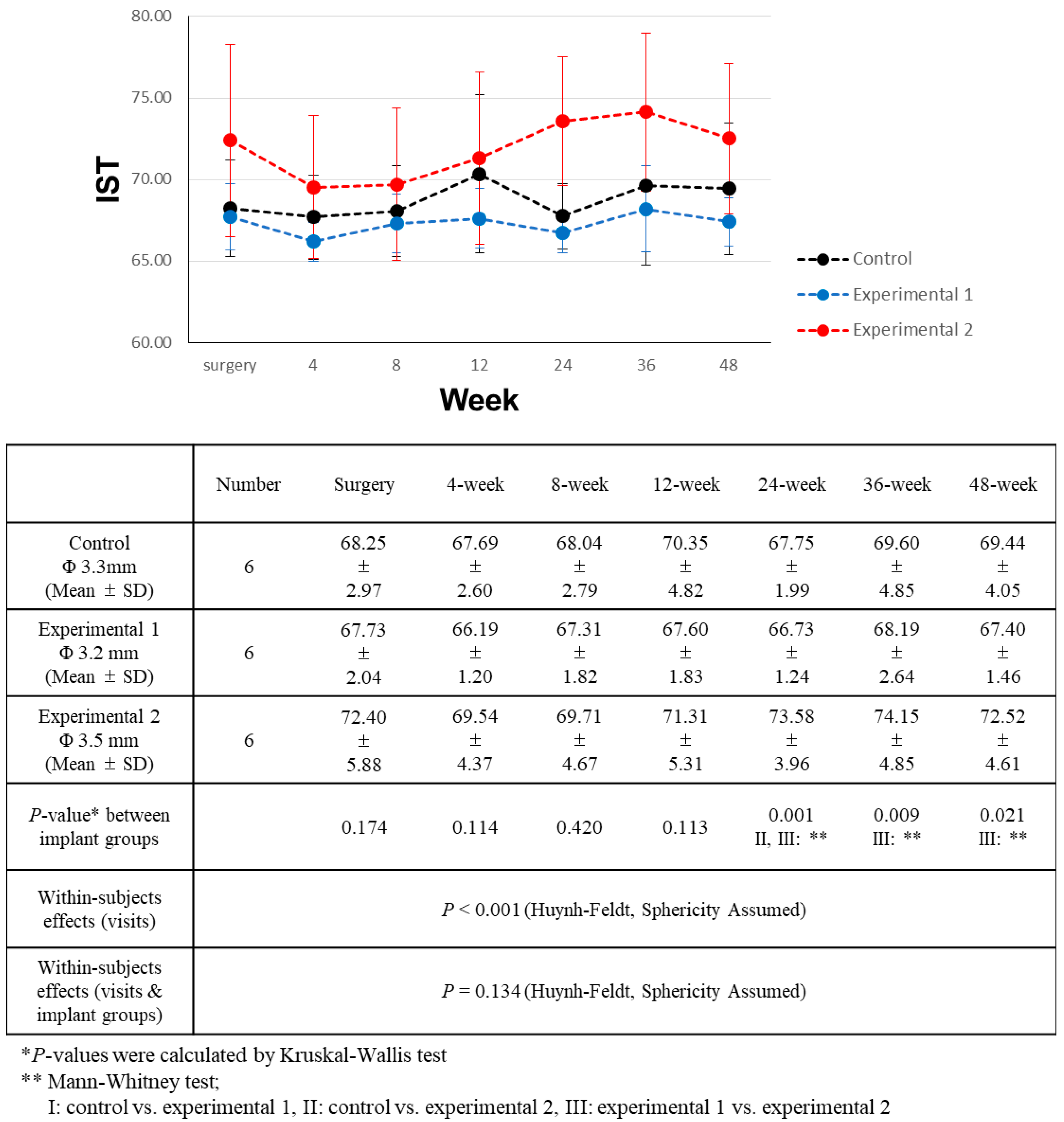
3.4. Implant Stability Comparison
3.5. Soft Tissue Health Parameter
3.6. Pink and White Esthetic Score
3.7. Patient Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Couso-Queiruga, E.; Ahmad, U.; Elgendy, H.; Barwacz, C.; González-Martín, O.; Avila-Ortiz, G. Characterization of Extraction Sockets by Indirect Digital Root Analysis. Int. J. Periodontics Restor. Dent. 2021, 41, 141. [Google Scholar] [CrossRef]
- Chappuis, V.; Araújo, M.G.; Buser, D. Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontology 2000 2017, 73, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Zaniboni, M. Clinical outcomes of GBR procedures to correct peri-implant dehiscences and fenestrations: A systematic review. Clin. Oral Implants Res. 2009, 20, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Schiegnitz, E.; Al-Nawas, B. Narrow-diameter implants: A systematic review and meta-analysis. Clin. Oral Implants Res. 2018, 29, 21–40. [Google Scholar] [CrossRef]
- Davarpanah, M.; Martinez, H.; Tecucianu, J.F.; Celletti, R.; Lazzara, R. Small-diameter implants: Indications and contraindications. J. Esthet. Restor. Dent. 2000, 12, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Piattelli, A.; Carinci, F. Clinical outcome of narrow diameter implants: A retrospective study of 510 implants. J. Periodontol. 2008, 79, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Al-Nawas, B.; Domagala, P.; Fragola, G.; Freiberger, P.; Ortiz-Vigón, A.; Rousseau, P.; Tondela, J. A prospective noninterventional study to evaluate survival and success of reduced diameter implants made from titanium-zirconium alloy. J. Oral Implantol. 2015, 41, e118–e125. [Google Scholar] [CrossRef] [PubMed]
- Klein, M.O.; Schiegnitz, E.; Al-Nawas, B. Systematic review on success of narrow-diameter dental implants. Int. J. Oral Maxillofac. Implants 2014, 29, 43. [Google Scholar] [CrossRef]
- Bidra, A.S.; Almas, K. Mini implants for definitive prosthodontic treatment: A systematic review. J. Prosthet. Dent. 2013, 109, 156–164. [Google Scholar] [CrossRef]
- Vigolo, P.; Givani, A.; Majzoub, Z.; Oordioli, G. Clinical evaluation of small-diameter implants in single-tooth and multiple-implant restorations: A 7-year retrospective study. Int. J. Oral Maxillofac. Implants 2004, 19, 703. [Google Scholar]
- Alrabiah, M. Comparison of survival rate and crestal bone loss of narrow diameter dental implants versus regular dental implants: A systematic review and meta-analysis. J. Investig. Clin. Dent. 2019, 10, e12367. [Google Scholar] [CrossRef]
- Cruz, R.; Lemos, C.; de Batista, V.; Yogui, F.; Oliveira, H.; Verri, F. Narrow-diameter implants versus regular-diameter implants for rehabilitation of the anterior region: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2021, 50, 674–682. [Google Scholar] [CrossRef]
- Ganeles, J.; Zöllner, A.; Jackowski, J.; Ten Bruggenkate, C.; Beagle, J.; Guerra, F. Immediate and early loading of Straumann implants with a chemically modified surface (SLActive) in the posterior mandible and maxilla: 1-year results from a prospective multicenter study. Clin. Oral Implants Res. 2008, 19, 1119–1128. [Google Scholar] [CrossRef] [PubMed]
- Ioannidou, E.; Doufexi, A. Does loading time affect implant survival? A meta-analysis of 1266 implants. J. Periodontol. 2005, 76, 1252–1258. [Google Scholar] [CrossRef] [PubMed]
- Ye, M.; Liu, W.; Cheng, S.; Yan, L. Immediate vs conventional loading of mandibular overdentures: A comprehensive systematic review and meta-analysis of randomized controlled trials. J. Oral Implantol. 2022, 48, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Khzam, N.; Arora, H.; Kim, P.; Fisher, A.; Mattheos, N.; Ivanovski, S. Systematic review of soft tissue alterations and esthetic outcomes following immediate implant placement and restoration of single implants in the anterior maxilla. J. Periodontol. 2015, 86, 1321–1330. [Google Scholar] [CrossRef] [PubMed]
- Glauser, R.; Zembic, A.; Hämmerle, C.H. A systematic review of marginal soft tissue at implants subjected to immediate loading or immediate restoration. Clin. Oral Implants Res. 2006, 17, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Al-Nawas, B.; Brägger, U.; Meijer, H.J.; Naert, I.; Persson, R.; Perucchi, A.; Quirynen, M.; Raghoebar, G.M.; Reichert, T.E.; Romeo, E. A double-blind randomized controlled trial (rct) of titanium-13zirconium versus titanium grade iv small-diameter bone level implants in edentulous mandibles–results from a 1-year observation period. Clin. Implant Dent. Relat. Res. 2012, 14, 896–904. [Google Scholar] [CrossRef] [PubMed]
- Mombelli, A.; Van Oosten, M.; Schürch, E., Jr.; Lang, N. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol. Immunol. 1987, 2, 145–151. [Google Scholar] [CrossRef]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef]
- Fürhauser, R.; Florescu, D.; Benesch, T.; Haas, R.; Mailath, G.; Watzek, G. Evaluation of soft tissue around single-tooth implant crowns: The pink esthetic score. Clin. Oral Implants Res. 2005, 16, 639–644. [Google Scholar] [CrossRef]
- Belser, U.C.; Grütter, L.; Vailati, F.; Bornstein, M.M.; Weber, H.P.; Buser, D. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: A cross-sectional, retrospective study in 45 patients with a 2-to 4-year follow-up using pink and white esthetic scores. J. Periodontol. 2009, 80, 140–151. [Google Scholar] [CrossRef]
- Karoussis, I.K.; Salvi, G.E.; Heitz-Mayfield, L.J.; Brägger, U.; Hämmerle, C.H.; Lang, N.P. Long-term implant prognosis in patients with and without a history of chronic periodontitis: A 10-year prospective cohort study of the ITI® Dental Implant System. Clin. Oral Implants Res. 2003, 14, 329–339. [Google Scholar] [CrossRef]
- Kahraman, S.; Bal, B.; Asar, N.; Turkyilmaz, I.; Tözüm, T. Clinical study on the insertion torque and wireless resonance frequency analysis in the assessment of torque capacity and stability of self-tapping dental implants. J. Oral Rehabil. 2009, 36, 755–761. [Google Scholar] [CrossRef]
- Kim, H.-J.; Kim, Y.-K.; Joo, J.-Y.; Lee, J.-Y. A resonance frequency analysis of sandblasted and acid-etched implants with different diameters: A prospective clinical study during the initial healing period. J. Periodontal Implant Sci. 2017, 47, 106–115. [Google Scholar] [CrossRef]
- Guler, A.U.; Sumer, M.; Duran, I.; Sandikci, E.O.; Telcioglu, N.T. Resonance frequency analysis of 208 Straumann dental implants during the healing period. J. Oral Implantol. 2013, 39, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Degidi, M.; Iezzi, G.; Petrone, G.; Piattelli, A. Correlation between implant stability quotient and bone-implant contact: A retrospective histological and histomorphometrical study of seven titanium implants retrieved from humans. Clin. Implant Dent. Relat. Res. 2006, 8, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Nkenke, E.; Hahn, M.; Weinzierl, K.; Radespiel-Tröger, M.; Neukam, F.W.; Engelke, K. Implant stability and histomorphometry: A correlation study in human cadavers using stepped cylinder implants. Clin. Oral Implants Res. 2003, 14, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.-L.; Tsai, M.-T.; Su, K.-C.; Li, Y.-F.; Hsu, J.-T.; Chang, C.-H.; Fuh, L.-J.; Wu, A.Y.-J. Relation between initial implant stability quotient and bone-implant contact percentage: An in vitro model study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, e356–e361. [Google Scholar] [CrossRef] [PubMed]
- Romeo, E.; Lops, D.; Amorfini, L.; Chiapasco, M.; Ghisolfi, M.; Vogel, G. Clinical and radiographic evaluation of small-diameter (3.3-mm) implants followed for 1–7 years: A longitudinal study. Clin. Oral Implants Res. 2006, 17, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Pedrinaci, I.; Sun, T.C.; Sanz, M.; Sanz-Esporrin, J.; Hamilton, A.; Gallucci, G.O. Implant survival in the anterior mandible: A retrospective cohort study. Clin. Oral Implants Res. 2023, 34, 463–474. [Google Scholar] [CrossRef]
- Lee, J.S.; Kim, H.M.; Kim, C.S.; Choi, S.H.; Chai, J.K.; Jung, U.W. Long-term retrospective study of narrow implants for fixed dental prostheses. Clin. Oral Implants Res. 2013, 24, 847–852. [Google Scholar] [CrossRef]
- Lambert, F.E.; Lecloux, G.; Grenade, C.; Bouhy, A.; Lamy, M.; Rompen, E.H. Less invasive surgical procedures using narrow-diameter implants: A prospective study in 20 consecutive patients. J. Oral Implantol. 2015, 41, 693–699. [Google Scholar] [CrossRef]
- Grandi, T.; Svezia, L.; Grandi, G. Narrow implants (2.75 and 3.25 mm diameter) supporting a fixed splinted prostheses in posterior regions of mandible: One-year results from a prospective cohort study. Int. J. Implant Dent. 2017, 3, 43. [Google Scholar] [CrossRef] [PubMed]
- Blanes, R.J.; Bernard, J.P.; Blanes, Z.M.; Belser, U.C. A 10-year prospective study of ITI dental implants placed in the posterior region. I: Clinical and radiographic results. Clin. Oral Implants Res. 2007, 18, 699–706. [Google Scholar] [CrossRef]
- Ortega-Oller, I.; Suárez, F.; Galindo-Moreno, P.; Torrecillas-Martínez, L.; Monje, A.; Catena, A.; Wang, H.L. The influence of implant diameter on its survival: A meta-analysis based on prospective clinical trials. J. Periodontol. 2014, 85, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Ćorić, A.; Kovačić, I.; Kiršić, S.P.; Čelebić, A. Are Mini Dental Implants Suitable for Support of Crowns or Small Bridges in the Mandibular Incisor Region? A 5-year Longitudinal Study. J. Oral Maxillofac. Surg. 2022, 80, 1811–1826. [Google Scholar] [CrossRef] [PubMed]
- Bergkvist, G.; Simonsson, K.; Rydberg, K.; Johansson, F.; Dérand, T. A finite element analysis of stress distribution in bone tissue surrounding uncoupled or splinted dental implants. Clin. Implant Dent. Relat. Res. 2008, 10, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.-M.; Leu, L.-J.; Wang, J.-S.; Lin, L.-D. Effects of prosthesis materials and prosthesis splinting on peri-implant bone stress around implants in poor-quality bone: A numeric analysis. Int. J. Oral Maxillofac. Implants 2002, 17, 231. [Google Scholar] [PubMed]
- Guichet, D.L.; Yoshinobu, D.; Caputo, A.A. Effect of splinting and interproximal contact tightness on load transfer by implant restorations. J. Prosthet. Dent. 2002, 87, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Hoshaw, S.J.; Brunski, J.B.; Cochran, G.V. Mechanical loading of Brånemark implants affects interfacial bone modeling and remodeling. Int. J. Oral Maxillofac. Implants 1994, 9, 345. [Google Scholar]
- Quirynen, M.; Naert, I.; Van Steenberghe, D. Fixture design and overload influence marginal bone loss and future success in the Brånemark® system. Clin. Oral Implants Res. 1992, 3, 104–111. [Google Scholar] [CrossRef] [PubMed]
- de Medeiros, R.A.; Pellizzer, E.P.; Vechiato Filho, A.J.; Dos Santos, D.M.; da Silva, E.V.; Goiato, M.C. Evaluation of marginal bone loss of dental implants with internal or external connections and its association with other variables: A systematic review. J. Prosthet. Dent. 2016, 116, 501–506.e5. [Google Scholar] [CrossRef] [PubMed]
- Vercruyssen, M.; Coucke, W.; Naert, I.; Jacobs, R.; Teughels, W.; Quirynen, M. Depth and lateral deviations in guided implant surgery: An RCT comparing guided surgery with mental navigation or the use of a pilot-drill template. Clin. Oral Implants Res. 2015, 26, 1315–1320. [Google Scholar] [CrossRef] [PubMed]
- Olate, S.; Lyrio, M.C.N.; de Moraes, M.; Mazzonetto, R.; Moreira, R.W.F. Influence of diameter and length of implant on early dental implant failure. J. Oral Maxillofac. Surg. 2010, 68, 414–419. [Google Scholar] [CrossRef]



| Control Group | Experimental 1 | Experimental 2 | |
|---|---|---|---|
| Straumann® BLT NC, SLActive® | NeoBiotech CMI IS-III Active® S-Narrow | NeoBiotech CMI IS-III Active® Narrow | |
| Diameter | Φ 3.3 mm | Φ 3.2 mm | Φ 3.5 mm |
| Body Shape | Tapered Body | Straight Body | Straight Body |
| Pitch Height | 0.8 mm | 0.9 mm | 0.9 mm |
| Thread Depth | 0.3 mm | 0.25 mm | 0.35 mm |
| Implant-Abutment Interface | Internal Conical (15°) | Internal Conical (11°, 2.1 hex) | Internal Conical (11°, 2.1 hex) |
| Surface Treatment | SLA surface | SLA surface | SLA surface |
| Micro Threads | None | None | None |
| Variables | Control (Straumann BLT® Φ 3.3 mm NC, SLActive®) | Experimental 1 (NeoBiotech IS-III Active® S-Narrow) | Experimental 2 (NeoBiotech IS-III Active® Narrow) | p-Value * | |
|---|---|---|---|---|---|
| Subject based (N = 18) | Participant number | 6 | 6 | 6 | - |
| Age (Mean ± SD) | 61.17 ± 4.98 | 67.50 ± 5.88 | 66.33 ± 5.62 | ||
| 20–60 | 3 | 2 | 1 | 0.532 | |
| Over 60 | 3 | 4 | 5 | 0.378 | |
| Sex Male/Female | 4/2 | 1/5 | 3/3 | 0.226 | |
| Implant based (N = 36) | Implant number | 12 | 12 | 12 | - |
| Mandibular central incisors (Left/right) | 0/0 | 2/3 | 1/3 | ||
| Mandibular lateral incisors (Left/right) | 6/6 | 3/4 | 5/3 | ||
| Prostheses unit number (2/3/4) | 0/0/6 | 2/2/2 | 1/2/3 | ||
| Implant type (number of implants) | Φ 3.3 × 10 mm (9) | Φ 3.2 × 10 mm (8) | Φ 3.5 × 10 mm (8) | ||
| Φ 3.3 × 12 mm (3) | Φ 3.2 × 11.5 mm (4) | Φ 3.5 × 11.5 mm (4) | |||
| Bone graft | Number (application/implants) | 5/12 | 7/12 | 4/12 |
| Implant Type | Number of Failed Patients/Implants | Time Point | Implant Position | Implant Size | Bone Graft | Failure Mode | Cause of Failure |
|---|---|---|---|---|---|---|---|
| Control * (BLT Φ 3.3 mm NC, SLActive®) | 3/4 | Visit 5 | #32 | Φ 3.3 × 10 mm | Yes | Fixture failure | Severe peri-implantitis |
| Visit 6 | #32 | Φ 3.3 × 10 mm | No | Fixture failure | Osseointegration failure (peri-implant radiolucency) | ||
| Visit 7 | #32 ** | Φ 3.3 × 12 mm | No | Fixture failure | Osseointegration failure (mobility without peri-implant radiolucency) | ||
| Visit 7 | #42 ** | Φ 3.3 × 12 mm | No | Fixture failure | |||
| Experimental 1 (CMI IS-III Active ® S-Narrow Φ 3.2 mm) | 3/3 | Visit 5 | #42 | Φ 3.2 × 10 mm | Yes | Fixture failure | Use of hard food reported |
| Visit 7 | #32 | Φ 3.2 × 10 mm | Yes | ISQ or IST < 65 | |||
| Visit 7 | #31 | Φ 3.2 × 10 mm | No | Fixture failure | Osseointegration failure (peri-implant radiolucency) | ||
| Experimental 2 (CMI IS-III Active ® Narrow Φ 3.5 mm) | 1/1 | Visit 3 (Surgery) | #42 | Φ 3.5 × 10 mm | No | ISQ or IST < 65 |
| Control | Experimental 1 | Experimental 2 | |||
|---|---|---|---|---|---|
| Patient Number | 3 | 4 | 6 | ||
| Duration | Area | Mean ± SD (mm) | Mean ± SD (mm) | Mean ± SD (mm) | p-Value * |
| 12 week follow up | Mesial | 0.00 ± 0.00 | 0.59 ± 0.59 | 0.71 ± 0.73 | 0.055 |
| Distal | 0.19 ± 0.31 | 0.02 ± 0.05 | 0.25 ± 0.43 | 0.592 | |
| Avg. | 0.10 ± 0.15 | 0.30 ± 0.31 | 0.48 ± 0.50 | 0.224 | |
| 24 week follow up | Mesial | 0.20 ± 0.44 | 0.65 ± 0.41 | 0.68 ± 0.68 | 0.185 |
| Distal | 0.33 ± 0.37 | 0.13 ± 0.36 | 0.17 ± 0.35 | 0.384 | |
| Avg. | 0.26 ± 0.23 | 0.39 ± 0.17 | 0.42 ± 0.40 | 0.684 | |
| 48 week follow up | Mesial | 0.32 ± 0.48 | 0.74 ± 0.39 | 0.64 ± 0.63 | 0.309 |
| Distal | 0.43 ± 0.32 | 0.13 ± 0.33 | 0.10 ± 0.26 | 0.078 | |
| Avg. | 0.38 ± 0.36 | 0.43 ± 0.30 | 0.37 ± 0.37 | 0.749 | |
| Control | Experimental I | Experimental II | p-Value * | |
|---|---|---|---|---|
| Participant number | 6 | 6 | 6 | - |
| Insertion torque (Ncm)(Mean ± SD) | 37.92 ± 2.47 | 41.25 ± 3.61 | 37.92 ± 3.80 | 0.048 |
| ISQ at surgery (Mean ± SD) | 67.32 ± 2.79 | 68.67 ± 3.16 | 68.21 ± 2.31 | 0.355 |
| IST at surgery (Mean ± SD) | 67.72 ± 2.04 | 73.40 ± 5.88 | 68.25 ± 2.97 | 0.174 |
| Control | Experimental 1 | Experimental 2 | ||
|---|---|---|---|---|
| ISQ | Pearson Correlation Coefficient | 0.274 * | 0.111 | 0.709 ** |
| R2 | 0.075 | 0.012 | 0.503 | |
| IST | Pearson Correlation Coefficient | 0.136 | 0.090 | 0.188 |
| R2 | 0.019 | 0.008 | 0.035 |
| Control | Experimental 1 | Experimental 2 | ||
|---|---|---|---|---|
| Participant number | 4 | 5 | 6 | |
| Parameters | Mean ± SD (mm) | Mean ± SD (mm) | Mean ± SD (mm) | p-value * |
| Modified plaque index | 1.15 ± 0.87 | 1.05 ± 0.54 | 0.90 ± 0.58 | 0.113 |
| Modified sulcus bleeding index | 0.75 ± 0.63 | 0.63 ± 0.68 | 0.68 ± 0.57 | 0.540 |
| Pocket Depth (mm) | 3.53 ± 0.49 | 3.55 ± 0.43 | 3.35 ± 0.75 | 0.832 |
| Width of keratinized mucosa (mm) | 4.00 ± 0.50 | 4.40 ± 1.11 | 4.08 ± 1.38 | 0.750 |
| PES (Maximum 14) | WES (Maximum 10) | |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Control | 8.00 ± 0.82 | 3.67 ± 0.47 |
| Experimental 1 | 9.25 ± 2.86 | 5.50 ± 0.50 |
| Experimental 2 | 10.50 ± 1.12 | 7.17 ± 2.54 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, J.-H.; Lim, Y.-J.; Lee, J.; Baek, Y.-W.; Kim, M.-J.; Kwon, H.-B. A One-Year Randomized Controlled Clinical Trial of Three Types of Narrow-Diameter Implants for Fixed Partial Implant-Supported Prosthesis in the Mandibular Incisor Area. Bioengineering 2024, 11, 272. https://doi.org/10.3390/bioengineering11030272
Ahn J-H, Lim Y-J, Lee J, Baek Y-W, Kim M-J, Kwon H-B. A One-Year Randomized Controlled Clinical Trial of Three Types of Narrow-Diameter Implants for Fixed Partial Implant-Supported Prosthesis in the Mandibular Incisor Area. Bioengineering. 2024; 11(3):272. https://doi.org/10.3390/bioengineering11030272
Chicago/Turabian StyleAhn, Ji-Ho, Young-Jun Lim, Jungwon Lee, Yeon-Wha Baek, Myung-Joo Kim, and Ho-Beom Kwon. 2024. "A One-Year Randomized Controlled Clinical Trial of Three Types of Narrow-Diameter Implants for Fixed Partial Implant-Supported Prosthesis in the Mandibular Incisor Area" Bioengineering 11, no. 3: 272. https://doi.org/10.3390/bioengineering11030272
APA StyleAhn, J.-H., Lim, Y.-J., Lee, J., Baek, Y.-W., Kim, M.-J., & Kwon, H.-B. (2024). A One-Year Randomized Controlled Clinical Trial of Three Types of Narrow-Diameter Implants for Fixed Partial Implant-Supported Prosthesis in the Mandibular Incisor Area. Bioengineering, 11(3), 272. https://doi.org/10.3390/bioengineering11030272